Analysis of Differences in User Groups and Post Sentiment of COVID-19 Vaccine Hesitators in Chinese Social-Media Platforms
Abstract
1. Introduction
2. Literature Review
2.1. Vaccine Hesitancy
2.2. User Groups
2.3. Sentiment Analysis
3. Methods
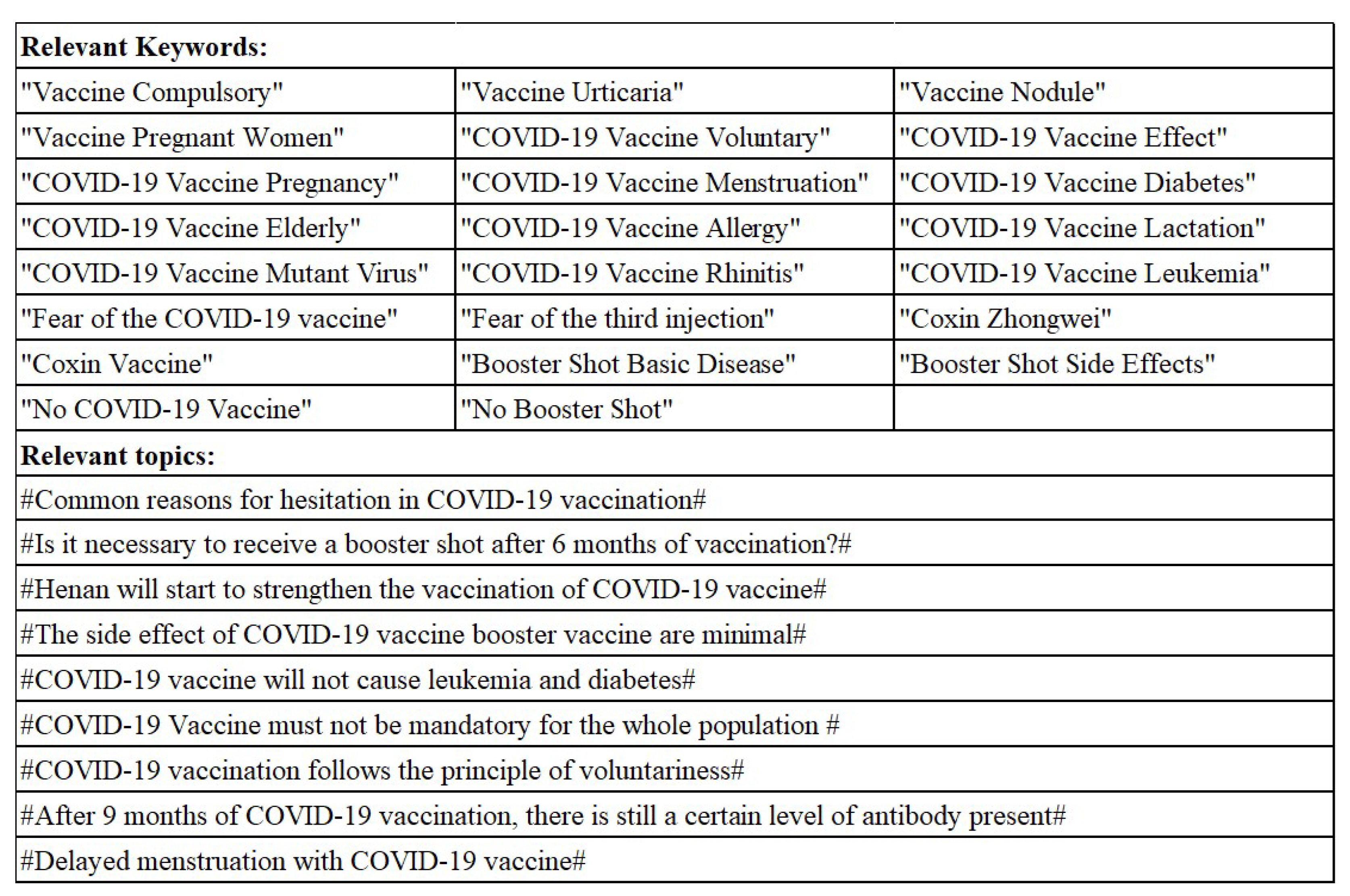
3.1. Data Collection
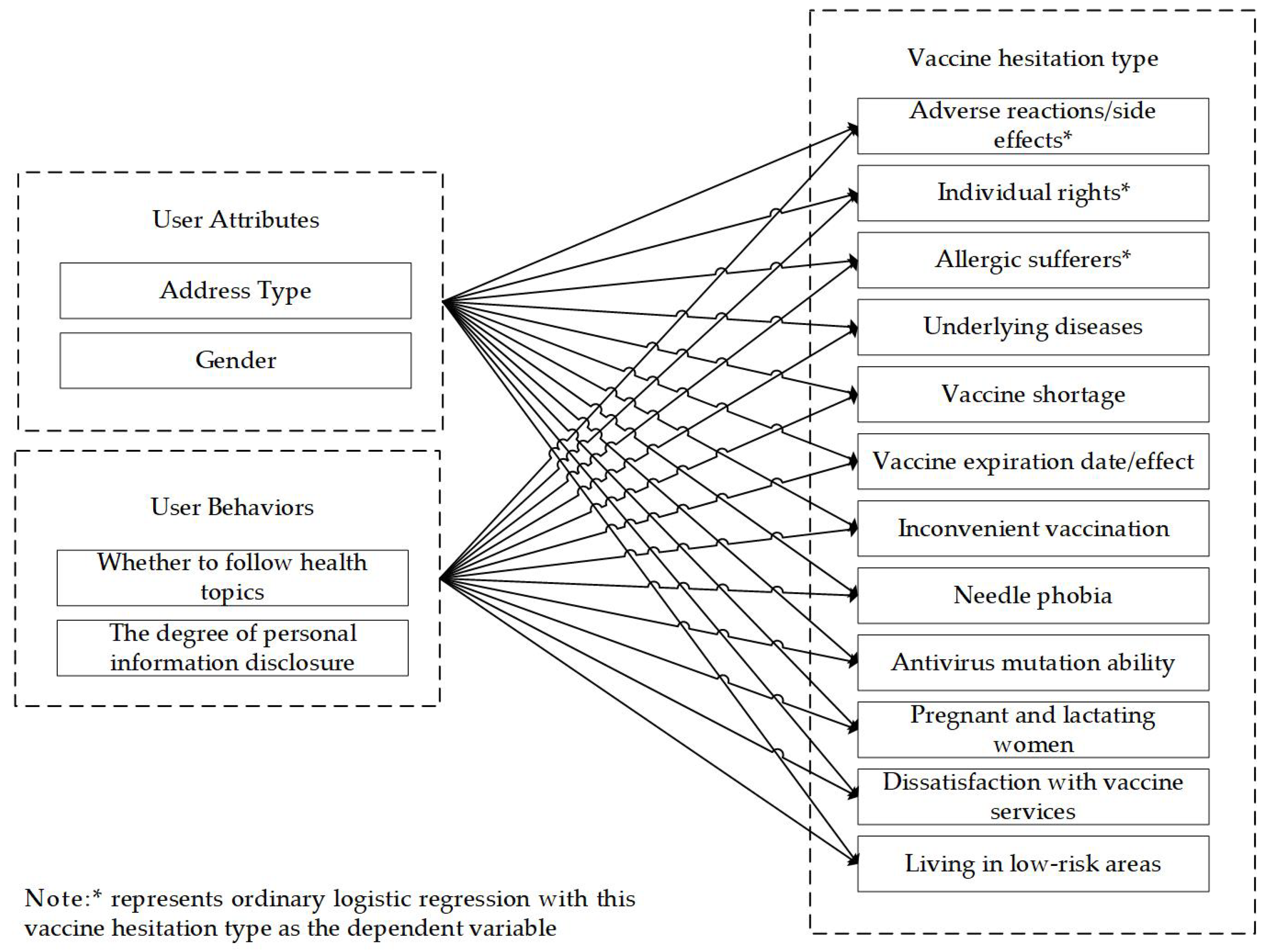
3.2. User-Groups Analysis
3.3. Text Sentiment Analysis
4. Results
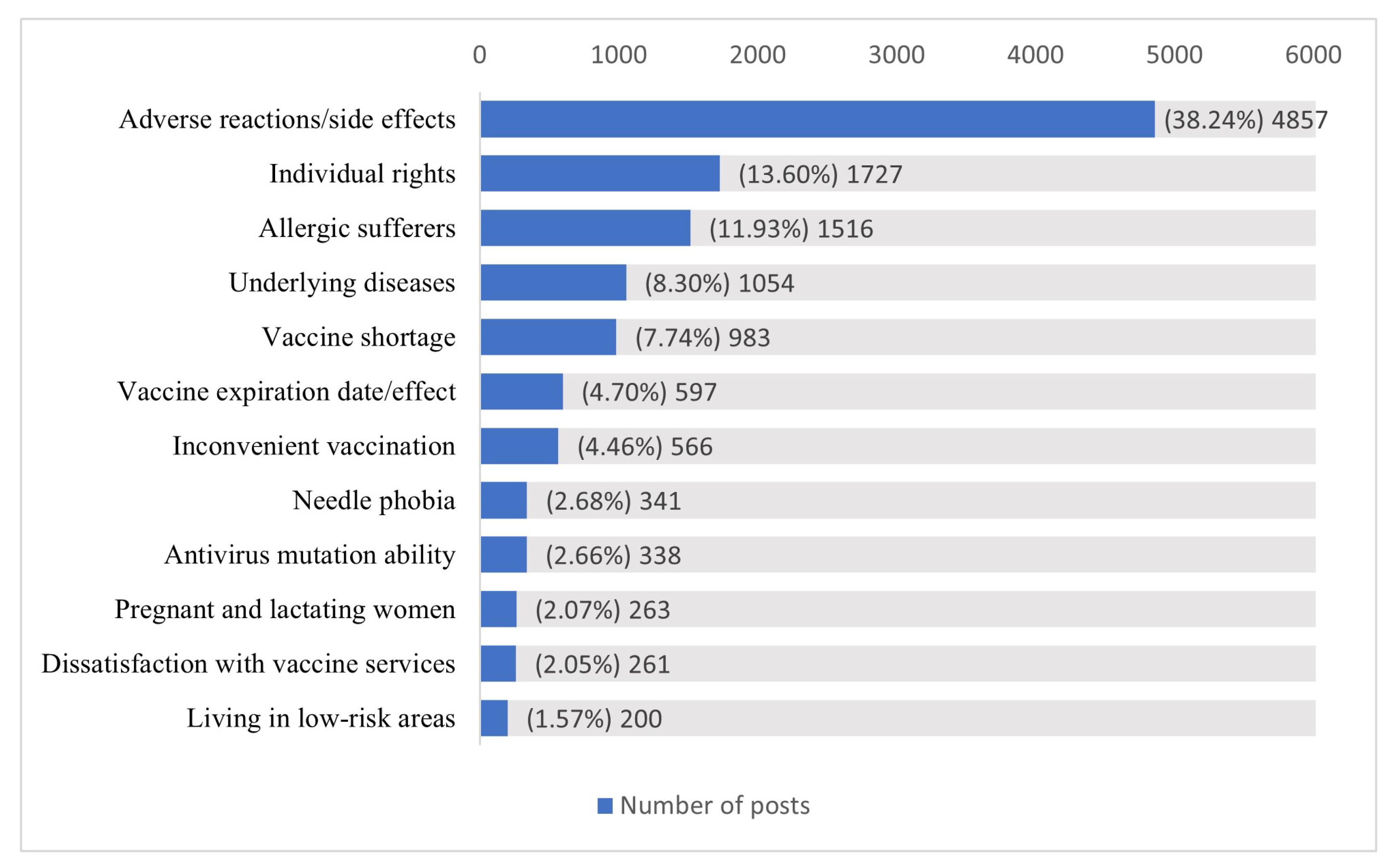
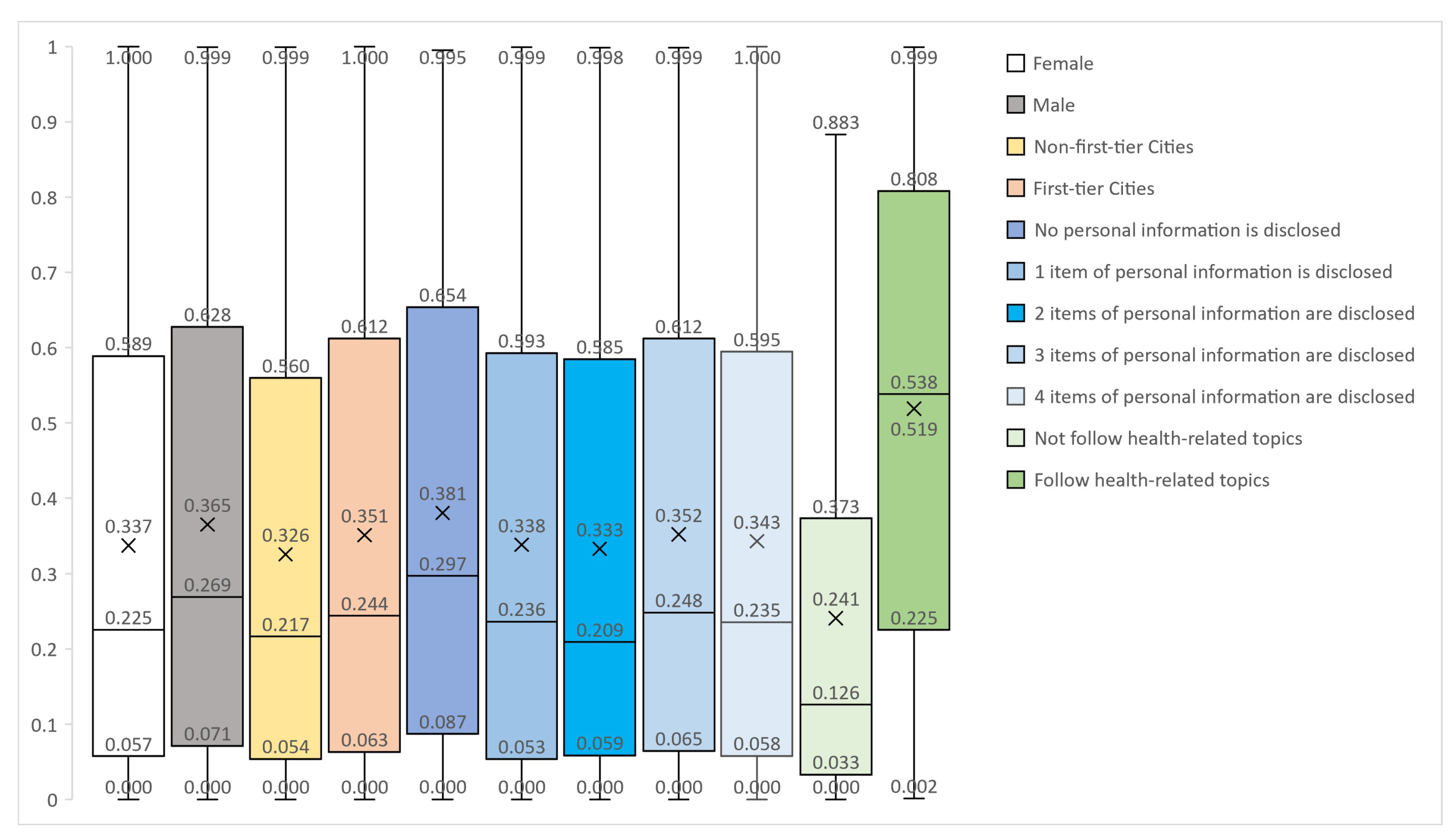
4.1. User-Groups Analysis Results
4.1.1. Differential Analysis of User Gender
4.1.2. Differential Analysis of User Address Types
4.1.3. Differential Analysis of the Degree of Personal-Information Disclosure
4.1.4. Differential Analysis of Whether to Follow Health Topics
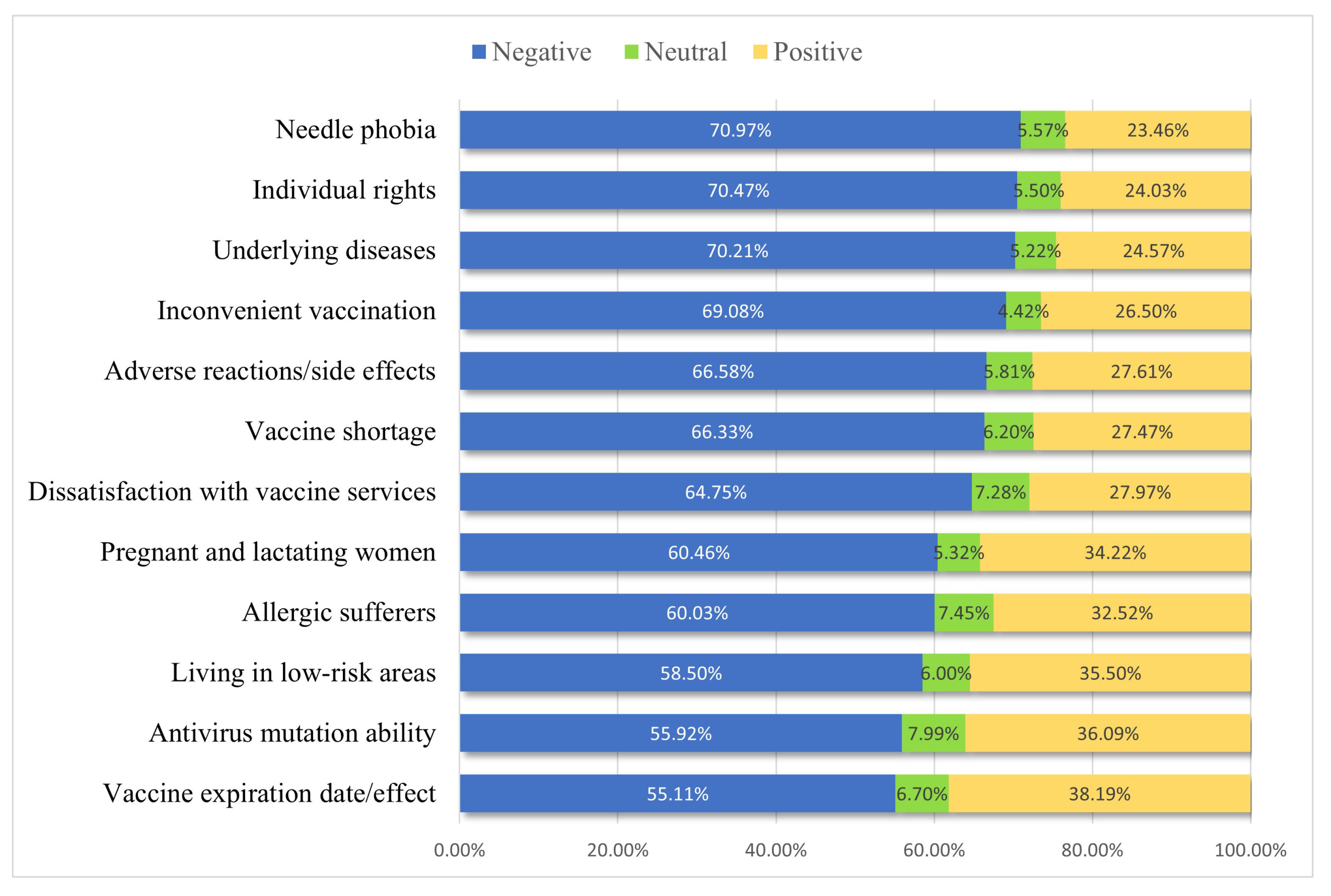
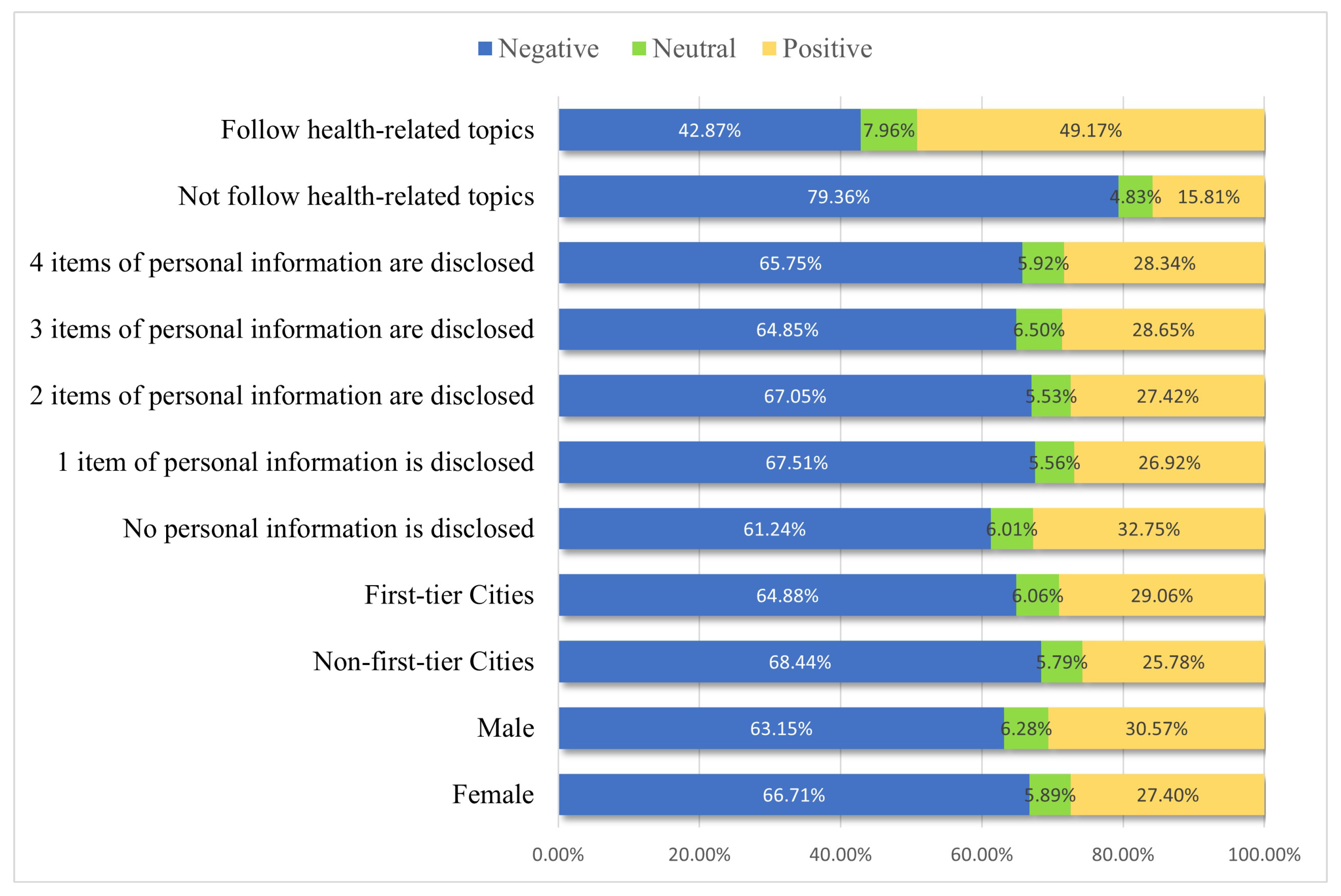
4.2. Text Sentiment-Analysis Results
5. Disscusson
6. Conclusions
6.1. Academic Contribution
6.2. Practical Significance
6.3. Limitation and Future Work
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- A Comprehensive Review of COVID-19 Characteristics|Biological Procedures Online|Full Text. Available online: https://biologicalproceduresonline.biomedcentral.com/articles/10.1186/s12575-020-00128-2 (accessed on 10 January 2023).
- Coronavirus Disease (COVID-19). Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 11 January 2023).
