Efficacy of Cognitive Behavior Therapy in Reducing Depression among Patients with Coronary Heart Disease: An Updated Systematic Review and Meta-Analysis of RCTs
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Eligibility Criteria
2.2.1. Types of Participants
2.2.2. Types of Interventions
2.2.3. Types of Comparators
2.2.4. Types of Outcome Measures
2.2.5. Types of Studies
2.3. Data Collection and Analysis
2.3.1. Search Strategy
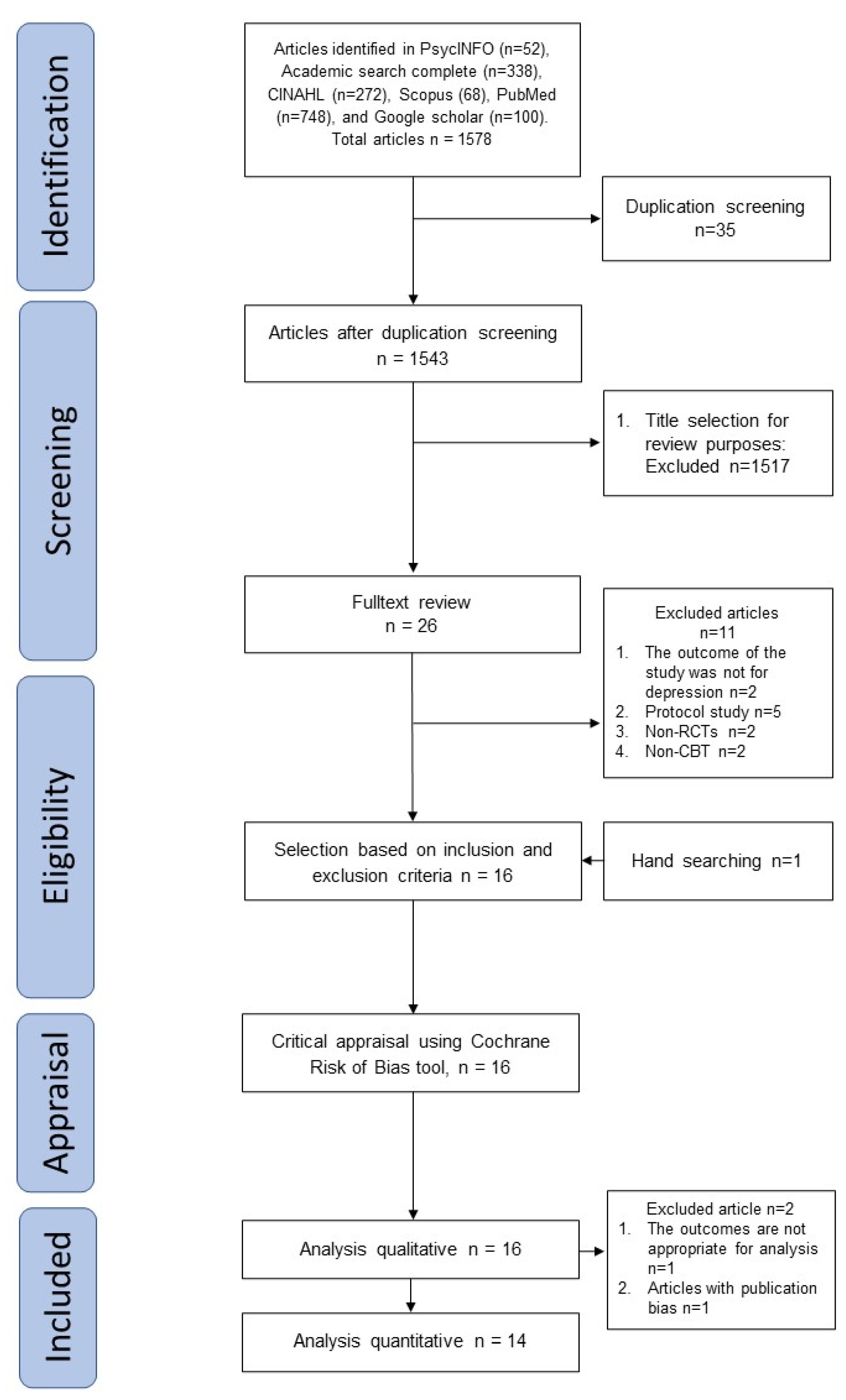
2.3.2. Study Selection
2.3.3. Data Extraction
2.3.4. Assessment of Risk of Bias in Included Studies
2.3.5. Data Synthesis
2.3.6. Publication Bias
2.3.7. Subgroup Analysis
2.3.8. Sensitivity Analysis
3. Results
3.1. Study Selection
3.2. Characteristics of the Included Studies
3.2.1. Participants
3.2.2. Intervention
3.2.3. Comparator
3.3. Risk of Bias within Studies
3.4. Sensitivity Analysis
3.5. Publication Bias
3.6. Efficacy of CBT in Reducing Depression among Patients with CHD
3.7. Subgroup Analysis
4. Discussion
4.1. Principal Results
4.2. Limitations
4.3. Implications for Clinical Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mensah, G.A.; Roth, G.A.; Fuster, V. The Global Burden of Cardiovascular Diseases and Risk Factors: 2020 and beyond. J. Am. Coll. Cardiol. 2019, 74, 2529–2532. [Google Scholar] [CrossRef]
- Chow, C.; Atkins, E.; Islam, S.; Lung, T.; Conroy, K. Reducing the burden of Cardiovascular Disease in Indonesia; Jakarta: Cardiovascular Division, Health Services Research Centre, The George Institute for Global Health: Sydney, Australia, 2017. [Google Scholar]
- Kronish, I.M.; Rieckmann, N.; Burg, M.M.; Edmondson, D.; Schwartz, J.E.; Davidson, K.W. The effect of enhanced depression care on adherence to risk-reducing behaviors after acute coronary syndromes: Findings from the COPES trial. Am. Heart J. 2012, 164, 524–529. [Google Scholar] [CrossRef] [PubMed]
- Smallheer, B.; Dietrich, M.S. Social Support, Self-Efficacy, and Helplessness Following Myocardial Infarctions. Crit. Care Nurs. Q. 2019, 42, 246–255. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Kivimaki, M. Stress and cardiovascular disease. Nat. Rev. Cardiol. 2012, 9, 360–370. [Google Scholar] [CrossRef]
- Von Känel, R.; Hari, R.; Schmid, J.-P.; Saner, H.; Begré, S. Distress related to myocardial infarction and cardiovascular outcome: A retrospective observational study. BMC Psychiatry 2011, 11, 98. [Google Scholar] [CrossRef]
- Zuidersma, M.; Thombs, B.D.; de Jonge, P. Onset and Recurrence of Depression as Predictors of Cardiovascular Prognosis in Depressed Acute Coronary Syndrome Patients: A Systematic Review. Psychother. Psychosom. 2011, 80, 227–237. [Google Scholar] [CrossRef]
