The Complexity of Burnout Experiences among Care Aides: A Person-Oriented Approach to Burnout Patterns
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Sample
2.2. Variables and Measures
2.3. Analysis
3. Results
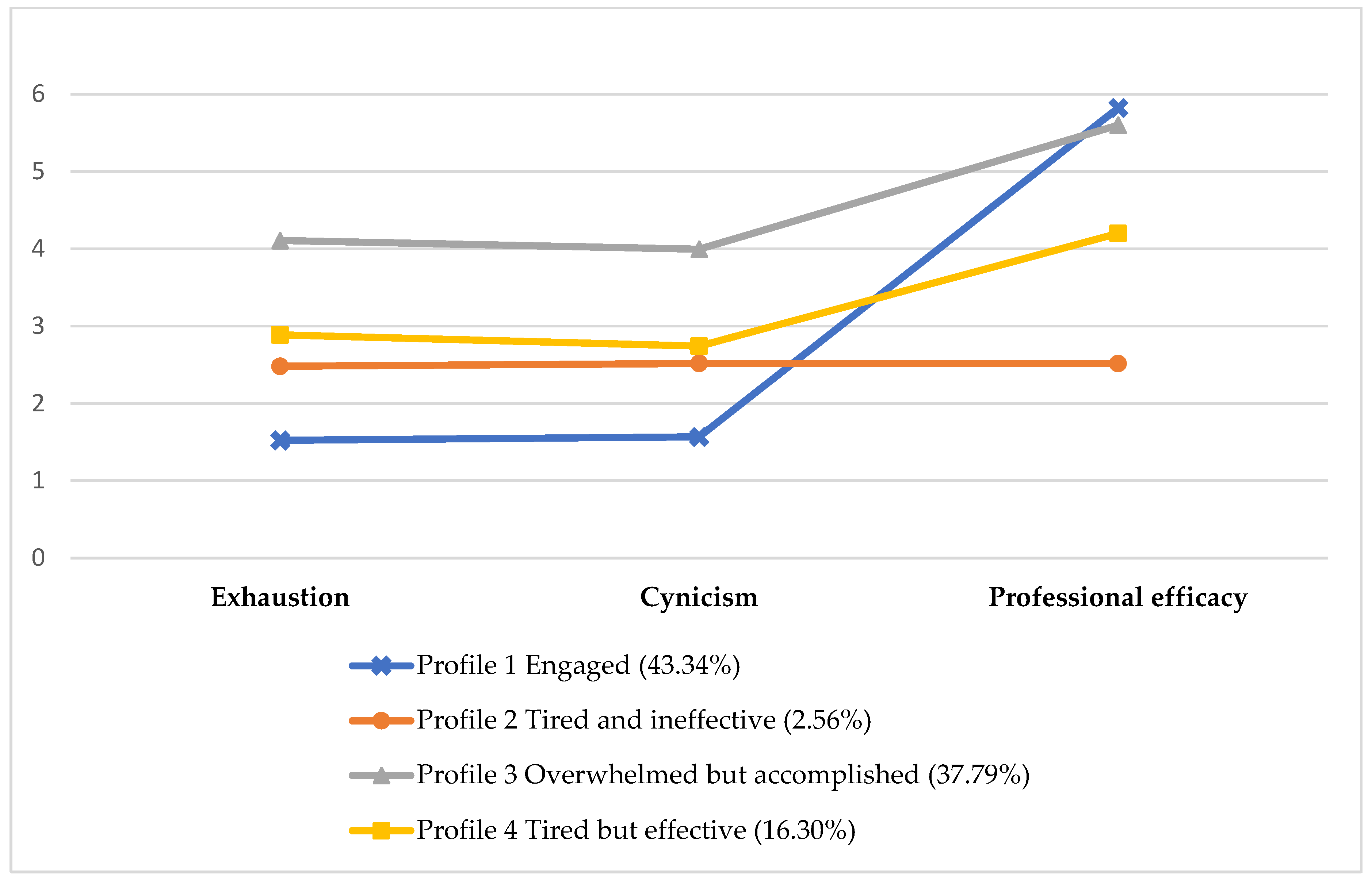
3.1. Four Burnout Patterns
3.2. Differences in Demographics and Job-Related Characteristics by Burnout Pattern
4. Discussion
4.1. Complex Relationships among Burnout Dimensions
Theoretical Implications
4.2. Associations of Burnout Patterns with Work Environment and Quality of Work-Life
Practical Implications
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chamberlain, S.A.; Hoben, M.; Squires, J.E.; Cummings, G.G.; Norton, P.; Estabrooks, C.A. Who is (still) looking after mom and dad? Few improvements in care aides’ quality-of-work life. Can. J. Aging Rev. Can. Vieil. 2019, 38, 35–50. [Google Scholar] [CrossRef] [PubMed]
- Estabrooks, C.A.; Squires, J.E.; Carleton, H.L.; Cummings, G.G.; Norton, P.G. Who is looking after Mom and Dad? Unregulated workers in Canadian long-term care homes. Can. J. Aging Rev. Can. Vieil. 2015, 34, 47–59. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Iaconi, A.; Song, Y.; Norton, P.G.; Squires, J.E.; Keefe, J.; Cummings, G.G.; Estabrooks, C.A. Care Aides Working Multiple Jobs: Considerations for Staffing Policies in Long-Term Care Homes During and after the COVID-19 Pandemic. J. Am. Med. Dir. Assoc. 2020, 21, 1390–1391. [Google Scholar] [CrossRef] [PubMed]
- Cooper, S.L.; Carleton, H.L.; Chamberlain, S.A.; Cummings, G.G.; Bambrick, W.; Estabrooks, C.A. Burnout in the nursing home health care aide: A systematic review. Burn. Res. 2016, 3, 76–87. [Google Scholar] [CrossRef]
- Maslach, C.; Schaufeli, W.B.; Leiter, M.P. Job burnout. Annu. Rev. Psychol. 2001, 52, 397–422. [Google Scholar] [CrossRef]
- Mäkikangas, A.; Kinnunen, U. The person-oriented approach to burnout: A systematic review. Burn. Res. 2016, 3, 11–23. [Google Scholar] [CrossRef]
- Chamberlain, S.A.; Gruneir, A.; Hoben, M.; Squires, J.E.; Cummings, G.G.; Estabrooks, C.A. Influence of organizational context on nursing home staff burnout: A cross-sectional survey of care aides in Western Canada. Int. J. Nurs. Stud. 2017, 71, 60–69. [Google Scholar] [CrossRef]
- Jeon, Y.H.; Luscombe, G.; Chenoweth, L.; Stein-Parbury, J.; Brodaty, H.; King, M.; Haas, M. Staff outcomes from the caring for aged dementia care resident study (CADRES): A cluster randomised trial. Int. J. Nurs. Stud. 2012, 49, 508–518. [Google Scholar] [CrossRef]