- Stasi, C.; Fallani, S.; Voller, F.; Silvestri, C. Treatment for COVID-19: An Overview. Eur. J. Pharmacol. 2020, 889, 173644. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.T.; Luo, Y.L.; Xia, S.C.; Sun, Q.F.; Ding, J.G.; Zhou, Y.; Chen, W.; Wang, X.F.; Zhang, W.W.; Du, W.J.; et al. Clinical Efficacy of Lopinavir/Ritonavir in the Treatment of Coronavirus Disease 2019. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 3390–3396. [Google Scholar] [PubMed]
- Capalbo, C.; Aceti, A.; Simmaco, M.; Bonfini, R.; Rocco, M.; Ricci, A.; Napoli, C.; Rocco, M.; Alfonsi, V.; Teggi, A.; et al. The Exponential Phase of the Covid-19 Pandemic in Central Italy: An Integrated Care Pathway. Int. J. Environ. Res. Public Health 2020, 17, 3792. [Google Scholar] [CrossRef] [PubMed]
- Haji Abdolvahab, M.; Moradi-Kalbolandi, S.; Zarei, M.; Bose, D.; Majidzadeh-A, K.; Farahmand, L. Potential Role of Interferons in Treating COVID-19 Patients. Int. Immunopharmacol. 2021, 90, 107171. [Google Scholar] [CrossRef]
- Yan, Z.; Yang, M.; Lai, C.-L. Long COVID-19 Syndrome: A Comprehensive Review of Its Effect on Various Organ Systems and Recommendation on Rehabilitation Plans. Biomedicines 2021, 9, 966. [Google Scholar] [CrossRef]
- Ruggiero, V.; Aquino, R.P.; Del Gaudio, P.; Campiglia, P.; Russo, P. Post-COVID Syndrome: The Research Progress in the Treatment of Pulmonary Sequelae after COVID-19 Infection. Pharmaceutics 2022, 14, 1135. [Google Scholar] [CrossRef]
