The Impact of Caregiving on Successful Ageing of Informal Carers: A Qualitative Study among Respiratory Patients’ Caregivers
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Methods
2.3. Analysis
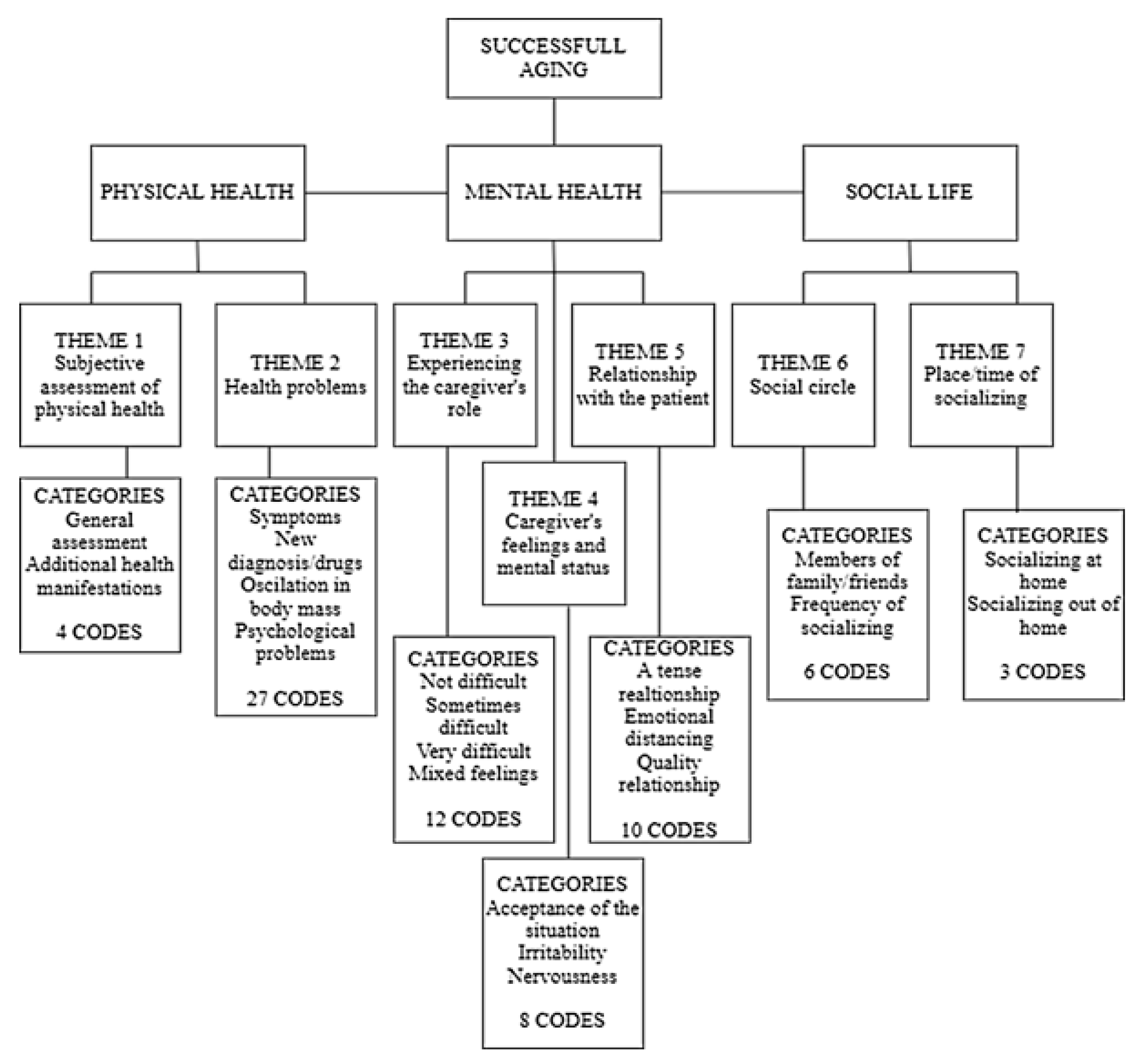
3. Results
“He can’t do anything anymore. Not even talk. We get along as a patient and a nurse (laughs). It’s the only thing that connects us. My constant concern for him and his need for my help. We agree only on that”.(Caregiver 7)
“As in any marriage, we sometimes argue. But I’m gentler in an argument than before my illness (laughs). We actually get along well. The disease did not manage to destroy us”.(Caregiver 8)
“Our relationship is quite turbulent. Mom always has to be right and always uses the sentence: I’m seriously ill! And that’s how she always provokes a feeling of remorse in me. But I have to take care of her”.(Caregiver 9)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Semi-Structured Interview Questions
- Please describe your typical day.
