Abstract
Healthcare professionals’ health literacy (HL) knowledge and skills influence their interaction with older adults. Healthcare professionals, when effectively communicating with older adults, can empower and enhance patients’ skills to make informed decisions about their health. The study aimed to adapt and pilot test a HL toolkit to enhance the HL skills of health professionals working with older adults. A mixed methodology of three phases was used. Initially, the healthcare professionals’ and older adults’ needs were identified. Following a literature review of existing tools, a HL toolkit was selected, translated, and adapted into Greek. The HL toolkit was introduced to 128 healthcare professionals as part of 4 h webinars; 82 healthcare professionals completed baseline and post assessments, and 24 healthcare professionals implemented it in their clinical practice. The questionnaires used included an interview on HL knowledge, communication strategies, and self-efficacy using a communication scale. HL and communication strategies knowledge (13 items) and self-efficacy in communication (t = −11.127, df = 81, p < 0.001) improved after the end of the HL webinars, and improvement was retained during the follow-up after 2 months (H = 8.99, df = 2, p < 0.05). A culturally adapted HL toolkit was developed to support the needs of healthcare professionals working with older adults, taking into consideration their feedback in all phases of the development.
1. Introduction
According to WHO, strengthening the health literacy (HL) skills of the general population is a multicomponent process involving the participation of healthcare organizations, healthcare professionals, healthcare users, and the environment [1]. An improvement in healthcare organizations’ and healthcare professionals’ HL skills could be beneficial for national healthcare systems, considering that studies have associated patients’ low HL with higher medical costs [2,3].
Older adults are considered a vulnerable population with low HL [4], who may face cognitive, sensory, and other physical challenges that prevent them from communicating effectively with healthcare professionals [5]. Older adults’ low HL is associated with negative health outcomes, such as deteriorated physical and cognitive functioning, worse mental health, low medication adherence, worse disease management, fewer health-related preventive actions, longer hospital stays, frequent emergency admissions, and overall higher mortality rates [3,4].
Among the objectives of “Healthy People” for 2030, an initiative running for almost thirty years by the US Department of Health and Human Services, are access to healthcare services and an improvement in communication among healthcare providers and patients (i.e., involve patients in decision-making, assure understanding, increase clear communication) [6]. Older adults are coping with barriers in accessing and utilizing healthcare services [7]. Factors influencing access to healthcare services in primary care include individual (literacy and education, health beliefs, limited mobility, limited digital skills), socioeconomic, cultural/linguistic, environmental (geographical location, transportation, visit modality), and organizational (staff shortage) factors [8,9,10]. Healthcare professionals play a crucial role in assisting healthcare users to overcome the aforementioned barriers, as it was stated in Ottawa Chart [11], through the redistribution of power, participation, and healthcare users becoming experts.
The knowledge and comprehension of HL among healthcare professionals influence the communication between healthcare professionals and older individuals with chronic diseases and their families [5]. Communication and empowerment of the high-risk population are considered one of the ten attributes of HL organizations [12]. Organizational HL is gaining prominence within health organizations. The ten attributes of HL organizations include [12] leadership to promote HL; integration of HL in planning; evaluation measures; training of the workforce on HL issues; participation of healthcare users in the design, implementation, and evaluation of the health services; combating stigma; use of HL strategies in communication; accessible services and health resources provided by the organization; clear communication; and empowered users in high-risk situations (medication adherence) [12].
The use of clear language without medical jargon, the use of a person-centered approach, and the implementation of communication strategies according to healthcare professionals working with older adults improved communication with them [13]. According to the HL Universal Precautions, healthcare professionals should not assume the HL level of their patients based on their appearance [14]. The Agency of Healthcare and Research Quality developed a universal precautions toolkit for physicians including 20 tools [15], which was later updated to 21 tools [16]. The main categories included were raising awareness, improving spoken and written communication, and improving supportive systems [16]. To the authors’ knowledge, there is no HL toolkit adapted to the needs of healthcare professionals working with older adults [17]. The study aimed to adapt and pilot a health literacy toolkit to enhance the HL skills of healthcare professionals working with older people to validly detect and empower patients’ HL levels.
2. Materials and Methods
2.1. Study Design
The current study followed a mixed method design with three phases lasting 24 months (November 2020 to October 2022) and following the cultural adaptation process model (CAP): (1) examining the target groups’ needs, (2) developing the adaptation methodology, and (3) adapting the selected tools and pilot testing them [18]. Target groups of the adaptation process were healthcare professionals working with older adults (Figure 1).