- Long COVID or Post COVID-19 Syndrome. Mult. Scler. Relat. Disord. 2021, 55, 103268. [CrossRef]
- Haeusermann, T.; Romero-Kornblum, H.; Dzeng, E. Of Care, Cure and the in-between: COVID-19 Treatment in a New York City Intensive Care Unit. Int. J. Care Caring 2022, 6, 67–84. [Google Scholar] [CrossRef]
- Cazzola, M.; de Novellis, V.; Bianco, A.; Rogliani, P.; Matera, M.G. Disputes over the Production and Dissemination of Misinformation in the Time of COVID-19. Respir. Med. 2021, 182, 106380. [Google Scholar] [CrossRef]
- Derosa, G.; Maffioli, P.; D’Angelo, A.; Di Pierro, F. Nutraceutical Approach to Preventing Coronavirus Disease 2019 and Related Complications. Front. Immunol. 2021, 12, 582556. [Google Scholar] [CrossRef]
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J.A. Vaccine Hesitancy: An Overview. Hum. Vaccines Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Zhong, X.; Fu, H.; He, M.; Hu, R. COVID-19 Vaccine Hesitancy and GAD: The Role of Risk Perception and Vaccination Status. Front. Public Health 2022, 10, 994330. [Google Scholar] [CrossRef]
- Feikin, D.R.; Higdon, M.M.; Abu-Raddad, L.J.; Andrews, N.; Araos, R.; Goldberg, Y.; Groome, M.J.; Huppert, A.; O’Brien, K.L.; Smith, P.G.; et al. Duration of Effectiveness of Vaccines against SARS-CoV-2 Infection and COVID-19 Disease: Results of a Systematic Review and Meta-Regression. Lancet 2022, 399, 924–944. [Google Scholar] [CrossRef]
