Physical Inactivity, Sedentary Behavior and Quality of Life in the Chilean Population: ENCAVI Results, 2015–2016
Abstract
1. Introduction
2. Materials and Methods
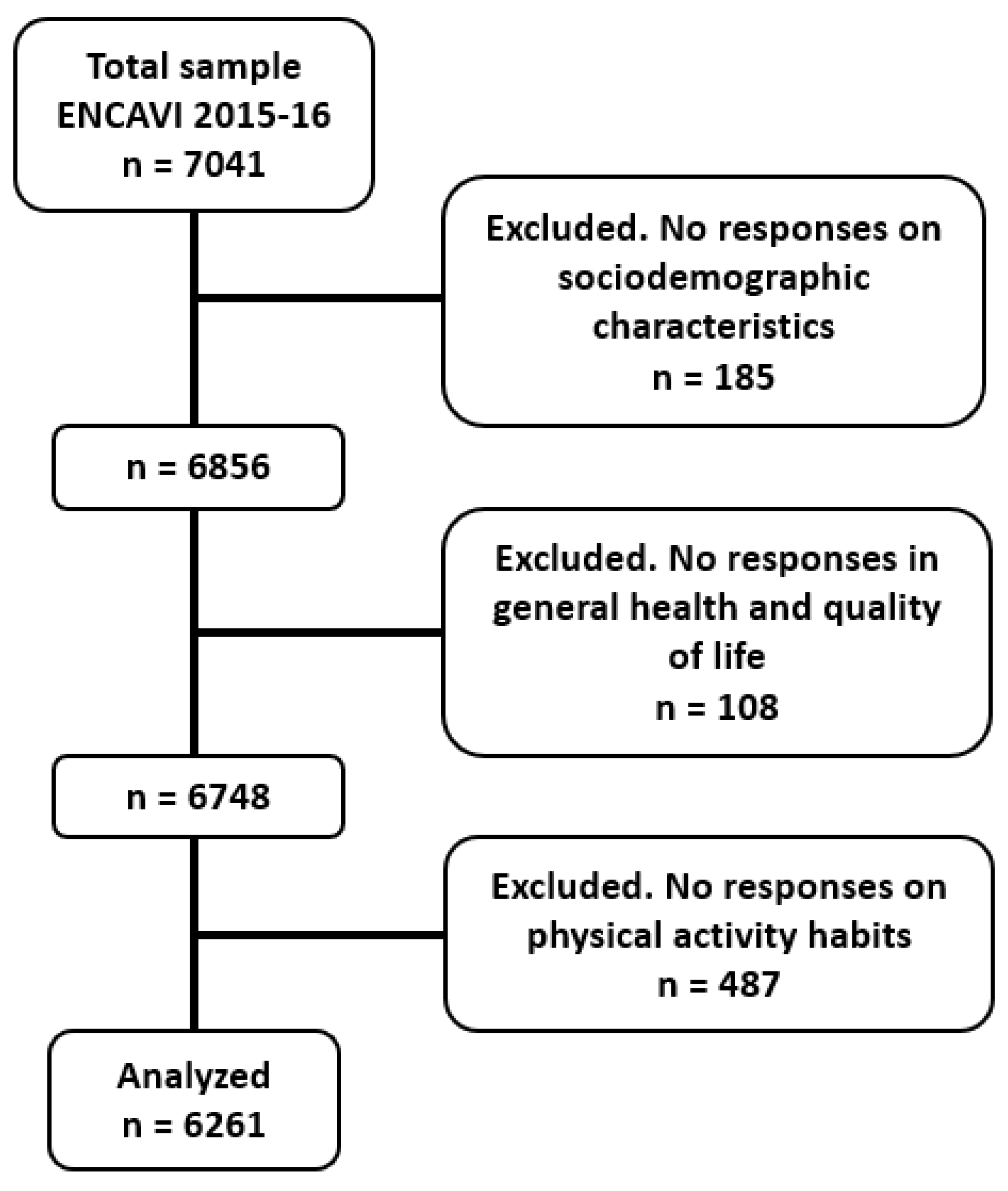
2.1. Participants
2.2. Selection of Variables
2.3. Statistical Analyses
3. Results
3.1. Sociodemographic Characteristics
3.2. PI and SB
4. Discussion
4.1. PI and SB Levels
4.2. Quality of Life
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schuch, F.B.; Vancampfort, D. Physical Activity, Exercise, and Mental Disorders: It Is Time to Move On. Trends Psychiatry Psychother. 2021, 43, 177–184. [Google Scholar] [CrossRef] [PubMed]
- An, H.Y.; Chen, W.; Wang, C.W.; Yang, H.F.; Huang, W.T.; Fan, S.Y. The Relationships between Physical Activity and Life Satisfaction and Happiness among Young, Middle-Aged, and Older Adults. Int. J. Environ. Res. Public Health 2020, 17, 4817. [Google Scholar] [CrossRef] [PubMed]
- Amatriain-Fernández, S.; Murillo-Rodríguez, E.S.; Gronwald, T.; Machado, S.; Budde, H. Benefits of Physical Activity and Physical Exercise in the Time of Pandemic. Psychol. Trauma 2020, 12, S264. [Google Scholar] [CrossRef]
- Watson, M.C.; Lloyd, J. Physical Activity: Manifold Benefits for Health and Wellbeing. BMJ 2022, 376, 815. [Google Scholar] [CrossRef] [PubMed]
- Otto, C.M. Heartbeat: Benefits of Continued Physical Activity in Late Life. Heart 2022, 108, 325–327. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide Trends in Insufficient Physical Activity from 2001 to 2016: A Pooled Analysis of 358 Population-Based Surveys with 1·9 Million Participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Ferrari, G.L.d.M.; Kovalskys, I.; Fisberg, M.; Gómez, G.; Rigotti, A.; Sanabria, L.Y.C.; García, M.C.Y.; Torres, R.G.P.; Herrera-Cuenca, M.; Zimberg, I.Z.; et al. Socio-Demographic Patterning of Objectively Measured Physical Activity and Sedentary Behaviours in Eight Latin American Countries: Findings from the ELANS Study. Eur. J. Sport Sci. 2020, 20, 670–681. [Google Scholar] [CrossRef]
- Bernabe-Ortiz, A.; Carrillo-Larco, R.M. Physical Activity Patterns Among Adolescents in the Latin American and Caribbean Region. J. Phys. Act. Health 2022, 19, 607. [Google Scholar] [CrossRef]
- Haileamlak, A. Physical Inactivity: The Major Risk Factor for Non-Communicable Diseases. Ethiop. J. Health Sci. 2019, 29, 810. [Google Scholar] [CrossRef]
- Duran, A.T.; Romero, E.; Diaz, K.M. Is Sedentary Behavior a Novel Risk Factor for Cardiovascular Disease? Curr. Cardiol. Rep. 2022, 24, 393–403. [Google Scholar] [CrossRef]
