Infant and Young Child Feeding Knowledge among Caregivers of Children Aged between 0 and 24 Months in Seshego Township, Limpopo Province, South Africa
Abstract
1. Background
2. Methodology
2.1. Research Design and Setting
2.2. Population and Sampling of the Study
2.3. Instruments and Data Collection
2.4. Data Analysis
2.5. Ethical Issues
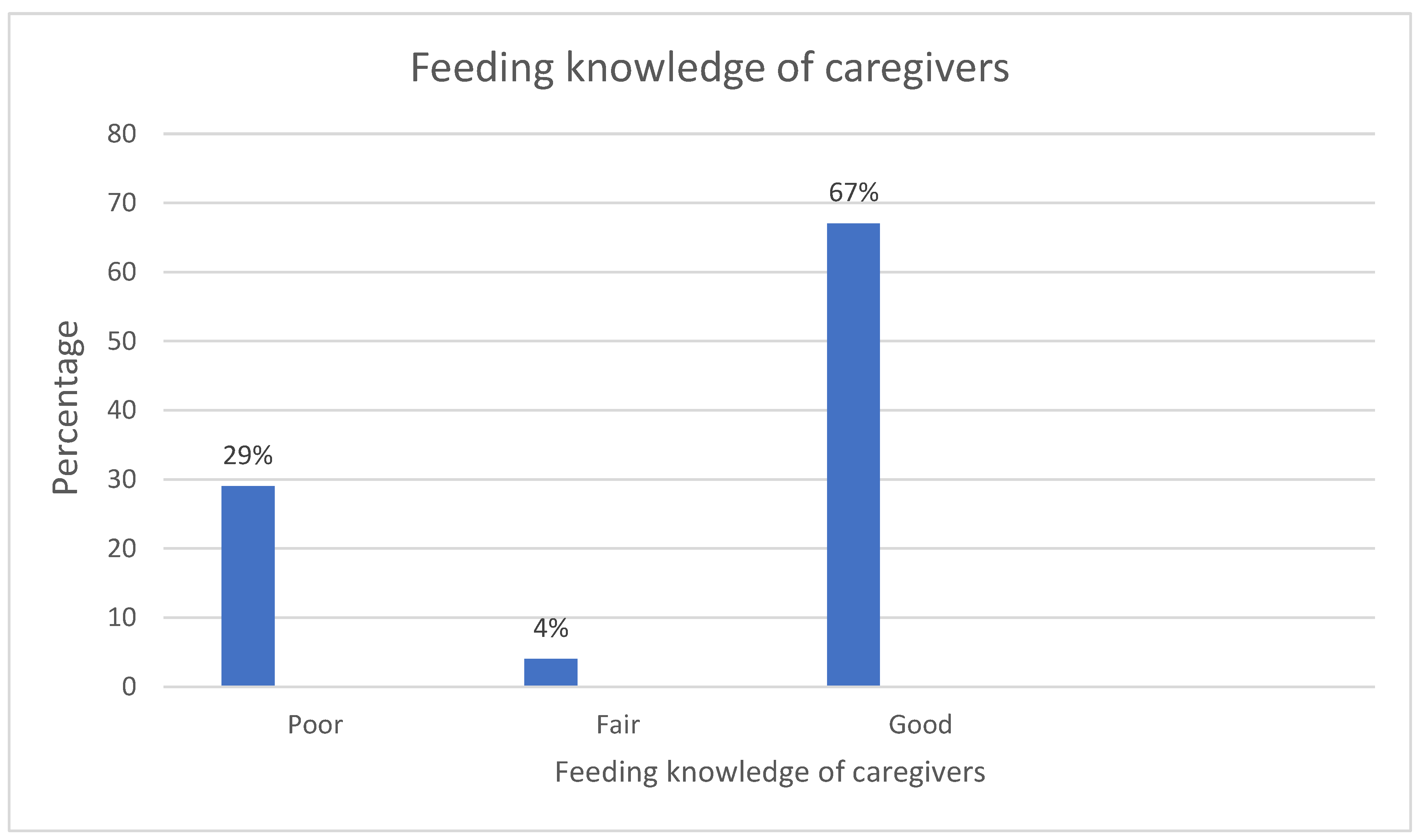
3. Results
Socio-Demographic Profile
4. Discussions
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Disclaimer
References
- World Health Organization. The Global Burden of Disease: 2004 Update; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- World Health Organization. Infant and Young Child Feeding. Available online: www.who.int (accessed on 9 June 2022).