- COVID-19 Vaccines Advice. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines/advice (accessed on 11 January 2023).
- Emary, K.R.W.; Golubchik, T.; Aley, P.K.; Ariani, C.V.; Angus, B.; Bibi, S.; Blane, B.; Bonsall, D.; Cicconi, P.; Charlton, S.; et al. Efficacy of ChAdOx1 NCoV-19 (AZD1222) Vaccine against SARS-CoV-2 Variant of Concern 202012/01 (B.1.1.7): An Exploratory Analysis of a Randomised Controlled Trial. Lancet 2021, 397, 1351–1362. [Google Scholar] [CrossRef]
- Li, Z.; Ji, Y.; Sun, X. The Impact of Vaccine Hesitation on the Intentions to Get COVID-19 Vaccines: The Use of the Health Belief Model and the Theory of Planned Behavior Model. Front. Public Health 2022, 10, 882909. [Google Scholar] [CrossRef] [PubMed]
- Zeng, B.; Gao, L.; Zhou, Q.; Yu, K.; Sun, F. Effectiveness of COVID-19 Vaccines against SARS-CoV-2 Variants of Concern: A Systematic Review and Meta-Analysis. BMC Med. 2022, 20, 200. [Google Scholar] [CrossRef]
- Ma, C.; Sun, W.; Tang, T.; Jia, M.; Liu, Y.; Wan, Y.; Han, J.; Rodewald, L.; Li, J.; Song, Y.; et al. Effectiveness of Adenovirus Type 5 Vectored and Inactivated COVID-19 Vaccines against Symptomatic COVID-19, COVID-19 Pneumonia, and Severe COVID-19 Caused by the B.1.617.2 (Delta) Variant: Evidence from an Outbreak in Yunnan, China, 2021. Vaccine 2022, 40, 2869–2874. [Google Scholar] [CrossRef]
- COVID-19 Vaccines. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines (accessed on 9 January 2023).