- Ramarajan, L.; Barsade, S.G.; Burack, O.R. The influence of organizational respect on emotional exhaustion in the human services. J. Posit. Psychol. 2008, 3, 4–18. [Google Scholar] [CrossRef]
- Yeatts, D.E.; Cready, C.; Swan, J.; Shen, Y. The perception of “training availability” among certified nurse aides: Relationship to CNA performance, turnover, attitudes, burnout, and empowerment. Gerontol. Geriatr. Educ. 2010, 31, 115–132. [Google Scholar] [CrossRef]
- Meyer, J.P.; Stanley, L.J.; Vandenberg, R.J. A person-centered approach to the study of commitment. Hum. Resour. Manag. Rev. 2013, 23, 190–202. [Google Scholar] [CrossRef]
- Bergman, L.R.; Magnusson, D.; El Khouri, B.M. Studying Individual Development in An Interindividual Context: A Person-Oriented Approach; Psychology Press: London, UK, 2003; Volume 4. [Google Scholar]
- Muthen, B.; Muthen, L.K. Integrating person-centered and variable-centered analyses: Growth mixture modeling with latent trajectory classes. Alcohol. Clin. Exp. Res. 2000, 24, 882–891. [Google Scholar] [CrossRef]
- Golembiewski, R.T.; Munzenrider, R.F. Phases of Burnout: Developments in Concepts and Applications; Praeger Publishers: Westport, CT, USA, 1986. [Google Scholar]
- Leiter, M.P.; Maslach, C. The impact of interpersonal environment on burnout and organizational commitment. J. Organ. Behav. 1988, 9, 297–308. [Google Scholar] [CrossRef]
- Lee, R.T.; Ashforth, B.E. A longitudinal study of burnout among supervisors and managers: Comparisons between the Leiter and Maslach (1988) and Golembiewski et al. (1986) models. Organ. Behav. Hum. Decis. Process. 1993, 54, 369–398. [Google Scholar] [CrossRef]
- Taris, T.W.; Le Blanc, P.M.; Schaufeli, W.B.; Schreurs, P.J. Are there causal relationships between the dimensions of the Maslach Burnout Inventory? A review and two longitudinal tests. Work Stress 2005, 19, 238–255. [Google Scholar] [CrossRef]
- Estabrooks, C.A.; Squires, J.E.; Cummings, G.G.; Teare, G.F.; Norton, P.G. Study protocol for the translating research in elder care (TREC): Building context—An organizational monitoring program in long-term care project (project one). Implement. Sci. 2009, 4, 52. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P.; Schaufeli, W.B.; Schwab, R.L. Maslach Burnout Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1986; Volume 21. [Google Scholar]
- Bakker, A.B.; Demerouti, E.; Schaufeli, W.B. Validation of the Maslach burnout inventory-general survey: An internet study. Anxiety Stress Coping 2002, 15, 245–260. [Google Scholar] [CrossRef]
