Unemployment and Substance Use: An Updated Review of Studies from North America and Europe
Abstract
1. Introduction
- To what extent are substance use and SUD affecting the unemployed versus the employed?
- To what extent does substance use and SUD increase the likelihood of unemployment and decrease the chances of employment or being rehired?
- To what extent is unemployment a risk factor for SUD?
- Does unemployment increase the risk of relapse after treatment?
- Does unemployment reduce the success of smoking cessation?
- To what extent are substance-use patterns associated with unemployment rates and are there cyclical fluctuations?
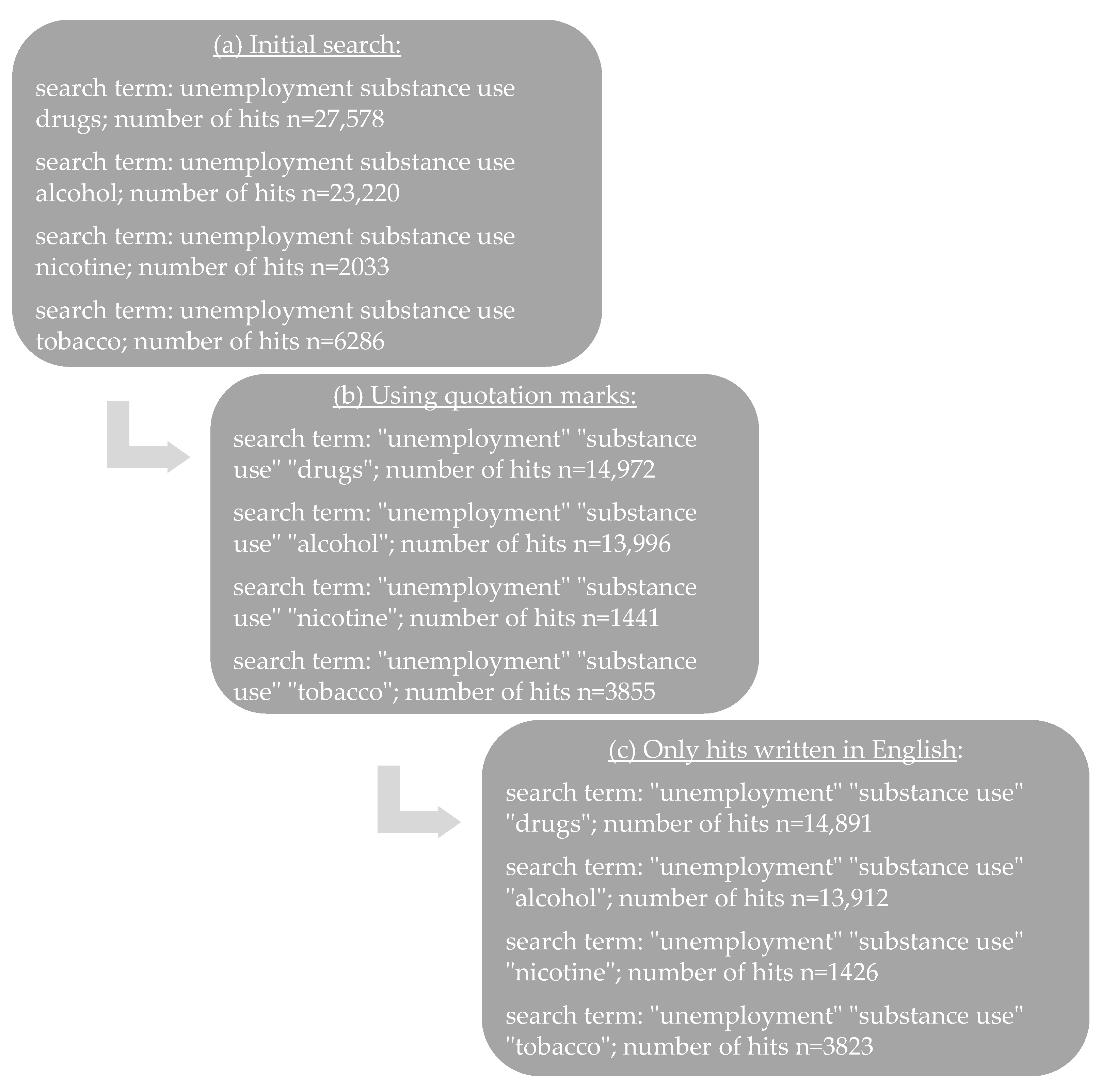
2. Materials and Methods
3. Results
3.1. Prevalence of SUD among the Employed and Unemployed
| Data Source | Authors | N, Age | Substance-Use Disorders | U (%) | E (%) | OR E = 1 | ||
|---|---|---|---|---|---|---|---|---|
| U.K. MCS/ ALSPAC/ NS/BCS70/ NCDS/ USOC/ ELSA/GS 2020 | Green, M. et al., 2022 [45] | 27,841 16–66 | Current smoking (furloughed, no longer employed, stable unemployed) Current vaping (furloughed, no longer employed, stable unemployed) Current drinking (furloughed, no longer employed, stable unemployed) | |||||
| France CONSTANCES 2012/2018 | El Haddad et al., 2022 [46] | 1427 18–69 | Tobacco use | |||||
| Light smoker | 19.4 | 14.2 | ||||||
| Moderate smoker | 6.5 | 7.3 | ||||||
| Heavy smoker | 2.2 | 0.6 | ||||||
| Cannabis use | ||||||||
| >12 months ago | 13.0 | 13.0 | ||||||
| <1x per month | 8.1 | 8.1 | ||||||
| ≥1x per month | 16.2 | 8.1 | ||||||
| Alcohol use | ||||||||
| Frequency [0–2/3–5/6+ AUDIT sub-score] | 34.6/33.0/32.4 | 32.2/38.2/29.6 | ||||||
| Dependence [1,2/3+ AUDIT sub-score] | 29.7/24.3 | 30.6/19.6 | ||||||
| Denmark DNHS 2010 | Egan, K. et al., 2021 [47] | 84,474 18–60 | Median alcohol consumption (5th–95th) | 7.13 drinks/week | 9.1 drinks/week | |||
| Problem drinking | 5.7 | 2.8 | ||||||
| Current smoker | 35.5 | 18.1 | ||||||
| Netherlands DLCS 2006–2013 | Mangot-Sala, L. et al., 2021 [34] | 45,967 25–50 | Short U | Long U | ||||
| Abstainer | 16.71 *** | 22.86 *** | 15.15 *** | |||||
| Moderate drinking (<1.5 drinks/day) | 71.75 | 62.60 | 71.59 | |||||
| Heavy drinking (≥1.5 drinks/day) | 11.54 | 14.55 | 13.26 | |||||
| Binge drinking (≥5 [♂]/≥4 [♀] drinks/occasion) | 12.50 | 13.07 * | 10.86 * | |||||
| USA TEDS 1993–2016 | Azagba, S. et al., 2021 [48] | n.a. ≥18 | Treatment admissions for primary substance abuse (opiates, cocaine, alcohol, marijuana, other drugs, stimulants) | |||||
| Sweden SWIP 2010–2017 | Jonsson, J. et al., 2021 [26] | 2,743,764 18–61 | Substance abuse | ♂97/♀8 cases; Adjusted HR *****: 1.0 | ♂6902/♀5245 cases in standard employment; Adjusted HR: 2.5 | |||
| England GP 2011–2017 | Vandoros, S. et al., 2020 [49] | 8736 n.a. | Opioid prescribing | |||||
| Defined daily dose per capita | 1.745 | |||||||
| Items per capita | 0.102 | |||||||
| Quantity per capita | 9.526 | |||||||
| Defined daily dose per 1000 days | 19.108 | |||||||
| USA CARDIA 2005–2010 | Swift, S. et al., 2020 [50] | 1307 n.a. | Binge drinking, past 30-day drug use | |||||
| Italy n.a. 2019 | De Sio, S. et al., 2020 [41] | 314 n.a. | Carbohydrate-deficient transferrin | 13.4 | 7.0 | 0.47 | ||
| Aspartate transaminase | 23.6 ** | 12.1 ** | 0.42 ** | |||||
| Alanine transaminase | 55.7 ** | 34.8 ** | 0.39 ** | |||||
| γ-glutamyltransferase | 29.3 * | 17.8 * | 0.48 * | |||||
| Mean corpuscular volume | 23.6 ** | 10.8 ** | 0.37 ** | |||||
| Spain EDADES 2007/2013 | Casal, B. et al., 2020 [40] | 23,258/ 22,862; 16–64 | 2007 | 2013 | 2007 | 2013 | ||
| Cannabis use | 13.52 | 34.23 | 56.40 | 36.63 | ||||
| Cocaine use | 15.87 | 37.45 | 62.19 | 44.57 | ||||
| Both | 16.49 | 39.61 | 59.72 | 40.82 | ||||
| Denmark DNHS 2010 | Bæksgaard Jørgensen, M. et al., 2019 [51] | 86,417 18–60 | Median alcohol consumption (5th–95th) | 10.0 drinks/week | 7.6 drinks/week | |||
| Problem drinking | 5.1 | 2.8 | ||||||
| Current smoker | 38.1 | 23.0 | ||||||
| France CONSTANCES 2012–2016 | Airagnes, G. et al., 2019 [52] | 18,879 18–69 | Alcohol use | |||||
| Dangerous | 16.4 | 11.5 | 1.46 *** | |||||
| Problematic or dependence | 3.4 | 1.5 | 1.92 *** | |||||
| Tobacco use | ||||||||
| Light smoker | 14.3 | 10.5 | 1.54 *** | |||||
| Moderate smoker | 10.0 | 6.6 | 1.69 *** | |||||
| Heavy smoker | 3.5 | 2.1 | 1.78 ** | |||||
| Cannabis use | ||||||||
| >12 months ago | 43.9 | 39.5 | 1.45 *** | |||||
| <1x per month | 6.5 | 4.0 | 1.87 *** | |||||
| ≥1x per month | 8.8 | 4.0 | 1.68 *** | |||||
| USA n.a. n.a. | Miguel, A. et al., 2019 [43] | 553 ≥18 | History of cocaine use | |||||
| Age of cocaine onset | 20.6 ± 5.6 years | 21.3 ± 7 years | ||||||
| Years of cocaine use | 10.3 ± 7.9 years | 8.8 ± 7.7 years | ||||||
| Days of cocaine use in 28 days prior to treatment | 14.5 ± 8.6 days | 14 ± 9.1 days | ||||||
| Pretreatment cocaine positive urine result | 72.8 | 77.2 | 1.61 | |||||
| History of substance abuse treatment | ||||||||
| Treatment naïve | 16.4 | 15.6 | ||||||
| Number outpatient substance-use treatments | 2.2 ± 3.3 treatments | 2.4 ± 3.4 | ||||||
| Number inpatient substance-use treatments | 2.7 ± 4.3 treatments | 2.9 ± 5.9 | ||||||
| Concomitant psychiatric disorders | ||||||||
| Lifetime alcohol-use disorder | 68 | 68.3 | ||||||
| Germany SUNRISE 2021 | Scherbaum, N. et al., 2018 [25] | 87 25–49 | Alcohol abuse/addiction | 5.8/69.8 | ||||
| Opioid abuse/addiction | 2.3/4.7 | |||||||
| Opioid dependence, but in substitution treatment | 10.5 | |||||||
| Cannabis abuse/addiction | 0.5/26.7 | |||||||
| Sedative/hypnotics abuse/addiction | 4.7/7.0 | |||||||
| Cocaine abuse/addiction | 7.0/4.7 | |||||||
| Stimulants abuse/addiction | 7.0/2.3 | |||||||
| Hallucinogen abuse | 2.3 | |||||||
| Polydrugmania | 1.2 | |||||||
| Spain EDADES 2013 | Teixidó-Compañó, E. et al., 2018 [32] | 14,113 25–64 | Hazardous drinking | ♂7.9; ♀2.6 | ♂6.2; ♀3.9 | |||
| Heavy cannabis use | ♂6.2; ♀1.5 | ♂2.4; ♀0.6 | ||||||
| Hypnosedative consumption | ♂9.9; ♀18.4 | ♂6.4; ♀13.4 | ||||||
