Prevalence of Work-Related Musculoskeletal Disorders and Its Effects amongst Nurses in the Selected Intellectual Disability Unit of the Limpopo Province
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Site
2.2. Population and Sampling
2.3. Data Collection
2.4. Data Analysis
2.5. Reliability and Validity of the Study
3. Presentation of Results
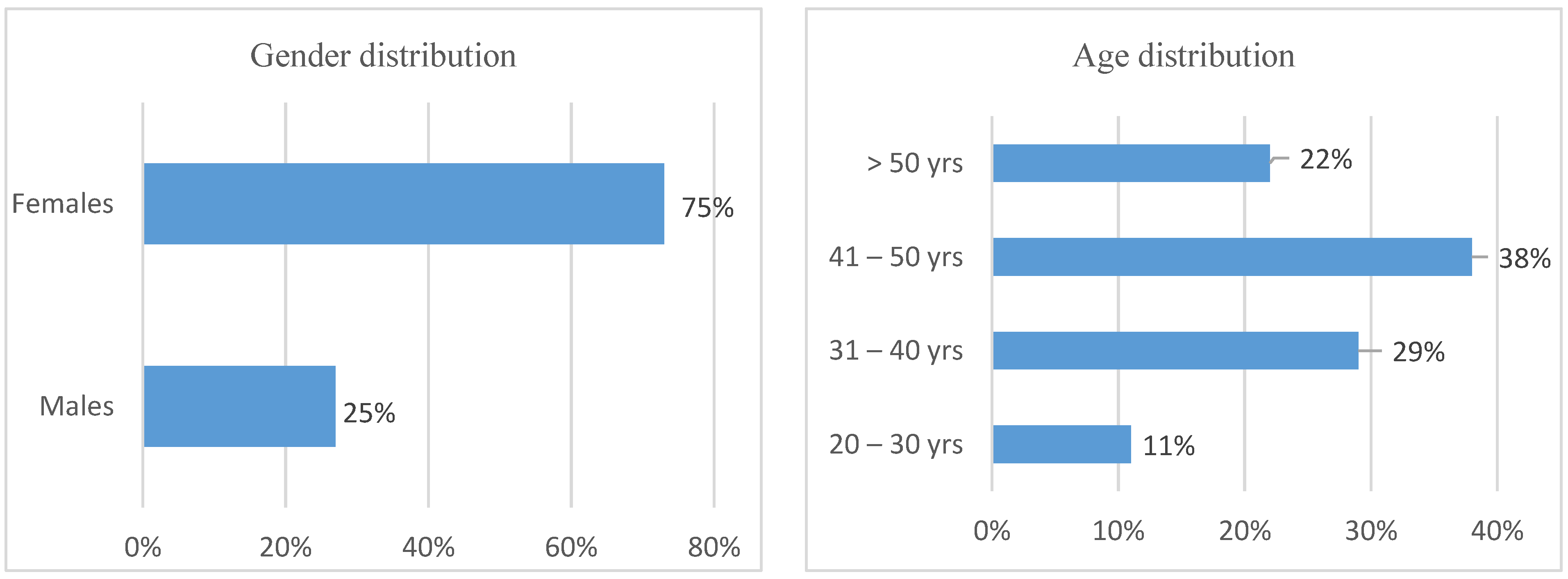
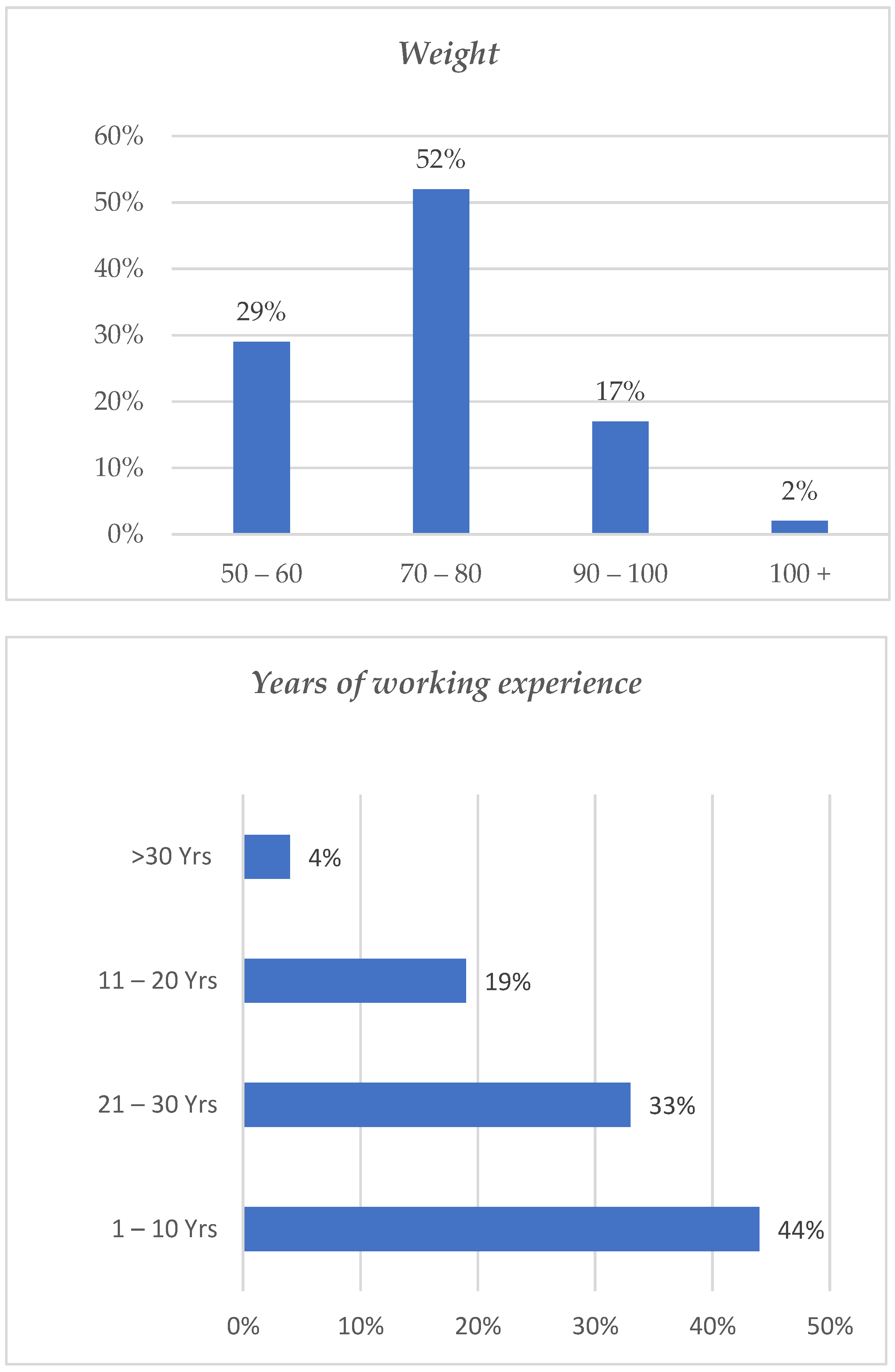
Demographic Profile of the Participants
4. Discussion of Research Results
Limitation of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO/ILO: Almost 2 Million People Die from Work-Related Causes Each Year. Available online: https://www.who.int/news/item/16-09-2021-who-ilo-almost-2-million-people-die-from-work-related-causes-each-year#:~:text=Occupational%20injuries%20caused%2019%20perergonomic%20risk%20factors%2C%20and%20noise (accessed on 15 December 2020).
