Person-Centeredness in Digital Primary Healthcare Services—A Scoping Review
Abstract
1. Background
2. Methods
2.1. Design
2.2. Stage One: Identifying the Research Question
- How is research conducted within the field of PC and digital primary health care?
- What sort of available evidence exists within the field of PC and digital primary health care?
- What are the knowledge gaps within the field of PC and digital primary health care?
2.3. Stage Two: Finding Relevant Studies
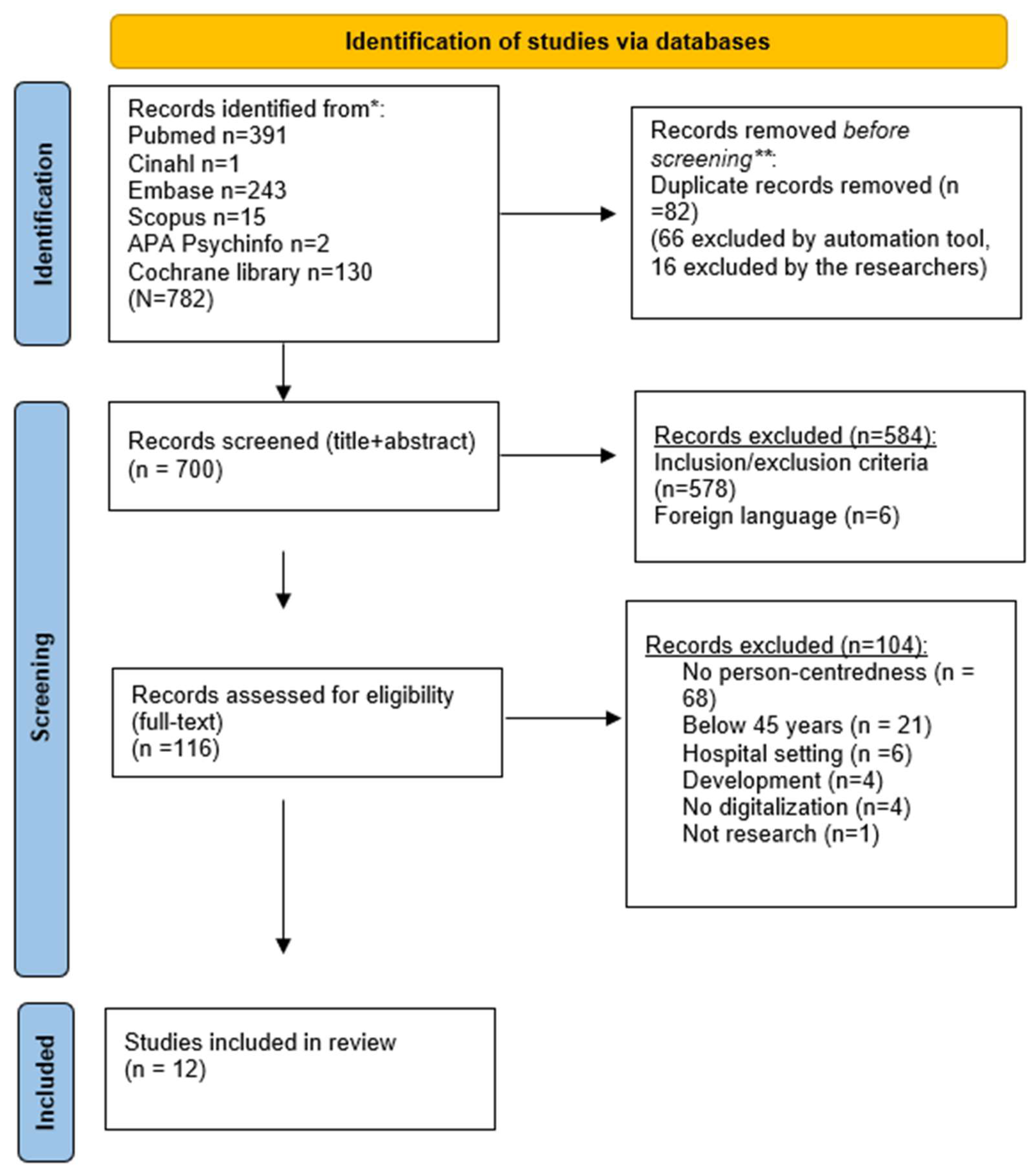
2.4. Stage Three: Study Selection
- Primary/community healthcare services;
- Digital healthcare services;
- Person or patient centeredness;
- Middle-aged and aged adults (45 years and older) [28];
- Scandinavian and English language;
- Peer-reviewed articles;
- Not limited to study design or methodological approach.
