Factors Associated with Lack of Health Screening among People with Disabilities Using Andersen’s Behavioral Model
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Analysis Data
2.2. Analysis Variables
2.2.1. Dependent Variable
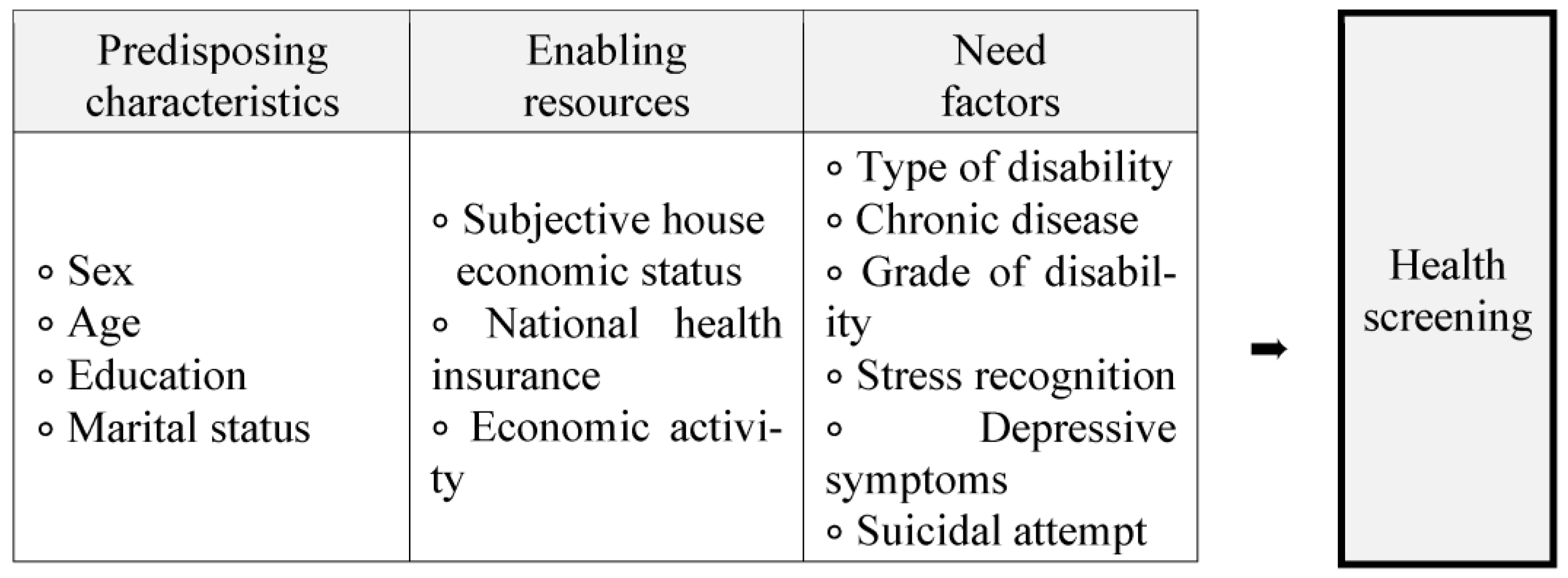
2.2.2. Independent Variable
- Predisposing factors
- Enabling resources
- Need factors
2.3. Data Analysis
3. Results
3.1. General Characteristics
3.2. Health Screening Participation Rates and Reasons for Not Participation Health Screening
3.3. Comparison of Factors According to Health Screening Status
3.4. Analysis of Influencing Factors Related to Non-Participating in Health Screening
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cho, B.L.; Ahn, E.M. Present status and problems of health screening program in Korea. Health Welfare Policy Forum 2013, 198, 48–54. [Google Scholar]
- Yeo, J.Y.; Jeong, H.S. Determinants of health screening and its effects on health behaviors. Health Policy Manag. 2012, 22, 49–64. [Google Scholar] [CrossRef]
- Kim, Y.S.; Lee, J.A. National health examination expansion policy. J. Korean Med. Assoc. 2017, 60, 104–107. [Google Scholar] [CrossRef]
- Cho, B.; Lee, C.M. Current situation of national health screening systems in Korea. J. Korean Med. Assoc 2011, 54, 666–669. [Google Scholar] [CrossRef]
- National Health Insurance Services. National Health Screening Statistical; National Health Insurance Services; Health Insurance Review and Assessment Service: Wonju, Republic of Korea, 2020. [Google Scholar]
- National Rehabilitation Center. Health Management Project of Persons with Disabilities; Ministry of Health and Welfare, National Rehabilitation Center: Seoul, Republic of Korea, 2022; Volume 2021. [Google Scholar]
- Ministry of Government Legislation. Act on Guarantee of Right to Health and Access to Medical Services for Persons with Disabilities; Act No. 13661; Ministry of Government Legislation: Sejong-si, Republic of Korea, 2015. [Google Scholar]
- Park, J.H.; Lee, J.S.; Lee, J.Y.; Hong, J.Y.; Kim, S.Y.; Kim, S.O.; Cho, B.H.; Kim, Y.I.; Shin, Y.S.; Kim, Y. Factors affecting national health insurance mass screening participation in the disabled. J. Prev. Med. Public Health 2006, 39, 511–519. [Google Scholar] [PubMed]
- Yoon, K. A Study of Prevalence of Obesity and Policy Development for Reducing Obesity among People with Disabilities in Korea; Seoul National University: Seoul, Republic of Korea, 2011. [Google Scholar]
- Kim, S.H. National Survey of the Disabled; Ministry of Health and Welfare; Korea Institute for Health and Social Affairs: Sejong, Republic of Korea, 2018; Volume 2017. [Google Scholar]
- National Rehabilitation Center. Health Management Project of Persons with Disabilities; Ministry of Health and Welfare; National Rehabilitation Center: Seoul, Republic of Korea, 2018; Volume 2017. [Google Scholar]