- Odebiyi, D.O.; Okafor, U.A. Musculoskeletal Disorders, Workplace Ergonomics and Injury Prevention. In Ergonomics—New Insights; Intech Open: London, UK, 2023. [Google Scholar]
- Yan, P.; Li, F.; Zhang, L.; Yang, Y.; Huang, A.; Wang, Y.; Yao, H. Prevalence of Work-Related Musculoskeletal Disorders in the Nurses Working in Hospitals of Xinjiang Uygur Autonomous Region. Pain Res. Manag. 2017, 2017, 5757108. [Google Scholar] [CrossRef] [PubMed]
- Attar, S.M. Frequency and risk factors of musculoskeletal pain in nurses at a tertiary centre in Jeddah, Saudi Arabia: A cross sectional study. BMC Res. Notes 2014, 7, 61. [Google Scholar] [CrossRef] [PubMed]
- Arsalani, N.; Fallahi-Khoshknab, M.; Josephson, M.; Lagerström, M. Musculoskeletal Disorders and Working Conditions Among Iranian Nursing Personnel. Int. J. Occup. Saf. Ergon. 2014, 20, 671–680. [Google Scholar] [CrossRef]
- Kasa, A.S.; Workineh, Y.; Ayalew, E.; Temesgen, W.A. Low back pain among nurses working in clinical settings of Africa: Systematic review and meta-analysis of 19 years of studies. BMC Musculoskelet. Disord. 2020, 21, 310. [Google Scholar] [CrossRef]
- Abla Kofi-Bediako, W.; Sama, G.; Yarfi, C.; Ed-Bansah, D.; Appah Acquah, A. Work-Related Musculoskeletal Disorders among Nurses at the Ho Teaching Hospital, Ghana. In Proceedings of the 2021 HFES 65th International Annual Meeting, Baltimore, MD, USA, 3–8 October 2021; SAGE Publications: Los Angeles, CA, USA, 2021; Volume 65, pp. 1291–1294. [Google Scholar]
- Davis, K.; Dunning, K.; Jewell, G.; Lockey, J. Cost and disability trends of work-related musculoskeletal disorders in Ohio. Occup. Med. 2014, 64, 608–615. [Google Scholar] [CrossRef]
- National Academy of Sciences. Musculoskeletal Disorders and the Workplace: Low Back and Upper Extremities; National Academy Press: Washington, DC, USA, 2001. [Google Scholar]
- Kgakge, K.; Hlongwa, M.; Ginindza, T. The distribution of work-related musculoskeletal disorders among nurses in sub-Saharan Africa: A scoping review protocol. Syst. Rev. 2021, 10, 229. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-F.; Yeh, C.-M.; Huang, S.-L.; Ho, C.-C.; Li, R.-H.; Wang, W.-H.; Tang, F.-C. Work Ability and Quality of Life in Patients with Work-Related Musculoskeletal Disorders. Int. J. Environ. Res. Public Health 2020, 17, 3310. [Google Scholar] [CrossRef]
- Brien, K.; Lukhele, Z.; Nhlapo, J.M.; Pieterse, A.; Swanepoel, A.; Wagener, L.; Mashola, M.K. Work-related musculoskeletal disorders in nurses working in South African spinal cord rehabilitation units. Int. J. Afr. Nurs. Sci. 2018, 8, 107–111. [Google Scholar] [CrossRef]
- Albanesi, B.; Piredda, M.; Bravi, M.; Bressi, F.; Gualandi, R.; Marchetti, A.; Facchinetti, G.; Ianni, A.; Cordella, F.; Zollo, L.; et al. Interventions to prevent and reduce work-related musculoskeletal injuries and pain among healthcare professionals. A comprehensive systematic review of the literature. J. Saf. Res. 2022, 82, 124–143. [Google Scholar] [CrossRef]
- Denge, T.; Rakhudu, M. Perceptions of nurses on occupational health hazards and safety practices in Ditsobotla public hospitals in North-West province. Curationis J. Democr. Nurs. Organ. S. Afr. 2022, 45, 2220. [Google Scholar] [CrossRef]
- Amare, T.G.; Tesfaye, T.T.; Girmay, B.; Gebreagziabher, T.T. Exposure to Occupational Health Hazards Among Nursing and Midwifery Students During Clinical Practice. Risk Manag. Healthc. Policy 2021, 14, 2211. [Google Scholar] [CrossRef] [PubMed]
- Shree, A.; Shukla, P.C. Intellectual Disability: Definition, classification, causes and characteristics. Learn. Community Int. J. Educ. Soc. Dev. 2016, 7, 9. [Google Scholar] [CrossRef]