- Lane, D.; Carroll, D.; Ring, C.; Beevers, D.; Lip, G.Y. Effects of depression and anxiety on mortality and quality-of-life 4 months after myocardial infarction. J. Psychosom. Res. 2000, 49, 229–238. [Google Scholar] [CrossRef]
- Müller-Tasch, T.; Peters-Klimm, F.; Schellberg, D.; Holzapfel, N.; Barth, A.; Jünger, J.; Szecsenyi, J.; Herzog, W. Depression Is a Major Determinant of Quality of Life in Patients with Chronic Systolic Heart Failure in General Practice. J. Card. Fail. 2007, 13, 818–824. [Google Scholar] [CrossRef]
- Nuraeni, A.; Mirwanti, R.; Anna, A.; Prawesti, A.; Emaliyawati, E. Faktor yang Memengaruhi Kualitas Hidup Pasien dengan Penyakit Jantung Koroner [Factors Affecting Quality of Life of Patients with Coronary Heart Disease]. J. Keperawatan Padjadjaran 2016, 4, 107–116. [Google Scholar] [CrossRef]
- Lichtman, J.H.; Froelicher, E.S.; Blumenthal, J.A.; Carney, R.M.; Doering, L.V.; Frasure-Smith, N.; Freedland, K.E.; Jaffe, A.S.; Leifheit-Limson, E.C.; Sheps, D.S.; et al. Depression as a Risk Factor for Poor Prognosis among Patients with Acute Coronary Syndrome: Systematic Review and Recommendations. Circulation 2014, 129, 1350–1369. [Google Scholar] [CrossRef]
- Vaccarino, V.; Badimon, L.; Bremner, J.D.; Cenko, E.; Cubedo, J.; Dorobantu, M.; Duncker, D.J.; Koller, A.; Manfrini, O.; Milicic, D.; et al. Depression and coronary heart disease: 2018 position paper of the ESC working group on coronary pathophysiology and microcirculation. Eur. Heart J. 2019, 41, 1687–1696. [Google Scholar] [CrossRef] [PubMed]
- Kuhlmann, S.L.; Arolt, V.; Haverkamp, W.; Martus, P.; Ströhle, A.; Waltenberger, J.; Rieckmann, N.; Müller-Nordhorn, J. Prevalence, 12-Month Prognosis, and Clinical Management Need of Depression in Coronary Heart Disease Patients: A Prospective Cohort Study. Psychother. Psychosom. 2019, 88, 300–311. [Google Scholar] [CrossRef]
- Carney, R.M.; Freedland, K.E.; Steinmeyer, B.; Rubin, E.H.; Mann, D.L.; Rich, M.W. Cardiac Risk Markers and Response to Depression Treatment in Patients with Coronary Heart Disease. Psychosom. Med. 2016, 78, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Rosic, D.; Krstacic, G.; Krstacic, A.; Brborovic, O.; Filipcic, I.; Jelavic, M.M. The Role of Ambulatory Cardiac Rehabilitation in Improvement of Quality of Life, Anxiety and Depression. Psychiatr. Danub. 2020, 32 (Suppl. S4), 496–504. [Google Scholar]
- Nikrahan, G.R.; Laferton, J.A.; Asgari, K.; Kalantari, M.; Abedi, M.R.; Etesampour, A.; Rezaei, A.; Suarez, L.; Huffman, J.C. Effects of Positive Psychology Interventions on Risk Biomarkers in Coronary Patients: A Randomized, Wait-List Controlled Pilot Trial. Psychosomatics 2016, 57, 359–368. [Google Scholar] [CrossRef]
- Dowlati, Y.; Herrmann, N.; Swardfager, W.L.; Reim, E.K.; Lanctôt, K.L. Efficacy and Tolerability of Antidepressants for Treatment of Depression in Coronary Artery Disease: A Meta-Analysis. Can. J. Psychiatry 2010, 55, 91–99. [Google Scholar] [CrossRef]