- Schutte, N.; Toppinen, S.; Kalimo, R.; Schaufeli, W. The factorial validity of the Maslach Burnout Inventory-General Survey (MBI-GS) across occupational groups and nations. J. Occup. Organ. Psychol. 2000, 73, 53–66. [Google Scholar] [CrossRef]
- Leiter, M.P.; Schaufeli, W.B. Consistency of the burnout construct across occupations. Anxiety Stress Coping 1996, 9, 229–243. [Google Scholar] [CrossRef]
- Estabrooks, C.A.; Squires, J.E.; Hayduk, L.A.; Cummings, G.G.; Norton, P.G. Advancing the argument for validity of the Alberta Context Tool with healthcare aides in residential long-term care. BMC Med. Res. Methodol. 2011, 11, 107. [Google Scholar] [CrossRef]
- Knopp-Sihota, J.A.; Niehaus, L.; Squires, J.E.; Norton, P.G.; Estabrooks, C.A. Factors associated with rushed and missed resident care in western C anadian nursing homes: A cross-sectional survey of health care aides. J. Clin. Nurs. 2015, 24, 2815–2825. [Google Scholar] [CrossRef] [PubMed]
- Bowling, N.A.; Hammond, G.D. A meta-analytic examination of the construct validity of the Michigan Organizational Assessment Questionnaire Job Satisfaction Subscale. J. Vocat. Behav. 2008, 73, 63–77. [Google Scholar] [CrossRef]
- Spreitzer, G.M. Psychological empowerment in the workplace: Dimensions, measurement, and validation. Acad. Manag. J. 1995, 38, 1442–1465. [Google Scholar] [CrossRef]
- Ginsburg, L.; Berta, W.; Baumbusch, J.; Rohit Dass, A.; Laporte, A.; Reid, R.C.; Squires, J.; Taylor, D. Measuring work engagement, psychological empowerment, and organizational citizenship behavior among health care aides. Gerontologist 2016, 56, e1–e11. [Google Scholar] [CrossRef] [PubMed]
- Schaufeli, W.B.; Bakker, A.B.; Salanova, M. The measurement of work engagement with a short questionnaire: A cross-national study. Educ. Psychol. Meas. 2006, 66, 701–716. [Google Scholar] [CrossRef]
- Choi, J.N. Change-oriented organizational citizenship behavior: Effects of work environment characteristics and intervening psychological processes. J. Organ. Behav. Int. J. Ind. Occup. Organ. Psychol. Behav. 2007, 28, 467–484. [Google Scholar] [CrossRef]
- Ware, J.E.; Kosinski, M.; Dewey, J.E.; Gandek, B. How to Score and Interpret Single-Item Health Status Measures: A Manual for Users of the SF-8 Health Survey; QualityMetric Incorporated: Lincoln, RI, USA, 2001; Volume 15, p. 5. [Google Scholar]
- Ferguson, S.L.; Moore, E.W.G.; Hull, D.M. Finding latent groups in observed data: A primer on latent profile analysis in Mplus for applied researchers. Int. J. Behav. Dev. 2020, 44, 458–468. [Google Scholar] [CrossRef]
- Muthén, B.; Muthén, L. Mplus; Chapman and Hall/CRC: London, UK, 2017. [Google Scholar]