- Martin, S.; Orlowski, M.; Ellison, S.A. Sociodemographic predictors of cervical cancer screening in women with a medical disability. Soc. Work Public Health 2013, 28, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Reichard, A.; Stolzle, H.; Sella, A.C.; Shireman, T.I. Quality of Diabetes Care for Adults with Physical Disabilities in Kansas. Disabil. Health J. 2012, 5, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Welfare. The 5th Policy Plan for Persons with Disabilities (2011–2022); Ministry of Health and Welfare: Sejong, Republic of Korea, 2018. [Google Scholar]
- Andersen, R.A. Behavioral Model of Families’ Use of Health Services; University of Chicago Research Series; University of Chicago: Chicago, IL, USA, 1968; Volume 25, pp. 25–32. [Google Scholar]
- Lederle, M.; Tempes, J.; Bitzer, E.M. Application of Andersen’s behavioural model of health services use: A scoping review with a focus on qualitative health services research. BMJ Open 2021, 11, e045018. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H. National Survey of the Disabled; Ministry of Health and Welfare; Korea Institute for Health and Social Affairs: Sejong, Republic of Korea, 2021; Volume 2020. [Google Scholar]
- National Rehabilitation Center. Health Management Project of Persons with Disabilities; Ministry of Health and Welfare; National Rehabilitation Center: Seoul, Republic of Korea, 2019; Volume 2018. [Google Scholar]
- Reichard, A.; Fox, M.H. Using population-based data to examine preventive services by disability type among dually eligible (medicare/Medicaid) adults. Disabil. Health J. 2013, 6, 75–86. [Google Scholar] [CrossRef] [PubMed]
- Hong, M.H. Relationships of obesity, total-cholesterol, hypertension, and hyperglycemia in health examinees with disabilities. J. Korea Acad.-Ind. Coop. Soc. 2016, 17, 865–875. [Google Scholar]
- Han, S.H.; Jo, E.H.; Son, J.A.; So, E.S. Factors Association National Health Screening Program Participation According to Sex in Korean: Using the Fifth Korea National Health and Nutrition Examination Survey (KNHANES VI, 2013). Korea J. Health Educ. Promot. 2016, 33, 37–48. [Google Scholar] [CrossRef]
- Choi, R.; Hwang, B.D. Use Characteristics of Health Examination Services from Health Insurance Subscribers. J. Korea Contents Assoc. 2011, 11, 331–340. [Google Scholar] [CrossRef]
- Medeiros, A.D.A.; Galvão, M.H.R.; Barbosa, I.R.; Oliveira, A.G.R.D.C. Use of rehabilitation services by persons with disabilities in Brazil: A multivariate analysis from Andersen’s behavioral model. PLoS ONE 2021, 16, e0250615. [Google Scholar] [CrossRef] [PubMed]
- Kuay, L.K. Factors associated with non-participation in a health screening program and its barriers: Findings from the Community Empowers the Nation Programme (KOSPEN), Malaysia 2016. Int. J. Public Health Res. 2020, 10. Available online: https://spaj.ukm.my/ijphr/index.php/ijphr/article/view/258 (accessed on 26 December 2022).