- Doody, O.; Slevin, E.; Taggart, L. A survey of nursing and multidisciplinary team members’ perspectives on the perceived contribution of intellectual disability clinical nurse specialists. J. Clin. Nurs. 2019, 28, 3879–3889. [Google Scholar] [CrossRef]
- Friese, T.; Ailey, S. Specific standards of care for adults with intellectual disabilities. Nurs. Manag. 2015, 22, 32–37. [Google Scholar] [CrossRef]
- Saberipour, B.; Ghanbari, S.; Zarea, K.; Gheibizadeh, M.; Zahedian, M. Investigating prevalence of musculoskeletal disorders among Iranian nurses: A systematic review and meta-analysis. Clin. Epidemiol. Glob. Health 2019, 7, 513–518. [Google Scholar] [CrossRef]
- Heidari, M.; Borujeni, M.G.; Rezaei, P.; Abyaneh, S.K. Work-Related Musculoskeletal Disorders and Their Associated Factors in Nurses: A Cross-Sectional Study in Iran. Malays. J. Med. Sci. 2019, 26, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.-Y.K.; Wong, M.-T.; Yu, Y.-C.; Ju, Y.-Y. Work-related musculoskeletal disorders and ergonomic risk factors in special education teachers and teacher’s aides. BMC Public Health 2016, 16, 137. [Google Scholar] [CrossRef]
- Luan, H.D.; Hai, N.T.; Xanh, P.T.; Giang, H.T.; Van Thuc, P.; Hong, N.M.; Khue, P.M. Musculoskeletal disorders: Prevalence and associated factors among district hospital nurses in Haiphong, Vietnam. BioMed Res. Int. 2018, 2018, 3162564. [Google Scholar] [CrossRef]
- Munabi, I.G.; Buwembo, W.; Kitara, D.L.; Ochieng, J.; Mwaka, E.S. Musculoskeletal disorder risk factors among nursing professionals in low resource settings: A cross-sectional study in Uganda. BMC Nurs. 2014, 13, 7. [Google Scholar] [CrossRef]
- Chiwaridzo, M.; Makotore, V.; Dambi, J.M.; Munambah, N.; Mhlanga, M. Work-related musculoskeletal disorders among registered general nurses: A case of a large central hospital in Harare, Zimbabwe. BMC Res. Notes 2018, 11, 315. [Google Scholar] [CrossRef] [PubMed]
- Tinubu, B.M.S.; Mbada, C.E.; Oyeyemi, A.L.; Fabunmi, A.A. Work-Related Musculoskeletal Disorders among Nurses in Ibadan, South-west Nigeria: A cross-sectional survey. BMC Musculoskelet. Disord. 2010, 11, 12. [Google Scholar] [CrossRef]
- Akodu, A.K.; Ashalejo, Z.O. Work-related musculoskeletal disorders and work ability among hospital nurses. J. Taibah Univ. Med. Sci. 2019, 14, 252–261. [Google Scholar] [CrossRef] [PubMed]
- Khumalo, K.; Haffejee, F. Prevalence and associated risk factors of low back pain among users of a primary health care clinic serving semi-urban and rural settlements in KwaZulu-Natal, South Africa. Afr. Health Sci. 2022, 22, 592–601. [Google Scholar] [CrossRef]
- Mutanda, T.; Mwaka, E.; Sekimpi, P.; Ntuulo, J. Occupation-related musculoskeletal disorders among nurses at the National Referral Hospital, Mulago in Uganda. Occup. Med. Health Aff. 2017, 5, 3. [Google Scholar] [CrossRef]
- Krishnan, K.S.; Raju, G.; Shawkataly, O. Prevalence of Work-Related Musculoskeletal Disorders: Psychological and Physical Risk Factors. Int. J. Environ. Res. Public Health 2021, 18, 9361. [Google Scholar] [CrossRef] [PubMed]
- Tariah, H.A.; Nafai, S.; Alajmi, M.; Almutairi, F.; Alanazi, B. Work-related musculoskeletal disorders in nurses working in the Kingdom of Saudi Arabia. Work 2020, 65, 421–428. [Google Scholar] [CrossRef]
- Taghinejad, H.; Azadi, A.; Suhrabi, Z.; Sayedinia, M. Musculoskeletal Disorders and Their Related Risk Factors Among Iranian Nurses. Biotechnol. Health Sci. 2016, 3, e34473. [Google Scholar] [CrossRef]
