Female Medical Students’ Experiences of Sexism during Clinical Placements: A Qualitative Study
Abstract
1. Introduction
2. Methods
2.1. Study Design and Setting
2.2. Recruitment and Sampling
2.3. Data Collection
2.4. Patient and Public Involvement Statement
2.5. Data Analysis
3. Results
3.1. Theme 1: Experiences of Sexism
3.1.1. Sexual Harassment
“I have had my bum pinched once after taking someone’s bloods.”-P0003
“The elderly gentleman just pointed at my breasts and goes, “Look! Look at the size of those”. I didn’t know how to react. And all the staff just looked at me, didn’t say anything, and continued the consultation.”-P0016
“We didn’t exchange names or anything like that. So then in the evening, about 11 o’clock at night, he added me on Facebook. Presumably he got my name from my badge.”-P0014
“he’s like, Yeah, I’ll sign it off if you go out with me.”-P0002
3.1.2. Negative Teaching Experiences
“He just didn’t want to look at me, it was just so awkward.”-P0011
“He would speak to literally the boys and not speak to me.”-P0010
“They literally said to me “what is the point of me teaching you when you’re a woman and you’re just going to choose your babies over your career and want to be a GP anyway?”.”-P0013
3.1.3. Gendered Stereotyping
“I think nurses do an amazing job. And I’d be proud to be a nurse. But I worked really, really hard to get here. And I keep working hard. And it’s just frustrating when I get called nurse.”-P0007
“They just look at you and all they see is a carrier of children.”-P0006
“You get told that that specialty is not for you because you need to have children”-P0003
“I’ve been told that I should be a GP because it means that you can have a family”-P0008
3.1.4. Microaggressions
“Things that annoy me the most are when other medical students patronise me, because it happens a fair bit…it’s annoying that he would even think to say that when I’m sure he wouldn’t say that to a guy.”-P0001
“You don’t say sweetheart to the boys. Why? Because it feels very patronising.”-P0006
“It was always a male consultant overcompensating, saying that all of the female consultants were fantastic and don’t get me wrong. It’s nicer to hear something good than something terrible, but I sort of got the impression, it was a bit much, you know, almost like they were trying to prove a point”-P0003
3.2. Theme 2: Impact of Sexism
3.2.1. Emotional and Psychological Impacts
“It’s really disheartening”-P0004
“It makes it feel like the career that I want is just so out of reach just because of what I want outside of medicine”-P0010
“When I first was discovering how sexist medicine was, it got me so down and depressed, it made me really disengaged with the whole thing”-P0011
“It’s uncomfortable. Especially that it’s supposed to be a professional environment.”-P0005
“The decisions I’ve made for example not wanting to do surgery. It’s not based on that one session that I had, but it’s experiences like that, that happen over and over.”-P0017
“A passing comment it can really sit with you, and I’ll think about it for weeks after. Like I still think about it now and that was in July last year.”-P0004
3.2.2. Impact on Learning
“I never went back on the ward. That’s how I dealt with it.”-P0002
“That made me not really want to go to clinics anymore, and it’s changed where I was going to apply for my foundation year programme.”-P0013
“I was then missing the teachings so I was missing out on what I could have been taught.”-P0010
“When it comes from a teacher, a mentor, it affects me more”-P0012
“I literally, I couldn’t concentrate on anything!”-P0006
“You might be less likely to go, you might be less likely to listen, to trust them.”-P0003
“It can feel like a confidence knock”-P0012
3.2.3. Conscious Behavioural Changes
“It makes you more wary around what clothes I can wear.”-P0016
“I do feel a bit more protective over my name badge now. So I’ll try and cover it with my hair, or I won’t wear it as often.”-P0014
3.3. Theme 3: Barriers and Facilitators to Reporting
3.3.1. Hierarchy and Power Imbalance
“We shouldn’t, we can’t complain because he’s so much more senior than us.”-P0004
3.3.2. Negative Experiences and Futility of Reporting
“I’ve thought countless times shall I report them? But then I don’t know how.”-P0012
“I don’t actually know what the official reporting procedures are.”-P0009