- Research published before 2012;
- Conference abstracts;
- Unpublished material;
- Dissertations;
- Reviews;
- Electronic health records;
- Abstract missing.
2.5. Stage Four: Charting the Data
2.6. Stage Five: Collating, Summarizing and Reporting the Results
3. Results
3.1. Description of the Included Studies
3.2. Methods Used in the Included Studies
3.3. Existing Evidence
3.3.1. Accessibility
3.3.2. Self-Management
3.3.3. Digitalization at Odds with Patient-Centeredness
3.3.4. Situation Awareness
3.4. Knowledge Gaps
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- OECD Empowering the Health Workforce. Strategies to Make the Most of the Digital Revolution. 2021. Available online: https://www.oecd.org/publications/empowering-the-health-workforce-to-make-the-most-of-the-digital-revolution-37ff0eaa-en.htm (accessed on 5 April 2023).
- Bureau of Labor Statistics. Employment Projections. 2017. Available online: https://data.bls.goc/projections/occupationProj (accessed on 5 April 2023).
- World Health Organization. Recommendations on Digital Interventions for Health System Strengthening. 2019. Available online: https://www.who.int/publications/i/item/9789241550505 (accessed on 5 April 2023).
- Digital Health Workforce Academy. What Is Digital Health? And Why Does It Matter? 2020. Available online: https://www.hisa.org.au/wp-content/uploads/2019/12/What_is_Digital_Health.pdf (accessed on 5 April 2023).
- Fatehi, F.; Samadbeik, M.; Kazemi, A. What is digital health? Review of definitions. Stud. Health Technol. Inform. 2020, 275, 67–71. [Google Scholar]
- Dorning, H. Consensus on Quality. 2015. Available online: https://www.nuffieldtrust.org.uk/qualitywatch/consensus-on-quality-full-report (accessed on 5 April 2023).
- Ibrahim, M.; Yusoff, H.; Bakar, Y.; Aung, M.; Abas, M.; Ramli, R. Digital health for quality health care: A systematic mapping of review studies. Digit. Health 2022, 8, 20552076221085810. [Google Scholar] [PubMed]
- Zhao, J.; Gao, S.; Wang, J.; Liu, X.; Hao, Y. Differentiation between two health care concepts: Person-centered and patient-centered care. Int. J. Nurs. Sci. 2016, 3, 398–402. [Google Scholar]
- American Geriatrics Society Expert Panel on Person-Centered Care. Person-centered care: A definition and essential elements. J. Am. Geriatr. Soc. 2016, 64, 15–18. [Google Scholar] [CrossRef]
- McCormack, B.; Dewing, T.; McCance, T. Developing person-centred Care: Addressing contextual challenges through practice development. Online J. Issues Nurs. 2011, 16, 3. [Google Scholar] [CrossRef] [PubMed]
- New England Journal of Medicine Group. What Is Patient-Centred Care? NEJM Catal. 1 January 2017. Available online: https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0559 (accessed on 5 April 2023).
- Miles, A.; Asbridge, J. Clarifying the concepts, epistemology and lixicon of person-centredness: An essential pre-requisite for the effecitve operationalization of PCH within modern health care systems. Eur. J. Pers. Cent. Healthc. 2014, 2, 1–15. [Google Scholar]
- Miles, A.; Asbridge, J. The chronic illness problem. The person-centered solution. Europ J. Pers. Cent. Healthc. 2016, 4, 1–5. [Google Scholar] [CrossRef]
- Godinho, M.; Jonnagaddala, J.; Gudi, N. M-health for integrated people-centred health services in the western pacific: A systematic review. Int. J. Med. Inform. 2020, 142, 104259. [Google Scholar] [CrossRef]
- World Health Organization. Framework on Integrated, People-Centred Health Services; World Health Organization: Geneva, Switzerland, 2016. Available online: https://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_39-en.pdf (accessed on 5 April 2023).