- Wang, Z.; Jin, X.; Liu, Y.; Wang, C.; Li, J.; Tian, L.; Teng, W. Sedentary Behavior and the Risk of Stroke: A Systematic Review and Dose-Response Meta-Analysis. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 2705–2713. [Google Scholar] [CrossRef] [PubMed]
- Jochem, C.; Wallmann-Sperlich, B.; Leitzmann, M.F. The Influence of Sedentary Behavior on Cancer Risk: Epidemiologic Evidence and Potential Molecular Mechanisms. Curr. Nutr. Rep. 2019, 8, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Friedenreich, C.M.; Ryder-Burbidge, C.; McNeil, J. Physical Activity, Obesity and Sedentary Behavior in Cancer Etiology: Epidemiologic Evidence and Biologic Mechanisms. Mol. Oncol. 2021, 15, 790–800. [Google Scholar] [CrossRef] [PubMed]
- Haskell, W.L.; Lee, I.M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; Macera, C.A.; Heath, G.W.; Thompson, P.D.; Bauman, A. Physical Activity and Public Health: Updated Recommendation for Adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1081–1093. [Google Scholar] [CrossRef] [PubMed]
- van der Ploeg, H.P.; Hillsdon, M. Is Sedentary Behaviour Just Physical Inactivity by Another Name? Int. J. Behav. Nutr. Phys. Act. 2017, 14, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Thivel, D.; Tremblay, A.; Genin, P.M.; Panahi, S.; Rivière, D.; Duclos, M. Physical Activity, Inactivity, and Sedentary Behaviors: Definitions and Implications in Occupational Health. Front. Public Health 2018, 6, 288. [Google Scholar] [CrossRef]
- Dempsey, P.C.; Matthews, C.E.; Dashti, S.G.; Doherty, A.R.; Bergouignan, A.; van Roekel, E.H.; Dunstan, D.W.; Wareham, N.J.; Yates, T.E.; Wijndaele, K.; et al. Sedentary Behavior and Chronic Disease: Mechanisms and Future Directions. J. Phys. Act. Health 2020, 17, 52–61. [Google Scholar] [CrossRef]
- Leiva, A.M.; Martínez, M.A.; Cristi-Montero, C.; Salas, C.; Ramírez-Campillo, R.; Martínez, X.D.; Aguilar-Farías, N.; Celis-Morales, C. Sedentary Lifestyle Is Associated with Metabolic and Cardiovascular Risk Factors Independent of Physical Activity. Rev. Med. Chil. 2017, 145, 458–467. [Google Scholar] [CrossRef]
- Ahumada Tello, J.; Toffoletto, M.C.; Ahumada Tello, J.; Toffoletto, M.C. Factors Associated with Sedentary Lifestyle and Physical Inactivity in Chile: A Qualitative Systematic Review. Rev. Med. Chil. 2020, 148, 233–241. [Google Scholar] [CrossRef]
- Zheng, C.; Huang, W.Y.; Sheridan, S.; Sit, C.H.P.; Chen, X.K.; Wong, S.H.S. COVID-19 Pandemic Brings a Sedentary Lifestyle in Young Adults: A Cross-Sectional and Longitudinal Study. Int. J. Environ. Res. Public Health 2020, 17, 6035. [Google Scholar] [CrossRef]