- Smith, P.J.; Sherwood, A.; Mabe, S.; Watkins, L.; Hinderliter, A.; Blumenthal, J.A. Physical activity and psychosocial function following cardiac rehabilitation: One-year follow-up of the ENHANCED study. Gen. Hosp. Psychiatry 2017, 49, 32–36. [Google Scholar] [CrossRef]
- Peterson, J.C.; Charlson, M.E.; Wells, M.T.; Altemus, M. Depression, Coronary Artery Disease, and Physical Activity: How Much Exercise Is Enough? Clin. Ther. 2014, 36, 1518–1530. [Google Scholar] [CrossRef]
- Carney, R.M.; Freedland, K.E.; Rubin, E.H.; Rich, M.W.; Steinmeyer, B.C.; Harris, W.S. Omega-3 Augmentation of Sertraline in Treatment of Depression in Patients with Coronary Heart Disease. JAMA 2009, 302, 1651–1657. [Google Scholar] [CrossRef]
- Nijjar, P.S.; Connett, J.E.; Lindquist, R.; Brown, R.; Burt, M.; Pergolski, A.; Wolfe, A.; Balaji, P.; Chandiramani, N.; Yu, X.; et al. Randomized Trial of Mindfulness-Based Stress Reduction in Cardiac Patients Eligible for Cardiac Rehabilitation. Sci. Rep. 2019, 9, 18415. [Google Scholar] [CrossRef]
- Masjedi-Arani, A.; Yoosefee, S.; Hejazi, S.; Jahangirzade, M.; Jamshidi, M.-A.; Heidari, M.; Farhoush, M. Effectiveness of an Islamic Approach to Hope Therapy on Hope, Depression, and Anxiety in Comparison with Conventional Hope Therapy in Patients with Coronary Heart Disease. J. Adv. Med. Biomed. Res. 2020, 28, 82–89. [Google Scholar] [CrossRef]
- Magán, I.; Casado, L.; Jurado-Barba, R.; Barnum, H.; Redondo, M.M.; Hernandez, A.V.; Bueno, H. Efficacy of psychological interventions on psychological outcomes in coronary artery disease: Systematic review and meta-analysis. Psychol. Med. 2020, 51, 1846–1860. [Google Scholar] [CrossRef]
- Richards, S.H.; Anderson, L.; E Jenkinson, C.; Whalley, B.; Rees, K.; Davies, P.; Bennett, P.; Liu, Z.; West, R.; Thompson, D.R.; et al. Psychological interventions for coronary heart disease: Cochrane systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2017, 25, 247–259. [Google Scholar] [CrossRef]
- Reavell, J.; Hopkinson, M.; Clarkesmith, D.; Lane, D.A. Effectiveness of Cognitive Behavioral Therapy for Depression and Anxiety in Patients with Cardiovascular Disease: A Systematic Review and Meta-Analysis. Psychosom. Med. 2018, 80, 742–753. [Google Scholar] [CrossRef]
- Borenstein, M.; Higgins, L.V.; Rothsiein, H.R. Fixed-effect vs Random-effects models (in introduction to meta-analysis). Introd. Meta-Anal. 2009, 77, 85. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 89, 105906. [Google Scholar]
- Courtois, C.A.; Sonis, J. Guideline: What is Cognitive Behavioral Therapy? Am. Psychol. Assoc. 2017. Available online: https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral.pdf (accessed on 20 January 2023).