- Ekman, I.; Swedberg, K.; Taft, C.; Lindseth, A.; Norberg, A.; Brink, E. Person-centred care-ready for prime time. Eur. J. Cardiovasc. Nurs. 2011, 10, 248–251. [Google Scholar] [CrossRef]
- Helgesen, A.; Fagerli, L.; Grøndahl, V. Health care staff’s experiences of implementing one to one contact in nursing homes. Nurs. Ethics 2020, 27, 505–513. [Google Scholar] [CrossRef]
- Polin, K.; Hjartoland, M.; Maresso, A.; van Ginneken, E.; Busse, R.; Quentin, W. “Top-three” health reforms in 31 high-income countries in 2018 and 2019: An expert informed overview. Health Policy 2021, 125, 815–832. [Google Scholar] [CrossRef]
- Carter, R.; Riverin, B.; Levesque, J.F.; Gariepy, G.; Quesnel-Vallée, A. The impact of primary care reform on health system performance in Canada: A systematic review. BMC Health Serv. Res. 2016, 16, 324. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Technical Series on Primary Health Care. Digital Technologies: Shaping the Future of Primary Health Care. 2018. Available online: https://apps.who.int/iris/handle/10665/326573 (accessed on 5 April 2023).
- Allvin, R.; Bisholt, B.; Blomberg, K.; Bååth, C.; Wangensteen, S. Self-assessed competence and need for further training among registered nurses in somatic hospitals in Sweden: A cross-sectional survey. BMC Nurs. 2020, 19, 74. [Google Scholar] [CrossRef] [PubMed]
- Lundgren, A.; Vestergård, L.; Bogason, A.; Jokinen, J.; Penje, O.; Wang, S. Digital Health Care and Social Care-Regional Development Impacts in the Nordic Countries; Stockholm, Sweden. 2020. Available online: https://nordregio.org/publications/digital-health-care-and-social-care-regional-development-impacts-in-the-nordic-countries/ (accessed on 5 April 2023).
- Neves, A.; Burgers, J. Digital technologies in primary care: Implications for patient care and future research. Eur. J. Gen. Pract. 2022, 28, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Method. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 20, 69. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467. [Google Scholar] [CrossRef]
- Mourad, O.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar]
- Cambridge Dictionary. Middle Age. 2022. Available online: https://dictionary.cambridge.org/dictionary/english/middle-aged (accessed on 5 April 2023).
- Munn, Z.; Peters, M.; Stern, C.; Tutanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Peters, M.; Godfrey, C.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C. Guidance for conducting systematic scoping reviews. Int. J. Evid. Based Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef]
- Bekelman, D.B.; Plomondon, M.E.; Carey, E.P.; Sullivan, M.D.; Nelson, K.M.; Hattler, B.; McBryde, C.F.; Lehmann, K.G.; Gianola, K.; Heidenreich, P.A.; et al. Primary Results of the Patient-Centered Disease Management (PCDM) for Heart Failure Study: A Randomized Clinical Trial. JAMA Intern. Med. 2015, 175, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, J.S.; Wünsche, B.; Lutteroth, C. Designing and evaluating a patient-centred health management system for seniors. J. Telemed. Telecare 2016, 22, 96–104. [Google Scholar] [CrossRef] [PubMed]
- DiCarlo, L.A.; Weinstein, R.L.; Morimoto, C.B.; Savage, G.M.; Moon, G.L.; Au-Yeung, K. Patient-Centered Home Care Using Digital Medicine and Telemetric Data for Hypertension: Feasibility and Acceptability of Objective Ambulatory Assessment. J. Clin. Hypertens. 2016, 18, 901–906. [Google Scholar] [CrossRef] [PubMed]