“[Medical School Management] said ‘the goal of medical school is to provide a safe environment for men to make these mistakes so that when they qualify as a doctor, they don’t go on to make those mistakes… and lose their registration and harm patients’.”-P0011
“Barriers to reporting aren’t necessarily that the roots aren’t there, but the people that you’re reporting to don’t take it seriously.”-P0015
“I got an email from the uni being like, ‘we’ve seen your thing and we’re happy you brought this up to my attention. We’re going to make a forthcoming meeting with you to see what’s happened’. No one ever made a meeting. That was 11 weeks ago now.”-P0004
“They took his word over mine.”-P0016
“You have to prove something that’s happened, and a lot of things are very difficult to prove, because there is no objective proof you can provide.”-P0013
“Wellbeing got in touch with me saying, “we’re sorry this happened. We don’t know about feeding it back, but we can certainly do sessions to deal with your anxiety and help you”.”-P0011
“It’s not really worth putting all that effort into reporting it and not getting anywhere with it.”-P0014
“How bad does the sexism have to be for something to be done about it?”-P0007
“I don’t want to put myself at risk of anything bad happening, by reporting this.”-P0006
3.4. Theme 4: Student Recommendations
3.4.1. Raising Awareness and Empowering Students
“I think there should be some formal teaching at uni about what sexism can look like in the medical sphere, what they would like you to do about it. I think if uni were giving us a lecture saying- this is the reporting process, this is what it can look like, we will endorse and we will back you if you were to complain about it.”-P0011
“I think we could do with like a couple of communication sessions on how to deal with these things at the time, how to recognise them, we need a better reporting process in place and where to access the reporting system as well.”-P0014
“Medical school teaching us how to respond to issues and teaching us how to be able to report them would really help.”-P0012
“We don’t really teach men how to not be sexist.”-P0011
3.4.2. Improving Reporting Outcomes, Recognising the Severity of the Issue and Encouraging Reporting
“I guess the med school and hospitals could take the issue more seriously.”-P0015
“I think each trust should have a way of reporting sexism or sex discrimination…in an anonymous way.”-P0009
3.4.3. Provision of a Safe Space for Discussion
“More education earlier on in the degree, a harder stance against these issues and providing forums for people to share their experiences.”-P0017
4. Discussion
4.1. Reflexivity
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Swim, J.K.; Hyers, L.L. Sexism. Handbook of Prejudice, Stereotyping, and Discrimination. In Routledge Handbooks Online; Psychology Press: New York, NY, USA, 2009. [Google Scholar]
- Council of Europe. Recommendation on Preventing and Combating Sexism-Gender Matters-publi.coe.int. Gend Matters 2019. Available online: https://www.coe.int/en/web/gender-matters/recommendation-on-preventing-and-combating-sexism (accessed on 8 March 2023).
- White, G.E. Sexual harassment during medical training: The perceptions of medical students at a university medical school in Australia. Med. Educ. 2008, 34, 980–986. [Google Scholar] [CrossRef]
- Sexual Harassment in the Workplace|Equality and Human Rights Commission n.d. Available online: https://www.equalityhumanrights.com/en/sexual-harassment-workplace (accessed on 11 November 2021).
- United Nations Development Programme. Tackling Social Norms: A game Changer for Gender Inequalities; UNDP: New York, NY, USA, 2020. [Google Scholar] [CrossRef]
- Timmerman, G.; Bajema, C. Sexual Harassment in the Workplace in the European Union. Available online: https://www.un.org/womenwatch/osagi/pdf/shworkpl.pdf (accessed on 11 November 2022).
- Kraus, F.; Cebille, P. Survey: European Observatory on Sexism and Sexual Harassment at Work. Available online: https://feps-europe.eu/publication/697-survey-european-observatory-on-sexism-and-sexual-harassment-at-work/ (accessed on 11 November 2022).
- Adams, L.; Hilger, L.; Moselen, E.; Basi, T.; Gooding, O.; Hull, J. 2020 Sexual Harassment Survey; Government Equalities Office: London, UK, 2020. [Google Scholar]
- Gender Equality Policy Hub n.d. Available online: https://www.parliament.uk/mps-lords-and-offices/offices/commons/scrutinyunit/gender-equality-policy-map/ (accessed on 21 April 2022).