| Variables | N | (%) | |
|---|---|---|---|
| Sex | Male | 3935 | −59.1 |
| Female | 2725 | −40.9 | |
| Age(years) (mean ± SD) | 63.6 ± 15.1 | ||
| 20~39 | 579 | −8.7 | |
| 40~59 | 1916 | −28.8 | |
| 60~79 | 3217 | −48.3 | |
| ≥80~ | 948 | −14.2 | |
| Education | Uneducated/Elementary | 2315 | −38.9 |
| Middle school | 1165 | −19.6 | |
| High school | 2155 | −36.2 | |
| ≥College | 314 | −5.3 | |
| Marital status | Married | 3376 | −50.7 |
| Others | 3279 | −49.3 | |
| Subjective house economic status | Low level | 4676 | −70.2 |
| Middle level | 1926 | −28.9 | |
| High level | 58 | −0.9 | |
| National health insurance (NHI) | Health insurance | 4731 | −71 |
| Medical aid | 1808 | −27.1 | |
| others | 121 | −1.8 | |
| Economic activity | No | 5015 | −75.3 |
| Yes | 1645 | −24.7 | |
| Type of disability | Physical function disability | 1770 | −26.6 |
| Disability of brain lesion | 791 | −11.9 | |
| Visual impairment | 782 | −11.7 | |
| Hearing impairment | 975 | −14.6 | |
| Developmental disability | 505 | −7.6 | |
| Others | 1837 | −27.6 | |
| Chronic disease | No | 1622 | −24.4 |
| Yes | 5038 | −75.6 | |
| Grade of disability | Severe (1~3 grade) | 3290 | −49.4 |
| Mild (4~6 grade) | 3370 | −50.6 | |
| Stress recognition | Little | 935 | −14 |
| Moderate | 3361 | −50.5 | |
| High | 2364 | −35.5 | |
| Depressive symptoms | No | 5343 | −80.2 |
| Yes | 1317 | −19.8 | |
| Suicidal ideation | No | 5840 | −87.7 |
| Yes | 820 | (12.3) | |
| Suicidal attempt | No | 6611 | −99.3 |
| Yes | 49 | −0.7 | |
| Variables | Health Screening | Total | |||||
|---|---|---|---|---|---|---|---|
| Yes | No | ||||||
| N | (%) | N | (%) | N | (%) | ||
| Participation rates of untreated experiences | |||||||
| Untreated experiences | 4599 | −69.1 | 2061 | −30.9 | 6660 | −100 | |
| Cause of non-participation in health screening experiences | |||||||
| Lack of symptoms | 678 | −32.9 | |||||
| Poor transportation service | 421 | −20.4 | |||||
| Economic problems | 170 | −8.2 | |||||
| Lack of time | 127 | −6.2 | |||||
| Anxiety about the health screening results | 90 | −4.4 | |||||
| Communication problems | 85 | −4.1 | |||||
| Lack of knowledge about health screening | 81 | −3.9 | |||||
| Inadequate facilities for people with disabilities in medical institutions | 68 | −3.3 | |||||
| No one to accompany during visit | 62 | −3 | |||||
| Health screening problems | 24 | −1.2 | |||||
| Other | 255 | −12.4 | |||||
| Variables | Health Screening | Total | Chi-Square | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes | No | ||||||||