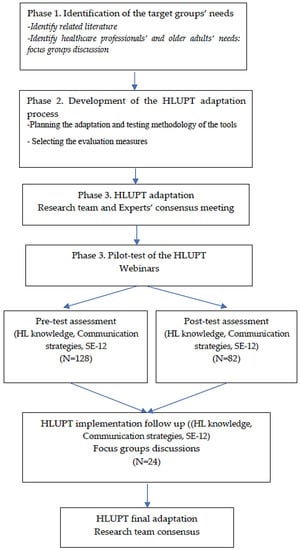
Figure 1.
HLUPT cultural adaptation process.
2.1.1. Examining the Target Groups’ Needs
Identify related literature. A scoping review was conducted by the research group for the period 2000 to 2020 to identify tools for translation and adaptation, HL training courses, and evaluation measures. The literature search of five electronic databases (PubMed, MEDLINE, CINAHL, PsychInfo, and Opengrey) resulted in 27 papers, and it was concluded that there is a lack of HL tools tailored for healthcare professionals working with older healthcare users [17]. The most used HL toolkit was the HLUPT. Information is available in the published scoping review [17].
Identify healthcare professionals’ and older healthcare users’ needs. Two focus groups were conducted to assess the HL knowledge and communication needs of healthcare professionals (n = 7) and older healthcare users (n = 5). Questions included topics on HL knowledge, perspectives on barriers and facilitators in patient–healthcare professional interaction, and healthcare professionals’ training needs [13]. Healthcare professionals reported that trust, collaboration, patients’ education, psychological resilience, carers’ participation, use of plain language, and compassion facilitated their interaction with older healthcare users. On the other hand, the rigid lifestyle of older adults and any cognitive, emotional, sensory, and physical health issues comprised barriers. Older healthcare users considered as important elements in their interaction with healthcare professionals the appropriate preparation before their visit, the assessment of the severity of their health problems, their carers’ participation, nonuse of medical jargon, patients’ involvement in decision-making, equality, respect, compassion, and healthcare professionals’ encouraging discussion [13].
2.1.2. Developing the HLUPT Adaptation Methodology
Permission to adapt the health literacy toolkit was granted by Advancing Excellence in Health Care. A certified translator from English to Greek and a group of HL experts were identified to evaluate the terminology, and cultural appropriacy of the selected tools, supplementary material, and inclusion criteria for the tools were agreed upon. The inclusion criterion set was that the tool to be in accordance with national health system processes in Greece.
This pilot test method has already been used in the adaptation of HLUPT for cardiology and rheumatology [19]. Healthcare professionals were initially informed about the HLUPT tools during a 4 h webinar and were then asked to use the toolkit for a two-month period. The webinars were delivered online for two main reasons: to facilitate participation from different regions of Greece and to ensure safety due to pandemic restrictions. Overall, six webinars of 12–20 participants each were delivered from October 2021 to June 2022.
The content of the webinars derived from the work by Kripalani et al. [14] with permission to use and adapt the workshop material, “Strategies to improve communication between pharmacy staff and patients: A training program for pharmacy staff curriculum guide”. The webinar included a theoretical section in the form of a presentation on the definition of HL, red flags for identifying older patients with low HL, and an introduction to the HL toolkit. The second section outlined the most important communication strategies (plain language, teach-back, summarizing the main message, and searching for online information). The third section consisted of role-playing exercises. Evaluation of the knowledge and communication skills was designed at baseline, after the end of the webinar, and for the small sample that implemented the adapted HLUPT after the end of a two-month period.
2.1.3. HLUPT Adaptation
In collaboration with the research team, a group of four HL experts evaluated the terminology and cultural appropriacy of the selected tools and supplementary material. The research team tailored the language to be culturally sensitive to Greek content and values and ensured the content was applicable to healthcare professionals working with older adults according to the ecological validity model (16).
In the pre-piloting phase, the research team excluded information regarding private insurance forms, nonmedical support and medical resources, referrals, and literacy and math resources (Table 1).

Table 1.
Health Literacy Universal Precautions Toolkit (HLUPT) selected tools before piloting.