- Schaffer DeRoo, S.; Pudalov, N.J.; Fu, L.Y. Planning for a COVID-19 Vaccination Program. JAMA 2020, 323, 2458–2459. [Google Scholar] [CrossRef]
- Chen, Y.-T. The Effect of Vaccination Rates on the Infection of COVID-19 under the Vaccination Rate below the Herd Immunity Threshold. Int. J. Environ. Res. Public Health 2021, 18, 7491. [Google Scholar] [CrossRef] [PubMed]
- Uzun, O.; Akpolat, T.; Varol, A.; Turan, S.; Bektas, S.G.; Cetinkaya, P.D.; Dursun, M.; Bakan, N.; Ketencioglu, B.B.; Bayrak, M.; et al. COVID-19: Vaccination vs. Hospitalization. Infection 2022, 50, 747–752. [Google Scholar] [CrossRef]
- Lin, X.-Q.; Zhang, M.-X.; Chen, Y.; Xue, J.-J.; Chen, H.-D.; Tung, T.-H.; Zhu, J.-S. Relationship between Knowledge, Attitudes, and Practices and COVID-19 Vaccine Hesitancy: A Cross-Sectional Study in Taizhou, China. Front. Med. 2022, 9, 770933. [Google Scholar] [CrossRef] [PubMed]
- Olagoke, A.A.; Olagoke, O.O.; Hughes, A.M. Intention to Vaccinate Against the Novel 2019 Coronavirus Disease: The Role of Health Locus of Control and Religiosity. J. Relig. Health 2021, 60, 65–80. [Google Scholar] [CrossRef] [PubMed]
- Seddig, D.; Maskileyson, D.; Davidov, E.; Ajzen, I.; Schmidt, P. Correlates of COVID-19 Vaccination Intentions: Attitudes, Institutional Trust, Fear, Conspiracy Beliefs, and Vaccine Skepticism. Soc. Sci. Med. 2022, 302, 114981. [Google Scholar] [CrossRef]
- Wang, J.; Ji, Q.; Dong, S.; Zhao, S.; Li, X.; Zhu, Q.; Long, S.; Zhang, J.; Jin, H. Factors Influencing Vaccine Hesitancy in China: A Qualitative Study. Vaccines 2021, 9, 1291. [Google Scholar] [CrossRef] [PubMed]
- Feng, H.; Zhu, H.; Zhang, H.; Cao, L.; Li, L.; Wang, J.; Huang, Y.; Lai, X.; Lyu, Y.; Jing, R.; et al. Caregivers’ Intentions to COVID-19 Vaccination for Their Children in China: A Cross-Sectional Survey. Hum. Vaccine Immunother. 2021, 17, 4799–4805. [Google Scholar] [CrossRef]
- Sun, Y.; Chen, X.; Cao, M.; Xiang, T.; Zhang, J.; Wang, P.; Dai, H. Will Healthcare Workers Accept a COVID-19 Vaccine When It Becomes Available? A Cross-Sectional Study in China. Front. Public Health 2021, 9. [Google Scholar]
- Yang, R.; Penders, B.; Horstman, K. Addressing Vaccine Hesitancy in China: A Scoping Review of Chinese Scholarship. Vaccines 2020, 8, 2. [Google Scholar] [CrossRef]
- Shen, X.; Dong, H.; Feng, J.; Jiang, H.; Dowling, R.; Lu, Z.; Lv, C.; Gan, Y. Assessing the COVID-19 Vaccine Hesitancy in the Chinese Adults Using a Generalized Vaccine Hesitancy Survey Instrument. Hum. Vaccine Immunother. 2021, 17, 4005–4012. [Google Scholar] [CrossRef]
- Qin, C.; Yan, W.; Tao, L.; Liu, M.; Liu, J. The Association between Risk Perception and Hesitancy toward the Booster Dose of COVID-19 Vaccine among People Aged 60 Years and Older in China. Vaccines 2022, 10, 1112. [Google Scholar] [CrossRef]
- Liu, H.; Zhou, Z.; Tao, X.; Huang, L.; Zhu, E.; Yu, L.; Zhang, M. COVID-19 Vaccine Hesitancy among Chinese Residents under the Free Vaccination Policy. Rev. Assoc. Med. Bras. 2021, 67, 1317–1321. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Reticencia a La Vacunación: Un Desafío Creciente Para Los Programas de Inmunización. Available online: https://www.who.int (accessed on 8 January 2023).
- Zhu, J.; Weng, F.; Zhuang, M.; Lu, X.; Tan, X.; Lin, S.; Zhang, R. Revealing Public Opinion towards the COVID-19 Vaccine with Weibo Data in China: BertFDA-Based Model. Int. J. Environ. Res. Public Health 2022, 19, 13248. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhou, Y.; Zhang, W.; Evans, R.; Zhu, C. Concerns Expressed by Chinese Social Media Users During the COVID-19 Pandemic: Content Analysis of Sina Weibo Microblogging Data. J. Med. Internet Res. 2020, 22, e22152. [Google Scholar] [CrossRef]
- Larson, H.J.; Gakidou, E.; Murray, C.J.L. The Vaccine-Hesitant Moment. N. Engl. J. Med. 2022, 387, 58–65. [Google Scholar] [CrossRef]
- Peretti-Watel, P.; Larson, H.J.; Ward, J.K.; Schulz, W.S.; Verger, P. Vaccine Hesitancy: Clarifying a Theoretical Framework for an Ambiguous Notion. PLoS Curr. 2015, 7, 6844c80ff9f5b273f34c91f71b7fc289. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, M.J. Vaccine Hesitancy: Public Trust, Expertise, and the War on Science; University of Pittsburgh Press: Pittsburgh, PA, USA, 2021; ISBN 978-0-8229-4655-7. [Google Scholar]
- Razai, M.S.; Chaudhry, U.A.R.; Doerholt, K.; Bauld, L.; Majeed, A. COVID-19 Vaccination Hesitancy. BMJ 2021, 373, n1138. [Google Scholar] [CrossRef]
- Webb Hooper, M.; Nápoles, A.M.; Pérez-Stable, E.J. No Populations Left Behind: Vaccine Hesitancy and Equitable Diffusion of Effective COVID-19 Vaccines. J. Gen. Intern. Med. 2021, 36, 2130–2133. [Google Scholar] [CrossRef]
- Robertson, E.; Reeve, K.S.; Niedzwiedz, C.L.; Moore, J.; Blake, M.; Green, M.; Katikireddi, S.V.; Benzeval, M.J. Predictors of COVID-19 Vaccine Hesitancy in the UK Household Longitudinal Study. Brain Behav. Immun. 2021, 94, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Mask Usage, Social Distancing, Racial, and Gender Correlates of COVID-19 Vaccine Intentions among Adults in the US. PLoS ONE 2021, 16, e0246970. Available online: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0246970 (accessed on 2 March 2023).