- Stockwell, S.; Trott, M.; Tully, M.; Shin, J.; Barnett, Y.; Butler, L.; McDermott, D.; Schuch, F.; Smith, L. Changes in Physical Activity and Sedentary Behaviours from before to during the COVID-19 Pandemic Lockdown: A Systematic Review. BMJ Open Sport Exerc. Med. 2021, 7, e000960. [Google Scholar] [CrossRef] [PubMed]
- Runacres, A.; Mackintosh, K.A.; Knight, R.L.; Sheeran, L.; Thatcher, R.; Shelley, J.; McNarry, M.A. Impact of the Covid-19 Pandemic on Sedentary Time and Behaviour in Children and Adults: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 11286. [Google Scholar] [CrossRef] [PubMed]
- Sepúlveda-Loyola, W.; Rodríguez-Sánchez, I.; Pérez-Rodríguez, P.; Ganz, F.; Torralba, R.; Oliveira, D.V.; Rodríguez-Mañas, L. Impact of Social Isolation Due to COVID-19 on Health in Older People: Mental and Physical Effects and Recommendations. J. Nutr. Health Aging 2020, 24, 938–947. [Google Scholar] [CrossRef] [PubMed]
- Pecanha, T.; Goessler, K.F.; Roschel, H.; Gualano, B. Social Isolation during the COVID-19 Pandemic Can Increase Physical Inactivity and the Global Burden of Cardiovascular Disease. Am. J. Physiol. Heart Circ. Physiol. 2020, 318, H1441–H1446. [Google Scholar] [CrossRef]
- Panahi, S.; Tremblay, A. Sedentariness and Health: Is Sedentary Behavior More Than Just Physical Inactivity? Front. Public Health 2018, 6, 258. [Google Scholar] [CrossRef]
- Chandrasekaran, B.; Pesola, A.J.; Rao, C.R.; Arumugam, A. Does Breaking up Prolonged Sitting Improve Cognitive Functions in Sedentary Adults? A Mapping Review and Hypothesis Formulation on the Potential Physiological Mechanisms. BMC Musculoskelet. Disord. 2021, 22, 1–16. [Google Scholar] [CrossRef]
- Silva, D.R.; Barboza, L.L.; Baldew, S.S.; Anza-Ramirez, C.; Ramírez-Vélez, R.; Schuch, F.B.; Gomes, T.N.; Sadarangani, K.P.; García-Hermoso, A.; Nieto-Martinez, R.; et al. Measurement of Physical Activity and Sedentary Behavior in National Health Surveys, South America. Rev. Panam. Salud Publica 2022, 46, 7. [Google Scholar] [CrossRef]
- Werneck, A.O.; Baldew, S.S.; Miranda, J.J.; Díaz Arnesto, O.; Stubbs, B.; Silva, D.R. Physical Activity and Sedentary Behavior Patterns and Sociodemographic Correlates in 116,982 Adults from Six South American Countries: The South American Physical Activity and Sedentary Behavior Network (SAPASEN). Int. J. Behav. Nutr. Phys. Act. 2019, 16, 1–11. [Google Scholar] [CrossRef]
- ENCAVI—Encuesta Nacional de Calidad de Vida y Salud—EPI—Departamento de Epidemiologia. Available online: http://epi.minsal.cl/encuesta-encavi/ (accessed on 18 January 2022).
- Ministerio de Salud Encuesta Nacional de Salud 2016-2017. Primeros Resultados. Available online: http://epi.minsal.cl/wp-content/uploads/2016/06/InformeENS_2009-2010_CAP1.pdf (accessed on 30 May 2022).