- Clark, S.L.; Muthén, B. Relating Latent Class Analysis Results to Variables Not Included in the Analysis. 2009. Available online: https://www.statmodel.com/download/relatinglca.pdf (accessed on 15 December 2022).
- StataCorp. Stata Statistical Software: Release 16; StataCorp LLC.: College Station, TX, USA, 2019. [Google Scholar]
- Edú-Valsania, S.; Laguía, A.; Moriano, J.A. Burnout: A review of theory and measurement. Int. J. Environ. Res. Public Health 2022, 19, 1780. [Google Scholar] [CrossRef]
- Leiter, M.P.; Maslach, C. Latent burnout profiles: A new approach to understanding the burnout experience. Burn. Res. 2016, 3, 89–100. [Google Scholar] [CrossRef]
- Schult, T.M.; Mohr, D.C.; Osatuke, K. Examining burnout profiles in relation to health and well-being in the Veterans Health Administration employee population. Stress Health 2018, 34, 490–499. [Google Scholar] [CrossRef]
- Onder, C.; Basim, N. Examination of developmental models of occupational burnout using burnout profiles of nurses. J. Adv. Nurs. 2008, 64, 514–523. [Google Scholar] [CrossRef]
- Potard, C.; Landais, C. The use of cluster analysis to identify different burnout profiles among nurses and care assistants for older adults. Geriatr. Nurs. 2021, 42, 1135–1142. [Google Scholar] [CrossRef]
- Leiter, M.P.; Maslach, C.; Burnout, E.; Friedman, H. (Eds.) Encyclopedia of Mental Health; Academic Press: Cambridge, MA, USA, 1998. [Google Scholar]
- Schaufeli, W.B.; Salanova, M. Efficacy or inefficacy, that’s the question: Burnout and work engagement, and their relationships with efficacy beliefs. Anxiety Stress Coping 2007, 20, 177–196. [Google Scholar] [CrossRef]
- Worley, J.A.; Vassar, M.; Wheeler, D.L.; Barnes, L.L. Factor structure of scores from the Maslach Burnout Inventory: A review and meta-analysis of 45 exploratory and confirmatory factor-analytic studies. Educ. Psychol. Meas. 2008, 68, 797–823. [Google Scholar] [CrossRef]
- Kim, H.; Ji, J. Factor structure and longitudinal invariance of the Maslach Burnout Inventory. Res. Soc. Work Pract. 2009, 19, 325–339. [Google Scholar] [CrossRef]
- Mäkikangas, A.; Leiter, M.P.; Kinnunen, U.; Feldt, T. Profiling development of burnout over eight years: Relation with job demands and resources. Eur. J. Work Organ. Psychol. 2021, 30, 720–731. [Google Scholar] [CrossRef]
- Consiglio, C.; Borgogni, L.; Vecchione, M.; Maslach, C. Self-efficacy, perceptions of context, and burnout: A multilevel study on nurses. Med. Lav. 2014, 105, 255–268. [Google Scholar]