| USA NESARC 2001–2004/ 2012–2013 | Okechukwu, C. et al., 2018 [38] | 23,446/ 23,346 ≥18 | 2012–13 | 2012–13 | ||||
| Past year marijuana use (daily/weekly/ ≤monthly) | 22.95 (7.56/4.62/10.77/77.05) | 10.27 (3.02/1.89/5.36) | ||||||
| Past year use disorder | 6.65 | 2.63 | ||||||
| Lifetime alcohol disorder | 47.71 | 33.04 | ||||||
| Lifetime drug disorder | 12.20 | 5.79 | ||||||
| Netherlands HIS 2004–2013 | De Goeij, M. et al., 2017 [53] | 26,355 30–64 | Episodic drinking | |||||
| Before economic crisis (2004–2008) | 1.3 | 0.87 | ||||||
| During economic crisis (2008–2013) | 2.9 | 1.24 | ||||||
| USA PSID 1999–2011 | Grafova, I. et al., 2017 [31] | 41,231 n.a. | Current smoker | ♂19.87; ♀18.52 | ||||
| Former smoker | ♂30.69; ♀27.55 | |||||||
| Smoking relapse | ♂8.09; ♀10.20 | |||||||
| Increased cigarette consumption | ♂14.24; ♀15.98 | |||||||
| Quit smoking | ♂17.19; ♀17.93 | |||||||
| Decreased cigarette consumption | ♂42.50; ♀43.04 | |||||||
| Spain Flash EB 2011/2014 | Ayllón, S. et al., 2018 [29] | n.a. 15–24 | 2011 | 2014 | ||||
| Consumption of cannabis | ||||||||
| At any point in time | 24.0 | 28.5 | ||||||
| Last 30 days | 5.0 | 5.7 | ||||||
| Last 12 months | 7.4 | 8.7 | ||||||
| >12 months ago | 11.6 | 14.1 | ||||||
| Consumption of new substances | ||||||||
| At any point in time | 4.7 | 7.4 | ||||||
| Last 30 days | 1.1 | |||||||
| Last 12 months | 2.2 | |||||||
| >12 months ago | 4.0 | |||||||
| Germany SUF 2016 | Hollederer, A. et al., 2016 [27] | 8951 15–64 | Consumption of beer, wine or mixed drinks | |||||
| every day | ♂9.1; ♀0.3 | ♂7.9; ♀1.4 *** | ||||||
| several times a week | ♂14.2; ♀4.2 | ♂24.1; ♀10.6 *** | ||||||
| once a week | ♂16.0; ♀9.7 | ♂26.9; ♀15.3 *** | ||||||
| less common | ♂32.7; ♀36.0 | ♂31.0; ♀50.6 *** | ||||||
| Consumption of spirits | ||||||||
| every day | ♂1.2; ♀ <0.1 | ♂0.2; 0.0 f *** | ||||||
| several times a week | ♂1.9; ♀0.2 | ♂2.5; 0.7 f *** | ||||||
| once a week | ♂6.6; ♀1.7 | ♂12.7; 2.4 f *** | ||||||
| less common | ♂36.3; ♀20.5 | ♂45.7; 35.1 f *** | ||||||
| Nicotine consumption | ♂66.0 ***; ♀52.1 *** | ♂32.2 ***; 25.6 f *** | ||||||
| AT/BE/CZ/DK/FR/DE/IT/NL/ES/SE/CH ****** SHARE 2006–2012 | Bosque-Prous, M. et al., 2015 [39] | 7615 50–64 | Hazardous drinking (≥40 g and ≥20 g of pure alcohol per day) | 7.3 | 7.1 | |||
| USA SSDP n.a. | Lee, J. et al., 2015 [54] | n.a. 22–33 | Heavy episodic drinking (>6 months of use) Daily cigarette smoking (>6 months of use) Marijuana use (>6 months of use) | |||||
| USA FTDO 1992–1994 | Chintakrindi, S. et al., 2015 [55] | n.a. n.a. | Drug use prior to arrest (used alcohol, marijuana, uppers, cocaine, crack, heroin, any drugs) | |||||
| Finland SF 2000–2007 | Paljärvi, T. et al., 2014 [42] | 204,422 45–64 | Alcohol-related death in relation to average annual number of days | 177.5 days | 134.9 days | |||
| USA NSDUH 2002–2004/ 2005–2007/ 2008/ 2009–2010 | Compton, W. et al., 2014 [28] | ~ 405,000 ≥18 | 2009–10 | 2009–10 | ||||
| Heavy alcohol use (≥5 drinks on ≥5 days) | 0.58 | 0.16 **** | 1.17 | |||||
| Illicit drug use | 0.66 | 0.18 **** | 1.60 | |||||
| Tobacco use | 0.98 | 0.31 **** | 1.56 | |||||
| Alcohol abuse/dependence | 0.57 | 0.16 **** | 1.28 | |||||
| Illicit drug abuse/dependence | 0.37 | 0.08 **** | 1.79 | |||||
| USA n.a. 1983/ 1985–1986/ 1992/1997/ 2002/2007/ 2012–2013 | Brook, J. et al., 2014 [56] | 2012–13 528 ∅43 | 2012–13 | |||||
| Heavy/continuous smokers | 3.84 * | |||||||
| Late starters | 1.57 | |||||||
| Occasional smokers | 4.03 * | |||||||
| Quitters/decreasers | 1.51 | |||||||
| USA NAS12 2009–2010 | Mulia, N. et al., 2014 [33] | 5382 ≥18 | Alcohol-related health problems prior to recession | 14.6 | ||||
| USA NESARC 2001–2002/ 2004–2005 | Baldwin, M. et al., 2013 [57] | n.a. 19–60 | Part-time | Full-time | ||||
| Alcohol disorder (not employed, employed part-time, and employed full-time in each wave 1 and 2) | 39.67 | 34.26 | 86.63 | |||||
| Drug disorder (not employed, employed part-time, and employed full-time in each wave 1 and 2) | 45.88 | 21.26 | 83.34 | |||||
| USA CLS 2004–2005 | Arria, A. et al., 2013 [58] | 620 17–19 | Part-time | Full-time | ||||
| Alcohol consumption | 4.8 | 3.9 | 4.8 | |||||
| Drug use pattern group | ||||||||
| Infrequent marijuana use | 29.4 | 19.7 | 25.7 | |||||
| Sporadic drug use | 35.5 | 35.5 | 41.0 | |||||
| Persistent drug use | 29.4 | 21.1 | 14.3 | |||||
| USA HRS 1992–2008 | Deb, P. et al., 2012 [59] | 20,557 ≥50 | Daily number of drinks | 0.818 drinks/day | 0.811 drinks/day | |||
| Germany SOEP 1998–2009 | Schunck, R. et al., 2012 [30] | 17,028 17–65 | Smoking Number of cigarettes/day | 48.94 17.08 cigarettes/day | 33.34 16.60 cigarettes/day | |||
| USA NESARC 2001–2002/ 2004–2005 | Dávalos, M. et al., 2012 [60] | 34,120 ≥18 | Alcohol consumption (past year) | |||||
| Any binge drinking | 21.8/24.9 | |||||||
| Days of binge drinking (≥5 [♂]/ ≥ 4 [♀] drinks per episode) | 12.8 days/12.7 days | |||||||
| Driving after too much | 2.7/3.7 | |||||||
| to drink (≥1 in past year) | ||||||||
| Abuse and/or dependence | 7.7/9.0 | |||||||
| USA n.a. n.a. | Weber, E. et al., 2012 [44] | 110 n.a. | Metamphetamine (MA) use characteristics | |||||
| Age of first use | 22.5 years | 21.9 years | ||||||
| Total duration of use | 11.4 years | 7.7 years | ||||||
| Total quantity of use | 4834 g | 3704 g | ||||||
| Last use | 139 days | 188 days | ||||||
| Injection MA use ever | 52.1 * | 13.3 * | ||||||
| Non-MA dependence | ||||||||
| Cannabis (lifetime) | 10.4 | 20.0 | ||||||
| Alcohol (lifetime) | 35.4 | 40.0 | ||||||
| Cocaine (lifetime) | 20.8 | 33.3 | ||||||
| Other substances (lifetime) | 14.6 | 6.7 | ||||||
3.2. SUD as a Risk Factor for Unemployment
3.3. Unemployment as a Risk Factor for the Development of SUD
3.4. Unemployment as a Risk Factor for Relapses after Smoking Cessation
3.5. Unemployment Reducing the Success of Smoking Cessation