- Celis-Morales, C.; Salas, C.; Alduhishy, A.; Sanzana, R.; Martínez, M.A.; Leiva, A.; Diaz, X.; Martínez, C.; Álvarez, C.; Leppe, J.; et al. Socio-Demographic Patterns of Physical Activity and Sedentary Behaviour in Chile: Results from the National Health Survey 2009–2010. J. Public Health 2016, 38, e98–e105. [Google Scholar] [CrossRef]
- Cristi-Montero, C.; Sadarangani, K.P.; Garrido-Méndez, A.; Poblete-Valderrama, F.; Díaz-Martínez, X.; Celis-Morales, C. Relación Entre Niveles de Actividad Física y Sedentarismo Con Síndrome Metabólico. ENS Chile 2009-2010. Salud. Publica Mex. 2019, 61, 166–173. [Google Scholar] [CrossRef]
- Martínez, M.P.; Gallardo, I.; Martínez, M.P.; Gallardo, I. Reliability and Construct Validity of SF-12 to Measure Health Related Quality of Life in Chilean Subjects. Rev. Med. Chil. 2020, 148, 1568–1576. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E.; Kosinski, M.; Turner-Bowker, D.M.; Gandek, B. How to Score version 2 of the SF-12 health survey (with a supplement documenting version 1). QualityMetric Incorporated. 2002. Available online: http://pascal-francis.inist.fr/vibad/index.php?action=getRecordDetail&idt=28671750 (accessed on 30 January 2023).
- World Health Organization Physical Activity Guidelines. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 6 March 2022).
- Blair, S.N.; Connelly, J.C. How Much Physical Activity Should We Do? The Case for Moderate Amounts and Intensities of Physical Activity. Res. Q. Exerc. Sport 2013, 67, 193–205. [Google Scholar] [CrossRef]
- Yang, Y.J. An Overview of Current Physical Activity Recommendations in Primary Care. Korean J. Fam. Med. 2019, 40, 135. [Google Scholar] [CrossRef]
- de Craemer, M.; van Stappen, V.; Brondeel, R.; Iotova, V.; Chakarova, N.; Rurik, I.; Lindström, J.; Kivelä, J.; Moreno, L.A.; Mavrogianni, C.; et al. Self-Reported Lifestyle Behaviours in Families with an Increased Risk for Type 2 Diabetes across Six European Countries: A Cross-Sectional Analysis from the Feel4Diabetes-Study. BMC Endocr. Disord 2022, 22, 213. [Google Scholar] [CrossRef] [PubMed]
- Maheronnaghsh, S.; Vaz, M.; Shahedi, S.; Candidate, P. Occupational Sedentary Behaviour and Physical Activity among Office Workers of University of Porto: A Pilot Study. 2021. EasyChair Preprints. Available online: https://easychair.org/publications/preprint/TQGV (accessed on 30 January 2023).
- Concha-Cisternas, Y.; Petermann Rocha, F.; Garrido-Méndez, A.; Díaz-Martínez, X.; Leiva, A.M.; Salas-Bravo, C.; Martínez-Sanguinetti, M.A.; Iturra-González, J.A.; Matus, C.; Vásquez Gómez, J.A.; et al. Caracterización de Los Patrones de Actividad Física En Distintos Grupos Etarios Chilenos. Nutr. Hosp. 2018, 36, 149–158. [Google Scholar] [CrossRef]
- Fernández-Verdejo, R.; Suárez-Reyes, M.; Fernández-Verdejo, R.; Suárez-Reyes, M. Physical Inactivity versus Sedentariness: Analysis of the Chilean National Health Survey 2016-2017. Rev. Med. Chil. 2021, 149, 103–109. [Google Scholar] [CrossRef]
- Moreno-Llamas, A.; García-Mayor, J.; de la Cruz-Sánchez, E. Urban-Rural Differences in Trajectories of Physical Activity in Europe from 2002 to 2017. Health Place 2021, 69, 102570. [Google Scholar] [CrossRef]
- Wendt, A.; Machado, A.K.F.; Costa, C.S.; Blumenberg, C.; Ricardo, L.I.C.; Martins, R.C.; Mielke, G.I. Rural–Urban Differences in Physical Activity and TV-Viewing in Brazil. Rural Remote Health 2022, 22, 1–8. [Google Scholar] [CrossRef]
- Robertson, M.C.; Song, J.; Taylor, W.C.; Durand, C.P.; Basen-Engquist, K.M. Urban-Rural Differences in Aerobic Physical Activity, Muscle Strengthening Exercise, and Screen-Time Sedentary Behavior. J. Rural. Health 2018, 34, 401–410. [Google Scholar] [CrossRef]
- Sallis, J.F.; Cerin, E.; Conway, T.L.; Adams, M.A.; Frank, L.D.; Pratt, M.; Salvo, D.; Schipperijn, J.; Smith, G.; Cain, K.L.; et al. Physical Activity in Relation to Urban Environments in 14 Cities Worldwide: A Cross-Sectional Study. Lancet 2016, 387, 2207–2217. [Google Scholar] [CrossRef]
- Huang, N.C.; Kung, S.F.; Hu, S.C. The Relationship between Urbanization, the Built Environment, and Physical Activity among Older Adults in Taiwan. Int. J. Environ. Res. Public Health 2018, 15, 836. [Google Scholar] [CrossRef] [PubMed]
- Wicks, C.; Barton, J.; Orbell, S.; Andrews, L. Psychological Benefits of Outdoor Physical Activity in Natural versus Urban Environments: A Systematic Review and Meta-Analysis of Experimental Studies. Appl. Psychol. Health Well Being 2022, 14, 1037–1061. [Google Scholar] [CrossRef] [PubMed]
- Bornioli, A.; Parkhurst, G.; Morgan, P.L. The Psychological Wellbeing Benefits of Place Engagement during Walking in Urban Environments: A Qualitative Photo-Elicitation Study. Health Place 2018, 53, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Desarrollo Social; Subsecretaría de Servicios Sociales Ley-20670—Biblioteca Del Congreso Nacional. Available online: https://www.bcn.cl/leychile/navegar?idNorma=1051410 (accessed on 3 January 2023).
