Translation, Cross-Cultural Adaptation and Psychometric Validation of the Arabic Version of the Cardiac Rehabilitation Barriers Scale (CRBS-A) with Strategies to Mitigate Barriers
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Materials: Cardiac Rehabilitation Barriers Scale and Barrier Mitigation Strategies
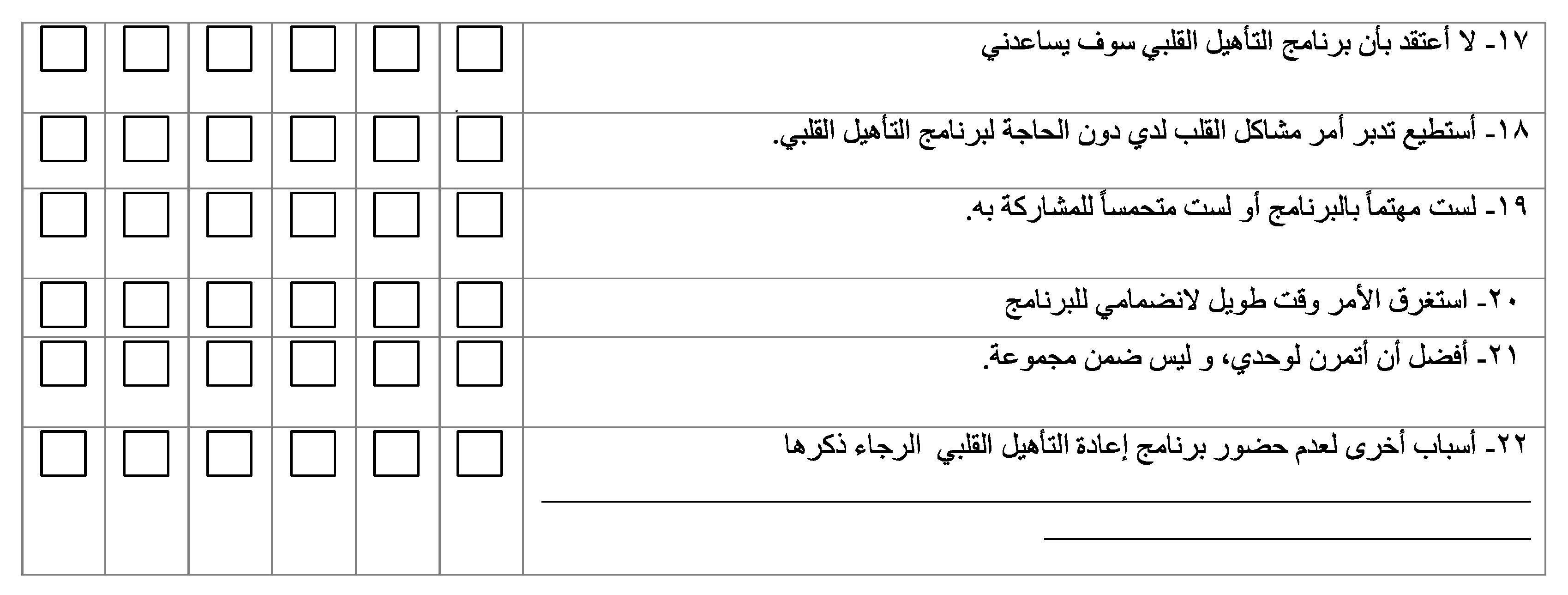
2.3. Phase 1: Multi-Step Process for Arabic Translation and Cultural Adaptation of CRBS and Associated Barrier Mitigation Strategies
2.4. Phase 2: Cross-Sectional Survey of Patients for Psychometric Validation
2.4.1. Procedure
2.4.2. Setting and Participants
2.4.3. Measures
2.5. Data Analysis
3. Results
3.1. Translation and Cultural Adaptation
3.2. Psychometric Validation
3.3. Main Barriers and Usefulness of Strategies to Mitigate These Barriers
4. Discussion
4.1. Implications
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Mitigation Responses for Each Barrier
- Distance
- 2.
- Cost
- 3.
- Transportation Problems
- 4.
- Family Responsibilities
- Ask extended family members to take over some of your family responsibilities for a short period.
- Some cardiac rehab programs welcome family members into the program. If your family member is an adult that can do some basic walking, they may be able to join in and reap the benefits as well. Ask your program.
- See if you can hire someone (e.g., teen neighbor, personal support worker, cleaning help) to take over some of your family responsibilities in the short term.
- Check with your primary care provider for available community services for caregiving in the home/respite.
- Ask your cardiac rehab program about home-based options. It may be possible for you to get your cardiac rehab through phone or video calls with your cardiac rehab team, after going for a few sessions to become oriented.
- 5.
- Not knowing about cardiac rehabilitation
- 6.
- I do not need cardiac rehab
- 7.