- Davidson, K.W.; Bigger, J.T.; Burg, M.M.; Carney, R.M.; Chaplin, W.F.; Czajkowski, S.; Dornelas, E.; Duer-Hefele, J.; Frasure-Smith, N.; Freedland, K.E.; et al. Centralized, Stepped, Patient Preference–Based Treatment for Patients with Post–Acute Coronary Syndrome Depression. JAMA Intern. Med. 2013, 173, 997–1004. [Google Scholar] [CrossRef] [PubMed]
- O’Neil, A.; Taylor, B.; Hare, D.; Sanderson, K.; Cyril, S.; Venugopal, K.; Chan, B.; Atherton, J.J.; Hawkes, A.; Walters, D.L.; et al. Long-term efficacy of a tele-health intervention for acute coronary syndrome patients with depression: 12-month results of the MoodCare randomized controlled trial. Eur. J. Prev. Cardiol. 2014, 22, 1111–1120. [Google Scholar] [CrossRef]
- Nejati, M.; Sharifinia, A.; Maleki, M.; Bayazi, M.H. Comparison of the effectiveness of cognitive-behavioral group intervention for coronary heart disease and cognitive therapy in groups on type D personality and psychological distress on coronary heart patients- a randomized clinical trial. Curr. Psychol. 2022, 41, 4001–4011. [Google Scholar] [CrossRef]
- Berkman, L.F.; Blumenthal, J.; Burg, M.; Carney, R.M.; Catellier, D.; Cowan, M.J.; Czajkowski, S.M.; DeBusk, R.; Hosking, J.; Jaffee, A.; et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: The Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA J. Am. Med. Assoc. 2003, 289, 3106–3116. [Google Scholar] [CrossRef]
- O’Neil, A.; Taylor, B.; Sanderson, K.; Cyril, S.; Chan, B.; Hawkes, A.L.; Hare, D.L.; Jelinek, M.; Venugopal, K.; Atherton, J.J.; et al. Efficacy and Feasibility of a Tele-health Intervention for Acute Coronary Syndrome Patients with Depression: Results of the “MoodCare” Randomized Controlled Trial. Ann. Behav. Med. 2014, 48, 163–174. [Google Scholar] [CrossRef]
- Fernandes, A.C.; McIntyre, T.; Coelho, R.; Prata, J.; Maciel, M.J. Brief psychological intervention in phase I of cardiac rehabilitation after acute coronary syndrome. Rev. Port. Cardiol. 2017, 36, 641–649. [Google Scholar] [CrossRef] [PubMed]
- Freedland, K.E.; Skala, J.A.; Carney, R.M.; Rubin, E.H.; Lustman, P.J.; Dávila-Román, V.G.; Steinmeyer, B.C.; Hogue, C.W. Treatment of Depression after Coronary Artery Bypass Surgery. Arch. Gen. Psychiatry 2009, 66, 387–396. [Google Scholar] [CrossRef] [PubMed]
- Zetta, S.; Smith, K.; Jones, M.; Allcoat, P.; Sullivan, F. Evaluating the Angina Plan in Patients Admitted to Hospital with Angina: A Randomized Controlled Trial. Cardiovasc. Ther. 2011, 29, 112–124. [Google Scholar] [CrossRef] [PubMed]
- Dao, T.K.; Youssef, N.A.; Armsworth, M.; Wear, E.; Papathopoulos, K.N.; Gopaldas, R. Randomized controlled trial of brief cognitive behavioral intervention for depression and anxiety symptoms preoperatively in patients undergoing coronary artery bypass graft surgery. J. Thorac. Cardiovasc. Surg. 2011, 142, e109–e115. [Google Scholar] [CrossRef]
- Norlund, F.; Wallin, E.; Olsson, E.M.G.; Wallert, J.; Burell, G.; von Essen, L.; Held, C. Internet-Based Cognitive Behavioral Therapy for Symptoms of Depression and Anxiety among Patients with a Recent Myocardial Infarction: The U-CARE Heart Randomized Controlled Trial. J. Med. Internet Res. 2018, 20, e88. [Google Scholar] [CrossRef]