- Appelgren, M.; Bahtsevani, C.; Persson, K.; Borglin, G. Nurses’ experiences of caring for patients with intellectual developmental disorders: A systematic review using a meta-ethnographic approach. BMC Nurs. 2018, 17, 51. [Google Scholar] [CrossRef]
- Maree, K.; Pietersen, J. Sampling. In First Step in Research, 2nd ed.; Maree, K., Ed.; Van Schaik Publisher: Pretoria, South Africa, 2016; pp. 192–202. [Google Scholar]
- Brink, H.; Van der Walt, C.; Van Rensburg, G. Fundamentals of Research Methodology for Health Care Professionals; Juta and Company Ltd.: Western Cape, South Africa, 2018. [Google Scholar]
- Leedy, P.; Ormrod, J. Practical Research: Planning and Design, 11th ed.; Pearson: London, UK, 2015. [Google Scholar]
- Yasobant, S.; Rajkumar, P. Work-related musculoskeletal disorders among health care professionals: A cross-sectional assessment of risk factors in a tertiary hospital, India. Indian J. Occup. Environ. Med. 2014, 18, 75–81. [Google Scholar] [CrossRef]
- Zayed, H.A.; Saied, S.M.; El-Sallamy, R.M.; Shehata, W.M. Work-related musculoskeletal disorders among nursing staff of Tanta University Hospitals: Pattern, risk factors, and coping strategies. Egypt. J. Community Med. 2019, 37, 51–61. [Google Scholar]
- Naushad, A.; Alsaraeji, Z.; Ruhumbika, Y.; Isong, E.U.; Alfoteih, Y. The prevelence of work-related musculoskeletal disorders among the nurses in Dubai: Occupational health study. Med. Leg. Update 2019, 19, 156–160. [Google Scholar] [CrossRef]
- Anap, D.; Iyer, C.; Rao, K. Work related musculoskeletal disorders among hospital nurses in rural Maharashtra, India: A multi centre survey. Int. J. Res. Med. Sci. 2013, 1, 101–107. [Google Scholar] [CrossRef]
- Sethi, J.; Sandhu, J.S.; Imbanathan, V. Effect of Body Mass Index on work related musculoskeletal discomfort and occupational stress of computer workers in a developed ergonomic setup. BMC Sports Sci. Med. Rehabil. 2011, 3, 22. [Google Scholar] [CrossRef]
- Karkousha, R.N.; Elhafeza, H.M. Relation between the prevelance of work-related musculoskeletal disorders and years of job experience among workers of Nag Hammadi sugar factory in Egypt. Bull. Fac. Phys. Ther. 2017, 22, 23–26. [Google Scholar]
- Rypicz, Ł.; Karniej, P.; Witczak, I.; Kołcz, A. Evaluation of the occurrence of work-related musculoskeletal pain among anesthesiology, intensive care, and surgical nurses: An observational and descriptive study. Nurs. Health Sci. 2020, 22, 1056–1064. [Google Scholar] [CrossRef]
- Lin, S.C.; Lin, L.L.; Liu, C.J.; Fang, C.K.; Lin, M.H. Exploring the factors affecting musculoskeletal disorders risk among hospital nurses. PLoS ONE 2020, 15, e0231319. [Google Scholar] [CrossRef] [PubMed]
- Bhimani, R. Prevention of Work-related Musculoskeletal Injuries in Rehabilitation Nursing. Rehabil. Nurs. 2016, 41, 326–335. [Google Scholar] [CrossRef]
- Teeple, E.; Collins, J.E.; Shrestha, S.; Dennerlein, J.T.; Losina, E.; Katz, J.N. Outcomes of safe patient handling and mobilization programs: A meta-analysis. Work 2017, 58, 173–184. [Google Scholar] [CrossRef]
- Lee, S.-J.; Rempel, D. Comparison of lift use, perceptions, and musculoskeletal symptoms between ceiling lifts and floor-based lifts in patient handling. Appl. Ergon. 2020, 82, 102954. [Google Scholar] [CrossRef]
- Mbombi, M.O.; Mothiba, T.M.; Malema, R.N.; Malatji, M. The effects of absenteeism on nurses remaining on duty at a tertiary hospital of Limpopo province. Curationis 2018, 41, 1–5. [Google Scholar] [CrossRef]

| WMSD | Age Category | |||
|---|---|---|---|---|
| Pain | 20–30 | 31–40 | 41–50 | 50+ |
| Pains aggravated by work | 0 (0%) | 1 (12.5%) | 2 (25%) | 4 (50%) |