- Yoda, T.; Katsuyama, H. Willingness to Receive COVID-19 Vaccination in Japan. Vaccines 2021, 9, 48. [Google Scholar] [CrossRef]
- Akbas Gunes, N. Parents’ Perspectives about Vaccine Hesitancies and Vaccine Rejection, in the West of Turkey. J. Pediatr. Nurs. 2020, 53, e186–e194. [Google Scholar] [CrossRef] [PubMed]
- Pl, R.; Ml, P.; Ml, K. Acceptability of a COVID-19 Vaccine among Adults in the United States: How Many People Would Get Vaccinated? Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef]
- Huang, C.-L.; Chen, J.-Y.; Lin, X.-Q.; Deng, J.-S.; Tung, T.-H.; Zhu, J.-S. Parents’ Willingness to Pay for Their Children’s COVID-19 Vaccine in Taiwan, China: A Cross-Sectional Study. Hum. Vaccines Immunother. 2023, 19, 2168936. [Google Scholar] [CrossRef]
- Shen, X.; Wu, X.; Deng, Z.; Liu, X.; Zhu, Y.; Huang, Y.; Deng, Y.; Tian, Q.; Gan, Y.; Gong, Y.; et al. Analysis on Vaccine Hesitation and Its Associated Factors among Parents of Preschool Children in Songgang Street, Shenzhen. Sci. Rep. 2022, 12, 9467. [Google Scholar] [CrossRef]
- Cooper, A. The Inmates Are Running the Asylum. In Software-Ergonomie ’99: Design von Informationswelten; Arend, U., Eberleh, E., Pitschke, K., Eds.; Berichte des German Chapter of the ACM; Vieweg+Teubner Verlag: Wiesbaden, Germany, 1999; p. 17. ISBN 978-3-322-99786-9. [Google Scholar]
- Brickey, J.; Walczak, S.; Burgess, T. Comparing Semi-Automated Clustering Methods for Persona Development. IEEE Trans. Softw. Eng. 2012, 38, 537–546. [Google Scholar] [CrossRef]
- User Profiles in Organizational Environments. Available online: https://schlr.cnki.net/en/Detail/index/journal (accessed on 12 December 2022).
- Quintana, R.M.; Haley, S.R.; Levick, A.; Holman, C.; Hayward, B.; Wojan, M. The Persona Party: Using Personas to Design for Learning at Scale. In Proceedings of the 2017 CHI Conference Extended Abstracts on Human Factors in Computing Systems; Association for Computing Machinery: New York, NY, USA, 2017; pp. 933–941. [Google Scholar]
- Tan, H.; Peng, S.; Liu, J.-X.; Zhu, C.-P.; Zhou, F. Generating Personas for Products on Social Media: A Mixed Method to Analyze Online Users. Int. J. Hum. Comput. Interact. 2022, 38, 1255–1266. [Google Scholar] [CrossRef]
- Xu, Y.; Lee, M.J. Identifying Personas in Online Shopping Communities. Multimodal Technol. Interact. 2020, 4, 19. [Google Scholar] [CrossRef]
- Mulder, S.; Yaar, Z. The User Is Always Right: A Practical Guide to Creating and Using Personas for the Web (VOICES); New Riders Publishing: Indianapolis, IN, USA, 2006; ISBN 978-0-321-43453-1. [Google Scholar]
- An, J.; Kwak, H.; Jung, S.; Salminen, J.; Jansen, B.J. Customer Segmentation Using Online Platforms: Isolating Behavioral and Demographic Segments for Persona Creation via Aggregated User Data. Soc. Netw. Anal. Min. 2018, 8, 54. [Google Scholar] [CrossRef]
- Almeshari, M.; Dowell, J.; Nyhan, J. Museum Mobile Guide Preferences of Different Visitor Personas. J. Comput. Cult. Herit. 2021, 14, 1–13. [Google Scholar] [CrossRef]
- Yoo, S.; Lee, K. A Data-Driven Approach to Identifying Music Listener Groups Based on Users’ Playrate Distributions of Listening Events. In Proceedings of the Adjunct Publication of the 25th Conference on User Modeling, Adaptation and Personalization; Association for Computing Machinery: New York, NY, USA, 2017; pp. 77–81. [Google Scholar]
- ten Klooster, I.; Wentzel, J.; Sieverink, F.; Linssen, G.; Wesselink, R.; van Gemert-Pijnen, L. Personas for Better Targeted EHealth Technologies: User-Centered Design Approach. JMIR Hum. Factors 2022, 9, e24172. [Google Scholar] [CrossRef]
- Haldane, V.; Koh, J.J.K.; Srivastava, A.; Teo, K.W.Q.; Tan, Y.G.; Cheng, R.X.; Yap, Y.C.; Ong, P.-S.; Dam, R.M.V.; Foo, J.M.; et al. User Preferences and Persona Design for an MHealth Intervention to Support Adherence to Cardiovascular Disease Medication in Singapore: A Multi-Method Study. JMIR mHealth uHealth 2019, 7, e10465. [Google Scholar] [CrossRef] [PubMed]
- Haupt, M.R.; Weiss, S.M.; Chiu, M.; Cuomo, R.; Chein, J.M.; Mackey, T. Psychological and Situational Profiles of Social Distance Compliance during COVID-19. J. Commun. Healthc. 2022, 15, 44–53. [Google Scholar] [CrossRef]
- Massey, P.M.; Chiang, S.C.; Rose, M.; Murray, R.M.; Rockett, M.; Togo, E.; Klassen, A.C.; Manganello, J.A.; Leader, A.E. Development of Personas to Communicate Narrative-Based Information About the HPV Vaccine on Twitter. Front. Digit. Health 2021, 3, 682639. [Google Scholar] [CrossRef] [PubMed]
- Yin, H.; Song, X.; Yang, S.; Li, J. Sentiment Analysis and Topic Modeling for COVID-19 Vaccine Discussions. World Wide Web 2022, 25, 1067–1083. [Google Scholar] [CrossRef]
- Mäntylä, M.V.; Graziotin, D.; Kuutila, M. The Evolution of Sentiment Analysis—A Review of Research Topics, Venues, and Top Cited Papers. Comput. Sci. Rev. 2018, 27, 16–32. [Google Scholar] [CrossRef]
- Tavoschi, L.; Quattrone, F.; D’Andrea, E.; Ducange, P.; Vabanesi, M.; Marcelloni, F.; Lopalco, P.L. Twitter as a Sentinel Tool to Monitor Public Opinion on Vaccination: An Opinion Mining Analysis from September 2016 to August 2017 in Italy. Hum. Vaccine Immunother. 2020, 16, 1062–1069. [Google Scholar] [CrossRef]
- Gao, H.; Guo, D.; Wu, J.; Zhao, Q.; Li, L. Changes of the Public Attitudes of China to Domestic COVID-19 Vaccination After the Vaccines Were Approved: A Semantic Network and Sentiment Analysis Based on Sina Weibo Texts. Front. Public Health 2021, 9, 723015. [Google Scholar] [CrossRef]
- Ding, J.; Wang, A.; Zhang, Q. Mining the Vaccination Willingness of China Using Social Media Data. Int. J. Med. Inform. 2023, 170, 104941. [Google Scholar] [CrossRef]