2.2. Sample and Recruitment Process of the HLUPT Pilot Phase
Over 250 professionals were invited to participate in the pilot phase of the HLUPT. Recruitment followed a convenience and snowball sampling procedure, according to which professionals invited colleagues via social media, online groups, healthcare services, and university departments. The eligibility criteria for the healthcare professionals included: being a physician, nurse, psychologist, or other healthcare professional, speaking and writing in Greek, and working in a primary healthcare setting (e.g., hospital, day center, day clinic). Initially, 128 healthcare professionals registered to attend the webinar, and 82 completed the post-training assessment. The most common explanations for drop-out were time constraints and an abundance of responsibilities. Other reasons concerned organization barriers and the inability to comprehend the task of this phase. After the webinar, a small sample of healthcare professionals (n = 24) implemented the adapted HLUPT in their clinical practice for a two-month period. The healthcare professionals used up to three tools in their daily clinical practice for two months under the supervision of the research team. Short calls were scheduled with the researchers for questions or clarification. At the end of this two-month period, healthcare professionals evaluated their communication skills and knowledge of HL and participated in three focus groups.
Three focus groups were organized with 15 participants. The discussion was facilitated with the use of a guide that included questions regarding the HL toolkit and the way they used the selected HL tools (i.e., how they implemented the tools, barriers to implementation, evaluation of the practicality of the tools, suggestions of HL tools from the toolkit, written language of the toolkit, organization and staff attitudes toward the toolkit, and future training needs). The focus group sessions lasted between 40 and 60 min. The principal author (A.E.) served as a moderator and the second author (A.K.) as an observer.
2.3. Questionnaires Used in the HLUPT Pilot Phase
Demographic information (e.g., gender, age, education, profession, professional experience, and type of healthcare service) was obtained from healthcare professionals at baseline. To assess HL knowledge and communication skills, 13 Likert-type questions were adapted based on the research conducted by Mackert [20], including HL perceived knowledge, perceived ability to identify low-HL patients, communication skills, and one open question on the definition of HL.
Self-Efficacy-12 questionnaire was validated in Greek for the purpose of pilot test phase [21]. The questionnaire consists of 12 items measuring healthcare professionals’ self-efficacy of skills used during the patient–clinician encounter, rated on a 10-point Likert scale ranging from 1 = very uncertain to 10 = very certain. The sum of scores ranges from 12–120, and higher scores indicate higher levels of self-efficacy in skills [22]. The first 10 items measure “self-efficacy in communication skills and strategies”, and the last two items measure “self-efficacy of successful interaction”. Both factors of the Greek version have shown high internal consistency (factor 1: α = 0.95 and factor 2: α = 0.93), similar to the total scale (α = 0.96).
2.4. Statistical Analysis
Descriptive statistics and dependent sample t-tests were computed to compare the pre- and post-assessments. The Kruskal–Wallis test was used to compare baseline, post-, and follow-up scores for the sample of 24 healthcare professionals. Three focus group discussions evaluated the usefulness of the HL toolkit after implementing the selected tools for a two-month period. Transcribed scripts, derived from the focus group discussions, were content analyzed.
2.5. Ethics and Informed Consent
Permission to conduct the study was granted by the bioethics committee of the Hellenic Mediterranean University (63/EMΠ 95). All participants were fully informed of the study aims and the requirements for their participation in the study. Consent forms were signed before the pilot testing, and all participants were informed that they could withdraw their participation and that their data could be excluded by contacting the main investigator. Researchers in all phases of the study promoted the wellbeing of the participants. The researcher/trainer tried to make participants feel comfortable and resolve any kind of conflict. To safeguard sensitive personal data, a database protected by password was developed and stored on the research team’s university computers; only members of the research team had access to the database.
3. Results
3.1. Descriptive Characteristics
Most of the participants who attended the webinars were women (n = 120, 93.8%) with tertiary and postgraduate education (N = 105, 82%), a mean age of 44 years old, and worked in public healthcare services (n = 103, 83%). Nurses (n = 36, 28.1%), health visitors (n = 30, 23.4%), and social workers (n = 22, 17.2%) were the professions with the highest representation in the sample. Physicians, physiotherapists, and occupational therapists had the lowest participation. Almost half of the sample had over 10 years of experience with older healthcare users (Table 2).

Table 2.
Descriptive characteristics of the participants.