3.6. Substance-Use Patterns Based on Unemployment Rates and Business Cycle/Cyclical Fluctuations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jahoda, M.; Lazarfeld, P.F.; Zeisel, H. Die Arbeitslosen von Marienthal. Ein Soziographischer Versuch über die Wirkungen langandauernder Arbeitslosigkeit; Suhrkamp: Frankfurt am Main, Germany, 1975. [Google Scholar]
- Herbig, B.; Dragano, N.; Angerer, P. Health in the long-term unemployed. Dtsch. Arztebl. Int. 2013, 110, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Kroll, L.E.; Lampert, T. Unemployment, social support and health problems: Results of the GEDA study in Germany, 2009. Dtsch. Arztebl. Int. 2011, 108, 47–52. [Google Scholar]
- Berth, H.; Förster, P.; Stöbel-Richter, Y.; Balck, F.; Brähler, E. Arbeitslosigkeit und psychische Belastung. Ergebnisse einer Längsschnittstudie 1991 bis 2004. Z. Med. Psychol. 2006, 15, 111–116. [Google Scholar]
- Hanisch, K.A. Job loss and unemployment research from 1994 to 1998: A review and recommendations for research and intervention. J. Vocat. Behav. 1999, 55, 188–220. [Google Scholar] [CrossRef]
- Leeflang, R.L.; Klein-Hesselink, D.J.; Spruit, I.P. Health effects of unemployment—I. Long-term unemployed men in a rural and an urban setting. Soc. Sci. Med. 1992, 34, 341–350. [Google Scholar] [CrossRef]
- Roelfs, D.J.; Shor, E.; Davidson, K.W.; Schwartz, J.E. Losing life and livelihood: A systematic review and meta-analysis of unemployment and all-cause mortality. Soc. Sci. Med. 2011, 72, 840–854. [Google Scholar] [CrossRef] [PubMed]
- McKee-Ryan, F.; Song, Z.; Wanberg, C.R.; Kinicki, A.J. Psychological and physical well-being during unemployment: A meta-analytic study. J. Appl. Psychol. 2005, 90, 53–76. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.W.; Balluz, L.S.; Ford, E.S.; Giles, W.H.; Strine, T.W.; Moriarty, D.G.; Croft, J.B.; Mokdad, A.H. Associations between short- and long-term unemployment and frequent mental distress among a national sample of men and women. J. Occup. Environ. Med. 2003, 45, 1159–1166. [Google Scholar] [CrossRef]
- Janlert, U.; Hammarstrom, A. Which theory is best? Explanatory models of the relationship between unemployment and health. BMC Public Health 2009, 9, 235. [Google Scholar]
- Catalano, R.; Goldman-Mellor, S.; Saxton, K.; Margerison-Zilko, C.; Subbaraman, M.; LeWinn, K.; Anderson, E. The health effects of economic decline. Annu. Rev. Public. Health 2011, 32, 431–450. [Google Scholar] [CrossRef]
- Dooley, D.; Catalano, R.; Hough, R. Unemployment and alcohol disorder in 1910 and 1990: Drift versus social causation. J. Occup. Organ. Psychol. 1992, 65, 277–290. [Google Scholar] [CrossRef]
- Henkel, D. Unemployment and substance use: A review of the literature (1990–2010). Curr. Drug. Abuse Rev. 2011, 4, 4–27. [Google Scholar] [CrossRef] [PubMed]
- Mossakowski, K.N. Is the duration of poverty and unemployment a risk factor for heavy drinking? Soc. Sci. Med. 2008, 67, 947–955. [Google Scholar] [CrossRef]
- Collaborators, G.B.D.M.D. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022, 9, 137–150. [Google Scholar]
- Alcohol, G.B.D.; Drug Use, C. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry 2018, 5, 987–1012. [Google Scholar]
- Castelpietra, G.; Knudsen, A.K.S.; Agardh, E.E.; Armocida, B.; Beghi, M.; Iburg, K.M.; Logroscino, G.; Ma, R.; Starace, F.; Steel, N.; et al. The burden of mental disorders, substance use disorders and self-harm among young people in Europe, 1990–2019: Findings from the Global Burden of Disease Study 2019. Lancet Reg. Health Eur. 2022, 16, 100341. [Google Scholar] [CrossRef]
- Whiteford, H.A.; Degenhardt, L.; Rehm, J.; Baxter, A.J.; Ferrari, A.J.; Erskine, H.E.; Charlson, F.J.; Norman, R.E.; Flaxman, A.D.; Johns, N.; et al. Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet 2013, 382, 1575–1586. [Google Scholar] [CrossRef]
- Whiteford, H.A.; Ferrari, A.J.; Degenhardt, L.; Feigin, V.; Vos, T. The global burden of mental, neurological and substance use disorders: An analysis from the Global Burden of Disease Study 2010. PLoS ONE 2015, 10, e0116820. [Google Scholar] [CrossRef]
- Brenner, M.H. Trends in alcohol consumption and associated illnesses. Some effects of economic changes. Am. J. Public. Health 1975, 65, 1279–1292. [Google Scholar]
- Brenner, M.H. Mortality and the national economy. Lancet 1975, 26, 568–573. [Google Scholar]
- Forcier, M.W. Unemployment and alcohol abuse: A review. J. Occup. Med. 1988, 30, 246–251. [Google Scholar] [PubMed]
- Winton, M.; Heather, N.; Robertson, I. Effects of unemployment on drinking behavior: A review of the relevant evidence. Int. J. Addict. 1986, 21, 1261–1283. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Scherbaum, N.; Specka, M.; Kaspar, C.; Mikoteit, T.; Lieb, B. [Unemployment and Addiction: The SUNRISE Project]. Gesundheitswesen 2018, 80, 73–78. [Google Scholar]
- Jonsson, J.; Muntaner, C.; Bodin, T.; Alderling, M.; Rebeka, R.; Burstrom, B.; Davis, L.; Gunn, V.; Hemmingsson, T.; Julia, M.; et al. Low-quality employment trajectories and risk of common mental disorders, substance use disorders and suicide attempt: A longitudinal study of the Swedish workforce. Scand. J. Work. Environ. Health 2021, 47, 509–520. [Google Scholar] [CrossRef]
- Hollederer, A.; Voigtlander, S. [Health of the unemployed and its effects on labour market integration: Results of the Labour Market and Social Security (PASS) panel study, waves 3 to 7 (2008/09-2013)]. Bundesgesundheitsblatt Gesundh. Gesundh. 2016, 59, 652–661. [Google Scholar] [CrossRef]
- Compton, W.M.; Gfroerer, J.; Conway, K.P.; Finger, M.S. Unemployment and substance outcomes in the United States 2002–2010. Drug. Alcohol. Depend. 2014, 142, 350–353. [Google Scholar] [CrossRef]
- Ayllon, S.; Ferreira-Batista, N.N. Unemployment, drugs and attitudes among European youth. J. Health Econ. 2018, 57, 236–248. [Google Scholar] [CrossRef]
- Schunck, R.; Rogge, B.G. No causal effect of unemployment on smoking? A German panel study. Int. J. Public Health 2012, 57, 867–874. [Google Scholar] [CrossRef]
- Grafova, I.B.; Monheit, A.C. How does actual unemployment and the perceived risk of joblessness affect smoking behavior? Gender and intra-family effects. Rev. Econ. Househ. 2019, 17, 201–227. [Google Scholar] [CrossRef]