- Already exercising at home/community
- 8.
- Severe weather
- 9.
- Exercise is tiring and painful
- 10.
- Travel
- 11.
- Time constraints
- Talk to your cardiac rehab team about session time availability to find something that works for you.
- Some programs have home-based supports, so you exercise when you can at home or in your community but have regular contacts with the cardiac rehab staff to address all your heart risk factors and educate you about your heart health via phone or videocall at your convenience.
- Talk to your cardiac rehab program contact about what parts of the program are most important for you, and how you can fit it in.
- Most programs offer stress management, which includes a time management component. This can help you get a better hold of you
- Remember you do not need to do all your exercise at once; you can do 10 min here and there each day.
- See if family members or others can take some of your load while you are doing your cardiac rehab program. Your loved ones want to see you well and have you around for many more years to come.
- 12.
- Work responsibilities
- 13.
- Not having energy
- 14.
- Other health problems
- For patients with diabetes, the rehab team will teach you about eating timing in relation to exercise, help you to assess your blood sugar, and teach you about caring for your feet.
- For patients with arthritis, the rehab team can suggest non-weight-bearing exercise and work with you to achieve pain control.
- For patients with osteoporosis, your rehab team will assess you for your risk of a fall, and put extra safety measures in place where needed.
- 15.
- Too old
- 16.
- Doctor did not feel it was necessary
- 17.
- I do not think it will help me
- 18.
- Manage own heart problem
- 19.
- I am not interested or motivated
- 20.
- Too long to get referred into the program
- 21.
- Prefer to exercise alone
- 22.
- Here, are the other barriers of concern for you that you can discuss with your healthcare providers
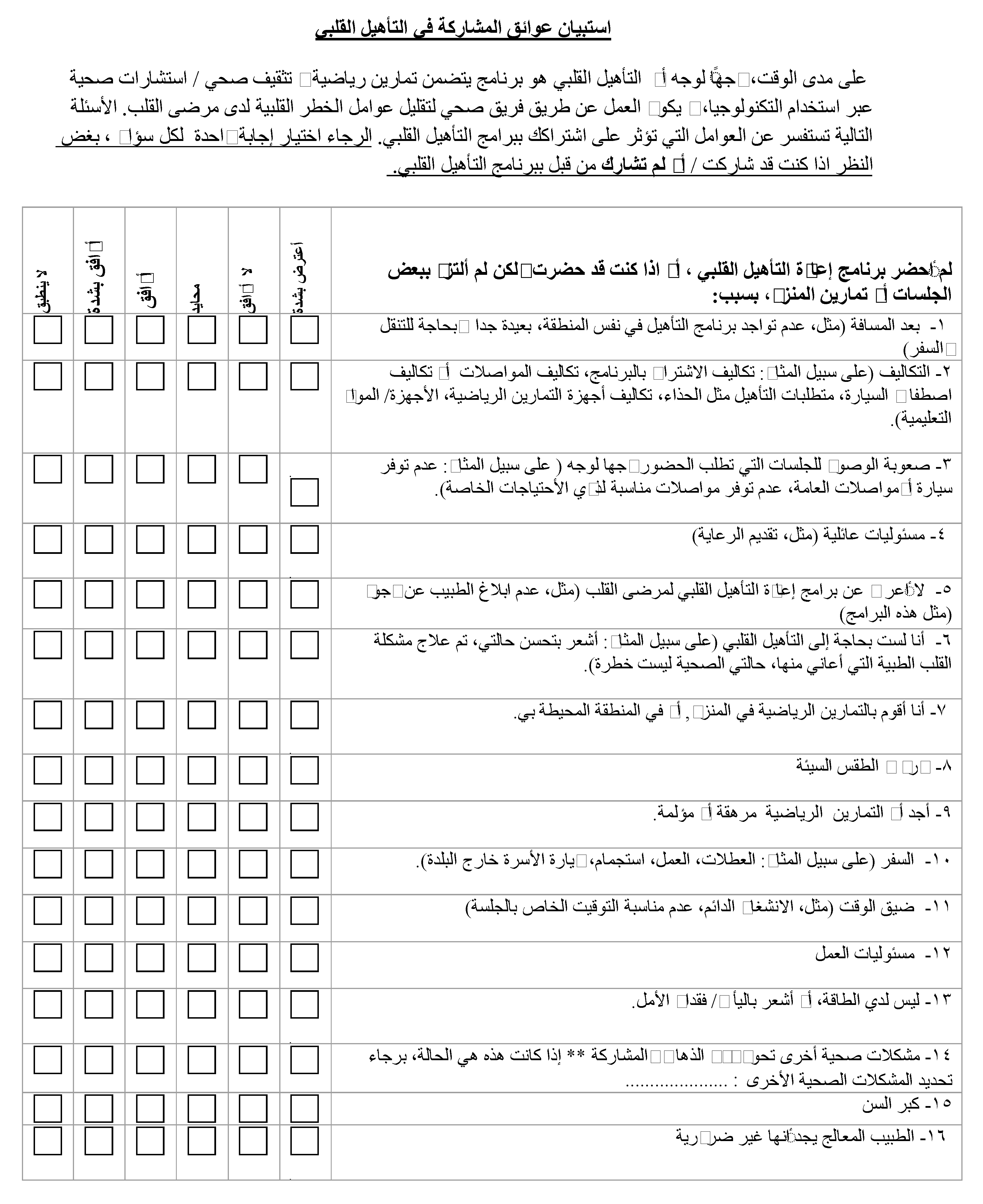
Appendix B. The CRBS-A
References
- Mensah, G.A.; Roth, G.A.; Fuster, V. The Global Burden of Cardiovascular Diseases and Risk Factors. J. Am. Coll Cardiol. 2019, 74, 2529–2532. [Google Scholar] [CrossRef]
- Turk-Adawi, K.; Sarrafzadegan, N.; Fadhil, I.; Taubert, K.; Sadeghi, M.; Wenger, N.K.; Tan, N.S.; Grace, S.L. Cardiovascular Disease in the Eastern Mediterranean Region: Epidemiology and Risk Factor Burden. Nat. Rev. Cardiol. 2018, 15, 106–119. [Google Scholar] [CrossRef] [PubMed]