- Do you have trouble sleeping? If so, what causes the difficulties? Can you remember how you slept before the onset of the disease in the family?
- Do you practice any physical activity? If so, what kind of physical activity and how often in the past month?
- Can you remember some activity you used to practice and now you are not able to? If you no longer perform certain physical activities, what are the reasons for that?
- How do you assess your physical health? Has there been any change since you took on the role of caregiver? Do you go to regular medical examinations?
- How do you feel about your role as a caregiver? Do you find this role difficult? If this role burdens you, what do you consider to be the main cause of that burden?
- What kind of relationship do you have with the care recipient? Is there anything in that relationship that has changed since you became a care provider? Do you agree with him/her? If something particularly bothers you in that relationship, what is it?
- Does the role of the caregiver and the activities related to that role affect how you feel? Are you more nervous than before?
- Are you bothered by anything related to providing care? Do you talk to anyone about any difficulties you may face? Do you unburden yourself to anyone?
- Have you ever sought or considered seeking professional, psychological help? If so, what motivated you to seek help?
- Have you been hanging out with relatives or friends lately? Where do you hang out most often?
- Have you been traveling lately (going on vacation or visiting relatives)? Has there been any change since you took on the role of caregiver? What would help you travel somewhere?
- How would your family members describe you? Have you changed since you took on the role of caregiver?
- Do family members or friends help you with caring for a sick family member? Do you need additional help?
- Have you had time lately to engage in some free activities (hobbies, visiting exhibitions, theater...)? If no, what was the reason for that?
References
- Directorate-General for Employment, Social Affairs and Inclusion (European Commission); London School of Economics and Political Science (LSE); Zigante V. Informal Care in Europe: Exploring Formalisation, Availability and Quality. Publications Office. 2018. Available online: https://op.europa.eu/en/publication-detail/-/publication/96d27995-6dee-11e8-9483-01aa75ed71a1/language-en (accessed on 3 January 2023).
- OECD. Informal Carers. Health at a Glance 2019: OECD Indicators. 2019. Available online: https://www.oecd-ilibrary.org/sites/a80d9f62-en/index.html?itemId=/content/component/a80d9f62-en (accessed on 3 January 2023).
- WHO. Global action plan on the public health response to dementia 2017–2025. In Global Action Plan on the Public Health Response to Dementia; World Health Organization: Geneva, Switzerland, 2017; pp. 2017–2025. [Google Scholar]
- United Nations Secretariat Building. Expert Group Meeting on Care and Older Persons: Links to Decent Work, Migration and Gender. New York. 2017. Available online: https://www.un.org/development/desa/ageing/wp-content/uploads/sites/24/2018/03/17-EGM-Care-Report-7-March-2018.pdf (accessed on 3 January 2023).