| Time of working limited due to pain | 0 (0%) | 2 (25%) | 3 (37.5%) | 2 (25%) |
| Experienced pain after lifting patients | 0 (0%) | 1 (12.5%) | 2 (25%) | 1 (12.5%) |
| Experienced pain after longstanding | 0 (0%) | 4 (50%) | 1 (12.5%) | 3 (37.5%) |
| Discomfort, Strains, Sprains, and Tears | ||||
| Discomfort, Strains, Sprains, and Tears aggravated by work | 1 (5%) | 2 (9%) | 1 (5%) | 3 (14%) |
| Time of working limited due to Discomfort, Strains, Sprains, and Tears | 2 (9%) | 0 (0%) | 1 (5%) | 2 (9%) |
| Experienced Discomfort, Strains, Sprains, and Tears after lifting patients | 1 (5%) | 1 (5%) | 2 (9%) | 1 (5%) |
| Experienced Discomfort, Strains, Sprains, and Tears after longstanding | 1 (5%) | 1 (5%) | 1 (5%) | 1 (5%) |
| Effects | WMSD | |
|---|---|---|
| Yes | No | |
| Absenteeism from work due WMSD | 31 (62%) | 19 (38%) |
| Change of working station due to WMSD | 31 (62%) | 19 (38%) |
| Missed work due to WMSD | 29 (58%) | 21 (42%) |
| WMSD interferes with the daily routine | 24 (48%) | 26 (52%) |
| Current work-related WMSD disturbs sleeping patterns | 26 (52%) | 24 (48%) |
| Risk Factors | WMSD | p-Value | |
|---|---|---|---|
| Yes | No | ||
| Age | 0.0130 | ||
| 20–30 | 0 (0%) | 8 (19%) | |
| 31–40 | 8 (31%) | 12 (28%) | |
| 41–50 | 8 (31%) | 18 (41%) | |
| 50+ | 10 (38%) | 5 (12%) | |
| Gender | 0.9230 | ||
| Male | 8 (31%) | 9 (21%) | |
| Female | 18 (69%) | 34 (79%) | |
| Years of Experience | 0.1640 | ||
| 1–10 | 7 (27%) | 23 (44%) | |
| 11–20 | 11 (42%) | 12 (28%) | |
| 21–30 | 6 (23%) | 7 (16%) | |
| 30+ | 2 (8%) | 1 (2%) | |
| Years in same unit | 0.3880 | ||
| 1–2 | 12 (46%) | 27 (63%) | |
| 3–4 | 9 (35%) | 13 (30%) | |
| 5–6 | 3 (12%) | 2 (8%) | |
| 7+ | 2 (8%) | 1 (2%) | |
| Hours of work per day | 0.92300 | ||
| 8 | 1 (4%) | 1 (2%) | |
| 12 | 23 (92%) | 39 (93%) | |
| 12+ | 1 (4%) | 2 (5%) | |
| Same position more than two hours | |||
| Yes | 10 (38%) | 14 (33%) | |
| No | 16 (62%) | 29 (67%) | |
| Patient lifting | 0.0320 | ||
| Yes | 23 (89%) | 28 (65%) | |
| No | 3 (11%) | 15 (35%) | |
| Extra job | 0.8650 | ||
| Yes | 21 (81%) | 34 (79%) | |
| No | 5 (19%) | 9 (21%) | |
| No enough resting during the day | 0.2470 | ||
| Yes | 14 (54%) | 17 (40%) | |
| No | 12 (46%) | 26 (60%) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muthelo, L.; Sinyegwe, N.F.; Phukubye, T.A.; Mbombi, M.O.; Ntho, T.A.; Mothiba, T.M. Prevalence of Work-Related Musculoskeletal Disorders and Its Effects amongst Nurses in the Selected Intellectual Disability Unit of the Limpopo Province. Healthcare 2023, 11, 777. https://doi.org/10.3390/healthcare11050777
Muthelo L, Sinyegwe NF, Phukubye TA, Mbombi MO, Ntho TA, Mothiba TM. Prevalence of Work-Related Musculoskeletal Disorders and Its Effects amongst Nurses in the Selected Intellectual Disability Unit of the Limpopo Province. Healthcare. 2023; 11(5):777. https://doi.org/10.3390/healthcare11050777
Chicago/Turabian StyleMuthelo, Livhuwani, Nakisani Faith Sinyegwe, Thabo Arthur Phukubye, Masenyani Oupa Mbombi, Tshepo Albert Ntho, and Tebogo Maria Mothiba. 2023. "Prevalence of Work-Related Musculoskeletal Disorders and Its Effects amongst Nurses in the Selected Intellectual Disability Unit of the Limpopo Province" Healthcare 11, no. 5: 777. https://doi.org/10.3390/healthcare11050777
APA StyleMuthelo, L., Sinyegwe, N. F., Phukubye, T. A., Mbombi, M. O., Ntho, T. A., & Mothiba, T. M. (2023). Prevalence of Work-Related Musculoskeletal Disorders and Its Effects amongst Nurses in the Selected Intellectual Disability Unit of the Limpopo Province. Healthcare, 11(5), 777. https://doi.org/10.3390/healthcare11050777