- GBD 2015 Eastern Mediterranean Region Cardiovascular Disease Collaborators. Burden of Cardiovascular Diseases in the Eastern Mediterranean Region, 1990–2015: Findings from the Global Burden of Disease 2015 Study. Int. J. Public Health 2018, 63, 137–149. [Google Scholar] [CrossRef] [PubMed]
- Raal, F.J.; Alsheikh-Ali, A.A.; Omar, M.I.; Rashed, W.; Hamoui, O.; Kane, A.; Alami, M.; Abreu, P.; Mashhoud, W.M. Cardiovascular Risk Factor Burden in Africa and the Middle East across Country Income Categories: A Post Hoc Analysis of the Cross-Sectional Africa Middle East Cardiovascular Epidemiological (ACE) Study. Arch. Public Health 2018, 76, 15. [Google Scholar] [CrossRef]
- Dibben, G.; Faulkner, J.; Oldridge, N.; Rees, K.; Thompson, D.R.; Zwisler, A.-D.; Taylor, R.S. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease. Cochrane Database Syst. Rev. 2021, 2021, 14651858. [Google Scholar] [CrossRef]
- Mamataz, T.; Uddin, J.; Ibn Alam, S.; Taylor, R.S.; Pakosh, M.; Grace, S.L. Effects of Cardiac Rehabilitation in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Prog. Cardiovasc. Dis. 2022, 70, 119–174. [Google Scholar] [CrossRef]
- Ragupathi, L.; Stribling, J.; Yakunina, Y.; Fuster, V.; McLaughlin, M.A.; Vedanthan, R. Availability, Use, and Barriers to Cardiac Rehabilitation in LMIC. Glob. Heart 2017, 12, 323. [Google Scholar] [CrossRef]
- Turk-Adawi, K.; Supervia, M.; Pesah, E.; Lopez-Jimenez, F.; Afaneh, J.; El-Heneidy, A.; Sadeghi, M.; Sarrafzadegan, N.; Alhashemi, M.; Papasavvas, T.; et al. Availability and Delivery of Cardiac Rehabilitation in the Eastern Mediterranean Region: How Does It Compare Globally? Int. J. Cardiol. 2019, 285, 147–153. [Google Scholar] [CrossRef]
- Critchley, K.; Ali Al- Ashwal, N.; Benjamin, K. Cardiac Rehabilitation Programs: An Investigation into the Reasons for Non-Attendance in Qatar. IGHPE 2017, 2, 1–11. [Google Scholar] [CrossRef]
- Clark, A.M.; King-Shier, K.M.; Thompson, D.R.; Spaling, M.A.; Duncan, A.S.; Stone, J.A.; Jaglal, S.B.; Angus, J.E. A Qualitative Systematic Review of Influences on Attendance at Cardiac Rehabilitation Programs after Referral. Am. Heart J. 2012, 164, 835–845.e2. [Google Scholar] [CrossRef]
- Shanmugasegaram, S.; Gagliese, L.; Oh, P.; Stewart, D.E.; Brister, S.J.; Chan, V.; Grace, S.L. Psychometric Validation of the Cardiac Rehabilitation Barriers Scale. Clin. Rehabil. 2012, 26, 152–164. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.; Ghisi, G.L.M.; Davis, E.; Grace, S.L. Cardiac Rehabilitation Barriers Scale (CRBS). In International Handbook of Behavioral Health Assessment; Springer: New York, NY, USA, 2023. [Google Scholar]
- Ethnologue. Available online: https://www.ethnologue.com/ (accessed on 7 February 2023).