- Ballard, O.; Morrow, A.L. Human milk composition: Nutrients and bioactive factors. Pediatr. Clin. N. Am. 2013, 60, 49–74. [Google Scholar] [CrossRef] [PubMed]
- Oddy, W.H. Breastfeeding protects against illness and infection in infants and children: A review of the evidence. Breastfeed Rev. 2001, 9, 11–18. [Google Scholar]
- Yan, J.; Liu, L.; Zhu, Y.; Huang, G.; Wang, P.P. The association between breastfeeding and childhood obesity: A meta-analysis. BMC Public Health 2014, 14, 1267. [Google Scholar] [CrossRef] [PubMed]
- Victora, C.G.; Bahl, R.; Barros, A.J.; França, G.V.; Horton, S.; Krasevec, J.; Murch, S.; Sankar, M.J.; Walker, N.; Rollins, N.C.; et al. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016, 387, 475–490. [Google Scholar] [CrossRef] [PubMed]
- Lamberti, L.M.; Zakarija-Grković, I.; Fischer Walker, C.L.; Theodoratou, E.; Nair, H.; Campbell, H.; Black, R.E. Breastfeeding for reducing the risk of pneumonia morbidity and mortality in children under two: A systematic literature review and meta-analysis. BMC Public Health 2013, 13 (Suppl. S3), S18. [Google Scholar] [CrossRef]
- Rodríguez, L.; Cervantes, E.; Ortiz, R. Malnutrition and gastrointestinal and respiratory infections in children: A public health problem. Int. J. Environ. Res. Public Health 2011, 8, 1174–1205. [Google Scholar] [CrossRef]
- Duijts, L.; Ramadhani, M.K.; Moll, H.A. Breastfeeding protects against infectious diseases during infancy in industrialized countries. A systematic review. Matern. Child Nutr. 2009, 5, 199–210. [Google Scholar] [CrossRef]
- Hahn-Holbrook, J.; Schetter, C.D.; Haselton, M.G. Breastfeeding and maternal mental and physical health. In Women’s Health Psychology; Spiers, M.V., Geller, P.A., Kloss, J.D., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2013; pp. 414–439. [Google Scholar]
- Dieterich, C.M.; Felice, J.P.; O’Sullivan, E.; Rasmussen, K.M. Breastfeeding and health outcomes for the mother-infant dyad. Pediatr. Clin. N. Am. 2013, 60, 31–48. [Google Scholar] [CrossRef] [PubMed]
- Stuebe, A. The risks of not breastfeeding for mothers and infants. Rev. Obstet. Gynecol. 2009, 2, 222–231. [Google Scholar]
- Quigley, M.; Carson, C.; Sacker, A.; Kelly, Y. Exclusive breastfeeding duration and infant infection. Eur. J. Clin. Nutr. 2016, 70, 1420–1427. [Google Scholar] [CrossRef]
- Greenwood, B. A global action plan for the prevention and control of pneumonia. Bull. World Health Organ. 2008, 86, 322. [Google Scholar] [CrossRef]
- Abeshu, M.A.; Lelisa, A.; Geleta, B. Complementary Feeding: Review of Recommendations, Feeding Practices, and Adequacy of Homemade Complementary Food Preparations in Developing Countries—Lessons from Ethiopia. Front. Nutr. 2016, 3, 41. [Google Scholar] [CrossRef]
- White, J.M.; Bégin, F.; Kumapley, R.; Murray, C.; Krasevec, J. Complementary feeding practices: Current global and regional estimates. Matern. Child Nutr. 2017, 13 (Suppl. S2), e12505. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guiding Principles for Complementary Feeding of the Breastfed Child; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Bhutta, Z.A.; Das, J.K.; Rizvi, A.; Gaffey, M.F.; Walker, N.; Horton, S.; Webb, P.; Lartey, A.; Black, R.E. Evidence-based interventions for improvement of maternal and child nutrition: What can be done and at what cost? Lancet 2013, 382, 452–477. [Google Scholar] [CrossRef] [PubMed]