3.2. HL Definition, Knowledge, and Communication Self-Efficacy
More than two-thirds of the healthcare professionals (n = 83, 64%) provided at baseline the HL definitions, whereas the remaining gave vague definitions of health, skills, knowledge, clinical diagnosis, and communication skills of healthcare professionals. Most of the respondents identified the ability to comprehend medical recommendations and treatment plans in order to make health decisions as the central aspect of the HL definition, while others identified the ability to comprehend medical jargon. Examples of the HL definitions follow:
“the skill to understand medical jargon and to use the internet to support your health”;
“the skill to understand the therapeutic plan”;
“the skill to understand and process health information to make health decisions”.
In the post-test assessment (after the end of the webinar), 82 participants had statistically significantly improved their HL knowledge in all 13 of Mackert’s interview items (Table 3).

Table 3.
Mackert’s interview items (n = 82).
There was a significant difference in SE-12-Gr between the baseline scores (M = 92.1, SD = 13.62) and the post-assessment scores for the 82 participants (M = 104.24, SD = 10.82) (t = −11.127, df = 81, p < 0.001) (Table 4).

Table 4.
Self-Efficacy-12-Gr (SE-12-Gr) in pre- and post-assessments (n = 82).
3.3. Implementation of HLUPT Tools in Clinical Practice
The sample that continued to the implementation of the three tools from the HLUPT for healthcare professionals working with older adults retained a higher rank mean (39.17) in the SE-12-Gr at the follow-up assessment compared with baseline (26.42) (Table 5).

Table 5.
Self-Efficacy-12-Gr (SE-12-Gr) in pre-, post-, and follow-up assessments (n = 24).
3.4. Focus Group Discussions
Of the 15 participants in the three groups, 29% (n = 7) used the HL toolkit for less than a week, 25% (n = 6) for 1 to 2 weeks, and the remaining participants (46%; n = 11) from 1 to 2 months. Half of the participants in the focus groups reported using the HL toolkit frequently during the aforementioned periods.
Three themes were discussed: (1) the preferred tools, (2) ways to improve the toolkit, and (3) HL toolkit usefulness and health organization acceptance.
- Preferred tools. The most preferred tool was “Tool 3. Teach-back method” (n = 9, 60%). Participants reported that they informed their coworkers, and they planned meetings to do so whenever possible using available material and instructions from “Tool 1. Raise awareness” of the HLUPT. Healthcare professionals working at home preferred “Tool 4. Brown bag medication review” and “Tool 10. Assisting older adults with their medical treatment.” “Tool 2. Clear communication” was also frequently selected and usually combined with “Tool 3”. Only in one case did a healthcare professional living and working in a rural area favor “Tool 6. Cultural and linguistic differences.”
- Ways to improve the toolkit. Participants in the focus group suggested ways to enhance the HL toolkit:
- -
- to utilize exercises and images to facilitate comprehension of the tools;
- -
- to include components for older adults with memory deficiencies and dementia in “Tool 3. Teach-back method”;
- -
- to introduce the concept of healthy and active aging;
- -
- to modify the toolkit for use by people working in the public and private sectors (e.g., banks, supermarkets, post offices);
- -
- to incorporate suggestions for healthcare professionals working with older adults who are illiterate in “Tool 10. Assisting older adults with their medical treatment”;
- -
- to include a friendly service environment adaptation tool.
- HL toolkit usefulness and health organization support. All the participants in the focus group assessed the HL toolkit as very useful and its resources as comprehensible. They acknowledged that they had to acquire this knowledge through practice with older adults. Participants reported that the toolkit could be a valuable resource for young healthcare professionals starting their careers and for older people to gain new knowledge. They discussed the difficulty in establishing an HL team within their organization because of social distance measures and relevant restrictions imposed by the COVID-19 pandemic (i.e., could not meet regularly with their colleagues). They also had difficulty approaching their experienced colleagues. In addition, frequent changes in supervisors/managers in public healthcare services posed a potential barrier to their efforts to raise HL awareness among the organization’s staff. The final adapted toolkit is available in Table 6.
 Table 6. Final adapted HLUPT for healthcare professionals working with older adults.
Table 6. Final adapted HLUPT for healthcare professionals working with older adults.
4. Discussion
The purpose of the study was the adaptation of a HL toolkit for healthcare professionals working with older adults. This study provided a toolkit written in plain language with examples of everyday clinical practice provided by healthcare professionals. After the 4 h webinars in the framework of the toolkit piloting, healthcare professionals improved their communication self-efficacy and HL knowledge, and this finding remained after the 2-month follow-up for the healthcare professionals who implemented the toolkit in their clinical practice.