- Chindhy, S.; Taub, P.R.; Lavie, C.J.; Shen, J. Current Challenges in Cardiac Rehabilitation: Strategies to Overcome Social Factors and Attendance Barriers. Expert Rev. Cardiovasc. Ther. 2020, 18, 777–789. [Google Scholar] [CrossRef] [PubMed]
- Wild, D.; Grove, A.; Martin, M.; Eremenco, S.; McElroy, S.; Verjee-Lorenz, A.; Erikson, P. Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: Report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health 2005, 8, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Grace, S.L.; Kotseva, K.; Whooley, M.A. Cardiac Rehabilitation: Under-Utilized Globally. Curr. Cardiol. Rep. 2021, 23, 118. [Google Scholar] [CrossRef]
- Moghei, M.; Oh, P.; Chessex, C.; Grace, S.L. Cardiac Rehabilitation Quality Improvement: A Narrative Review. J. Cardiopulm. Rehabil. Prev. 2019, 39, 226–234. [Google Scholar] [CrossRef]
- Gallagher, R.; Ghisi, G.L.M.; Buckley, J.; Contractor, A.; Yeung, C.; Grace, S.L. Promotion and advocacy for secondary prevention of cardiovascular disease through cardiac rehabilitation: The ICCPR reach, activities and outcomes. IJNCD 2023, in press. [Google Scholar]
- Zamanzadeh, V.; Ghahramanian, A.; Rassouli, M.; Abbaszadeh, A.; Alavi-Majd, H.; Nikanfar, A.-R. Design and Implementation Content Validity Study: Development of an Instrument for Measuring Patient-Centered Communication. J. Caring Sci. 2015, 4, 165–178. [Google Scholar] [CrossRef]
- Santiago de Araújo Pio, C.; Beckie, T.M.; Varnfield, M.; Sarrafzadegan, N.; Babu, A.S.; Baidya, S.; Buckley, J.; Chen, S.-Y.; Gagliardi, A.; Heine, M.; et al. Promoting Patient Utilization of Outpatient Cardiac Rehabilitation: A joint International Council and Canadian Association of Cardiovascular Prevention and Rehabilitation position statement. J. Cardiopulm. Rehabil. Prev. 2020, 40, 79–86. [Google Scholar] [CrossRef]
- Nunnally, J.C. Pyschometric Theory; McGraw-Hill: New York, NY, USA, 1978. [Google Scholar]
- Daly, J.; Sindone, A.P.; Thompson, D.R.; Hancock, K.; Chang, E.; Davidson, P. Barriers to Participation in and Adherence to Cardiac Rehabilitation Programs: A Critical Literature Review. Prog. Cardiovasc. Nurs. 2002, 17, 8–17. [Google Scholar] [CrossRef]
- Ghanbari-Firoozabadi, M.; Mirzaei, M.; Vafaii Nasab, M.; Grace, S.L.; Okati-Aliabad, H.; Madadizadeh, F.; Dadras, H.; Amrolahi, N.; Entezari, M.; Sadrbafghi, S.M. Cross-Cultural Adaptation and Psychometric Validation of the Persian Version of the Cardiac Rehabilitation Barriers Scale (CRBS-P). BMJ Open 2020, 10, e034552. [Google Scholar] [CrossRef]
- Bakhshayeh, S.; Sarbaz, M.; Kimiafar, K.; Vakilian, F.; Eslami, S. Barriers to Participation in Center-Based Cardiac Rehabilitation Programs and Patients’ Attitude toward Home-Based Cardiac Rehabilitation Programs. Physiother. Theory Pract. 2021, 37, 158–168. [Google Scholar] [CrossRef]
- Turk-Adawi, K.; Supervia, M.; Lopez-Jimenez, F.; Pesah, E.; Ding, R.; Britto, R.R.; Bjarnason-Wehrens, B.; Derman, W.; Abreu, A.; Babu, A.S.; et al. Cardiac Rehabilitation Availability and Density around the Globe. EClinicalMedicine 2019, 13, 31–45. [Google Scholar] [CrossRef] [PubMed]
- Ghisi, G.L.d.M.; dos Santos, R.Z.; Schveitzer, V.; Barros, A.L.; Recchia, T.L.; Oh, P.; Benetti, M.; Grace, S.L. Desenvolvimento e Validação Da Versão Em Português Da Escala de Barreiras Para Reabilitação Cardíaca. Arq. Bras. Cardiol. 2012, 98, 344–352. [Google Scholar] [CrossRef]