- Humphries, S.M.; Wallert, J.; Norlund, F.; Wallin, E.; Burell, G.; von Essen, L.; Held, C.; Olsson, E.M.G. Internet-Based Cognitive Behavioral Therapy for Patients Reporting Symptoms of Anxiety and Depression After Myocardial Infarction: U-CARE Heart Randomized Controlled Trial Twelve-Month Follow-up. J. Med. Internet Res. 2021, 23, e25465. [Google Scholar] [CrossRef]
- Norlund, F.; Olsson, E.; Pingel, R.; Held, C.; Svärdsudd, K.; Gulliksson, M.; Burell, G. Psychological mediators related to clinical outcome in cognitive behavioural therapy for coronary heart disease: A sub-analysis from the SUPRIM trial. Eur. J. Prev. Cardiol. 2017, 24, 917–925. [Google Scholar] [CrossRef]
- Doering, L.V.; Chen, B.; Bodán, R.C.; Magsarili, M.C.; Nyamathi, A.; Irwin, M. Early Cognitive Behavioral Therapy for Depression after Cardiac Surgery. J. Cardiovasc. Nurs. 2013, 28, 370–379. [Google Scholar] [CrossRef]
- Turner, A.; Hambridge, J.; Baker, A.L.; Bowman, J.; McElduff, P. Randomised controlled trial of group cognitive behaviour therapy versus brief intervention for depression in cardiac patients. Aust. N. Z. J. Psychiatry 2012, 47, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Rafanelli, C.; Gostoli, S.; Buzzichelli, S.; Guidi, J.; Sirri, L.; Gallo, P.; Marzola, E.; Bergerone, S.; De Ferrari, G.M.; Roncuzzi, R.; et al. Sequential Combination of Cognitive-Behavioral Treatment and Well-Being Therapy in Depressed Patients with Acute Coronary Syndromes: A Randomized Controlled Trial (TREATED-ACS Study). Psychother. Psychosom. 2020, 89, 345–356. [Google Scholar] [CrossRef]
- Kaambwa, B.; Gesesew, H.A.; Horsfall, M.; Chew, D. Quality of Life Changes in Acute Coronary Syndromes Patients: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 6889. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Gavaghan, D.; Egger, M. Publication and related bias in meta-analysis: Power of statistical tests and prevalence in the literature. J. Clin. Epidemiol. 2000, 53, 1119–1129. [Google Scholar] [CrossRef] [PubMed]
- Barth, J.; Paul, J.; Härter, M.; Bengel, J. Inpatient psychotherapeutic treatment for cardiac patients with depression in Germany short term results. GMS Psycho-Soc. Med. 2005, 2, Doc04. [Google Scholar]
- Chand, S.P.; Ravi, C.; Chakkamparambil, B.; Prasad, A.; Vora, A. CBT for depression: What the evidence says. Curr. Psychiatr. 2018, 17, 14–23. [Google Scholar]
- Nuraeni, A.; Praptiwi, A.; Nurhidayah, I. Depression, Recurrence, and Perceptions of Physical Fitness among CHD Patients: A Comparison based on Participation in Phase II Cardiac Rehabilitation Program. J. Keperawatan Padjadjaran 2020, 8, 233–244. [Google Scholar] [CrossRef]
- Nuraeni, A.; Suryani, S.; Trisyani, Y.; Pramukti, I. Social and Emotional Support Highly Associated with Helplessness among Coronary Heart Disease Patients. Open Access Maced. J. Med. Sci. 2021, 9, 1–6. [Google Scholar] [CrossRef]
- Nur’Aeni, A.; Mirwanti, R. Acceptance, Perceived Benefits, and Helplessness among Coronary Heart Disease Patients Undergoing Treatment in a Different Ward. Padjadjaran Acute Care Nurs. J. 2020, 1, 68–79. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.; Rothstein, H. Meta-analysis: Fixed effect vs. random effects. Meta-Analysis. com 2007, 1–162. Available online: https://www.meta-analysis.com/downloads/M-a_f_e_v_r_e_sv.pdf (accessed on 20 January 2023).