- Nieuwenhuijsen, M.J.; Dadvand, P.; Márquez, S.; Bartoll, X.; Barboza, E.P.; Cirach, M.; Borrell, C.; Zijlema, W.L. The Evaluation of the 3-30-300 Green Space Rule and Mental Health. Environ. Res. 2022, 215, 114387. [Google Scholar] [CrossRef] [PubMed]
- Marquez, D.X.; Aguinãga, S.; Vásquez, P.M.; Conroy, D.E.; Erickson, K.I.; Hillman, C.; Stillman, C.M.; Ballard, R.M.; Sheppard, B.B.; Petruzzello, S.J.; et al. A Systematic Review of Physical Activity and Quality of Life and Well-Being. Transl. Behav. Med. 2020, 10, 1098–1109. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Friedenreich, C.; Shiroma, E.J.; Lee, I.M. Physical Inactivity and Non-Communicable Disease Burden in Low-Income, Middle-Income and High-Income Countries. Br. J. Sports Med. 2022, 56, 101–106. [Google Scholar] [CrossRef]
- Hupin, D.; Roche, F.; Gremeaux, V.; Chatard, J.C.; Oriol, M.; Gaspoz, J.M.; Barthélémy, J.C.; Edouard, P. Even a Low-Dose of Moderate-to-Vigorous Physical Activity Reduces Mortality by 22% in Adults Aged ≥60 Years: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2015, 49, 1262–1267. [Google Scholar] [CrossRef]
- Ahmadi, M.N.; Clare, P.J.; Katzmarzyk, P.T.; del Pozo Cruz, B.; Lee, I.M.; Stamatakis, E. Vigorous Physical Activity, Incident Heart Disease, and Cancer: How Little Is Enough? Eur. Heart J. 2022, 43, 4801–4814. [Google Scholar] [CrossRef]
- Droomers, M.; Schrijvers, C.T.M.; Mackenbach, J.P. Educational Level and Decreases in Leisure Time Physical Activity: Predictors from the Longitudinal GLOBE Study. J. Epidemiol. Community Health (1978) 2001, 55, 562–568. [Google Scholar] [CrossRef]
- Kohl, H.W.; Cook, H.D. Educating the Student Body: Taking Physical Activity and Physical Education to School; The National Academies Press: Washington, DC, USA, 2013; pp. 1–488. [Google Scholar] [CrossRef]
- Miko, H.C.; Zillmann, N.; Ring-Dimitriou, S.; Dorner, T.E.; Titze, S.; Bauer, R. Effects of Physical Activity on Health. Gesundh. Suppl. 2020, 82, S184–S195. [Google Scholar] [CrossRef]
- Shin, C.N.; Lee, Y.S.; Belyea, M. Physical Activity, Benefits, and Barriers across the Aging Continuum. Appl. Nurs. Res. 2018, 44, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Skevington, S.M. Qualities of Life, Educational Level and Human Development: An International Investigation of Health. Soc. Psychiatry Psychiatr. Epidemiol. 2010, 45, 999–1009. [Google Scholar] [CrossRef] [PubMed]
- Han, K.T.; Park, E.C.; Kim, J.H.; Kim, S.J.; Park, S. Is Marital Status Associated with Quality of Life? Health Qual. Life Outcomes 2014, 12, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Purba, F.D.; Kumalasari, A.D.; Novianti, L.E.; Kendhawati, L.; Noer, A.H.; Ninin, R.H. Marriage and Quality of Life during COVID-19 Pandemic. PLoS ONE 2021, 16, e0256643. [Google Scholar] [CrossRef]
- Johannsen, D.L.; DeLany, J.P.; Frisard, M.I.; Welsch, M.A.; Rowley, C.K.; Fang, X.; Jazwinski, S.M.; Ravussin, E. Physical Activity in Aging: Comparison among Young, Aged, and Nonagenarian Individuals. J. Appl. Physiol. 2008, 105, 495–501. [Google Scholar] [CrossRef]