- Ansari, M.T.J.; Khan, N.A. Worldwide COVID-19 Vaccines Sentiment Analysis Through Twitter Content. Electron. J. Gen. Med. 2021, 18, em329. [Google Scholar] [CrossRef]
- Jang, H.; Rempel, E.; Roe, I.; Adu, P.; Carenini, G.; Janjua, N.Z. Tracking Public Attitudes Toward COVID-19 Vaccination on Tweets in Canada: Using Aspect-Based Sentiment Analysis. J. Med. Internet Res. 2022, 24, e35016. [Google Scholar] [CrossRef] [PubMed]
- Monselise, M.; Chang, C.-H.; Ferreira, G.; Yang, R.; Yang, C.C. Topics and Sentiments of Public Concerns Regarding COVID-19 Vaccines: Social Media Trend Analysis. J. Med. Internet Res. 2021, 23, e30765. [Google Scholar] [CrossRef]
- Yousef, M.; Dietrich, T.; Rundle-Thiele, S. Actions Speak Louder Than Words: Sentiment and Topic Analysis of COVID-19 Vaccination on Twitter and Vaccine Uptake. JMIR Form. Res. 2022, 6, e37775. [Google Scholar] [CrossRef]
- Rahmanti, A.R.; Chien, C.-H.; Nursetyo, A.A.; Husnayain, A.; Wiratama, B.S.; Fuad, A.; Yang, H.-C.; Li, Y.-C.J. Social Media Sentiment Analysis to Monitor the Performance of Vaccination Coverage during the Early Phase of the National COVID-19 Vaccine Rollout. Comput. Methods Programs Biomed. 2022, 221, 106838. [Google Scholar] [CrossRef]
- Sun, K.; Wang, H.; Zhang, J. The Impact Factors of Social Media Users’ Forwarding Behavior of COVID-19 Vaccine Topic: Based on Empirical Analysis of Chinese Weibo Users. Front. Public Health 2022, 10, 871722. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Wu, W.; Zhang, X.; Qiang, Y.; Liu, T.; Wu, L. A Short-Term Trend Prediction Model of Topic over Sina Weibo Dataset. J. Comb. Optim. 2014, 28, 613–625. [Google Scholar] [CrossRef]
- Song, T.; Huang, J.; Tan, Y.; Yu, Y. Using User- and Marketer-Generated Content for Box Office Revenue Prediction: Differences Between Microblogging and Third-Party Platforms. Inf. Syst. Res. 2019, 30, 191–203. [Google Scholar] [CrossRef]
- Shi, Z.; Rui, H.; Whinston, A.B. Content Sharing in a Social Broadcasting Environment: Evidence from Twitter. MIS Q. Manag. Inf. Syst. 2014, 38, 123–142. [Google Scholar] [CrossRef]
- Liu, J.; Lu, S.; Lu, C. Exploring and Monitoring the Reasons for Hesitation with COVID-19 Vaccine Based on Social-Platform Text and Classification Algorithms. Healthcare 2021, 9, 1353. [Google Scholar] [CrossRef]
- Umar, P.; Akiti, C.; Squicciarini, A.; Rajtmajer, S. Self-Disclosure on Twitter During the COVID-19 Pandemic: A Network Perspective. In Machine Learning and Knowledge Discovery in Databases. Applied Data Science Track; Dong, Y., Kourtellis, N., Hammer, B., Lozano, J.A., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 271–286. [Google Scholar]
- King, G.; Zeng, L. Logistic Regression in Rare Events Data. Political Analysis 2001, 9, 137–163. [Google Scholar] [CrossRef]
- Yang, X. A Simulation Study of Logistic Regression and RareEvents Logistic Regression Model. Master’s Thesis, Sichuan University, Chengdu, China, 2005. [Google Scholar]
- Salmerón, R.; García, C.B.; García, J. Variance Inflation Factor and Condition Number in Multiple Linear Regression. J. Stat. Comput. Simul. 2018, 88, 2365–2384. [Google Scholar] [CrossRef]
- García, C.B.; García, J.; López Martín, M.M.; Salmerón, R. Collinearity: Revisiting the Variance Inflation Factor in Ridge Regression. J. Appl. Stat. 2015, 42, 648–661. [Google Scholar] [CrossRef]
- Ahad, N.A.; Yahaya, S.S.S.; Yin, L.P. Robustness of S1 Statistic with Hodges-Lehmann for Skewed Distributions. AIP Conf. Proc. 2016, 1782, 050002. [Google Scholar] [CrossRef]
- Elliott, A.C.; Hynan, L.S. A SAS® Macro Implementation of a Multiple Comparison Post Hoc Test for a Kruskal–Wallis Analysis. Comput. Methods Programs Biomed. 2011, 102, 75–80. [Google Scholar] [CrossRef]
- Gefen, D.; Straub, D.W. Gender Differences in the Perception and Use of E-Mail: An Extension to the Technology Acceptance Model. MIS Q. 1997, 21, 389. [Google Scholar] [CrossRef]
- Cross, C.P.; Copping, L.T.; Campbell, A. Sex Differences in Impulsivity: A Meta-Analysis. Psychol. Bull. 2011, 137, 97–130. [Google Scholar] [CrossRef]
- Sl, K.; I, M.; En, F. Sex-Based Differences in Immune Function and Responses to Vaccination. Trans. R. Soc. Trop. Med. Hyg. 2015, 109, 9–15. [Google Scholar] [CrossRef]
- Heidari, S.; Palmer-Ross, A.; Goodman, T. A Systematic Review of the Sex and Gender Reporting in COVID-19 Clinical Trials. Vaccines 2021, 9, 1322. [Google Scholar] [CrossRef]
- McLenon, J.; Rogers, M.A.M. The Fear of Needles: A Systematic Review and Meta-Analysis. J. Adv. Nurs. 2019, 75, 30–42. [Google Scholar] [CrossRef]
- Skjefte, M.; Ngirbabul, M.; Akeju, O.; Escudero, D.; Hernandez-Diaz, S.; Wyszynski, D.F.; Wu, J.W. COVID-19 Vaccine Acceptance among Pregnant Women and Mothers of Young Children: Results of a Survey in 16 Countries. Eur. J. Epidemiol. 2021, 36, 197–211. [Google Scholar] [CrossRef]
- Huang, J.; Chan, S.C.; Ko, S.; Wang, H.H.X.; Yuan, J.; Xu, W.; Zheng, Z.-J.; Xue, H.; Zhang, L.; Jiang, J.Y.; et al. Factors Associated with Vaccination Intention against the COVID-19 Pandemic: A Global Population-Based Study. Vaccines 2022, 10, 1539. [Google Scholar] [CrossRef]
- Orenius, T.; LicPsych; Säilä, H.; Mikola, K.; Ristolainen, L. Fear of Injections and Needle Phobia Among Children and Adolescents: An Overview of Psychological, Behavioral, and Contextual Factors. SAGE Open Nurs. 2018, 4, 237796081875944. [Google Scholar] [CrossRef]
- Fu, W.; Sivajohan, B.; McClymont, E.; Albert, A.; Elwood, C.; Ogilvie, G.; Money, D. Systematic Review of the Safety, Immunogenicity, and Effectiveness of COVID-19 Vaccines in Pregnant and Lactating Individuals and Their Infants. Int. J. Gynaecol. Obstet. 2022, 156, 406–417. [Google Scholar] [CrossRef]