- Hamer, D.H.; Solomon, H.; Das, G.; Knabe, T.; Beard, J.; Simon, J.; Nisar, Y.B.; MacLeod, W.B. Importance of breastfeeding and complementary feeding for management and prevention of childhood diarrhoea in low- and middle-income countries. J. Global Health 2022, 12, 10011. [Google Scholar] [CrossRef]
- Khan, M.N.; Islam, M.M. Effect of exclusive breastfeeding on selected adverse health and nutritional outcomes: A nationally representative study. BMC Public Health 2017, 17, 889. [Google Scholar] [CrossRef]
- La Leche League International. Available online: www.llli.org (accessed on 26 November 2022).
- Martorell, R.; Kettel Khan, L.; Schroeder, D.G. Reversibility of stunting: Epidemiological findings in children from developing countries. Eur. J. Clin. Nutr. 1994, 58 (Suppl. S1), S45–S57. [Google Scholar]
- Pollitt, E.; Gorman, K.S.; Engle, P.L.; Rivera, J.A.; Martorell, R. Nutrition in early life and the fulfilment of intellectual potential. J. Nutr. 1995, 125, 1111S–1118S. [Google Scholar]
- Haas, J.D.; Scott, M.; Juan, R.; Reynaldo, M. Early nutrition and later physical work capacity. Nutr. Rev. 1996, 54, S41–S48. [Google Scholar] [CrossRef]
- Martin, R.M.; Smith, G.D.; Frankel, S.; Gunnell, D. Parents’ growth in childhood and the birth weight of their offspring. Epidemiology 2004, 15, 308–316. [Google Scholar] [CrossRef]
- Maponya, N.M.; Matlala, S.F. “They shouted at me to discontinue exclusive breastfeeding”: Narratives of mothers in Limpopo Province of South Africa as they grabble with exclusive breastfeeding. Bangladesh J. Med. Sci. 2022, 21, 813–819. [Google Scholar] [CrossRef]
- Malise, T.; Mushaphi, F.L.; Malise, S.A. Breastfeeding knowledge and practices among caregivers of children younger than 2 years from a rural area in the Limpopo Province, South Africa. S. Afr. J. Child Health 2019, 13, 115–119. [Google Scholar]
- Vitalis, D.; Vilar-Compte, M.; Nyhan, K.; Pérez-Escamilla, R. Breastfeeding inequities in South Africa: Can enforcement of the WHO Code help address them?—A systematic scoping review. Int. J. Equity Health 2021, 20, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Motebejana, T.T.; Nesamvuni, C.N.; Mbhenyane, X. Nutrition Knowledge of Caregivers Influences Feeding Practices and Nutritional Status of Children 2 to 5 Years Old in Sekhukhune District, South Africa. Ethiopia J. Health Sci. 2022, 32, 103–116. [Google Scholar]
- Nti, C.A.; Lartey, A. Influence of care practices on nutritional status of Ghanaian children. Nutr. Res. Pract. 2008, 2, 93–99. [Google Scholar] [CrossRef]
- Tessema, M.; Belachew, T.; Ersino, G. Feeding patterns and stunting during early childhood in rural communities of Sidama, South Ethiopia. Pan. Afr. Med. J. 2013, 14, 75. [Google Scholar] [CrossRef]