- Teixido-Compano, E.; Espelt, A.; Sordo, L.; Bravo, M.J.; Sarasa-Renedo, A.; Indave, B.I.; Bosque-Prous, M.; Brugal, M.T. Differences between men and women in substance use: The role of educational level and employment status. Gac. Sanit. 2018, 32, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Mulia, N.; Zemore, S.E.; Murphy, R.; Liu, H.; Catalano, R. Economic loss and alcohol consumption and problems during the 2008 to 2009 U.S. recession. Alcohol. Clin. Exp. Res. 2014, 38, 1026–1034. [Google Scholar] [CrossRef] [PubMed]
- Mangot-Sala, L.; Smidt, N.; Liefbroer, A.C. The association between unemployment trajectories and alcohol consumption patterns. Evidence from a large prospective cohort in The Netherlands. Adv. Life Course Res. 2021, 50, 100434. [Google Scholar] [PubMed]
- Robins, L.N.; Wing, J.; Wittchen, H.U.; Helzer, J.E.; Babor, T.F.; Burke, J.; Farmer, A.; Jablenski, A.; Pickens, R.; Regier, D.A.; et al. The Composite International Diagnostic Interview. An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch. Gen. Psychiatry 1988, 45, 1069–1077. [Google Scholar] [CrossRef]
- Robins, L.N.; Helzer, J.E.; Croughan, J.; Ratcliff, K.S. National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Arch. Gen. Psychiatry 1981, 38, 381–389. [Google Scholar] [CrossRef]
- First, M.B.; Spitzer, R.L.; Gibbon, M.; Williams, J.B.W. The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-IP); American Psychiatric Press: Washington, DC, USA, 1995. [Google Scholar]
- Okechukwu, C.A.; Molino, J.; Soh, Y. Associations Between Marijuana Use and Involuntary Job Loss in the United States: Representative Longitudinal and Cross-Sectional Samples. J. Occup. Environ. Med. 2019, 61, 21–28. [Google Scholar] [CrossRef]
- Bosque-Prous, M.; Espelt, A.; Sordo, L.; Guitart, A.M.; Brugal, M.T.; Bravo, M.J. Job Loss, Unemployment and the Incidence of Hazardous Drinking during the Late 2000s Recession in Europe among Adults Aged 50–64 Years. PLoS ONE 2015, 10, e0140017. [Google Scholar] [CrossRef]
- Casal, B.; Storti, C.C.; Morgan, D. Expenditure on the treatment of drug and alcohol disorders in hospitals: How much and what explain it? Int. J. Drug. Policy 2020, 79, 102750. [Google Scholar] [CrossRef]
- De Sio, S.; Tittarelli, R.; Di Martino, G.; Buomprisco, G.; Perri, R.; Bruno, G.; Pantano, F.; Mannocchi, G.; Marinelli, E.; Cedrone, F. Alcohol consumption and employment: A cross-sectional study of office workers and unemployed people. PeerJ 2020, 8, e8774. [Google Scholar] [CrossRef]
- Paljarvi, T.; Martikainen, P.; Leinonen, T.; Pensola, T.; Makela, P. Non-employment histories of middle-aged men and women who died from alcohol-related causes: A longitudinal retrospective study. PLoS ONE 2014, 9, e98620. [Google Scholar] [CrossRef]
- Miguel, A.Q.C.; Kiluk, B.D.; Roos, C.R.; Babuscio, T.A.; Nich, C.; Mari, J.J.; Carroll, K.M. Change in employment status and cocaine use treatment outcomes: A secondary analysis across six clinical trials. J. Subst. Abuse Treat. 2019, 106, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Weber, E.; Blackstone, K.; Iudicello, J.E.; Morgan, E.E.; Grant, I.; Moore, D.J.; Woods, S.P.; Translational Methamphetamine, A.R.C.G. Neurocognitive deficits are associated with unemployment in chronic methamphetamine users. Drug. Alcohol. Depend. 2012, 125, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Green, M.J.; Maddock, J.; Di Gessa, G.; Wielgoszewska, B.; Parsons, S.; Griffith, G.J.; Croft, J.; Stevenson, A.J.; Huggins, C.F.; Booth, C.; et al. The UK Coronavirus Job Retention Scheme and smoking, alcohol consumption and vaping during the COVID-19 pandemic: Evidence from eight longitudinal population surveys. BMC Med. 2022, 20, 345. [Google Scholar] [CrossRef] [PubMed]
- Haddad, R.E.; Matta, J.; Lemogne, C.; Melchior, M.; Zins, M.; Airagnes, G. The association between substance use and subsequent employment among students: Prospective findings from the CONSTANCES cohort. Soc. Psychiatry Psychiatr. Epidemiol. 2023, 58, 249–266. [Google Scholar] [CrossRef]
- Egan, K.K.; Jorgensen, M.B.; Christensen, A.I.; Bramming, M.; Lau, C.J.; Becker, U.; Tolstrup, J.S. Association between alcohol, socioeconomic position and labour market participation: A prospective cohort study of transitions between work and unemployment. Scand. J. Public. Health 2021, 49, 197–205. [Google Scholar] [CrossRef]
- Azagba, S.; Shan, L.; Qeadan, F.; Wolfson, M. Unemployment rate, opioids misuse and other substance abuse: Quasi-experimental evidence from treatment admissions data. BMC Psychiatry 2021, 21, 22. [Google Scholar] [CrossRef]
- Vandoros, S.; Gong, X.; Kawachi, I. The link between unemployment and opioid prescribing. An instrumental variable approach using evidence from England. J. Epidemiol. Community Health 2021, 75, 357–364. [Google Scholar]
- Swift, S.L.; Elfassy, T.; Bailey, Z.; Florez, H.; Feaster, D.J.; Calonico, S.; Sidney, S.; Kiefe, C.I.; Zeki Al Hazzouri, A. Association of negative financial shocks during the Great Recession with depressive symptoms and substance use in the USA: The CARDIA study. J. Epidemiol. Community Health 2020, 74, 995–1001. [Google Scholar] [CrossRef]
- Jorgensen, M.B.; Pedersen, J.; Thygesen, L.C.; Lau, C.J.; Christensen, A.I.; Becker, U.; Tolstrup, J.S. Alcohol consumption and labour market participation: A prospective cohort study of transitions between work, unemployment, sickness absence, and social benefits. Eur. J. Epidemiol. 2019, 34, 397–407. [Google Scholar] [CrossRef]
- Airagnes, G.; Lemogne, C.; Meneton, P.; Plessz, M.; Goldberg, M.; Hoertel, N.; Roquelaure, Y.; Limosin, F.; Zins, M. Alcohol, tobacco and cannabis use are associated with job loss at follow-up: Findings from the CONSTANCES cohort. PLoS ONE 2019, 14, e0222361. [Google Scholar] [CrossRef]