- Leiter, M.P.; Maslach, C. Areas of worklife: A structured approach to organizational predictors of job burnout. In Emotional and Physiological Processes and Positive Intervention Strategies; Emerald Group Publishing Limited: Bradford, UK, 2003. [Google Scholar]
- Dall’Ora, C.; Ball, J.; Reinius, M.; Griffiths, P. Burnout in nursing: A theoretical review. Hum. Resour. Health 2020, 18, 41. [Google Scholar] [CrossRef]
- Guthier, C.; Dormann, C.; Voelkle, M.C. Reciprocal effects between job stressors and burnout: A continuous time meta-analysis of longitudinal studies. Psychol. Bull. 2020, 146, 1146. [Google Scholar] [CrossRef]
- Nunnally, J.C. Psychometric Theory; McGraw-Hill: New York, NY, USA, 1967. [Google Scholar]
- Ghahramani, S.; Lankarani, K.B.; Yousefi, M.; Heydari, K.; Shahabi, S.; Azmand, S. A systematic review and meta-analysis of burnout among healthcare workers during COVID-19. Front. Psychiatry 2021, 12, 758849. [Google Scholar] [CrossRef]
| Model | Number of Free Parameters | Log Likelihood | AIC | BIC | Sample-Size Adjusted BIC | LMR Test p-Value a | Entropy | Latent Profile Probabilities (Range) | Smallest Class % |
|---|---|---|---|---|---|---|---|---|---|
| 3 profiles | 14 | −17,738.65 | 35,505.31 | 35,592.58 | 35,548.09 | <0.001 | 0.794 | 0.90–0.91 | 13.69 |
| 4 profiles | 18 | −17,445.20 | 34,926.39 | 35,038.60 | 34,981.40 | <0.002 | 0.829 | 0.89–0.91 | 2.56 |
| 5 profiles | 22 | −17,099.82 | 34,243.63 | 34,380.77 | 34,310.87 | 0.056 | 0.875 | 0.84–0.99 | 2.43 |
| 6 profiles | 26 | −16,782.44 | 33,616.87 | 33,778.94 | 33,696.33 | 0.002 | 0.908 | 0.86–1.00 | 1.06 |
| 7 profiles | 30 | −16,762.78 | 33,585.55 | 33,772.56 | 33,677.23 | 0.012 | 0.877 | 0.87–0.99 | 2.41 |
| Profile 1 Engaged (43.24%) | Profile 2 Tired and Ineffective (2.42%) | Profile 3 Overwhelmed but Accomplished (38.54%) | Profile 4 Tired but Effective (15.80%) | F (ANOVA) | p | |
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| Exhaustion composite score b | 1.47 (1.16) | 2.53 (1.79) | 4.15 (1.07) | 2.85 (1.53) | 1253.31 | <0.001 |
| I feel tired when I get up in the morning c | 1.77 (1.82) | 2.68 (1.97) | 4.17 (1.60) | 3.26 (1.88) | 488.76 | <0.001 |
| Working all day is really a strain b | 1.36 (1.80) | 2.60 (2.20) | 4.43 (1.58) | 2.67 (2.00) | 773.74 | <0.001 |
| I feel burned out from my work b | 1.26 (1.49) | 2.30 (2.16) | 3.85 (1.70) | 2.60 (1.88) | 626.55 | <0.001 |
| Cynicism composite score b | 1.50 (1.09) | 2.55 (1.66) | 4.05 (1.15) | 2.71 (1.40) | 1185.75 | <0.001 |
| I just want to do my job and not be bothered b | 3.20 (2.56) | 3.71 (2.34) | 5.15 (1.39) | 3.85 (2.07) | 224.54 | <0.001 |