| N | (%) | N | (%) | N | (%) | ||||
| Sex | |||||||||
| Male | 2753 | −59.9 | 1182 | −57.4 | 3935 | −59.1 | 3.709 | ||
| Female | 1846 | −40.1 | 879 | −42.6 | 2725 | −40.9 | |||
| Age (years) (mean±SD) | |||||||||
| 20~39 | 247 | −5.4 | 332 | −16.1 | 579 | −8.7 | 270.85 | * | |
| 40~59 | 1329 | −28.9 | 587 | −30.6 | 1916 | −28.8 | |||
| 60~79 | 2430 | −52.8 | 787 | −38.2 | 3217 | −48.3 | |||
| ≥80~ | 593 | −12.9 | 355 | −17.2 | 948 | −14.2 | |||
| Education | |||||||||
| Uneducated/Elementary | 1530 | −37.7 | 785 | −41.6 | 2315 | −38.9 | 17.359 | * | |
| Middle school | 849 | −20.9 | 316 | −16.8 | 1165 | −19.6 | |||
| High school | 1477 | −36.4 | 678 | −35.9 | 2155 | −36.2 | |||
| ≥College | 207 | −5.1 | 107 | −5.7 | 314 | −5.3 | |||
| Marital status | |||||||||
| Married | 2599 | −56.6 | 777 | −37.7 | 3376 | −50.7 | 202.761 | * | |
| Others | 1995 | −43.4 | 1284 | −62.3 | 3279 | −49.3 | |||
| Subjective house economic status | |||||||||
| Low level | 3091 | −67.2 | 1585 | −76.9 | 4676 | −70.2 | 64.252 | * | |
| Middle level | 1462 | −31.8 | 464 | −22.5 | 1926 | −28.9 | |||
| High level | 46 | −1 | 12 | −0.6 | 58 | −0.9 | |||
| National health insurance (NHI) | |||||||||
| Health insurance | 3463 | −75.3 | 1268 | −61.5 | 4731 | −71 | 142.829 | * | |
| Medical aid | 1048 | −22.8 | 760 | −36.9 | 1808 | −27.1 | |||
| Others | 88 | −1.9 | 33 | −1.6 | 121 | −1.8 | |||
| Economic activity | |||||||||
| No | 3242 | −70.5 | 1773 | −86 | 5015 | −75.3 | 184.615 | * | |
| Yes | 1357 | −29.5 | 288 | −14 | 1645 | −24.7 | |||
| Type of disability | |||||||||
| Physical function disability | 1338 | −29.1 | 432 | −21 | 1770 | −26.6 | 288,636 | * | |
| Brain lesion disability | 484 | −10.5 | 307 | −14.9 | 791 | −11.9 | |||
| Visually impaired | 592 | −12.9 | 190 | −9.2 | 782 | −11.7 | |||
| Hearing impairment | 717 | −15.6 | 258 | −12.5 | 975 | −14.6 | |||
| Developmental disability | 200 | −4.3 | 305 | −14.8 | 505 | −7.6 | |||
| Others | 1268 | −27.6 | 569 | −27.6 | 569 | −27.6 | |||
| Chronic disease | |||||||||
| Yes | 3543 | −77 | 1495 | −72.5 | 5038 | −75.6 | 15.65 | * | |
| No | 1056 | −23 | 566 | −27.5 | 1622 | −24.4 | |||
| Grade of disability | |||||||||
| Severe (1~3 grade) | 1993 | −43.3 | 1297 | −62.9 | 3290 | −49.4 | 218,618 | * | |
| Mild (3~6 grade) | 2606 | −56.7 | 764 | −37.1 | 3370 | −50.6 | |||
| Stress recognition | |||||||||
| Little | 629 | −13.7 | 306 | −14.8 | 935 | −14 | 55.415 | * | |
| Moderate | 2457 | −53.4 | 904 | −43.9 | 3361 | −50.5 | |||
| High | 1513 | −32.9 | 851 | −41.3 | 2364 | −35.5 | |||