- de Goeij, M.C.M.; Bruggink, J.W.; Otten, F.; Kunst, A.E. Harmful drinking after job loss: A stronger association during the post-2008 economic crisis? Int. J. Public. Health 2017, 62, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.O.; Hill, K.G.; Hartigan, L.A.; Boden, J.M.; Guttmannova, K.; Kosterman, R.; Bailey, J.A.; Catalano, R.F. Unemployment and substance use problems among young adults: Does childhood low socioeconomic status exacerbate the effect? Soc. Sci. Med. 2015, 143, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Chintakrindi, S.; Porter, J.; Kim, C.; Gupta, S. An Examination of Employment and Earning Outcomes of Probationers With Criminal and Substance Use Histories. SAGE Open. 2015, 5, 12. [Google Scholar] [CrossRef]
- Brook, J.S.; Zhang, C.; Burke, L.; Brook, D.W. Trajectories of cigarette smoking from adolescence to adulthood as predictors of unemployment status. Nicotine Tob. Res. 2014, 16, 1559–1566. [Google Scholar] [CrossRef]
- Baldwin, M.L.; Marcus, S.C. The impact of mental and substance-use disorders on employment transitions. Health Econ. 2014, 23, 332–344. [Google Scholar] [CrossRef]
- Arria, A.M.; Garnier-Dykstra, L.M.; Cook, E.T.; Caldeira, K.M.; Vincent, K.B.; Baron, R.A.; O’Grady, K.E. Drug use patterns in young adulthood and post-college employment. Drug. Alcohol. Depend. 2013, 127, 23–30. [Google Scholar] [CrossRef]
- Deb, P.; Gallo, W.T.; Ayyagari, P.; Fletcher, J.M.; Sindelar, J.L. The effect of job loss on overweight and drinking. J. Health Econ. 2011, 30, 317–327. [Google Scholar] [CrossRef]
- Davalos, M.E.; Fang, H.; French, M.T. Easing the pain of an economic downturn: Macroeconomic conditions and excessive alcohol consumption. Health Econ. 2012, 21, 1318–1335. [Google Scholar] [CrossRef]
- Harwood, H.J.; Fountain, D.; Fountain, G. Economic cost of alcohol and drug abuse in the United States, 1992: A report. Addiction 1999, 94, 631–635. [Google Scholar]
- Rehm, J.; Parry, C.D. Alcohol consumption and infectious diseases in South Africa. Lancet 2009, 374, 2053. [Google Scholar] [CrossRef]
- Nagelhout, G.E.; Hummel, K.; de Goeij, M.C.M.; de Vries, H.; Kaner, E.; Lemmens, P. How economic recessions and unemployment affect illegal drug use: A systematic realist literature review. Int. J. Drug. Policy 2017, 44, 69–83. [Google Scholar] [CrossRef] [PubMed]
- Alonso, J.; Angermeyer, M.C.; Bernert, S.; Bruffaerts, R.; Brugha, T.S.; Bryson, H.; de Girolamo, G.; Graaf, R.; Demyttenaere, K.; Gasquet, I.; et al. Prevalence of mental disorders in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr. Scand. Suppl. 2004, 21–27. [Google Scholar]
- Hall, W.; Teesson, M.; Lynskey, M.; Degenhardt, L. The 12-month prevalence of substance use and ICD-10 substance use disorders in Australian adults: Findings from the National Survey of Mental Health and Well-Being. Addiction 1999, 94, 1541–1550. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, R.; Bebbington, P.; Brugha, T.; Farrell, M.; Lewis, G.; Meltzer, H. British Psychiatric Morbidity Survey. Int. Rev. Psychiatry 2003, 15, 14–18. [Google Scholar] [CrossRef] [PubMed]
- OAS Office of Applied Studies, Substance Abuse and Mental Health Services Administration (SAMHSA). Results from the 2002–2004 National Survey on Drug Use and Health (NSDUH); OAS: Rockville, MD, USA, 2005. [Google Scholar]
- Sandwijk, J.; Cohen, P.; Langemeijer, M. Licit and Illicit Drug Use in Amsterdam. Report of a Household Survey in 1994 on the Prevalence of Drug Use among the Population of 12 Years and Over; Amsterdam Instituut voor Sociale Geografie, Universiteit Amsterdam: Amsterdam, The Netherlands, 1995. [Google Scholar]
- Benkert, O.; Hippius, H. Kompendium der Psychiatrischen Pharmakotherapie, 13th ed.; Springer: Heidelberg, Germany, 2021. [Google Scholar]
- Berger, M. Psychische Erkrankungen, 6th ed.; Elsevier: Munich, Germany, 2018. [Google Scholar]
- Goffman, E. Stigma. Notes on the Management of Spoiled Identity; Printice Hall: Englewood Cliffs, NJ, USA, 1963. [Google Scholar]
- Baldwin, M.L.; Marcus, S.C.; De Simone, J. Job loss discrimination and former substance use disorders. Drug. Alcohol. Depend. 2010, 110, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Csete, J.; Kamarulzaman, A.; Kazatchkine, M.; Altice, F.; Balicki, M.; Buxton, J.; Cepeda, J.; Comfort, M.; Goosby, E.; Goulao, J.; et al. Public health and international drug policy. Lancet 2016, 387, 1427–1480. [Google Scholar] [CrossRef] [PubMed]
- Golichenko, M.; Chu, S.K.H. Human rights in patient care: Drug treatment and punishment in Russia. Public. Health Rev. 2018, 39, 12. [Google Scholar] [CrossRef]
- Sander, G. State sanctioned killing in the name of drugs: Laws, practice and conflicting trends in Asia. Int. J. Drug. Policy 2021, 92, 103266. [Google Scholar] [CrossRef]
- Rehm, J.; Mathers, C.; Popova, S.; Thavorncharoensap, M.; Teerawattananon, Y.; Patra, J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 2009, 373, 2223–2233. [Google Scholar] [CrossRef]
- Mijares, J.C. Drug Use, Health and Labor Market Outcomes; Faculty of the Department of Economics, University of Houston: Houston, TX, USA, 2003. [Google Scholar]
- Paul, K.; Moser, K. Unemployment impairs mental health: Metaanalyses. J. Vocat. Behav. 2009, 74, 264–282. [Google Scholar] [CrossRef]
- Paul, K.I.; Geithner, E.; Moser, K. Latent deprivation among people who are employed, unemployed, or out of the labor force. J. Psychol. 2009, 143, 477–491. [Google Scholar] [CrossRef] [PubMed]
- Dunham, H.W. Theories and hypotheses in social psychiatry: An analysis of the evidence. Proc. Annu. Meet. Am. Psychopathol. Assoc. 1968, 57, 220–251. [Google Scholar] [PubMed]
- Dunham, H.W. Society, culture, and mental disorder. Arch. Gen. Psychiatry 1976, 33, 147–156. [Google Scholar] [CrossRef]
- Ettner, S.L. Measuring the human costs of a weak economy: Does unemployment lead to alcohol abuse? Soc. Sci. Med. 1997, 44, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Green, K.M.; Doherty, E.E.; Reisinger, H.S.; Chilcoat, H.D.; Ensminger, M. Social integration in young adulthood and the subsequent onset of substance use and disorders among a community population of urban African Americans. Addiction 2010, 105, 484–493. [Google Scholar] [CrossRef] [PubMed]