- Ingram, D.K. Age-Related Decline in Physical Activity: Generalization to Nonhumans. Med. Sci. Sports Exerc. 2000, 32, 1623–1629. [Google Scholar] [CrossRef]
| Total Sample (n = 6261) | Male (n = 2351) | Female (n = 3910) | p | ||
|---|---|---|---|---|---|
| Age c | 47.18 ± 18.60 | 47.09 ± 19.26 | 47.46 ± 18.29 | 0.623 a | |
| ≤44 | 2843 (45.41) | 1055 (44.87) | 1788 (45.73) | 0.752 b | |
| 45–59 | 1612 (25.75) | 606 (25.78) | 1006 (25.72) | ||
| ≥60 | 1806 (28.85) | 690 (29.35) | 1116 (28.54) | ||
| Marital Status | <0.001 b | ||||
| Single | 1593 (25.40) | 564 (24.00) | 1029 (26.30) | ||
| Married/partnered | 3763 (60.10) | 1486 (63.20) | 2277 (58.20) | ||
| DWW | 905 (14.50) | 301 (12.80) | 604 (15.04) | ||
| Residence Area | 0.001 b | ||||
| Urban | 5209 (83.20) | 2004 (85.20) | 3205 (82.00) | ||
| Rural | 1052 (16.80) | 347 (14.80) | 705 (18.00) | ||
| Educational Level | <0.001 b | ||||
| Low | 2395 (38.30) | 835 (35.50) | 1560 (39.90) | ||
| Medium | 2521 (40.30) | 959 (40.80) | 1562 (39.90) | ||
| High | 1345 (21.50) | 237 (23.70) | 788 (20.20) | ||
| Quality of Life c | <0.001 a | ||||
| PCS | 49.14 ± 9.58 | 50.41 ± 8.73 | 48.27 ± 10.09 | ||
| MCS | 51.65 ± 8.97 | 53.21 ± 7.99 | 51.03 ± 9.43 | ||
| WHO Parameters for Intense PA | |||
|---|---|---|---|
| Non-Compliant (<3 Days) | Compliant (≥3 Days) | p | |
| Inactive Person | Active Person | ||
| Total sample | 5236 (83.63) | 1025 (16.37) | |
| Gender | <0.001 b | ||
| Male | 1765 (33.70) | 586 (57.20) | |
| Female | 3471 (66.30) | 439 (42.80) | |
| Age | <0.001 b | ||
| ≤44 | 2216 (42.32) | 627 (61.17) | |
| 45–59 | 1332 (25.44) | 280 (27.32) | |
| ≥60 | 1688 (32.24) | 118 (11.51) | |
| Marital Status | 0.001 b | ||
| Single | 1310 (25.00) | 283 (27.60) | |
| Married/partnered | 3119 (59.60) | 644 (62.80) | |
| DWW | 807 (15.40) | 98 (9.60) | |
| Residence Area | <0.001 b | ||
| Urban | 4311 (82.30) | 898 (87.60) | |
| Rural | 925 (17.70) | 127 (12.40) | |
| Educational Level | <0.001 b | ||
| Low | 2144 (40.90) | 251 (24.50) | |
| Medium | 2015 (38.50) | 506 (49.40) | |
| High | 1077 (20.60) | 268 (26.10) | |
| Quality of Life c | <0.001 a | ||
| PCS | 48.35 ± 10.02 | 52.79 ± 6.37 | |
| MCS | 51.56 ± 9.19 | 53.29 ± 7.64 | |
| WHO Parameters for Moderate PA | ||||
|---|---|---|---|---|
| Non-Compliant (<5 days) | Compliant (≥5 days) | p | ||
| Inactive Person | Active Person | |||
| Total sample | 5220 (83.37) | 1041 (16.63) | ||
| Gender | <0.001 b | |||
| Male | 1842 (35.30) | 509 (48.90) | ||
| Female | 3378 (64.70) | 532 (51.10) | ||
| Age | <0.001 b | |||
| ≤44 | 2260 (43.30) | 583 (56.00) | ||
| 45–59 | 1336 (25.59) | 276 (26.51) | ||
| ≥60 | 1624 (31.11) | 182 (17.48) | ||
| Marital Status | <0.001 b | |||
| Single | 1338 (25.60) | 255 (24.50) | ||
| Married/partnered | 3070 (58.80) | 693 (66.60) | ||
| DWW | 812 (15.60) | 93 (8.90) | ||
| Residence Area | 0.030 b | |||
| Urban | 4319 (82.70) | 890 (85.50) | ||
| Rural | 901 (17.30) | 151 (14.50) | ||
| Educational Level | <0.001 b | |||
| Low | 2104 (40.30) | 291 (28.00) | ||
| Medium | 2035 (39.00) | 486 (46.70) | ||