- OECD. Care Needed: Improving the Lives of People with Dementia; OECD: Paris, France, 2018. [Google Scholar]
- Pressler, S.J.; Gradus-Pizlo, I.; Chubinski, S.D.; Smith, G.; Wheeler, S.; Sloan, R.; Jung, M. Family caregivers of patients with heart failure: A longitudinal study. J. Cardiovasc. Nurs. 2013, 28, 417–428. [Google Scholar] [CrossRef]
- AARP. Caregiving in the United States 2020; American Association of Retired Persons: Washington, DC, USA, 2020. [Google Scholar]
- Hopps, M.; Iadeluca, L.; McDonald, M.; Makinson, G.T. The burden of family caregiving in the United States: Work productivity, health care resource utilization, and mental health among employed adults. J. Multidiscip. Healthc. 2017, 10, 437. [Google Scholar] [CrossRef]
- Hilton, J.M.; Kopera-Frye, K.; Krave, A. Successful aging from the perspective of family caregivers. Fam. J. 2009, 17, 39–50. [Google Scholar] [CrossRef]
- Havighurst, R.J. Successful aging. Process Aging Soc. Psychol. Perspect. 1963, 1, 299–320. [Google Scholar]
- Teater, B.; Chonody, J.M. How do older adults define successful aging? A scoping review. Int. J. Aging Hum. Dev. 2020, 91, 599–625. [Google Scholar] [CrossRef]
- Kleineidam, L.; Thoma, M.V.; Maercker, A.; Bickel, H.; Mösch, E.; Hajek, A.; König, H.H.; Eisele, M.; Mallon, T.; Luck, T.; et al. What is successful aging? A psychometric validation study of different construct definitions. Gerontologist 2019, 59, 738–748. [Google Scholar] [CrossRef]
- Dixe, M.D.A.C.R.; da Conceição Teixeira, L.F.; Areosa, T.J.T.C.C.; Frontini, R.C.; de Jesus Almeida Peralta, T.; Querido, A.I.F. Needs and skills of informal caregivers to care for a dependent person: A cross-sectional study. BMC Geriatr. 2019, 19, 255. [Google Scholar] [CrossRef]
- García-Mochón, L.; Peña-Longobardo, L.M.; del Río-Lozano, M.; Oliva-Moreno, J.; Larrañaga-Padilla, I.; García-Calvente, M.D.M. Determinants of burden and satisfaction in informal caregivers: Two sides of the same coin? The CUIDAR-SE study. Int. J. Environ. Res. Public Health 2019, 16, 4378. [Google Scholar] [CrossRef]
- Reinhard, S.C.; Given, B.; Petlick, N.H.; Bemis, A. Supporting family caregivers in providing care. In Patient Safety and Quality: An Evidence-Based Handbook for Nurses; Hughes, R.G., Ed.; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2008. [Google Scholar]
- Schulz, R.; Sherwood, P.R. Physical and mental health effects of family caregiving. J. Soc. Work Educ. 2008, 44 (Suppl. S3), 105–113. [Google Scholar] [CrossRef]
- Perez, G.A.; Rose, K.M.; Caceres, B.A.; Spurlock, W.; Bowers, B.; Lutz, B.; Arslanian-Engoren, C.; Reuter-Rice, K.; Bressler, T.; Wicks, M.; et al. Position statement: Policies to support family caregivers. Nurs. Outlook 2018, 66, 337–340. [Google Scholar] [CrossRef] [PubMed]
- Nakken, N.; Janssen, D.J.A.; van den Bogaart, E.H.A.; Wouters, E.F.M.; Franssen, F.M.E.; Vercoulen, J.H.; Spruit, M.A. Informal caregivers of patients with COPD: Home Sweet Home? Eur. Respir. Rev. 2015, 24, 498–504. [Google Scholar] [CrossRef] [PubMed]
- Shebl, E.; Burns, B. Respiratory Failure; StatPearls: Treasure Islands, FL, USA, 2019. [Google Scholar]
- Simpson, A.C.; Rocker, G.M. Advanced chronic obstructive pulmonary disease: Impact on informal caregivers. J. Palliat. Care 2008, 24, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.; Moser, T. The art of coding and thematic exploration in qualitative research. Int. Manag. Rev. 2019, 15, 45–55. [Google Scholar]
- Carretero, S.; Garcés, J.; Ródenas, F.; Sanjosé, V. The informal caregiver’s burden of dependent people: Theory and empirical review. Arch. Gerontol. Geriatr. 2009, 49, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Vitaliano, P.P.; Zhang, J.; Scanlan, J.M. Is caregiving hazardous to one’s physical health? A meta-analysis. Psychol. Bull. 2003, 129, 946. [Google Scholar] [CrossRef]