- Innominato, P.; Komarzynski, S.; Karaboué, A.; Ulusakarya, A.; Bouchahda, M.; Haydar, M. Home-Based e-Health Platform for Multidimensional Telemonitoring of Symptoms, Body Weight, Sleep, and Circadian Activity: Relevance for Chronomodulated Administration of Irinotecan, Fluorouracil-Leucovorin, and Oxaliplatin at Home-Results From a Pilot Study. JCO Clin. Cancer Inform. 2018, 2, 1–15. [Google Scholar]
- Kim, H.; Tietsort, C.; Posteher, K.; Michaelides, A.; Toro-Ramos, T. Enabling self-management of a chronic condition through patient-centered coaching: A case of an m-health diabetes prevention program for older adults. Health Commun. 2020, 35, 1791–1799. [Google Scholar] [CrossRef]
- Radhakrishnan, K.; Xie, B.; Jacelon, C.S. Unsustainable Home Telehealth: A Texas Qualitative Study. Gerontologist 2016, 56, 830–840. [Google Scholar] [CrossRef]
- Ali, L.; Wallström, S.; Fors, A.; Barenfeld, E.; Fredholm, E.; Fu, M. Effects of Person-Centered Care Using a Digital Platform and Structured Telephone Support for People With Chronic Obstructive Pulmonary Disease and Chronic Heart Failure: Randomized Controlled Trial. J. Med. Internet Res. 2021, 23, e26794. [Google Scholar] [CrossRef]
- Barenfeld, E.; Ali, L.; Wallström, S.; Fors, A.; Ekman, I. Becoming more of an insider: A grounded theory study on patients’ experience of a person-centred e-health intervention. PLoS ONE 2020, 15, e0241801. [Google Scholar] [CrossRef]
- der Cingel, M.V.; Bulle-Smid, L.; Holterman, S.; Prins, H.; Keuning, W.; Hettinga, M. From clinical reasoning to ehealth interventions; a study on how nurses asses care and ehealth in home care. Nurse Educ. Pract. 2021, 50, 102925. [Google Scholar] [CrossRef]
- Jóhannsdóttir, T.B.; Ingadottir, B.; Svavarsdóttir, M.H. Rural patients’ experience of education, surveillance, and self-care support after heart disease related hospitalisation: A qualitative study. Int. J. Circumpolar Health 2021, 80, 2007667. [Google Scholar] [CrossRef]
- Smaradottir, B.F.; Berntsen, G.K.R.; Fensli, R.W. How to Enhance Digital Support for Cross-Organisational Health Care Teams? A User-Based Explorative Study. J. Healthc. Eng. 2020, 2020, 8824882. [Google Scholar] [CrossRef] [PubMed]
- Klein, J.; Hjeltnes, B.; Tunsjø, H.; Charnock, C. Can the use of assistive technology and interactive therapeutic robots in nursing homes contribute to the spread of infectious disease? Can. J. Infect. Control 2017, 32, 225–229. [Google Scholar]
- Radhakrishnan, K.; Toprac, P.; Matt, O.H.; Randolph, B.I.A.S.; Mackert, M.; Bo, X.I.E.; Miyong, K.I.M.; Bradley, P. Perceptions of Older Adults with Heart Failure on Playing an Interactive Digital e-Health Game (IDEG) for Learning About Heart Failure (HF): Prototype Development and Usability Testing. Stud. Health Technol. Inform. 2016, 225, 1026–1027. [Google Scholar]
- Klein, D.M.; Pham, K.; Samy, L.; Bluth, A.; Nazi, K.M.; Witry, M.; Klutts, J.S.; Grant, K.M.; Gundlapalli, A.V.; Kochersberger, G.; et al. The Veteran-Initiated Electronic Care Coordination: A Multisite Initiative to Promote and Evaluate Consumer-Mediated Health Information Exchange. Telemed. e-Health 2017, 23, 264–272. [Google Scholar] [CrossRef]
- World Health Organization. How to Strengthen Patientcentredness in Caring for People with Multimorbidity in Europe? 2016. Available online: https://www.euro.who.int/__data/assets/pdf_file/0008/337571/PB_22.pdf (accessed on 5 April 2023).