There are HL training courses and tools targeting healthcare professionals and physicians [14,23,24,25,26], but there is a lack of courses and tools targeting healthcare professionals working with older adults [17]. Older adults are considered an at-risk population with low HL, facing difficulty in adhering to the therapeutic plan and effectively communicating with healthcare professionals [4,5,27]. They face multiple health issues and are usually excluded by healthcare professionals from the decision-making process [28,29].
The findings of this study were valid and reliable. The three stages of the cultural adaptation process model [23] were as follows: setting the scene, planning the adaptation, and proceeding with the adaptation and pilot test. Our findings are in line with Mackert et al.’s [20] findings, according to which, on the one hand, participants overestimated their HL knowledge, and on the other hand, their knowledge improved after a training course. Similar studies assessing self-efficacy in communication found that it was improved after communication skills training of physicians and nurses [29]. Two-thirds of the participants in the present study were aware of and identified aspects of the HL concept (e.g., understanding health information, making health decisions, communication with physicians, and medical adherence).
Healthcare professionals perceived the HL toolkit as a valuable, easy-to-use resource in everyday clinical practice, and they contributed their expertise to the focus groups to improve the toolkit. The most preferred tools included “Tool 1. Raise awareness,” “Tool 2. Communicate clearly,” “Tool 3. Teach-back method,” “Tool 5. Brown bag medication review,” and “Tool 10. Assisting older adults with their medical treatment.” Callahan et al. [19] recognized the teach-back method and brown bag medication review as the most frequently used tools to raise awareness among staff. Older adults’ medication adherence is considered an important dimension of the healthcare professionals’ clinical work and usually is reported as the most difficult issue to handle in the older adults’ caregiving process [30].
Limitations of this study were the small number of medical professionals in the adaptation process and the small number of participants in the follow-up phase. For this reason, the results of the study concerning the specific sample could not be generalized to other healthcare professionals. The strength of the study included the involvement of healthcare professionals in all phases of the adaptation process and providing a toolkit tailored to the healthcare professionals’ needs. During the focus group discussions with older healthcare users regarding their interaction with healthcare professionals, they mostly focused on physicians’ input [13], and physicians were the least represented healthcare professional group in our sample. In addition, lack of funding prevented the linguistic adaptation of audiovisual materials that were included in the HLUPT. All video links were added to the toolkit, along with a note instructing users to enable subtitles when applicable.
Primary healthcare in Greece is delivered through public and private services, and healthcare users need to find and appraise healthcare services without any support from the healthcare system [31]. They need to decide on the proper healthcare professional specialty and healthcare department [31]. HL is a concept not fully appraised by health organizations in Greece, even if more and more discussions on the topic have been raised after the COVID-19 pandemic.
Future research could focus on the effectiveness of the HL toolkit within the context of healthcare professional practice and the adaptation of the toolkit to other high-risk populations (e.g., migrants). HL training among healthcare professionals builds networks, promotes HL leadership, empowers professionals, and builds HL organizations [32].
5. Conclusions
Public healthcare services could adopt the HL toolkit to support the training needs of primary care healthcare professionals [32]. We consider that the HL toolkit provides a set of 11 tools tailored to the needs of healthcare professionals working in the Greek context. The HL toolkit could assist healthcare professionals in their everyday clinical work, be part of vocational and educational seminars, and be promoted within the healthcare organizational context. The use of the HL toolkit will facilitate the clinical work of healthcare professionals working with older adults, and indirectly, it is expected to enhance the HL of older adults.
Author Contributions
Conceptualization, A.E.; methodology, A.E. and A.K.; validation, A.E., A.K. and M.R.; formal analysis, A.E.; investigation, A.E. and A.K.; writing—original draft preparation, A.E.; writing—review and editing, A.K. and M.R.; supervision, A.K.; project administration, A.E.; funding acquisition, A.E. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Hellenic Mediterranean University, grant number 67ΝH46ΜH2Ι-ΙΛ7.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of Hellenic Mediterranean University (protocol code 63 and 23 June 2021) for studies involving humans.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are unavailable due to privacy.
Acknowledgments
We would like to acknowledge the healthcare professionals who participated in all phases of the research and provided their valuable feedback on this work.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization (WHO). Health Literacy: The Solid Facts; World Health Organization: Geneva, Switzerland, 2013; Available online: https://apps.who.int/iris/bitstream/handle/10665/128703/e96854.pdf (accessed on 17 May 2020).