| High | 1081 (20.70) | 264 (25.40) | ||
| Quality of Life c | <0.001 a | |||
| PCS | 48.49 ± 9.96 | 51.99 ± 7.29 | ||
| MCS | 51.45 ± 9.10 | 53.85 ± 8.04 | ||
| WHO Parameters for Intense PA (n = 1539) | WHO Parameters for Moderate PA (n = 2335) | |||||
|---|---|---|---|---|---|---|
| Non-Compliant (<75 min) | Compliant (≥75 min) | p | Non-Compliant (<150 min) | Compliant (≥150 min) | p | |
| Inactive Person | Active Person | Inactive Person | Active Person | |||
| Gender | 0.005 b | <0.001 b | ||||
| Male | 144 (45.00) | 655 (53.73) | 879 (44.94) | 208 (54.88) | ||
| Female | 176 (55.00) | 564 (46.27) | 1077 (55.06) | 171 (45.12) | ||
| Age | 0.006 b | 0.005 b | ||||
| ≤44 | 173 (54.06) | 775 (63.58) | 1170 (59.82) | 194 (51.19) | ||
| 45–59 | 97 (30.31) | 306 (25.10) | 472 (24.13) | 117 (30.87) | ||
| ≥60 | 50 (15.63) | 138 (11.32) | 314 (16.05) | 68 (17.94) | ||
| Marital Status | 0.087 b | 0.411 b | ||||
| Single | 69 (21.56) | 337 (27.65) | 476 (24.34) | 100 (26.39) | ||
| Married/partnered | 214 (66.88) | 757 (62.10) | 1276 (65.24) | 247 (65.17) | ||
| DWW | 37 (11.56) | 125 (10.25) | 204 (10.43) | 32 (8.44) | ||
| Residence Area | 0.327 b | 0.001 b | ||||
| Urban | 278 (86.88) | 1083 (88.84) | 1740 (88.96) | 314 (82.85) | ||
| Rural | 42 (13.13) | 136 (11.16) | 216 (11.04) | 65 (17.15) | ||
| Educational Level | 0.785 b | <0.001 b | ||||
| Low | 76 (23.75) | 306 (25.10) | 476 (24.34) | 111 (29.29) | ||
| Medium | 153 (47.81) | 557 (45.69) | 852 (43.56) | 212 (55.94) | ||
| High | 91 (28.44) | 356 (29.20) | 628 (32.11) | 56 (14.78) | ||
| Quality of Life c | ||||||
| PCS | 51.67 ± 7.14 | 52.89 ± 6.22 | 0.004 a | 51.35 ± 7.35 | 52.22 ± 6.75 | 0.001 a |
| MCS | 52.79 ± 7.92 | 54.66 ± 7.73 | < 0.001 a | 52.16 ± 8.93 | 54.00 ± 7.81 | <0.001 a |
| Sedentary Time | |||||
|---|---|---|---|---|---|
| Low (0–3 Hours) 1 | Moderate (4–6 Hours) 2 | High (≥7 Hours) 3 | p | Post Hoc c | |
| Total sample | 3319 (53.01) | 2232 (35.65) | 710 (11.34) | ||
| Gender | 0.002 a | ||||
| Male | 1202 (36.20) | 841 (37.70) | 308 (43.4) | ||
| Female | 2117 (63.80) | 1394 (62.30) | 402 (56.6) | ||
| Age | <0.001 a | ||||
| ≤44 | 1473 (44.38) | 1024 (45.88) | 346 (48.73) | ||
| 45–59 | 933 (28.11) | 508 (22.76) | 171 (24.08) | ||
| ≥60 | 913 (27.51) | 700 (31.36) | 193 (27.18) | ||
| Marital Status | <0.001 a | ||||
| Single | 837 (25.20) | 554 (24.80) | 202 (28.50) | ||
| Married/partnered | 2070 (62.40) | 1320 (59.10) | 373 (52.50) | ||
| DWW | 412 (12.40) | 358 (16.00) | 135 (19.00) | ||
| Residence Area | <0.001 a | ||||
| Urban | 2658 (80.10) | 1949 (87.30) | 602 (84.80) | ||
| Rural | 661 (19.90) | 283 (12.70) | 108 (15.20) | ||
| Educational Level | <0.001 a | ||||
| Low | 1304 (39.30) | 806 (36.10) | 285 (40.10) | ||
| Medium | 1379 (41.50) | 869 (38.90) | 273 (38.50) | ||
| High | 636 (19.20) | 57 (25.00) | 152 (21.40) | ||
| Quality of Life d | |||||
| PCS | 49.56 ± 8.94 | 49.07 ± 9.78 | 46.82 ± 11.93 | 0.027 b | 1 > 3; 2 > 3 |
| MCS | 51.82 ± 8.62 | 52.33 ± 9.23 | 50.42 ± 9.64 | <0.001 b | 1 > 3; 2 > 3 |
| Physical Component Summary | Mental Component Summary | ||||