- Feinberg, L.; Reinhard, S.C.; Houser, A.; Choula, R. Valuing the Invaluable: 2011 Update, the Growing Contributions and Costs of Family Caregiving; AARP Public Policy Institution: Washington, DC, USA, 2011; p. 32. [Google Scholar]
- Gysels, M.H.; Higginson, I.J. Caring for a person in advanced illness and suffering from breathlessness at home: Threats and resources. Palliat. Support. Care 2009, 7, 153–162. [Google Scholar] [CrossRef]
- Carrieri, V.; Di Novi, C.; Jacobs, R.; Robone, S. Insecure, sick and unhappy? Well-being consequences of temporary employment contracts. In Factors Affecting Worker Well-Being: The Impact of Change in the Labor Market; Emerald Group Publishing Ltd.: Bingley, UK, 2014; pp. 157–193. [Google Scholar]
- Sarasa, S.; Mestres, J. Women’s Employment and the Adult Caring Burden. In Family Formation and Family Dilemmas in Contemporary Europe; Fundancion BBVA: Bilbao, Spain, 2007; pp. 185–221. Available online: https://books.google.rs/books?hl=en&lr=&id=SSfUpxasakIC&oi=fnd&pg=PA185&dq=related:yDBozx2SKkcJ:scholar.google.com/&ots=moKo5NPKqb&sig=NJti_xu49nbJgn-O2PsB2C_Vp0M&redir_esc=y#v=onepage&q&f=false (accessed on 3 January 2023).
- Brenna, E.; Di Novi, C. Is caring for older parents detrimental to women’s mental health? The role of the European North–South gradient. Rev. Econ. Househ. 2016, 14, 745–778. [Google Scholar] [CrossRef]
- Darragh, A.R.; Sommerich, C.M.; Lavender, S.A.; Tanner, K.J.; Vogel, K.; Campo, M. Musculoskeletal discomfort, physical demand, and caregiving activities in informal caregivers. J. Appl. Gerontol. 2015, 34, 734–760. [Google Scholar] [CrossRef]
- del-Pino-Casado, R.; Rodriguez Cardosa, M.; López-Martínez, C.; Orgeta, V. The association between subjective caregiver burden and depressive symptoms in carers of older relatives: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0217648. [Google Scholar] [CrossRef]
- Hajek, A.; König, H.-H. Informal caregiving and subjective well-being: Evidence of a population-based longitudinal study of older adults in Germany. J. Am. Med. Dir. Assoc. 2016, 17, 300–305. [Google Scholar] [CrossRef]
- Grunfeld, E.; Coyle, D.; Whelan, T.; Clinch, J.; Reyno, L.; Earle, C.C.; Willan, A.; Viola, R.; Coristine, M.; Janz, T.; et al. Family caregiver burden: Results of a longitudinal study of breast cancer patients and their principal caregivers. Cmaj 2004, 170, 1795–1801. [Google Scholar] [CrossRef] [PubMed]
- Do, Y.K.; Norton, E.C.; Stearns, S.C.; Van Houtven, C.H. Informal care and caregiver’s health. Health Econ. 2015, 24, 224–237. [Google Scholar] [CrossRef] [PubMed]
- Bolkhir, A.; Loiselle, M.M.; Evon, D.M.; Hayashi, P.H. Depression in primary caregivers of patients listed for liver or kidney transplantation. Prog. Transplant. 2007, 17, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Litwin, H.; Stoeckel, K.J.; Roll, A. Relationship status and depressive symptoms among older co-resident caregivers. Aging Ment. Health 2014, 18, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Crespo, M.; López, J.; Zarit, S.H. Depression and anxiety in primary caregivers: A comparative study of caregivers of demented and nondemented older persons. Int. J. Geriatr. Psychiatry 2005, 20, 591–592. [Google Scholar] [CrossRef]
- Sherwood, P.R.; Given, C.W.; Given, B.A.; Von Eye, A. Caregiver burden and depressive symptoms: Analysis of common outcomes in caregivers of elderly patients. J. Aging Health 2005, 17, 125–147. [Google Scholar] [CrossRef] [PubMed]
- Zarit, S.H.; Reamy, A.M. Future directions in family and professional caregiving for the elderly. Gerontology 2013, 59, 152–158. [Google Scholar] [CrossRef]
- El Habhoubi, E. The Effect of Caregiving on Employment and Mental Health Examined for Midlife European Citizens. Erasmus University Rotterdam. 2012. Available online: https://www.netspar.nl/assets/uploads/047_MSc_Essafia_El_Habhoubi.pdf (accessed on 3 January 2023).