- Howard, D.H.; Gazmararian, J.; Parker, R.M. The impact of low health literacy on the medical costs of Medicare managed care enrollees. Am. J. Med. 2005, 118, 371–377. [Google Scholar] [CrossRef] [PubMed]
- VandenBosch, J.; Van den Broucke, S.; Vancorenland, S.; Avalosse, H.; Verniest, R.; Callens, M. Health literacy and the use of healthcare services in Belgium. J. Epidemiol. Commun. Health 2016, 70, 1032–1038. [Google Scholar] [CrossRef]
- Chesser, A.K.; Woods, N.K.; Smothers, K.; Rogers, N. Health Literacy and Older Adults. Gerontol. Geriatr. Med. 2016, 2, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Speros, C. More than Words: Promoting Health Literacy in Older Adults. OJIN Online J. Issues Nurs. 2009, 14. [Google Scholar] [CrossRef]
- Healthy People 2030. Healthy People 2030 Objectives: Older People. U.S. Department of Health and Human Services. Available online: https://health.gov/healthypeople/objectives-and-data/browse-objectives/older-adults (accessed on 26 February 2021).
- Ford, J.A.; Wong, G.; Jones, A.P.; Steel, N. Access to primary care for socioeconomically disadvantaged older people in rural areas: A realist review. BMJ Open 2016, 6, e010652. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Guruge, S.; Montana, G. Older Immigrants’ Access to Primary Health Care in Canada: A Scoping Review. Can. J. Aging/La Rev. Can. Vieil. 2019, 38, 193–209. [Google Scholar] [CrossRef]
- Bodenheimer, T.; Pham, H.H. Primary Care: Current Problems and Proposed Solutions. Health Aff. 2010, 29, 799–805. [Google Scholar] [CrossRef]
- Ryskina, K.L.; Shultz, K.; Zhou, Y.; Lautenbach, G.; Brown, R.T. Older adults’ access to primary care: Gender, racial, and ethnic disparities in telemedicine. J. Am. Geriatr. Soc. 2021, 69, 2732–2740. [Google Scholar] [CrossRef]
- World Health Organisation. The Ottawa Charter for Health Promotion; WHO: Geneva, Switzerland, 1986. [Google Scholar]
- Brach, C.; Keller, D.; Hernandez, L.M.; Baur, C.; Parker, R.; Dreyer, B.; Schyve, P.; Lemerise, A.J.; Schillinger, D. Ten Attributes of Health Literate Health Care Organizations. Discussion Paper. Available online: https://nam.edu/wp-content/uploads/2015/06/BPH_Ten_HLit_Attributes.pdf (accessed on 1 March 2023).
- Efthymiou, A.; Rovithis, M.; Kalaitzaki, A. The Perspectives on Barriers and Facilitators in Communication by the Healthcare Professionals and Older Healthcare Users: The Role of Health Literacy. J. Psychol. Psychother. Res. 2022, 9, 1–11. [Google Scholar] [CrossRef]
- Kripalani, S.; Jacobson, K.L. Strategies to Improve Communication between Pharmacy Staff and Patients: A Training Program for Pharmacy Staff Curriculum Guide. Agency for Healthcare Research and Quality. 2007. Available online: https://www.ahrq.gov/health-literacy/improve/pharmacy/guide/train.html (accessed on 22 February 2021).
- DeWalt, D.A.; Broucksou, K.A.; Hawk, V.; Brach, C.; Hink, A.; Rudd, R.; Callahan, L. Developing and testing the health literacy universal precautions toolkit. Nurs. Outlook 2011, 59, 85–94. [Google Scholar] [CrossRef]
- Brega, A.; Barnard, J.; Mabachi, N.M.; Weiss, B.D.; DeWalt, D.A.; Brach, C.; Cifuentes, M.; Albright, K.; West, D.R. Health Literacy Universal Precautions Toolkit, 2nd ed; AHRQ Publication: Rockville, MD, USA, 2015. Available online: http://www.ahrq.gov/qual/literacy/healthliteracytoolkit.pdf (accessed on 1 March 2023).