| I have become more cynical about whether my work contributes anything b | 0.66 (1.33) | 2.07 (2.14) | 3.51 (1.96) | 2.06 (1.90) | 706.27 | <0.001 |
| I have become less enthusiastic b | 0.64 (1.20) | 1.87 (1.93) | 3.49 (1.85) | 2.23 (1.84) | 810.01 | <0.001 |
| Professional efficacy composite score c | 5.82 (0.31) | 2.45 (0.61) | 5.60 (0.42) | 4.15 (0.41) | 4775.3 | <0.001 |
| In my opinion, I am good at my job c | 5.95 (0.24) | 4.59 (1.85) | 5.84 (0.41) | 5.45 (0.96) | 256.97 | <0.001 |
| I feel exhilarated when I accomplish something at work c | 5.84 (0.46) | 1.41 (1.48) | 5.54 (0.74) | 3.53 (1.77) | 1487.55 | <0.001 |
| I have accomplished many worthwhile things in this job c | 5.67 (0.69) | 1.35 (1.24) | 5.41 (0.78) | 3.46 (1.66) | 1296.43 | <0.001 |
| Profile 1 Engaged (43.24%) | Profile 2 Tired and Ineffective (2.42%) | Profile 3 Overwhelmed but Accomplished (38.54%) | Profile 4 Tired but Effective (15.80%) | Chi2 | Multiple Comparison with p < 0.008 b | |
|---|---|---|---|---|---|---|
| Freq (%) | Freq (%) | Freq (%) | Freq (%) | |||
| Age | 47.03 *** | PF 4 vs. PF 1, PF 3 | ||||
| <30 years | 111 (6.82) | 12 (13.19) | 119 (8.20) | 76 (12.77) | ||
| 30–39 years | 326 (20.02) | 17 (18.68) | 320 (22.05) | 152 (25.55) | ||
| 40–49 years | 518 (31.82) | 25 (27.47) | 455 (31.36) | 188 (31.60) | ||
| 50–59 years | 470 (28.87) | 22 (24.18) | 406 (27.98) | 121 (20.34) | ||
| > = 60 years | 203 (12.47) | 15 (16.48) | 151 (10.41) | 58 (9.75) | ||
| Female | 1452 (89.24) | 83 (91.21) | 1285 (88.62) | 539 (90.74) | 2.34 | none |
| Born outside of Canada | 1247 (76.60) | 66 (72.53) | 1160 (79.94) | 417 (70.08) | 24.05 *** | PF 4 vs. PF 1, PF 3 |
| English as a second language | 1092 (67.08) | 56 (61.54) | 1046 (72.09) | 377 (63.36) | 19.36 *** | PF 3 vs. PF 1, PF 4 |
| Working in 2 or more NHs | 389 (23.89) | 29 (32.22) | 355 (24.48) | 142 (23.87) | 3.30 | none |
| Shift worked most | 8.69 | none | ||||
| Day shift | 803 (49.32) | 40 (43.96) | 769 (53.00) | 297 (49.92) | ||
| Evening shift | 607 (37.29) | 40 (43.96) | 519 (35.77) | 215 (36.13) | ||
| Night shift | 218 (13.39) | 11 (12.09) | 163 (11.23) | 83 (13.95) | ||
| Facility Size | 6.39 | none | ||||
| Small (<80 beds) | 193 (11.86) | 5 (5.49) | 195 (13.44) | 77 (12.94) | ||
| Med (80–120 beds) | 507 (31.14) | 28 (30.77) | 448 (30.88) | 181 (30.42) | ||
| Large (>120 beds) | 928 (57) | 58 (63.74) | 808 (55.69) | 337 (56.64) | ||
| Ownership | 4.52 | none | ||||
| Public not for profit | 329 (20.21) | 16 (17.58) | 288 (19.85) | 115 (19.33) | ||
| Voluntary not for profit | 634 (38.94) | 36 (39.56) | 531 (36.6) | 242 (40.67) | ||