- Legislation.gov.uk. Equality Act 2010. Natl Arch n.d. Available online: https://www.legislation.gov.uk/ukpga/2010/15/contents (accessed on 24 January 2022).
- British Medical Association. Sexism in Medicine; BMA: London, UK, 2021. [Google Scholar]
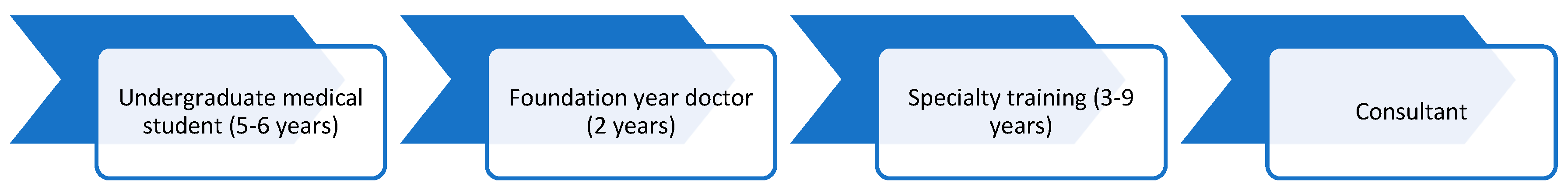
- Health Education England, South East. Training Pathway, School of Medicine. Work Kent Surrey Sussex n.d. Available online: https://kss.hee.nhs.uk/medicine/training-pathway/ (accessed on 12 February 2023).
- Fnais, N.; Soobiah, C.; Chen, M.H.; Lillie, E.; Perrier, L.; Tashkhandi, M.; Straus, S.E.; Mamdani, M.; Al-Omran, M.; Tricco, A.C. Harassment and Discrimination in Medical Training. Acad. Med. 2014, 89, 817–827. [Google Scholar] [CrossRef] [PubMed]
- BMA Survey Finds That Sexism Is Widespread in Medicine-BMA Media Centre-BMA. Br Med Assoc Trade Union Prof Body Dr UK n.d. Available online: https://www.bma.org.uk/bma-media-centre/bma-survey-finds-that-sexism-is-widespread-in-medicine (accessed on 9 November 2021).
- Carr, P.L.; Gunn, C.; Kaplan, S.A.; Raj, A.; Freund, K.M. Inadequate Progress for Women in Academic Medicine: Findings from the National Faculty Study. J. Women’s Health 2015, 24, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Bagenal, J.; Baxter, N. Sexual misconduct in medicine must end. Lancet 2022, 399, 1030–1032. [Google Scholar] [CrossRef] [PubMed]
- Fleming, S.; Fisher, R. Sexual assault in surgery: A painful truth. Bull. R. Coll. Surg. Engl. 2021, 103, 282–285. [Google Scholar] [CrossRef]
- Lay, K. MeToo Moment for NHS as Female Surgeons Speak out. The Times 2022. Available online: https://www.thetimes.co.uk/article/metoo-moment-for-nhs-as-female-surgeons-speak-out-qzw3tbs56 (accessed on 16 August 2022).
- Surviving in Scrubs. Surviv Scrubs n.d. Available online: https://survivinginscrubsorg.wordpress.com/ (accessed on 16 August 2022).
- General Medical Council. Awarding Bodies and New Schools. Gen Med Counc n.d. Available online: https://www.gmc-uk.org/education/reports-and-reviews/awarding-bodies-and-new-schools (accessed on 13 April 2022).
- University of Birmingham. Medical Students by Gender 2022. Available online: https://www.thecompleteuniversityguide.co.uk/universities/university-of-birmingham (accessed on 1 March 2023).
- University of Birmingham. Medical School Size 2021. Available online: https://www.birmingham.ac.uk/university/colleges/mds/about/study.aspx (accessed on 13 April 2022).
- Students O for. Medical and Dental Intakes-Office for Students. Off Stud 2019. Available online: https://www.officeforstudents.org.uk/advice-and-guidance/funding-for-providers/health-education-funding/medical-and-dental-intakes/ (accessed on 30 October 2021).