- Puls, R.; Mümken, S. Zum Einfluss der Arbeitsplatzsicherheit auf den Alkohol-, Tabak- und Medikamentenkonsum: Stand der internationalen Forschung [The effects of job insecurity on the consumption of alcohol, tobacco and prescription drugs: A review of the international literature]. In Arbeitslosigkeit und Sucht. Ein Handbuch für Wissenschaft und Praxis [Unemployment and addiction. A Handbook for Research and Practice]; Henkel, D., Zemlin, U., Eds.; Fachhochschulverlag: Frankfurt am Main, Germany, 2008; pp. 70–91. [Google Scholar]
- Catalano, R.; Dooley, D.; Wilson, G.; Hough, R. Job loss and alcohol abuse: A test using data from the Epidemiologic Catchment Area project. J. Health Soc. Behav. 1993, 34, 215–225. [Google Scholar] [CrossRef]
- Henkel, D.; Dornbusch, P.; Zemlin, U. Predictors of alcohol relapses among the unemployed 6 months after treatment: Empirical results and conclusions for treatment and rehabilitation programs. Suchttherapie 2005, 6, 165–175. [Google Scholar] [CrossRef]
- European Monitoring Centre for Drugs and Drug Addiction. EMCDDA-Data. Lisboa, 27 October 2010. Available online: www.emcdda.europa.eu (accessed on 28 January 2023).
- Adamson, S.J.; Sellman, J.D.; Frampton, C.M. Patient predictors of alcohol treatment outcome: A systematic review. J. Subst. Abuse Treat. 2009, 36, 75–86. [Google Scholar] [CrossRef]
- Brewer, D.D.; Catalano, R.F.; Haggerty, K.; Gainey, R.R.; Fleming, C.B. A meta-analysis of predictors of continued drug use during and after treatment for opiate addiction. Addiction 1998, 93, 73–92. [Google Scholar] [CrossRef]
- Eisenberg, M.J.; Filion, K.B.; Yavin, D.; Belisle, P.; Mottillo, S.; Joseph, L.; Gervais, A.; O’Loughlin, J.; Paradis, G.; Rinfret, S.; et al. Pharmacotherapies for smoking cessation: A meta-analysis of randomized controlled trials. CMAJ 2008, 179, 135–144. [Google Scholar] [CrossRef]
- Ranney, L.; Melvin, C.; Lux, L.; McClain, E.; Lohr, K.N. Systematic review: Smoking cessation intervention strategies for adults and adults in special populations. Ann. Intern. Med. 2006, 145, 845–856. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.D.; Wilken, L.A.; Winkler, S.R.; Lin, S.J. Systematic review and meta-analysis of combination therapy for smoking cessation. J. Am. Pharm. Assoc. 2008, 48, 659–665. [Google Scholar] [CrossRef] [PubMed]
- Paavola, M.; Vartiainen, E.; Puska, P. Smoking cessation between teenage years and adulthood. Health Educ. Res. 2001, 16, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Rose, J.S.; Chassin, L.; Presson, C.C.; Sherman, S.J. Prospective predictors of quit attempts and smoking cessation in young adults. Health Psychol. 1996, 15, 261–268. [Google Scholar] [CrossRef]
- Weden, M.M.; Astone, N.M.; Bishai, D. Racial, ethnic, and gender differences in smoking cessation associated with employment and joblessness through young adulthood in the US. Soc. Sci. Med. 2006, 62, 303–316. [Google Scholar] [CrossRef]
- Forbes, J.F.; McGregor, A. Unemployment and mortality in post-war Scotland. J. Health Econ. 1984, 3, 239–257. [Google Scholar] [CrossRef]
- McAvinchey, I.D. A comparison of unemployment, income and mortality interaction for five European countries. Appl. Econ. 1988, 20, 453–471. [Google Scholar] [CrossRef]
- Ruhm, C.J. Economic conditions and alcohol problems. J. Health Econ. 1995, 14, 583–603. [Google Scholar] [CrossRef]
- Freeman, D.G. A note on ‘Economic conditions and alcohol problems’. J. Health Econ. 1999, 18, 661–670. [Google Scholar] [CrossRef]
- Dee, T.S. Alcohol abuse and economic conditions: Evidence from repeated cross-sections of individual-level data. Health Econ. 2001, 10, 257–270. [Google Scholar] [CrossRef]
- Ruhm, C.J. Are recessions good for your health? Quart. J. Econ. 2000, 115, 617–650. [Google Scholar] [CrossRef]
- Andrews, G.; Henderson, S.; Hall, W. Prevalence, comorbidity, disability and service utilisation. Overview of the Australian National Mental Health Survey. Br. J. Psychiatry 2001, 178, 145–153. [Google Scholar] [CrossRef]
- Fryers, T.; Melzer, D.; Jenkins, R. Social inequalities and the common mental disorders: A systematic review of the evidence. Soc. Psychiatry Psychiatr. Epidemiol. 2003, 38, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Jacobi, F.; Wittchen, H.U.; Holting, C.; Hofler, M.; Pfister, H.; Muller, N.; Lieb, R. Prevalence, co-morbidity and correlates of mental disorders in the general population: Results from the German Health Interview and Examination Survey (GHS). Psychol. Med. 2004, 34, 597–611. [Google Scholar] [CrossRef] [PubMed]
| Data Source, N, Age | Authors | Substance-Use Variables | Labor Market Outcomes | Effects |
|---|---|---|---|---|
| France, CONSTANCES 2012/2018, 1427, 18–69 | El Haddad et al., 2022 [46] | Tobacco and cannabis use, alcohol frequency of use and dependence | Unemployment/ Employment | Tobacco and risky alcohol use do not significantly affect employment unlike weekly use of cannabis (OR 1.73) and alcohol dependence (OR 1.65). |
| Denmark, DNHS, 2010, 84,474, 18–60 | Egan, K. et al., 2021 [47] | Median alcohol consumption, problem drinking, current smoker | Unemployment/ Employment | People who drink more alcohol up to problem drinking are more likely affected to become unemployed. |
| Spain, EDADES, 2007/2013, 22,862, 15–64 | Casal, B. et al., 2020 [40] | Consumption of cannabis, cocaine and both of them | Unemployment/ Employment | Cannabis and cocaine use has an higher impact on unemployment, especially in economic recession. |
| Denmark, DNHS, 2010, 86,417, 18–60 | Bæksgaard Jørgensen, M. et al., 2019 [51] | Median alcohol consumption, problem drinking, current smoker | Unemployment/ Employment | People who drink more alcohol up to problem drinking are more likely affected to become unemployed; moreover, they have a lower chance to return to work. |
| France, CONSTANCES, 2012–2016, 18,879, 18–69 | Airagnes, G. et al., 2019 [52] | Consumption of alcohol, tobacco and cannabis | Unemployment/ Employment | All the substance-use variables show correlation with short-term unemployment. |