| Private for profit | 665 (40.85) | 39 (42.86) | 632 (43.56) | 238 (40.00) | ||
| Health Region | 62.51 *** | PF 3 vs. PF 1, PF 4 | ||||
| Alberta Health Edmonton Zone | 402 (24.69) | 28 (30.77) | 299 (20.61) | 165 (27.73) | ||
| Alberta Health Calgary Zone | 297 (18.24) | 16 (17.58) | 266 (18.33) | 117 (19.66) | ||
| British Columbia Interior Health Authority | 194 (11.92) | 9 (9.89) | 110 (7.58) | 67 (11.26) | ||
| British Columbia Fraser Health Authority | 453 (27.83) | 13 (14.29) | 446 (30.74) | 125 (21.01) | ||
| Winnipeg Regional Health Authority | 282 (17.32) | 25 (27.47) | 330 (22.74) | 121 (20.34) | ||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | F | Multiple Comparison with p < 0.008 b | |
| Years worked as a care aide | 12.27 (9.40) | 14.12 (10.53) | 11.85 (8.79) | 11.06 (7.84) | 4.50 ** | PF 4 vs. PF 1, PF 2 |
| Years worked on the current unit | 6.09 (6.34) | 7.81 (8.62) | 6.16 (6.11) | 5.96 (6.01) | 2.36 | none |
| Profile 1 Engaged (43.24%) | Profile 2 Tired and Ineffective (2.42%) | Profile 3 Overwhelmed but Accomplished (38.54%) | Profile 4 Tired but Effective (15.80%) | Multiple Comparison with p < 0.008 b | |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| Work environment | |||||
| Leadership (1–5) | 4.08 (0.55) | 3.70 (0.71) | 3.92 (0.55) | 3.86 (0.56) | PF 1 > PFs 3, 4 > PF 2 |
| Culture (1–5) | 4.19 (0.47) | 3.83 (0.60) | 4.00 (0.52) | 3.92 (0.52) | PF 1 > PF 3 > PFs 2, 4 |
| Evaluation (1–5) | 3.87 (0.59) | 3.58 (0.74) | 3.76 (0.60) | 3.63 (0.62) | PF 1 > PF 3 > PFs 2, 4 |
| Formal interactions (0–4) | 1.50 (0.78) | 1.46 (1.01) | 1.50 (0.83) | 1.40 (0.82) | PFs 1, 3 > PF 4 |
| Informal interactions (0–9) | 4.23 (1.70) | 3.62 (1.98) | 4.18 (1.74) | 3.85 (1.76) | PFs 1, 3 > PFs 2, 4 |
| Social capital (1–5) | 4.16 (0.50) | 3.80 (0.51) | 4.01 (0.50) | 3.90 (0.51) | PF 1 > PF 3 > PFs 2, 4 |
| Structural resources (0–7) | 2.80 (1.54) | 2.47 (1.78) | 2.63 (1.56) | 2.33 (1.57) | PF 1 > PF 3 > PF 4 |
| Organizational slack-space (1–5) | 3.64 (1.25) | 3.54 (1.25) | 3.51 (1.22) | 3.44 (1.20) | PF 1 > PF 3 > PF 4 |
| Organizational slack-time (1–5) | 3.65 (0.84) | 3.21 (0.99) | 3.39 (0.88) | 3.21 (0.82) | PF 1 > PF 3 > PFs 2, 4 |
| Organizational slack-staffing (1–5) | 3.10 (1.09) | 2.59 (1.16) | 2.68 (1.09) | 2.68 (1.09) | PF 1 > PFs 2, 3, 4 |
| Work-life experiences | |||||
| Responsive behaviors from residents (0–6) | 2.96 (1.71) | 3.32 (1.79) | 3.45 (1.63) | 3.34 (1.63) | PF 1 < PFs 2, 3, 4 |
| Rushed care (0–7) | 2.38 (2.63) | 3.41 (2.75) | 3.46 (2.76) | 3.34 (2.72) | PF 1 < PFs 2, 3, 4 |