- de Melo Ghisi, G.L.; dos Santos, R.Z.; Aranha, E.E.; Nunes, A.D.; Oh, P.; Benetti, M.; Grace, S.L. Perceptions of Barriers to Cardiac Rehabilitation Use in Brazil. Vasc. Health Risk Manag. 2013, 9, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Sérvio, T.C.; Britto, R.R.; de Melo Ghisi, G.L.; da Silva, L.P.; Silva, L.D.N.; Lima, M.M.O.; Pereira, D.A.G.; Grace, S.L. Barriers to Cardiac Rehabilitation Delivery in a Low-Resource Setting from the Perspective of Healthcare Administrators, Rehabilitation Providers, and Cardiac Patients. BMC Health Serv. Res. 2019, 19, 615. [Google Scholar] [CrossRef]
- da Cruz, M.M.A.; Ricci-Vitor, A.L.; Borges, G.L.B.; da Silva, P.F.; Turri-Silva, N.; Takahashi, C.; Grace, S.L.; Vanderlei, L.C.M. A Randomized, Controlled, Crossover Trial of Virtual Reality in Maintenance Cardiovascular Rehabilitation in a Low-Resource Setting: Impact on Adherence, Motivation, and Engagement. Phys. Ther. 2021, 101, pzab071. [Google Scholar] [CrossRef]
- Borges, G.L.B.; da Cruz, M.M.A.; Ricci-Vitor, A.L.; da Silva, P.F.; Grace, S.L.; Vanderlei, L.C.M. Publicly versus Privately Funded Cardiac Rehabilitation: Access and Adherence Barriers. A Cross-Sectional Study. Sao Paulo Med. J. 2022, 140, 108–114. [Google Scholar] [CrossRef]
- Santos, L.A.; Pinheiro, D.G.; Silva, J.M.D.; Borges, G.L.B.; Silva, P.F.D.; Ricci-Vitor, A.L.; Vanderlei, L.C.M. Analysis of Barriers to Public and Private Cardiac Rehabilitation Programs in Patients with Low and High Adherence. Braz. J. Cardiovasc. Surg. 2023, in press. [Google Scholar] [CrossRef]
- Rangel-Cubillos, D.M.; Vega-Silva, A.V.; Corzo-Vargas, Y.F.; Molano-Tordecilla, M.C.; Peñuela-Arévalo, Y.P.; Lagos-Peña, K.M.; Jácome-Hortúa, A.M.; Villamizar-Jaimes, C.J.; Grace, S.L.; Dutra de Souza, H.C.; et al. Examining Facilitators and Barriers to Cardiac Rehabilitation Adherence in a Low-Resource Setting in Latin America from Multiple Perspectives. Int. J. Environ. Res. Public Health 2022, 19, 1911. [Google Scholar] [CrossRef]
- Jácome Hortúa, A.M.; Angarita-Fonseca, A.; Villamizar Jaimes, C.J.; Martínez Marín, R.d.P.; Dutra de Souza, H.C.; de Paula Facioli, T.; Sánchez-Delgado, J.C. Reliability of the Scale of Barriers for Cardiac Rehabilitation in the Colombian Population. Int. J. Environ. Res. Public Health 2021, 18, 4351. [Google Scholar] [CrossRef]
- Vargas, Y.F.C.; Cubillos, D.M.R.; Silva, A.V.V.; Hortua, A.M.J.; Marin, R.d.P.M.; Jaiems, J.V.; Grace, S.L.; Sanchez Delgado, J.C. Barreras que influyen en la participacion y adherencia a los programas de rehabilitacion cardiaca de la cuidad de Bucaramanga. Rev. Colomb. Cardiol. 2020, 27, 21. [Google Scholar]
- Winnige, P.; Batalik, L.; Filakova, K.; Hnatiak, J.; Dosbaba, F.; Grace, S.L. Translation and Validation of the Cardiac Rehabilitation Barriers Scale in the Czech Republic (CRBS-CZE): Protocol to Determine the Key Barriers in East-Central Europe. Medicine 2020, 99, e19546. [Google Scholar] [CrossRef] [PubMed]
- Fatimah, N.; Grace, S.; Emaliyawati, E.; Somantri, I.; Sivapalan, D. Cardiac rehabilitation barriers in Indonesia. IJNCD 2017, 2, S7. [Google Scholar]
- Qiu, X.; Qiu, C.; Wang, Y.; Gao, M. Reliability and validity of Chinese version of Cardiac Rehabilitation Barriers Scale. Acad. J. Chin. PLA Med. Sch. 2018, 39, 1067–1071. [Google Scholar]
- Xie, X.; Chen, Q.; Liu, H. Barriers to Hospital-Based Phase 2 Cardiac Rehabilitation among Patients with Coronary Heart Disease in China: A Mixed-Methods Study. BMC Nurs. 2022, 21, 333. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Fowokan, A.; Grace, S.L.; Ding, B.; Meng, S.; Chen, X.; Xia, Y.; Zhang, Y. Translation, Cross-Cultural Adaptation, and Psychometric Validation of the Chinese/Mandarin Cardiac Rehabilitation Barriers Scale (CRBS-C/M). Rehabil. Res. Pract. 2021, 2021, 5511426. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Fule, W.; Bhutta, Z. Path analysis of influencing factors of outpatient cardiac rehabilitation program participation of patients with coronary heart disease in Shanghai. J. Shanghai Jiao Tong Univ. (Med. Sci.) 2022, 42, 1110–1115. [Google Scholar]