| Germany, SUNRISE, 2021, 87, 24–54 | Scherbaum, N. et al., 2018 [25] | Abuse/addiction of alcohol, opioids, cannabis, sedatives, hypnotics, cocaine and stimulants; hallucinogen abuse; polydrugmania | Unemployment | On average, 11 years after the start of substance use, the majority of participants become unemployed. |
| USA, NESARC, 2001–2004/2012–2013, 23,446/23,346, ≥18 | Okechukwu, C. et al., 2018 [38] | Past year marijuana use and use disorder, lifetime alcohol and drug disorder | Unemployment/ Employment | Past year marijuana use increases the risk of job loss by 50%, especially with daily use. |
| USA, FTDO, 1992–1994, n.a., n.a. | Chintakrindi, S. et al., 2015 [55] | Drug use prior to arrest (alcohol, marijuana, uppers, cocaine, crack, heroin, any drugs) | Unemployment/ Employment | Substance use is negatively associated with employment. |
| Finland, SF, 2000–2007, 204,422, 45–64 | Paljärvi, T. et al., 2014 [42] | Alcohol-related death in relation to average annual number of days | Unemployment/ Employment | In total, 56% of alcohol-related deaths concern people who were employed ten years prior death; and this about two years less in comparison to people who died of other reasons and five years less in comparison to people who did not die. |
| USA, n.a. 1983/1985–1986/1992/1997/2002/2007/2012–2013, 528, ∅43 | Brook, J. et al., 2014 [56] | Heavy/continuous smokers, late starters, occasional smokers, quitters/decreasers | Unemployment/ Employment | Continuous and occasional smoker tend to become unemployed in later years. |
| USA, CLS, 2004–2005, 620, 17–19 | Arria, A. et al., 2013 [58] | Alcohol consumption, drug use (infrequent marijuana use, sporadic and persistent drug use) | Unemployment/ Employment | Young adults with drug use over persistent time might have higher risk of unemployment after college. |
| USA, HRS, 1992–2008, 20,557, ≥50 | Deb, P. et al., 2012 [59] | Daily number of drinks | Unemployment/ Employment | People who show risky health patterns are particularly vulnerable for high rates of daily number of drinks in unemployment. |
| USA, n.a., n.a., 110, n.a. | Weber, E. et al., 2012 [44] | MA use characteristics (age of first use, total duration and quantity of use, last use, injection use) Non-MA dependence (cannabis, alcohol, cocaine, other substances) | Unemployment/ Employment | Neurocognitive deficits by methamphetamine use are associated with higher rates of unemployment. |
| Data Source, N, Age | Authors | Outcome Measures | Effects |
|---|---|---|---|
| U.K., MCS/ALSPAC/NS/BCS70/NCDS/USOC/ELSA/GS, 2020, 27,841, 16–66 | Green, M. et al., 2022 [45] | Current smoking, vaping, and drinking among furloughed, no longer employed and stable unemployed people | Only correlation between stable unemployment women and smoking (ARR * = 1.35) as well as no longer employed women and vaping (ARR = 2.74). |
| Netherlands, DLCS, 2006–2013, 45,967, 25–50 | Mangot-Sala, L. et al., 2021 [34] | Abstainers, moderate/heavy/binge drinking | Only correlation between long-term unemployment and heavy as well as binge drinking. Moreover, some short-term unemployed individuals are more likely to become abstinent. |
| USA, TEDS, 1993–2016, n.a., age ≥ 18 | Azagba, S. et al., 2021 [48] | Treatment admissions for primary substance abuse (opiates, cocaine, alcohol, marijuana, other drugs, stimulants) | For every unit of rising unemployment rate, opiate treatment admissions increase by 9%. Other substances are associated with similar results; only stimulants show negative correlation. |
| Sweden, SWIP, 2005–2017, 2,743,764, 18–61 | Jonsson, J. et al., 2021 [26] | Substance abuse | Unemployment is associated with higher risk of developing substance abuse (HR ** = 1.05–2.19). |
| England, GP, 2011–2017, 8736, n.a. | Vandoros, S. et al., 2020 [49] | Opioid prescribing | For every percentage point of rising unemployment rate, defined daily dose of opioid per capita increase by 0.017 (0.9% compared to the average). |
| USA, CARDIA, 2005–2010, 1307, n.a. | Swift, S. et al., 2020 [50] | Binge drinking, past 30-day drug use | Negative employment changes are associated with decreasing binge drinking, but increasing drug use in the past 30 days. |
| Italy, n.a., 2019, 314, n.a. | De Sio, S. et al., 2020 [41] | Alcohol-related biomarkers (carbohydrate-deficient transferrin, aspartate transaminase, alanine transaminase, γ-glutamyltransferase, mean corpuscular volume) | Office worker show lower rates in alcohol-related biomarkers then unemployed people. |
| USA, n.a., n.a., 553, ≥18 | Miguel, A. et al., 2019 [43] | History of cocaine use and substance abuse treatment, concomitant psychiatric (alcohol-use) disorders | Stable unemployment during treatment of cocaine use is associated with negative outcomes. In contrast, being employed during treatment is associated with better outcomes. |
| Spain, EDADES, 2013, 14,113, 25–64 | Teixidó-Compañó, E. et al., 2018 [32] | Hazardous drinking, heavy cannabis use, hypnosedative consumption | Unemployed people, no matter if male or female, show higher rates of cannabis and hypnosedative use, whereas unemployed women show less rates in alcohol drinking. |
| Netherlands, HIS, 2004–2013, 26,355, 30–64 | De Goeij, M. et al., 2017 [53] | Episodic drinking before and during 2008 economic crisis | Job loss during economic crisis is only associated with chronic (OR 1.43/OR 1.42), but not with episodic drinking. |
| USA, PSID, 1999–2011, 41,231, n.a. | Grafova, I. et al., 2017 [31] | Current and former smoker, smoking relapse, increased and decreased cigarette consumption, quit smoking | Unemployment initially decreases the risk of cigarette consumption and its relapse in men, but not in long term. |
| Spain, Flash EB 401, 2011/2014, n.a., 15–24 | Ayllón, S. et al., 2017 [29] | Consumption of cannabis and new substances | For 1% of rising unemployment rate, consumption of cannabis at any point in time among young people increases by 0.7%. |