- Cohen, S.A.; Cook, S.; Kelley, L.; Sando, T.; Bell, A.E. Psychosocial factors of caregiver burden in child caregivers: Results from the new national study of caregiving. Health Qual. Life Outcomes 2015, 13, 120. [Google Scholar] [CrossRef]
- Newman, K.; Wang, A.H.; Wang, A.Z.Y.; Hanna, D. The role of internet-based digital tools in reducing social isolation and addressing support needs among informal caregivers: A scoping review. BMC Public Health 2019, 19, 1495. [Google Scholar] [CrossRef]
- Zwar, L.; König, H.-H.; Hajek, A. Consequences of different types of informal caregiving for mental, self-rated, and physical health: Longitudinal findings from the German Ageing Survey. Qual. Life Res. 2018, 27, 2667–2679. [Google Scholar] [CrossRef]
| Variables | N | |
|---|---|---|
| Gender | Male | 1 |
| Female | 14 | |
| Work Status | Full-time job | 3 |
| Parent caregiver | 2 | |
| Retirement | 8 | |
| Unemployed | 2 | |
| Relationship with the patient | Daughter | 3 |
| Son | 1 | |
| Mother | 2 | |
| Wife | 9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benko Meštrović, S.; Šklempe Kokić, I.; Friganović, A.; Krupa, S.; Babić, D.; Zelko, E.; Đorđević, D. The Impact of Caregiving on Successful Ageing of Informal Carers: A Qualitative Study among Respiratory Patients’ Caregivers. Healthcare 2023, 11, 715. https://doi.org/10.3390/healthcare11050715
Benko Meštrović S, Šklempe Kokić I, Friganović A, Krupa S, Babić D, Zelko E, Đorđević D. The Impact of Caregiving on Successful Ageing of Informal Carers: A Qualitative Study among Respiratory Patients’ Caregivers. Healthcare. 2023; 11(5):715. https://doi.org/10.3390/healthcare11050715
Chicago/Turabian StyleBenko Meštrović, Snježana, Iva Šklempe Kokić, Adriano Friganović, Sabina Krupa, Dijana Babić, Erika Zelko, and Dušan Đorđević. 2023. "The Impact of Caregiving on Successful Ageing of Informal Carers: A Qualitative Study among Respiratory Patients’ Caregivers" Healthcare 11, no. 5: 715. https://doi.org/10.3390/healthcare11050715
APA StyleBenko Meštrović, S., Šklempe Kokić, I., Friganović, A., Krupa, S., Babić, D., Zelko, E., & Đorđević, D. (2023). The Impact of Caregiving on Successful Ageing of Informal Carers: A Qualitative Study among Respiratory Patients’ Caregivers. Healthcare, 11(5), 715. https://doi.org/10.3390/healthcare11050715