- Narrowing of NHS Gender Divide But Men Still the Majority in Senior Roles. NHS Digit n.d. Available online: https://digital.nhs.uk/news/2018/narrowing-of-nhs-gender-divide-but-men-still-the-majority-in-senior-roles (accessed on 13 April 2022).
- Stratton, T.D.; McLaughlin, M.A.; Witte, F.M.; Fosson, S.E.; Nora, L.M. Does Students? Exposure to Gender Discrimination and Sexual Harassment in Medical School Affect Specialty Choice and Residency Program Selection? Acad. Med. 2005, 80, 400–408. [Google Scholar] [CrossRef]
- Hirayama, M.; Fernando, S. Organisational barriers to and facilitators for female surgeons’ career progression: A systematic review. J. R. Soc. Med. 2018, 111, 324–334. [Google Scholar] [CrossRef]
- Harnois, C.E.; Bastos, J.L. Discrimination, Harassment, and Gendered Health Inequalities: Do Perceptions of Workplace Mistreatment Contribute to the Gender Gap in Self-reported Health? J. Health Soc. Behav. 2018, 59, 283–299. [Google Scholar] [CrossRef]
- Carr, P.L.; Szalacha, L.; Barnett, R.; Caswell, C.; Inui, T. A "Ton of Feathers": Gender Discrimination in Academic Medical Careers and How to Manage It. J. Women’s Health 2003, 12, 1009–1018. [Google Scholar] [CrossRef]
- Ilies, R.; Hauserman, N.; Schwochau, S.; Stibal, J. Reported Incidence Rates of Work-Related Sexual Harassment in the United States: Using Meta-Analysis to Explain Reported Rate Disparities. Pers. Psychol. 2003, 56, 607–631. [Google Scholar] [CrossRef]
- Najjar, I.; Socquet, J.; Gayet-Ageron, A.; Ricou, B.; Le Breton, J.; Rossel, A.; Abdulcadir, J.; Soroken, C.; Tessitore, E.; Gerstel, C.; et al. Prevalence and forms of gender discrimination and sexual harassment among medical students and physicians in French-speaking Switzerland: A survey. BMJ Open 2022, 12, e049520. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences, Engineering, and Medicine, Policy and Global Affairs, Committee on Women in Science, Engineering, and Medicine, Committee on the Impacts of Sexual Harassment in Academia. Sexual Harassment of Women: Climate, Culture, and Consequences in Academic Sciences, Engineering, and Medicine. Available online: https://pubmed.ncbi.nlm.nih.gov/29894119/ (accessed on 13 April 2022).
- Wigginton, B.; Lafrance, M.N. Learning critical feminist research: A brief introduction to feminist epistemologies and methodologies. Fem. Psychol. 2019. [Google Scholar] [CrossRef]
- Harding, S.; Norberg, K. New Feminist Approaches to Social Science Methodologies: An Introduction. Signs J. Women Cult. Soc. 2005, 30, 2009–2015. [Google Scholar] [CrossRef]
- Riger, S. Epistemological debates, feminist voices: Science, social values, and the study of women. Am. Psychol. 1992, 47, 730–740. [Google Scholar] [CrossRef]
- University of Birmingham. MDS Student Reporting n.d. Available online: https://fd7.formdesk.com/universityofbirmingham/mds-student-reporting (accessed on 8 May 2022).