- Chai, L.S.; Siop, S.; Putit, Z.; Lim, L.; Gunggu, A.; Tie, S.F. Translation, Adaptation, and Validation of the Malay Version of the Cardiac Rehabilitation Barriers Scale. J. Nurs. Res. 2020, 28, e64. [Google Scholar] [CrossRef]
- Singh, S.K.; Abdullah, K.L.; Abidin, I.Z.; Yahya, A. Perceived barriers among cardiac patients towards cardiac rehabilitation programme: A preliminary study. Malays. J. Med. Health Sci. 2020, 16, 3. [Google Scholar]
- Baek, S.; Park, H.; Lee, Y.; Grace, S.L.; Kim, W.-S. Translation, Cross-Cultural Adaptation and Psychometric Validation of the Korean-Language Cardiac Rehabilitation Barriers Scale (CRBS-K). Ann. Rehabil. Med. 2017, 41, 858. [Google Scholar] [CrossRef]
- Im, H.W.; Baek, S.; Jee, S.; Ahn, J.-M.; Park, M.W.; Kim, W.-S. Barriers to Outpatient Hospital-Based Cardiac Rehabilitation in Korean Patients with Acute Coronary Syndrome. Ann. Rehabil. Med. 2018, 42, 154. [Google Scholar] [CrossRef] [PubMed]
- Babu, A.S.; Lopez-Jimenez, F.; Thomas, R.J.; Isaranuwatchai, W.; Herdy, A.H.; Hoch, J.S.; Grace, S.L. Advocacy for Outpatient Cardiac Rehabilitation Globally. BMC Health Serv. Res. 2016, 16, 471. [Google Scholar] [CrossRef] [PubMed]
- Turk-Adawi, K.; Elshaikh, U.; Contractor, A.; Hashmi, F.; Thomas, E.E.; Raidah, F.; Grace, S.L. Development and evaluation of the International Council of Cardiovascular Prevention and Rehabilitation (ICCPR) Program Certification. Circ. Cardiovasc. Qual. Outcomes 2023. under review. [Google Scholar]
- Santiago de Araújo Pio, C.; Gagliardi, A.; Suskin, N.; Ahmad, F.; Grace, S.L. Implementing Recommendations for Inpatient Healthcare Provider Encouragement of Cardiac Rehabilitation Participation: Development and Evaluation of an Online Course. BMC Health Serv. Res. 2020, 20, 768. [Google Scholar] [CrossRef]
- Heald, F.A.; de Araújo Pio, C.S.; Liu, X.; Theurel, F.R.; Pavy, B.; Grace, S.L. Evaluation of an Online Course in 5 Languages for Inpatient Cardiac Care Providers on Promoting Cardiac Rehabilitation: Reach, effects, and satisfaction. J. Cardiopulm. Rehabil. Prev. 2021, in press. [Google Scholar] [CrossRef]
- Ivers, N.M.; Schwalm, J.-D.; Bouck, Z.; McCready, T.; Taljaard, M.; Grace, S.L.; Cunningham, J.; Bosiak, B.; Presseau, J.; Witteman, H.O.; et al. Interventions Supporting Long Term Adherence and Decreasing Cardiovascular Events after Myocardial Infarction (ISLAND): Pragmatic Randomised Controlled Trial. BMJ 2020, 369, m1731. [Google Scholar] [CrossRef]
- Grace, S.L.; Chessex, C.; Arthur, H.; Chan, S.; Cyr, C.; Dafoe, W.; Juneau, M.; Oh, P.; Suskin, N. Systematizing Inpatient Referral to Cardiac Rehabilitation 2010: Canadian Association of Cardiac Rehabilitation and Canadian Cardiovascular Society Joint Position Paper. J. Cardiopulm. Rehabil. Prev. 2011, 31, E1–E8. [Google Scholar] [CrossRef]
- Tsui, C.K.-Y.; Shanmugasegaram, S.; Jamnik, V.; Wu, G.; Grace, S.L. Variation in Patient Perceptions of Healthcare Provider Endorsement of Cardiac Rehabilitation. J. Cardiopulm. Rehabil. Prev. 2012, 32, 192–197. [Google Scholar] [CrossRef]
- Thomas, R.J.; Beatty, A.L.; Beckie, T.M.; Brewer, L.C.; Brown, T.M.; Forman, D.E.; Franklin, B.A.; Keteyian, S.J.; Kitzman, D.W.; Regensteiner, J.G.; et al. Home-Based Cardiac Rehabilitation. J. Am. Coll. Cardiol. 2019, 74, 133–153. [Google Scholar] [CrossRef]