- Ersino, G.; Henry, C.J.; Zello, G.A. Suboptimal Feeding Practices and High Levels of Undernutrition Among Infants and Young Children in the Rural Communities of Halaba and Zeway, Ethiopia. Food Nutr. Bull. 2016, 37, 409–424. [Google Scholar] [CrossRef] [PubMed]
- Issaka, A.I.; Agho, K.E.; Renzaho, A.M. Prevalence of key breastfeeding indicators in 29 sub-Saharan African countries: A meta-analysis of demographic and health surveys (2010-2015). BMJ Open 2017, 7, e014145. [Google Scholar] [CrossRef] [PubMed]
- Zongrone, A.; Winskell, K.; Menon, P. Infant and young child feeding practices and child undernutrition in Bangladesh: Insights from nationally representative data. Public Health Nutr. 2012, 15, 1697–1704. [Google Scholar] [CrossRef]
- Fadare, O.; Amare, M.; Mavrotas, G.; Akerele, D.; Ogunniyi, A. Mother’s nutrition-related knowledge and child nutrition outcomes: Empirical evidence from Nigeria. PLoS ONE 2019, 14, e0212775. [Google Scholar] [CrossRef]
- Debela, B.L.; Demmler, K.M.; Rischke, R.; Qaim, M. Maternal nutrition knowledge and child nutritional outcomes in urban Kenya. Appetite 2017, 116, 518–526. [Google Scholar] [CrossRef]
- Demilew, Y.M. Factors associated with mothers’ knowledge on infant and young child feeding recommendation in slum areas of Bahir Dar City, Ethiopia: Cross sectional study. BMC Res. Notes 2017, 10, 191. [Google Scholar] [CrossRef]
- Mphasha, M.H.; Skaal, L. Infant and Young Child Feeding Policy:do primary health care nurses adhere to the HIV breastfeeding recommendations in Limpopo province? S. Afr. J. Clin. Nutr. 2019, 32, 70–75. [Google Scholar] [CrossRef]
- Wu, Q.; Scherpbier, R.W.; van Velthoven, M.H.; Chen, L.; Wang, W.; Li, Y.; Zhang, Y.; Car, J. Poor infant and young child feeding practices and sources of caregivers’ feeding knowledge in rural Hebei Province, China: Findings from a cross-sectional survey. BMJ Open 2014, 4, e005108. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wu, Y.; Xiong, G.; Chao, T.; Jin, Q.; Liu, R.; Hao, L.; Wei, S.; Yang, N.; Yang, X. Introduction of complementary feeding before 4 months of age increases the risk of childhood overweight or obesity: A meta-analysis of prospective cohort studies. Nutr. Res. 2016, 36, 759–770. [Google Scholar] [CrossRef] [PubMed]
- Morgan, D.W.; Krejcie, R.V. Determining sample size for research activities. Educ. Psychol. Meas. 1970, 30, 607–610. [Google Scholar]
- Kreps, G.L. Promoting patient comprehension of relevant health information. Isr. J. Health Policy Res. 2018, 7, 56. [Google Scholar] [CrossRef]
- Kindig, D.A.; Panzer, A.M.; Nielsen-Bohlman, L. Health Literacy: A Prescription to End Confusion; National Academies Press: Washington, DC, USA, 2004. [Google Scholar]
- Kreps, G.L.; Villagran, M.M.; Zhao, X.; McHorney, C.; Ledford, C.; Weathers, M.; Keefe, B.P. Development and validation of motivational messages to improve prescription medication adherence for patients with chronic health problems. Patient Educ. Couns. 2011, 83, 365–371. [Google Scholar] [CrossRef]
- Amann, J.; Rubinelli, S.; Kreps, G.L. Revisiting the concept of health literacy: The patient as information seeker and provider. Eur. Health Psychol. 2015, 17, 286–290. [Google Scholar]