- Samuriwo, R.; Patel, Y.; Webb, K.; Bullock, A. ‘Man up’: Medical students’ perceptions of gender and learning in clinical practice: A qualitative study. Med. Educ. 2019, 54, 150–161. [Google Scholar] [CrossRef]
- Broad, J.; Matheson, M.; Verrall, F.; Taylor, A.K.; Zahra, D.; Alldridge, L.; Feder, G. Discrimination, harassment and non-reporting in UK medical education. Med. Educ. 2018, 52, 414–426. [Google Scholar] [CrossRef]
- Colenbrander, L.; Causer, L.; Haire, B. ‘If you can’t make it, you’re not tough enough to do medicine’: A qualitative study of Sydney-based medical students’ experiences of bullying and harassment in clinical settings. BMC Med. Educ. 2020, 20, 86. [Google Scholar] [CrossRef] [PubMed]
- Binder, R.; Garcia, P.; Johnson, B.; Fuentes-Afflick, E. Sexual Harassment in Medical Schools: The Challenge of Covert Retaliation as a Barrier to Reporting. Acad. Med. 2018, 93, 1770–1773. [Google Scholar] [CrossRef]
- Care Quality Commission. Fear of Raising Concerns about Care; CQC: London, UK, 2013. [Google Scholar]
- Ekpenyong, M.S.; Nyashanu, M.; Ibrahim, A.; Serrant, L. Perceived barriers to whistle blowing in healthcare amongst healthcare professionals: An integrative review. Int. J. Hum. Rights Health 2020, 14, 10–27. [Google Scholar] [CrossRef]
- Pritlove, C.; Juando-Prats, C.; Ala-Leppilampi, K.; Parsons, J.A. The good, the bad, and the ugly of implicit bias. Lancet 2019, 393, 502–504. [Google Scholar] [CrossRef]
- Fitzgerald, C.; Hurst, S. Implicit bias in healthcare professionals: A systematic review. BMC Med. Ethic 2017, 18, 19. [Google Scholar] [CrossRef] [PubMed]
- Chopik, W.J.; Giasson, H.L. Age Differences in Explicit and Implicit Age Attitudes Across the Life Span. Gerontologist 2017, 57, S169–S177. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, J.; Oakley, A. What Is Feminism?/Edited by Juliet Mitchell & Ann Oakley; Basil Blackwell: Oxford, UK, 1986. [Google Scholar]
- Office for Students. Prevent and Address Harassment and Sexual Misconduct-Statement of Expectations 2020. Available online: https://www.officeforstudents.org.uk/advice-and-guidance/student-wellbeing-and-protection/prevent-and-address-harassment-and-sexual-misconduct/statement-of-expectations/ (accessed on 26 February 2023).
- General Medical Council. Guidance on Undergraduate Clinical Placements n.d. Available online: https://www.gmc-uk.org/education/standards-guidance-and-curricula/guidance/undergraduate-clinical-placements/guidance-on-undergraduate-clinical-placements (accessed on 26 February 2023).
- Riley, R.; Buszewicz, M.; Kokab, F.; Teoh, K.; Gopfert, A.; Taylor, A.K.; Van Hove, M.; Martin, J.; Appleby, L.; Chew-Graham, C. Sources of work-related psychological distress experienced by UK-wide foundation and junior doctors: A qualitative study. BMJ Open 2021, 11, e043521. [Google Scholar] [CrossRef] [PubMed]
- Dardenne, B.; Dumont, M.; Bollier, T. Insidious dangers of benevolent sexism: Consequences for women’s performance. J. Pers. Soc. Psychol. 2007, 93, 764–779. [Google Scholar] [CrossRef]
- Rubin, M.; Paolini, S.; Subašić, E.; Giacomini, A. A confirmatory study of the relations between workplace sexism, sense of belonging, mental health, and job satisfaction among women in male-dominated industries. J. Appl. Soc. Psychol. 2019, 49, 267–282. [Google Scholar] [CrossRef]
- Sojo, V.E.; Wood, R.E.; Genat, A. Harmful Workplace Experiences and Women’s Occupational Well-Being. Psychol. Women Q. 2015, 40, 10–40. [Google Scholar] [CrossRef]
- Roberge, M.; van Dick, R. Recognizing the benefits of diversity: When and how does diversity increase group performance? Hum. Resour. Manag. Rev. 2010, 20, 295–308. [Google Scholar] [CrossRef]
- McIntosh, P. White Privilege: Unpacking the Invisible Knapsack (1989) 1. In On Privilege, Fraudulence, and Teaching as Learning, 1st ed.; Routledge: Oxfordshire, UK, 2019; pp. 29–34. [Google Scholar] [CrossRef]
- McIntosh, P. White Privilege and Male Privilege: A Personal Account of Coming to See Correspondences through Work in Women’s Studies (1988) 1. In On Privilege, Fraudulence, and Teaching as Learning, 1st ed.; Routledge: Oxfordshire, UK, 2019; pp. 17–28. [Google Scholar] [CrossRef]
- Fenton, R.A.; Mott, H.L.; McCartan, K.; Rumney, P.N. A Review of Evidence for Bystander Intervention to Prevent Sexual and Domestic Violence in Universities; University of the West of England: Bristol, UK, 2016. [Google Scholar]
- What Is Allyship? A Quick Guide. Incl Empl 2022. Available online: https://www.inclusiveemployers.co.uk/blog/quick-guide-to-allyship/ (accessed on 16 February 2023).