| Missed care (0–10) | 1.18 (1.73) | 1.78 (2.09) | 2.03 (2.27) | 1.94 (2.17) | PF 1 < PFs 2, 3, 4 |
| Adequate job orientation (1–5) | 4.27 (0.79) | 4.02 (0.75) | 4.11 (0.82) | 4.00 (0.84) | PF 1 > PF 3 > PFs 2, 4 |
| Job satisfaction (1–5) | 4.48 (0.51) | 4.00 (0.78) | 4.09 (0.67) | 4.02 (0.69) | PF 1 > PFs 2, 3, 4 |
| Psychological empowerment | |||||
| Competence (1–5) | 4.60 (0.45) | 4.29 (0.48) | 4.48 (0.46) | 4.35 (0.48) | PF 1 > PF 3 > PFs 2, 4 |
| Meaning (1–5) | 4.67 (0.45) | 4.29 (0.58) | 4.53 (0.48) | 4.38 (0.51) | PF 1 > PF 3 > PFs 2, 4 |
| Self-determination (1–5) | 4.22 (0.65) | 3.76 (0.85) | 4.01 (0.73) | 3.80 (0.75) | PF 1 > PF 3 > PFs 2, 4 |
| Impact (1–5) | 3.86 (0.69) | 3.32 (0.83) | 3.76 (0.64) | 3.48 (0.69) | PF 1 > PF 3 > PFs 2, 4 |
| Work engagement | |||||
| Vigor (0–6) | 5.73 (0.51) | 4.49 (1.63) | 5.12 (1.02) | 4.78 (1.23) | PF 1 > PF 3 > PF 4 > PF 2 |
| Dedication (0–6) | 5.88 (0.31) | 4.86 (1.49) | 5.49 (0.77) | 5.21 (0.99) | PF 1 > PF 3 > PF 4 > PF 2 |
| Absorption (0–6) | 5.92 (0.26) | 5.26 (1.13) | 5.74 (0.49) | 5.53 (0.71) | PF 1 > PF 3 > PF 4 > PF 2 |
| Organizational citizenship behaviors (1–5) | 3.89 (0.61) | 3.58 (0.70) | 3.87 (0.55) | 3.63 (0.59) | PFs 1, 3 > PF 4 > PF 2 |
| Health status | |||||
| Physical health (0–100) | 51.37 (6.82) | 48.15 (7.96) | 46.04 (8.48) | 46.89 (8.29) | PF 1 > PFs 2, 3, 4 |
| Mental health (0–100) | 54.29 (6.78) | 49.16 (10.70) | 49.20 (9.40) | 48.94 (9.45) | PF 1 > PFs 2, 3, 4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duan, Y.; Song, Y.; Thorne, T.E.; Iaconi, A.; Norton, P.G.; Estabrooks, C.A. The Complexity of Burnout Experiences among Care Aides: A Person-Oriented Approach to Burnout Patterns. Healthcare 2023, 11, 1145. https://doi.org/10.3390/healthcare11081145
Duan Y, Song Y, Thorne TE, Iaconi A, Norton PG, Estabrooks CA. The Complexity of Burnout Experiences among Care Aides: A Person-Oriented Approach to Burnout Patterns. Healthcare. 2023; 11(8):1145. https://doi.org/10.3390/healthcare11081145
Chicago/Turabian StyleDuan, Yinfei, Yuting Song, Trina E. Thorne, Alba Iaconi, Peter G. Norton, and Carole A. Estabrooks. 2023. "The Complexity of Burnout Experiences among Care Aides: A Person-Oriented Approach to Burnout Patterns" Healthcare 11, no. 8: 1145. https://doi.org/10.3390/healthcare11081145
APA StyleDuan, Y., Song, Y., Thorne, T. E., Iaconi, A., Norton, P. G., & Estabrooks, C. A. (2023). The Complexity of Burnout Experiences among Care Aides: A Person-Oriented Approach to Burnout Patterns. Healthcare, 11(8), 1145. https://doi.org/10.3390/healthcare11081145