- Williams, L.; Campbell, K.; Abbott, G.; Crawford, D.; Ball, K. Is maternal nutrition knowledge more strongly associated with the diets of mothers or their school-aged children? Public Health Nutr. 2012, 15, 1396–1401. [Google Scholar] [CrossRef]
- van Ansem, W.J.; Schrijvers, C.T.; Rodenburg, G.; van de Mheen, D. Maternal educational level and children’s healthy eating behaviour: Role of the home food environment (cross-sectional results from the INPACT study). Int. J. Behav. Nutr. Phys. Act. 2014, 11, 113. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Huo, J.; Sun, J.; Huang, J.; Gong, W.; Wang, O. Prevalence of Complementary Feeding Indicators and Associated Factors Among 6- to 23-Month Breastfed Infants and Young Children in Poor Rural Areas of China. Front. Public Health 2021, 9, 691894. [Google Scholar] [CrossRef] [PubMed]
- Raghupathi, V.; Raghupathi, W. The influence of education on health: An empirical assessment of OECD countries for the period 1995–2015. Arch. Public Health 2020, 78, 20. [Google Scholar] [CrossRef] [PubMed]
- Houts, P.S.; Doak, C.C.; Doak, L.G.; Loscalzo, M.J. The role of pictures in improving health communication: A review of research on attention, comprehension, recall, and adherence. Patient Educ. Couns. 2006, 61, 173–190. [Google Scholar] [CrossRef]
- Frans, R.A.; Malema, R.N.; Matlala, S.F. Knowledge and practices of mothers regarding exclusive breastfeeding in Mahwelereng local area of the Limpopo province, South Africa. Afr. J. Phys. Health Educ. Recreat. Danc. (AJPHERD) 2015, 1, 812–825. [Google Scholar]
- Assefa, D.G.; Woldensenbet, T.T.; Molla, W.; Zeleke, E.D.; Simie, T.G. Assessment of knowledge, attitude, and practice of mothers/caregivers on infant and young child feeding in Assosa Woreda, Assosa Zone, Benshangul Gumuz Region, Western Ethiopia: A cross-sectional study. Arch. Public Health 2021, 79, 170. [Google Scholar] [CrossRef]
- Boquien, C.-Y. Human Milk: An Ideal Food for Nutrition of Preterm Newborn. Front. Pediatr. 2018, 6, 295. [Google Scholar] [CrossRef]
- Tromp, I.; Kiefte-de Jong, J.; Raat, H.; Jaddoe, V.; Franco, O.; Hofman, A.; de Jongste, J.; Moll, H. Breastfeeding and the risk of respiratory tract infections after infancy: The Generation R Study. PLoS ONE 2017, 12, e0172763. [Google Scholar] [CrossRef]
- Al-Nawaiseh, F.K.; Al-Jaghbir, M.T.; Al-Assaf, M.S.; Al-Nawaiseh, H.K.; Alzoubi, M.M. Breastfeeding initiation and duration and acute otitis media among children less than two years of age in Jordan: Results from a case-control study. BMC Pediatr. 2022, 22, 370. [Google Scholar] [CrossRef]
- Shrestha, S.; Pokhre, M.; Mathema, S. Knowledge, Attitude and Practices among Mothers of Children 6 to 24 months of Age Regarding Complementary Feeding. J. Nepal. Med. Assoc. 2020, 58, 758–763. [Google Scholar] [CrossRef]
| Variables | Categories | n (%) |
|---|---|---|
| Age of mother/caregiver | 18–35 years | 69 (80.2%) |
| ≥36 years | 17 (19.8%) | |
| Race | Black | 85 (98.8%) |
| Coloured | 1 (1.2%) | |
| Education status | Secondary education or less | 48 (55.8%) |