- Tsouroufli, M. Breaking in and breaking out a medical school: Feminist academic interrupted? Equal. Divers. Incl. Int. J. 2012, 31, 467–483. [Google Scholar] [CrossRef]
- Yang, H.-C. What Should Be Taught and What Is Taught: Integrating Gender into Medical and Health Professions Education for Medical and Nursing Students. Int. J. Environ. Res. Public Health 2020, 17, 6555. [Google Scholar] [CrossRef]
- Mitchell, K.S.; Freitag, J.L. Forum Theatre for Bystanders. Violence Against Women 2011, 17, 990–1013. [Google Scholar] [CrossRef]
- Thomson, D.M.; Wood, J.T. Rewriting Gendered Scripts: Using Forum Theatre to Teach Feminist Agency. Fem. Teach. 2001, 13, 202–212. [Google Scholar]
- Webb, F.E.; Gibbons, K.; El-Ahwany, N.L. Tackling sexist inequality in medical school. BMJ 2021, 374, n2302. [Google Scholar] [CrossRef] [PubMed]
- Campbell, R.; Wasco, S.M. Feminist Approaches to Social Science: Epistemological and Methodological Tenets. Am. J. Community Psychol. 2000, 28, 773–791. [Google Scholar] [CrossRef] [PubMed]
- Nagy Hesse-Biber, S. Feminist Research Practice: A Primer n.d. Available online: https://birmingham-primo.hosted.exlibrisgroup.com/primo-explore/fulldisplay (accessed on 8 May 2022).
| English speaking |
| Woman or non-binary |
| University of X medical student |
| Clinical years (3–5) |
| Have experienced sexism on placement |
| Access to device with stable internet connection to carry out interview |
| Demographic | Category | Number |
|---|---|---|
| Gender | Woman | 17 |
| Ethnicity | Asian Indian | 4 |
| Mixed Asian + White | 2 | |
| White British | 11 | |
| Disability | No | 17 |
| Year group | 3 | 4 |
| 4 | 4 | |
| 5 | 9 | |
| Graduate entry | No | 14 |
| Yes | 3 | |
| Religion | Christian | 3 |
| Hindu | 3 | |
| Muslim | 1 | |
| No religion | 10 | |
| Sexual orientation | Straight | 12 |
| Gay | 1 | |
| Bisexual | 3 | |
| Other | 1 |
| Major Themes | Sub-Themes |
|---|---|
| Sexual harassment |
| Negative teaching experiences | |
| Gendered stereotyping | |
| Microaggressions | |
| Emotional and psychological impacts |
| Impact on learning | |
| Conscious behavioural changes | |
| Hierarchy and power imbalance |
| Negative experiences and futility of reporting | |
| Raising awareness and empowering students |
| Improving reporting outcomes, recognising the severity of the issue and encouraging reporting | |
| Provision of safe space for discussion |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ibrahim, D.; Riley, R. Female Medical Students’ Experiences of Sexism during Clinical Placements: A Qualitative Study. Healthcare 2023, 11, 1002. https://doi.org/10.3390/healthcare11071002
Ibrahim D, Riley R. Female Medical Students’ Experiences of Sexism during Clinical Placements: A Qualitative Study. Healthcare. 2023; 11(7):1002. https://doi.org/10.3390/healthcare11071002
Chicago/Turabian StyleIbrahim, Darya, and Ruth Riley. 2023. "Female Medical Students’ Experiences of Sexism during Clinical Placements: A Qualitative Study" Healthcare 11, no. 7: 1002. https://doi.org/10.3390/healthcare11071002
APA StyleIbrahim, D., & Riley, R. (2023). Female Medical Students’ Experiences of Sexism during Clinical Placements: A Qualitative Study. Healthcare, 11(7), 1002. https://doi.org/10.3390/healthcare11071002