| Sociodemographic Characteristics | n (%)/ Mean ± SD | Median CRBS-A Score (Interquartile Range) | p a |
|---|---|---|---|
| Age | 58.2 ± 13.9 | - | 0.62 |
| Less than 65 years old | 123 (59.4) | 2.8 (2.3–3.5) | |
| 65 years old or older | 66 (31.9) | 2.9 (2.6–3.3) | |
| Sex | 0.27 | ||
| Male | 128 (61.8) | 2.9 (2.5–3.4) | |
| Female | 75 (36.2) | 2.8 (2.4–3.3) | |
| Other/prefer not to answer | 2 (1.0) | ||
| Work status | 0.33 | ||
| Retired | 93 (44.9) | 3.0 (2.6–3.4) | |
| Full or part-time | 59 (28.5) | 2.7 (2.4–3.5) | |
| Unemployed | 27 (13.0) | 2.9 (2.3–3.5) | |
| Disability/sick leave/modified duties | 17 (8.2) | 2.7 (2.0–3.1) | |
| Looking to get a paid job | 8 (3.9) | 2.7 (2.6–3.3) | |
| Social support (/5) b | 3.3 ± 1.1 | - | 0.26 |
| Definitely | 32 (15.5) | 3.1 (2.6–3.5) | |
| Most of the time | 46 (22.2) | 3.0 (2.5–3.5) | |
| Sometimes | 78 (37.7) | 2.8 (2.4–3.3) | |
| Rarely | 34 (16.4) | 2.9 (2.6–3.3) | |
| Never | 13 (6.3) | 2.5 (2.1–3.0) | |
| Years of formal education | 13.2 ± 6.2 | - | 0.66 |
| Less than 8 years | 18 (8.7) | 2.8 (2.4–3.6) | |
| 8 or more years | 152 (73.4) | 2.7 (2.4–3.3) | |
| Worrying about having enough money to pay for health care | 0.20 | ||
| I often worry | 65 (31.4) | 2.8 (2.5–3.3) | |
| I worry sometimes | 105 (50.7) | 3.0 (2.6–3.5) | |
| I never worry | 35 (16.9) | 2.7 (2.3–2.9) | |
| Physical activity prior to heart problem | 0.58 | ||
| Yes | 40 (19.3) | 2.7 (2.4–3.6) | |
| No | 159 (76.8) | 2.9 (2.5–3.4) | |
| Referral to CR | 0.04 | ||
| Yes | 43 (20.8) | 2.6 (2.3–3.3) | |
| No/I do not know | 158 (76.3) | 3.1 (2.5–3.4) |
| Item | Factor 1: Time Conflicts/Lack of Perceived Need/Excuses | Factor 2: Prefer to Self-Manage | Factor 3: Logistical Barriers | Factor 4: Health System Issues/Comorbidities |
|---|---|---|---|---|
| 11. …of time constraints (e.g., too busy, inconvenient class time) | 0.799 | |||
| 7. …I already exercise at home, or in my community | 0.768 | |||
| 12. …of work responsibilities | 0.741 | |||
| 10. …travel (e.g., holidays, business, cottage) | 0.688 | |||
| 6. …I do not need cardiac rehab (e.g., feel well, heart problem treated, not serious) | 0.676 | |||
| 8. …severe weather | 0.674 | |||
| 9. …I find exercise tiring or painful | 0.480 | |||
| 4. … family responsibilities (e.g., caregiving) | 0.434 | |||
| 18. … I can manage my heart problem on my own | 0.840 | |||
| 17. … many people with heart problems do not go, and they are fine | 0.824 | |||
| 19. … I think I was referred, but the rehab program did not contact me | 0.786 | |||
| 21. …I prefer to take care of my health alone, not in a group | 0.604 | |||
| 15. …I am too old | 0.572 | |||
| 3. … difficulties in accessing sessions that require attendance in person (for example, lack of car or suitable transportation) | 0.818 | |||
| 2. … costs (e.g., program participation costs, transportation and parking costs, qualification requirements such as shoes, exercise, equipment/educational materials, equipment costs) | 0.725 | |||
| 1. … distance (e.g., there is not a program in the same area, too far for travel) | 0.661 | |||
| 5. …I did not know about cardiac rehab (e.g., doctor did not tell me about it) | −0.711 | |||
| 16. …my doctor did not feel it was necessary | −0.597 | |||
| 14. …other health problems prevent me from going. | 0.581 | |||
| 20. …it took too long to get referred and into the program | 0.576 | |||
| 13. …I do not have the energy | 0.413 | |||
| Variance explained | 23.3% | 17.8% | 12.7% | 8.9% |
| Eigenvalues | 7.50 | 2.41 | 2.03 | 1.25 |
| Reliability | 0.88 | 0.84 | 0.78 | 0.50 |