| Tertiary education | 38 (44.2%) | |
| Employment status | Temporary employed | 7 (8.1%) |
| Permanently employed | 9 (10.5%) | |
| Self employed | 11 (12.8%) | |
| Unemployed | 59 (68.6%) | |
| Source of income | Social grant | 58 (67.4%) |
| Pension fund | 1 (1.2%) | |
| Salary | 17 (19.8%) | |
| Other | 10 (11.6%) | |
| Number of household members | 1–5 | 55 (63.9%) |
| 6–10 | 31 (36.0%) | |
| Relationship to the child | Mother | 84 (97.7%) |
| Caregiver (grandmother, siblings of mother, nanny) | 2 (2.3%) | |
| Number of children | 1–2 | 52 (60.5%) |
| 3–8 | 34 (39.5%) | |
| Age of child in months | 0–6 | 45 (52.3%) |
| 7–12 | 22 (25.6%) | |
| 13–18 | 12 (13.9%) | |
| 19–24 | 7 (8.1%) |
| Knowledge of Caregivers Regarding Infant Feeding | Yes | Not Sure | No |
|---|---|---|---|
| Should breastfeeding be initiated immediately after birth? | 83 (96.5%) | 2 (2.3%) | 1 (1.2%) |
| Is exclusive breastfeeding up to 6 months? | 51 (59.3%) | 0 (0%) | 35 (40.7%) |
| Does breastmilk protect the child from diseases? | 78 (90.7%) | 2 (2.3%) | 6 (7%) |
| Can an HIV positive mother breastfeed? | 56 (65.1%) | 6 (7%) | 24 (27.9%) |
| Should solid food be introduced at 6 months? | 71 (82.6%) | 4 (4.7%) | 11 (12.7%) |
| Should breastfeeding be stopped when semi-solid and solid food are given? | 11 (12.7%) | 4 (4.7%) | 71 (82.6%) |
| Knowledge of Family by Socio-Demographic Profile | Overall Knowledge | p-Values * | |||
|---|---|---|---|---|---|
| Poor Knowledge | Fair Knowledge | Good Knowledge | |||
| Age | 18–35 | 3 | 20 | 46 | 0.751 |
| ≥36 | 0 | 8 | 9 | ||
| Education | Secondary or less | 1 | 3 | 0 | <0.001 |
| Tertiary or more | 2 | 25 | 55 | ||
| Employment | Employed | 1 | 12 | 14 | 0.564 |
| Unemployed | 2 | 16 | 41 | ||
| Number of children | 1–2 | 2 | 16 | 34 | 0.436 |
| 3–8 | 1 | 12 | 21 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muleka, N.; Maanaso, B.; Phoku, M.; Mphasha, M.H.; Makwela, M. Infant and Young Child Feeding Knowledge among Caregivers of Children Aged between 0 and 24 Months in Seshego Township, Limpopo Province, South Africa. Healthcare 2023, 11, 1044. https://doi.org/10.3390/healthcare11071044
Muleka N, Maanaso B, Phoku M, Mphasha MH, Makwela M. Infant and Young Child Feeding Knowledge among Caregivers of Children Aged between 0 and 24 Months in Seshego Township, Limpopo Province, South Africa. Healthcare. 2023; 11(7):1044. https://doi.org/10.3390/healthcare11071044
Chicago/Turabian StyleMuleka, Ndivhudzannyi, Baatseba Maanaso, Mafiwa Phoku, Mabitsela Hezekiel Mphasha, and Maishataba Makwela. 2023. "Infant and Young Child Feeding Knowledge among Caregivers of Children Aged between 0 and 24 Months in Seshego Township, Limpopo Province, South Africa" Healthcare 11, no. 7: 1044. https://doi.org/10.3390/healthcare11071044
APA StyleMuleka, N., Maanaso, B., Phoku, M., Mphasha, M. H., & Makwela, M. (2023). Infant and Young Child Feeding Knowledge among Caregivers of Children Aged between 0 and 24 Months in Seshego Township, Limpopo Province, South Africa. Healthcare, 11(7), 1044. https://doi.org/10.3390/healthcare11071044