- Erekson, D.M.; Lambert, M.J.; Eggett, D.L. The relationship between session frequency and psychotherapy outcome in a naturalistic setting. J. Consult. Clin. Psychol. 2015, 83, 1097–1107. [Google Scholar] [CrossRef]
- Beltman, M.W.; Voshaar, R.O.; Speckens, A. Cognitive–behavioural therapy for depression in people with a somatic disease: Meta-analysis of randomised controlled trials. Br. J. Psychiatry 2010, 197, 11–19. [Google Scholar] [CrossRef]
- Saengsiri, A.-O.; Thanasilp, S.; Preechawong, S. Factors predicting quality of life for coronary artery disease patients after percutaneous coronary intervention. Asian Biomed. 2014, 8, 31–42. [Google Scholar] [CrossRef]
- Herrmann-Lingen, C.; Beutel, M.E.; Bosbach, A.; Deter, H.-C.; Fritzsche, K.; Hellmich, M.; Jordan, J.; Jünger, J.; Ladwig, K.-H.; Michal, M.; et al. A Stepwise Psychotherapy Intervention for Reducing Risk in Coronary Artery Disease (SPIRR-CAD): Results of an Observer-Blinded, Multicenter, Randomized Trial in Depressed Patients with Coronary Artery Disease. Psychosom. Med. 2016, 78, 704–715. [Google Scholar] [CrossRef]
- Christensen, H.; Griffiths, K.M.; Mackinnon, A.; Brittliffe, K. Online randomized controlled trial of brief and full cognitive behaviour therapy for depression. Psychol. Med. 2006, 36, 1737–1746. [Google Scholar] [CrossRef]
- Cuijpers, P.; van Straten, A.; Warmerdam, L. Are individual and group treatments equally effective in the treatment of depression in adults? A meta-analysis. Eur. J. Psychiatry 2008, 22, 38–51. [Google Scholar] [CrossRef]
- Ryan, M.; Nitsun, M.; Gilbert, L.; Mason, H. A prospective study of the effectiveness of group and individual psychotherapy for women CSA survivors. Psychol. Psychother. Theory Res. Pract. 2005, 78, 465–480. [Google Scholar] [CrossRef] [PubMed]



| Test Name | Value | p |
|---|---|---|
| Fail-safe N | 377.000 | <0.001 |
| Begg and Mazumdar rank correlation | 0.011 | 1.000 |
| Egger’s regression | −0.013 | 0.989 |
| Trim and fill number of studies | 0.000 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nuraeni, A.; Suryani, S.; Trisyani, Y.; Sofiatin, Y. Efficacy of Cognitive Behavior Therapy in Reducing Depression among Patients with Coronary Heart Disease: An Updated Systematic Review and Meta-Analysis of RCTs. Healthcare 2023, 11, 943. https://doi.org/10.3390/healthcare11070943
Nuraeni A, Suryani S, Trisyani Y, Sofiatin Y. Efficacy of Cognitive Behavior Therapy in Reducing Depression among Patients with Coronary Heart Disease: An Updated Systematic Review and Meta-Analysis of RCTs. Healthcare. 2023; 11(7):943. https://doi.org/10.3390/healthcare11070943
Chicago/Turabian StyleNuraeni, Aan, Suryani Suryani, Yanny Trisyani, and Yulia Sofiatin. 2023. "Efficacy of Cognitive Behavior Therapy in Reducing Depression among Patients with Coronary Heart Disease: An Updated Systematic Review and Meta-Analysis of RCTs" Healthcare 11, no. 7: 943. https://doi.org/10.3390/healthcare11070943
APA StyleNuraeni, A., Suryani, S., Trisyani, Y., & Sofiatin, Y. (2023). Efficacy of Cognitive Behavior Therapy in Reducing Depression among Patients with Coronary Heart Disease: An Updated Systematic Review and Meta-Analysis of RCTs. Healthcare, 11(7), 943. https://doi.org/10.3390/healthcare11070943