| CRBS-A Item | Total (N = 207) | N/A (%) |
|---|---|---|
| 1. …distance (e.g., there is not a program in the same area, too far for travel) | 3.4 ± 1.5 | 21 (10.1) |
| 2. …costs (e.g., program participation costs, transportation and parking costs, qualification requirements such as shoes, exercise, equipment/educational materials, equipment costs) | 3.2 ± 1.5 | 19 (9.2) |
| 3. …difficulties in accessing sessions that require attendance in person (for example, lack of car or suitable transportation) | 3.4 ± 1.5 | 20 (9.7) |
| 4. …family responsibilities (e.g., caregiving) | 3.1 ± 1.5 | 20 (9.7) |
| 5. …I did not know about cardiac rehab (e.g., doctor did not tell me about it) | 4.1 ± 1.3 | 7 (3.4) |
| 6. …I do not need cardiac rehab (e.g., feel well, heart problem treated, not serious) | 2.6 ± 1.3 | 14 (6.8) |
| 7. …I already exercise at home, or in my community | 2.6 ± 1.4 | 17 (8.2) |
| 8. …severe weather | 2.8 ± 1.4 | 16 (7.7) |
| 9. …I find exercise tiring or painful | 2.9 ± 1.4 | 13 (6.3) |
| 10. …travel (e.g., holidays, business, cottage) | 2.3 ± 1.5 | 17 (8.2) |
| 11. …of time constraints (e.g., too busy, inconvenient class time) | 2.8 ± 1.4 | 20 (9.7) |
| 12. …of work responsibilities | 2.5 ± 1.6 | 31 (15.0) |
| 13. …I do not have the energy | 2.9 ± 1.4 | 15 (7.2) |
| 14. …other health problems prevent me from going. | 2.2 ± 1.4 | 33 (15.9) |
| 15. …I am too old | 2.7 ± 1.5 | 21 (10.1) |
| 16. …my doctor did not feel it was necessary | 3.6 ± 1.5 | 10 (4.8) |
| 17. …many people with heart problems do not go, and they are fine | 2.6 ± 1.4 | 17 (8.2) |
| 18. …I can manage my heart problem on my own | 2.8 ± 1.4 | 11 (5.3) |
| 19. …I think I was referred, but the rehab program did not contact me | 2.5 ± 1.4 | 17 (8.2) |
| 20. …it took too long to get referred and into the program | 2.5 ± 1.6 | 28 (13.5) |
| 21. …I prefer to take care of my health alone, not in a group | 2.8 ± 1.4 | 28 (13.5) |
| Factor 1: time conflicts/lack of perceived need/excuses | 2.7 ± 1.0 | - |
| Factor 2: prefer to self-manage | 2.7 ± 1.0 | - |
| Factor 3: logistical barriers | 3.3 ± 1.3 | - |
| Factor 4: health system issues/comorbidities | 3.1 ± 0.8 | - |
| Total CRBS-A | 2.9 ± 0.8 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aljehani, R.; Grace, S.L.; Aburub, A.; Turk-Adawi, K.; Ghisi, G.L.d.M. Translation, Cross-Cultural Adaptation and Psychometric Validation of the Arabic Version of the Cardiac Rehabilitation Barriers Scale (CRBS-A) with Strategies to Mitigate Barriers. Healthcare 2023, 11, 1196. https://doi.org/10.3390/healthcare11081196
Aljehani R, Grace SL, Aburub A, Turk-Adawi K, Ghisi GLdM. Translation, Cross-Cultural Adaptation and Psychometric Validation of the Arabic Version of the Cardiac Rehabilitation Barriers Scale (CRBS-A) with Strategies to Mitigate Barriers. Healthcare. 2023; 11(8):1196. https://doi.org/10.3390/healthcare11081196
Chicago/Turabian StyleAljehani, Raghdah, Sherry L. Grace, Aseel Aburub, Karam Turk-Adawi, and Gabriela Lima de Melo Ghisi. 2023. "Translation, Cross-Cultural Adaptation and Psychometric Validation of the Arabic Version of the Cardiac Rehabilitation Barriers Scale (CRBS-A) with Strategies to Mitigate Barriers" Healthcare 11, no. 8: 1196. https://doi.org/10.3390/healthcare11081196
APA StyleAljehani, R., Grace, S. L., Aburub, A., Turk-Adawi, K., & Ghisi, G. L. d. M. (2023). Translation, Cross-Cultural Adaptation and Psychometric Validation of the Arabic Version of the Cardiac Rehabilitation Barriers Scale (CRBS-A) with Strategies to Mitigate Barriers. Healthcare, 11(8), 1196. https://doi.org/10.3390/healthcare11081196