| Germany, SUF, 2016, 8951, 15–64 | Hollederer, A. et al., 2016 [27] | Consumption of beer, wine, alcoholic mixed drinks, spirits, and nicotine | Twice as high rate of unemployed smokers as employed smokers; but alcohol consumption rates are higher in employed people. |
| AT/BE/CZ/DK/FR/ DE/IT/NL/ES/SE/CH ***, SHARE, 2006–2012, 7615, 50–64 | Bosque-Prous, M. et al., 2015 [39] | Hazardous drinking | Increasing unemployment rate leads to increasing rates of hazardous drinking by 32%. |
| USA, SSDP, n.a., n.a., 22–33 | Lee, J. et al., 2015 [54] | Heavy episodic drinking, daily cigarette smoking, and marijuana use | Unemployment among young adults is associated with heavy episodic drinking. This does not apply to marijuana use and just possibly to daily cigarette smoking. |
| USA, NSDUH, 2002–2004/2005- 2007/2008/2009- 2010, ~405,000, ≥18 | Compton, W. et al., 2014 [28] | Heavy alcohol, illicit drug and tobacco use; alcohol and illicit drug abuse or dependence | Unemployed people tend to higher rates in all mentioned outcome measures; also during economic crisis. |
| USA, NAS12, 2009–2010, 5382, ≥18 | Mulia, N. et al., 2014 [33] | Alcohol-related health problems prior to recession | Job loss is associated with higher risk of alcohol-related health problems in men, especially drunkenness, its consequences and alcohol dependence. |
| USA, NESARC, 2001–2002/2004–2005, n.a., 19–60 | Baldwin, M. et al., 2013 [57] | Alcohol and drug disorder | Unemployed people with alcohol disorder in wave I have a 3.7 respectively 8.8 percentage point higher chance of finding part-time respectively full-time work in wave II. Part-time employed people with alcohol disorder in wave I have a 6.1 percentage point higher chance of continuing in their work in wave II while those with drug disorder have a 13.8 percentage point lower chance of this work in wave II. |
| Germany, SOEP, 1998–2009, 52,940, 17–65 | Schunck, R. et al., 2012 [30] | Smoking and number of cigarettes per day | Unemployment increases the risk of smoking, but not its intensity. |
| USA, NESARC, 2001–2002/2004–2005, 34,120, ≥18 | Dávalos, M. et al., 2011 | Alcohol consumption (binge drinking and its number of days, driving after too much to drink, abuse/dependence) | Unemployment is associated with rising alcoholic (binge) drinking events as well as its abuse/dependence. |
| Data Source, N, Age | Authors | Outcome Measures | Effects |
|---|---|---|---|
| U.K., MCS/ALSPAC/NS/BCS70/NCDS/USOC/ELSA/GS, 2020, 27,841, 16–66 | Green, M. et al., 2022 [45] | Smoking/vaping more–incl. relapse and initiation | In five out of seven surveys, unemployed participants tend to higher rates of smoking (incl. relapse and initiation) while in five out of six surveys, they tend to more vaping (incl. relapse and initiation). |
| USA, PSID, 1999–2011, 41,231, n.a. | Grafova, I. et al., 2017 [31] | Smoking relapse | In total, 10% of the unemployed participants who smoked in the past relapse until the second wave. |
| Germany, SOEP, 1998–2009, 52,940, 17–65 | Schunck, R. et al., 2012 [30] | Smoking and number of cigarettes per day | Unemployed people do not seem to show changes in smoking relapse. |
| Data Source, N, Age | Authors | Outcome Measures | Effects |
|---|---|---|---|
| UK, MCS/ALSPAC/NS/BCS70/NCDS/USOC/ELSA/GS, 2020, 27,841, 16–66 | Green, M. et al., 2022 [45] | Smoking/vaping less–incl. cessation | In two out of seven surveys, unemployed participants tend to lower rates of smoking (incl. cessation) while in one out of six surveys, they tend to less vaping (incl. cessation). |
| USA, PSID, 1999–2011, 41,231, n.a. | Grafova, I. et al., 2017 [31] | Quit smoking | A total of 1/5 of the unemployed participants who smoked in the past quit smoking until the second wave. |
| USA, n.a. 1983/1985–1986/ 1992/1997/2002/ 2007/2012–2013, 528, ∅43 | Brook, J. et al., 2014 [56] | Smoking quitters | Regarding unemployment, there seem to be no differences between smoking quitters and those who do not smoke. |
| Germany, SOEP, 1998–2009, 52,940, 17–65 | Schunck, R. et al., 2012 [30] | Smoking and number of cigarettes per day | Unemployed people do not seem to show changes in smoking cessation. |
| Data Source, N, Age | Authors | Dependent Variables | Effects |
|---|---|---|---|
| USA, TEDS, 1993–2016, n.a., ≥18 | Azagba, S. et al., 2021 [48] | Treatment admissions for primary substance abuse (opiates, cocaine, alcohol, marijuana, other drugs, stimulants) | Correlation between unemployment rates and annual substance abuse admissions has the same causal direction during economic crisis and during times without crisis. |
| Spain, EDADES, 2007/2013, 23,258/22,862, 16–64 | Casal, B. et al., 2020 [40] | Consumption of cannabis, cocaine, and both of them | Cannabis and cocaine use have an higher impact on unemployment especially in economic recessions. |
| Netherlands, HIS, 2004–2013, 26,355, 30–64 | De Goeij, M. et al., 2017 [53] | Episodic drinking before and during 2008 economic crisis | Job loss during economic crisis is associated with chronic alcohol use but not with episodic drinking. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nolte-Troha, C.; Roser, P.; Henkel, D.; Scherbaum, N.; Koller, G.; Franke, A.G. Unemployment and Substance Use: An Updated Review of Studies from North America and Europe. Healthcare 2023, 11, 1182. https://doi.org/10.3390/healthcare11081182
Nolte-Troha C, Roser P, Henkel D, Scherbaum N, Koller G, Franke AG. Unemployment and Substance Use: An Updated Review of Studies from North America and Europe. Healthcare. 2023; 11(8):1182. https://doi.org/10.3390/healthcare11081182
Chicago/Turabian StyleNolte-Troha, Carina, Patrik Roser, Dieter Henkel, Norbert Scherbaum, Gabriele Koller, and Andreas G. Franke. 2023. "Unemployment and Substance Use: An Updated Review of Studies from North America and Europe" Healthcare 11, no. 8: 1182. https://doi.org/10.3390/healthcare11081182
APA StyleNolte-Troha, C., Roser, P., Henkel, D., Scherbaum, N., Koller, G., & Franke, A. G. (2023). Unemployment and Substance Use: An Updated Review of Studies from North America and Europe. Healthcare, 11(8), 1182. https://doi.org/10.3390/healthcare11081182