- Efthymiou, A.; Kalaitzaki, A.; Kondilis, B.; Rovithis, M. Health literacy continuing education courses and tools for healthcare professionals: A scoping review. Gerontol. Geriatr. Educ. 2022, 1–36. [Google Scholar] [CrossRef]
- Rodríguez, M.M.D.; Baumann, A.A.; Schwartz, A.L. Cultural Adaptation of an Evidence Based Intervention: From Theory to Practice in a Latino/a Community Context. Am. J. Community Psychol. 2010, 47, 170–186. [Google Scholar] [CrossRef]
- Callahan, L.F.; Hawk, V.; Rudd, R.; Hackney, B.; Bhandari, S.; Prizer, L.P.; Bauer, T.K.; Jonas, B.; Mendys, P.; DeWalt, D. Adaptation of the health literacy universal precautions toolkit for rheumatology and cardiology—Applications for pharmacy professionals to improve self-management and outcomes in patients with chronic disease. Res. Soc. Adm. Pharm. 2013, 9, 597–608. [Google Scholar] [CrossRef]
- Mackert, M.; Ball, J.; Lopez, N. Health literacy awareness training for healthcare workers: Improving knowledge and intentions to use clear communication techniques. Patient Educ. Couns. 2011, 85, e225–e228. [Google Scholar] [CrossRef]
- Efthymiou, A.; Rovithis, M.; Kalaitzaki, A. Τhe Healthcare Professionals’ Self-reported Communication Skills with Older Healthcare Users in Greece: Validation of the Self-efficacy Questionnaire (SE-12-Gr). Health Commun. (in review).
- Axboe, M.K.; Christensen, K.S.; Kofoed, P.-E.; Ammentorp, J. Development and validation of a self-efficacy questionnaire (SE-12) measuring the clinical communication skills of health care professionals. BMC Med. Educ. 2016, 16, 1–10. [Google Scholar] [CrossRef]
- IMPACCT Erasmus+. Working with Patients with Limited Health Literacy. Future Learn. 2017. Available online: https://www.futurelearn.com/courses/working-health-literacy (accessed on 20 February 2021).
- University at Albany Centre for Public Health Continuing Education (Organisation), PHTC ONLINE: Health Literacy and Public Health Training. 2006. Available online: https://phtc-online.org/learning/?seriesId=4&status=all&sort=group (accessed on 20 February 2021).
- Center of Disease Control. Effective Communication for Healthcare Teams: Addressing HL, Limited English Proficiency and Cultural Difference. CDC TRAIN. 2019. Available online: https://www.train.org/cdctrain/course/1077848/ (accessed on 24 February 2021).
- Centre of Disease Control. Health Literacy for Public Health Professionals—WB4031R. CDC TRAIN. 2018. Available online: https://www.train.org/cdctrain/course/1078759/?activeTab=reviews (accessed on 20 February 2021).
- Sudore, R.L.; Mehta, K.M.; Simonsick, E.M.; Harris, T.B.; Newman, A.B.; Satterfield, S.; Rosano, C.; Rooks, R.N.; Rubin, S.M.; Ayonayon, H.N.; et al. Limited Literacy in Older People and Disparities in Health and Healthcare Access. J. Am. Geriatr. Soc. 2006, 54, 770–776. [Google Scholar] [CrossRef]
- James, B.D.; Boyle, P.A.; Bennett, J.S.; Bennett, D.A. The Impact of Health and Financial Literacy on Decision Making in Community-Based Older Adults. Gerontology 2012, 58, 531–539. [Google Scholar] [CrossRef]
- Mata, N.D.S.; de Azevedo, K.P.M.; Braga, L.P.; de Medeiros, G.C.B.S.; Segundo, V.H.D.O.; Bezerra, I.N.M.; Pimenta, I.D.S.F.; Nicolás, I.M.; Piuvezam, G. Training in communication skills for self-efficacy of health professionals: A systematic review. Hum. Resour. Health 2021, 19, 1–9. [Google Scholar] [CrossRef]
- Smaje, A.; Weston-Clark, M.; Raj, R.; Orlu, M.; Davis, D.; Rawle, M. Factors associated with medication adherence in older patients: A systematic review. Aging Med. 2018, 1, 254–266. [Google Scholar] [CrossRef]
- Lionis, C.; Papadakis, S.; Tatsi, C.; Bertsias, A.; Duijker, G.; Mekouris, P.-B.; Boerma, W.; Schäfer, W. Informing primary care reform in Greece: Patient expectations and experiences (the QUALICOPC study). BMC Health Serv. Res. 2017, 17, 255. [Google Scholar] [CrossRef]
- Naccarella, L.; Murphy, B. Key lessons for designing health literacy professional development courses. Aust. Health Rev. 2018, 42, 36. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).