- Muyldermans, J.; De Weerdt, L.; De Brabandere, L.; Maertens, K.; Tommelein, E. The Effects of COVID-19 Vaccination on Lactating Women: A Systematic Review of the Literature. Front. Immunol. 2022, 13, 852928. [Google Scholar] [CrossRef] [PubMed]
- Escudero, C.; Prieto-Montaño, P.; Audicana, M.T. Adverse Reactions to Anti-Infective Vaccines: An Emerging Problem in the COVID-19 Era. Curr. Treat. Opt. Allergy 2022, 9, 250–272. [Google Scholar] [CrossRef] [PubMed]
- Schinas, G.; Polyzou, E.; Mitropetrou, F.; Pazionis, A.; Gogos, C.; Triantos, C.; Akinosoglou, K. COVID-19 Vaccination in Patients with Chronic Liver Disease. Viruses 2022, 14, 2778. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Du, J.; Li, Z.; Xu, Z.; Wu, Y.; Duan, W.; Wang, W.; Zhang, T.; Xu, J.; Wu, H.; et al. It Is Time to Improve the Acceptance of COVID-19 Vaccines among People with Chronic Diseases: A Systematic Review and Meta-Analysis. J. Med. Virol. 2023, 95, e28509. [Google Scholar] [CrossRef] [PubMed]
- Moyer-Gusé, E.; Robinson, M.J.; Mcknight, J. The Role of Humor in Messaging about the MMR Vaccine. J. Health Commun. 2018, 23, 514–522. [Google Scholar] [CrossRef]
- Zhou, Z.; Zhu, Y.; Chu, M. Role of COVID-19 Vaccines in SARS-CoV-2 Variants. Front. Immunol. 2022, 13, 898192. [Google Scholar] [CrossRef]
- China|RSF. Available online: https://rsf.org/en/country/china (accessed on 28 February 2023).


| No. | Variable Name | Variable Type | Measurement Standard |
|---|---|---|---|
| 1 | Gender | 0–1 variables | 0 means female (9200); 1 means male (3503) |
| 2 | Address Type | Multicategorical variables | 0 indicates non-first-tier cities (6028); 1 indicates first-tier cities (2667); 2 indicates overseas (881); 3 indicates not reported (3127) |
| 3 | The degree of personal information disclosure | Multi-categorical variables | 0 means no personal information disclosed (516); 1 means 1 personal information is disclosed (1457); 2 means 2 items of personal information are disclosed (2407); 3 means that 3 items of personal information are disclosed (4014); 4 means that 4 items of personal information are disclosed (4309) |
| 4 | Whether to follow Health Topics | 0–1 variables | 0 means the user does not follow health-related topics (7956); 1 means that the user follows health-related topics (4747) |
| No. | Variable Name | VIF |
|---|---|---|
| 1 | Gender | 1.01 |
| 2 | Address type | 1.43 |
| 3 | The degree of personal-information disclosure | 1.44 |
| 4 | Whether to follow health topics | 1.00 |
| Average VIF | 1.22 |
| Type | Statistics | Degrees of Freedom | Significance a |
|---|---|---|---|
| Vaccine shortage | 0.148 | 983 | <0.001 |
| Individual rights | 0.167 | 1727 | <0.001 |
| Inconvenient vaccination | 0.152 | 566 | <0.001 |
| Dissatisfaction with vaccine services | 0.148 | 261 | <0.001 |
| Vaccine expiration date/effect | 0.144 | 597 | <0.001 |
| Living in low-risk areas | 0.137 | 200 | <0.001 |
| Antivirus mutation ability | 0.107 | 338 | <0.001 |
| Underlying diseases | 0.149 | 1054 | <0.001 |
| Adverse reactions/side effects | 0.145 | 4857 | <0.001 |
| Pregnant and lactating women | 0.147 | 263 | <0.001 |
| Needle phobia | 0.153 | 341 | <0.001 |
| Allergic sufferers | 0.112 | 1516 | <0.001 |
| Type | Comparison Type | Significance | Results of Two-Way Comparison (Emotional Score) |
|---|---|---|---|
| Individual rights | Vaccine shortage | 0.013 | Individual rights < Underlying diseases < Inconvenient vaccination, Adverse reactions/side effects < Needle phobia < Adverse reactions/side effects, Living in low-risk areas, Antivirus mutation ability |
| Vaccine expiration date/effect | <0.001 | ||
| Living in low-risk areas | <0.001 | ||
| Antivirus mutation ability | <0.001 | ||
| Adverse reactions/side effects | 0.002 | ||
| Living in low-risk areas | <0.001 | ||
| Pregnant and lactating women | <0.001 | ||
| Allergic sufferers | <0.001 | ||
| Inconvenient vaccination | Vaccine expiration date/effect | 0.001 | |
| Living in low-risk areas | 0.02 | ||
| Antivirus mutation ability | <0.001 | ||
| Allergic sufferers | <0.001 | ||
| Underlying diseases | Vaccine expiration date/effect | <0.001 | |
| Living in low-risk areas | 0.003 | ||
| Antivirus mutation ability | <0.001 | ||
| Pregnant and lactating women | 0.011 | ||
| Allergic sufferers | <0.001 | ||
| Adverse reactions/side effects | Vaccine expiration date/effect | <0.001 | |
| Living in low-risk areas | 0.027 | ||
| Antivirus mutation ability | <0.001 | ||
| Allergic sufferers | <0.001 | ||
| Needle phobia | Vaccine expiration date/effect | 0.045 | |
| Antivirus mutation ability | 0.003 | ||
| Allergic sufferers | 0.046 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, J.; Lu, S.; Zheng, H. Analysis of Differences in User Groups and Post Sentiment of COVID-19 Vaccine Hesitators in Chinese Social-Media Platforms. Healthcare 2023, 11, 1207. https://doi.org/10.3390/healthcare11091207
Liu J, Lu S, Zheng H. Analysis of Differences in User Groups and Post Sentiment of COVID-19 Vaccine Hesitators in Chinese Social-Media Platforms. Healthcare. 2023; 11(9):1207. https://doi.org/10.3390/healthcare11091207
Chicago/Turabian StyleLiu, Jingfang, Shuangjinhua Lu, and Huiqin Zheng. 2023. "Analysis of Differences in User Groups and Post Sentiment of COVID-19 Vaccine Hesitators in Chinese Social-Media Platforms" Healthcare 11, no. 9: 1207. https://doi.org/10.3390/healthcare11091207
APA StyleLiu, J., Lu, S., & Zheng, H. (2023). Analysis of Differences in User Groups and Post Sentiment of COVID-19 Vaccine Hesitators in Chinese Social-Media Platforms. Healthcare, 11(9), 1207. https://doi.org/10.3390/healthcare11091207