|---|---|---|---|---|---|
| Scores < 50 | Scores < 50 | ||||
| Odds Ratio (95% CI) | p | Odds Ratio (95% CI) | p | ||
| Intense Physical Activity | |||||
| <3 days/week | 1.941 (1.631–2.311) | <0.001 | 1.189 (1.023–1.382) | 0.024 | |
| Gender (female) | 1.473 (1.307–1.660) | <0.001 | 1.513 (1.353–1.692) | <0.001 | |
| Age (≤44 years) | 0.273 (0.242–0.309) | <0.001 | 0.972 (0.868–1.089) | 0.624 | |
| Marital status (Married/partnered) | 0.765 (0.682–0.858) | <0.001 | 0.837 (0.752–0.931) | 0.001 | |
| Area (urban) | 0.921 (0.682–0.858) | 0.280 | 1.022 (0.887–1.178) | 0.760 | |
| Educational level (<8 years) | 2.170 (1.925–2.445) | <0.001 | 1.410 (1.255–1.584) | <0.001 | |
| Hosmer–Lemeshow test a | 0.376 | 0.523 | |||
| Moderate Physical Activity | |||||
| <5 days/week | 1.750 (1.484–2.064) | <0.001 | 1.458 (1.254–1.694) | <0.001 | |
| Gender (female) | 1.528 (1.357–1.719) | <0.001 | 1.507 (1.349–1.684) | <0.001 | |
| Age (≤44 years) | 0.268 (0.237–0.303) | <0.001 | 0.978 (0.873–1.095) | 0.694 | |
| Marital status (Married/partnered) | 0.777 (0.693–0.871) | <0.001 | 0.846 (0.761–0.942) | 0.002 | |
| Area (urban) | 0.912 (0.786–1.059) | 0.229 | 1.020 (0.885–1.176) | 0.781 | |
| Educational level (<8 years) | 2.195 (1.948–2.473) | <0.001 | 1.402 (1.247–1.575) | <0.001 | |
| Hosmer–Lemeshow test a | 0.548 | 0.663 | |||
| Sedentary Behavior | |||||
| ≥6 h/week | 1.475 (1.280–1.700) | <0.001 | 1.257 (1.103–1.433) | 0.001 | |
| Gender (female) | 1.615 (1.435–1.817) | <0.001 | 1.563 (1.400–1.746) | <0.001 | |
| Age (≤44 years) | 0.259 (0.229–0.293) | <0.001 | 0.954 (0.852–1.067) | 0.408 | |
| Marital status (Married/partnered) | 0.777 (0.693–0.872) | <0.001 | 0.846 (0.760–0.941) | 0.002 | |
| Area (urban) | 0.901 (0.776–1.046) | 0.171 | 1.011 (0.877–1.165) | 0.877 | |
| Educational level (<8 years) | 2.248 (1.996–2.532) | <0.001 | 1.423 (1.267–1.599) | <0.001 | |
| Hosmer–Lemeshow test a | 0.624 | 0.796 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gonzalez-Torres, C.; Yuing, T.; Berral-de la Rosa, F.; Lizana, P.A. Physical Inactivity, Sedentary Behavior and Quality of Life in the Chilean Population: ENCAVI Results, 2015–2016. Healthcare 2023, 11, 1020. https://doi.org/10.3390/healthcare11071020
Gonzalez-Torres C, Yuing T, Berral-de la Rosa F, Lizana PA. Physical Inactivity, Sedentary Behavior and Quality of Life in the Chilean Population: ENCAVI Results, 2015–2016. Healthcare. 2023; 11(7):1020. https://doi.org/10.3390/healthcare11071020
Chicago/Turabian StyleGonzalez-Torres, Carlos, Tuillang Yuing, Francisco Berral-de la Rosa, and Pablo A. Lizana. 2023. "Physical Inactivity, Sedentary Behavior and Quality of Life in the Chilean Population: ENCAVI Results, 2015–2016" Healthcare 11, no. 7: 1020. https://doi.org/10.3390/healthcare11071020
APA StyleGonzalez-Torres, C., Yuing, T., Berral-de la Rosa, F., & Lizana, P. A. (2023). Physical Inactivity, Sedentary Behavior and Quality of Life in the Chilean Population: ENCAVI Results, 2015–2016. Healthcare, 11(7), 1020. https://doi.org/10.3390/healthcare11071020


_MD__MPH_PhD.png)