- Henni, S.; Maurud, S.; Fuglerud, K. The experiences, needs and barriers of people with impariments related to usability and accessibility of digital health solutions, levels of involvement in the design process and strategies for participatory and universal design: A scoping review. BMC Public Health 2022, 22, 35. [Google Scholar] [CrossRef] [PubMed]
- Leonardsen, A.; Hardeland, C.; Helgesen, A.; Grøndahl, V. Patient experiences with technology enabled care across health care settings—A systematic review. BMC Health Serv. Res. 2020, 24, 779. [Google Scholar]
- Pulvirenti, M.; McMillan, J.; Lawn, S. Empowerment, patient centred care and self-management. Health Expect. 2014, 17, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Hickmann, E.; Richter, P.; Schlieter, H. All together now- patient engagement, patient empowerment, and associated terms in personal health care. BMC Health Serv. Res. 2022, 22, 1116. [Google Scholar] [CrossRef]
- Leonardsen, A.; Helgesen, A.; Stensvold, A.; Magnussen, J.; Grøndahl, V. Cancer patients’ perspectives on remote monitoring at home during the COVID-19 pandemic- a qualitative study in Norway. BMC Health Serv. Res. 2022, 6, 453. [Google Scholar] [CrossRef]
- Stoumpos, A.; Kitsios, F.; Talias, M. Digital transformation in health care: Technology acceptance and its applications. Int. J. Environ. Res. Public Health 2023, 20, 3407. [Google Scholar] [CrossRef]
- Papavasiliou, S.; Reaiche, C.; Papavasiliou, S. Digital health and patient-centred care: A digital systems view. Syst. Res. Behav. Sci. 2020, 38, 231–245. [Google Scholar] [CrossRef]
- Odendaal, W.; Watkins, A.; Leon, J.; Goudge, N.; Griffiths, F.; Tomlinson, M. Health workers’ perceptions and experiences of using m-health technologies to deliver primary health care services: A qualitative evidence synthesis. Cochrane Database Syst. Rev. 2020, 3, CD011942. [Google Scholar] [CrossRef]
- World Health Organization. Digital Health. 2020. Available online: https://www.who.int/health-topics/digital-health (accessed on 5 April 2023).
- Jarva, E.; Oikarinen, A.; Andersson, J.; Tuomikoski, A.; Kääriäinen, M.; Meriläinen, M. Health care professionals’ perceptions of digital health competence: A qualitative descriptive study. Nurs. Open 2022, 9, 1379–1393. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.; Hossain, M.; Chou, W. Digital interventions to facilitate patient-provider communication in cancer care: A systematic review. Psycho-Oncol. 2019, 29, 591–603. [Google Scholar] [CrossRef] [PubMed]
- Byrne, N.; Baldwin, A.; Harvey, C. Whose centre is it anyway? Defining person-centred care in nursing: An integrative review. PLoS ONE 2020, 15, e0229923. [Google Scholar] [CrossRef]
- Glock, H.; Milos Nymberg, V.; Borgström Bolmsjö, B.; Holm, J.; Calling, S.; Pikkemaat, M. Attitudes, barriers and concerns regarding telemedicine among swedish primary care physicians: A qualitative study. Int. J. Gen. Med. 2021, 14, 9237–9246. [Google Scholar] [CrossRef]
- O’Connor, S.; Hanlon, P.; O’Donnell, C. Understanding factors affecting patient and public engagement and recruitment to digital health interventions: A systematic review of qualitative studies. BMC Med. Inform. Decis. Mak. 2016, 16, 120. [Google Scholar] [CrossRef]
| Search Words. | |
|---|---|
| Primary health care OR Community health care AND Digital OR Digit * OR Digital Health OR E-health OR Technology enabled care OR Telecare OR Telemedicine OR Telehealth OR Computer-based technologies | Patient-centeredness OR Patient-centeredness OR Patient-cent * OR Patient cent * OR Person-centeredness OR Person-centeredness OR Person-cent * OR Person cent * |
| Columns 1 and 2 combined with AND. | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leonardsen, A.-C.L.; Bååth, C.; Helgesen, A.K.; Grøndahl, V.A.; Hardeland, C. Person-Centeredness in Digital Primary Healthcare Services—A Scoping Review. Healthcare 2023, 11, 1296. https://doi.org/10.3390/healthcare11091296
Leonardsen A-CL, Bååth C, Helgesen AK, Grøndahl VA, Hardeland C. Person-Centeredness in Digital Primary Healthcare Services—A Scoping Review. Healthcare. 2023; 11(9):1296. https://doi.org/10.3390/healthcare11091296
Chicago/Turabian StyleLeonardsen, Ann-Chatrin Linqvist, Carina Bååth, Ann Karin Helgesen, Vigdis Abrahamsen Grøndahl, and Camilla Hardeland. 2023. "Person-Centeredness in Digital Primary Healthcare Services—A Scoping Review" Healthcare 11, no. 9: 1296. https://doi.org/10.3390/healthcare11091296
APA StyleLeonardsen, A.-C. L., Bååth, C., Helgesen, A. K., Grøndahl, V. A., & Hardeland, C. (2023). Person-Centeredness in Digital Primary Healthcare Services—A Scoping Review. Healthcare, 11(9), 1296. https://doi.org/10.3390/healthcare11091296