| Depressive symptom | |||||||||
| No | 3787 | −82.3 | 1556 | −75.5 | 5343 | −80.2 | 42.053 | * | |
| Yes | 812 | −17.7 | 505 | −24.5 | 1317 | −19.8 | |||
| Suicidal ideation | |||||||||
| No | 4124 | −89.7 | 1716 | −83.3 | 5840 | −87.7 | 54.182 | * | |
| Yes | 475 | −10.3 | 345 | −16.7 | 820 | −12.3 | |||
| Suicidal attempt | |||||||||
| No | 4570 | −99.4 | 2041 | −99 | 6611 | −99.3 | 2.25 | ||
| Yes | 29 | −0.6 | 20 | −1 | 49 | −0.7 | |||
| Variables | OR † | 95% CI ‡ | ||
|---|---|---|---|---|
| Predisposing characteristics | ||||
| Sex | Male | 1 | ||
| Female | 1.075 | (0.948~1.220) | ||
| Age group | 80 above | 1 | ||
| 60~79 | 0.551 | (0.491~0.658) | ||
| 40~59 | 791 | (0.635~0.987) | ||
| 20~39 * | 2.08 | (1.491~2.902) | ||
| Education | College or higher | 1 | ||
| High school | 1.024 | (0.775~1.427) | ||
| Middle school | 1.049 | (0.775~1.354) | ||
| Uneducated/Elementary * | 1.409 | (1.040~1.908) | ||
| Marital status | Married | 1 | ||
| Others * | 1.283 | (1.124~1.466) | ||
| Enabling resources | ||||
| Subjective house economic status | High level | 1 | ||
| Middle level * | 0.889 | (0.427~2.343) | ||
| Low level | 1.131 | (0.546~1.851) | ||
| National Health insurance (NHI) | Health insurance | 1 | ||
| Medical aid * | 1.226 | (1.061~1.417) | ||
| Economic | Yes | 1 | ||
| activity | No * | 2.078 | (1.740~2.482) | |
| Need factors | ||||
| Type of disability | Physical disability | 1 | ||
| Disability of brain lesion * | 1.606 | (1.313~1.965) | ||
| Visual impairment | 0.899 | (0.723~1.117) | ||
| Hearing impairment | 0.949 | (0.779~1.157) | ||
| Developmental disability * | 1.605 | (1.222~2.109) | ||
| Others | 1.142 | (0.962~1.356) | ||
| Chronic disease | Yes | 1 | ||
| No * | 1.401 | (1.204~1.630) | ||
| Grade of disability | Mild (4~6 grade) | 1 | ||
| Severe (1~3 grade) * | 1.54 | (1.353~1.752) | ||
| Stress recognition | Little | 1 | ||
| Moderate * | 0.793 | (0.664~0.947) | ||
| High | 1.096 | (0.906~1.326) | ||
| Depressive symptom | Yes | 1 | ||
| No | 1.05 | (0.881~1.252) | ||
| Suicidal ideation | No | 1 | ||
| Yes * | 1.324 | (1.078~1.626) | ||
| Suicidal attempt | No | 1 | ||
| Yes | 1.552 | (0.802~3.002) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.-S.; Ho, S.H. Factors Associated with Lack of Health Screening among People with Disabilities Using Andersen’s Behavioral Model. Healthcare 2023, 11, 656. https://doi.org/10.3390/healthcare11050656
Kim Y-S, Ho SH. Factors Associated with Lack of Health Screening among People with Disabilities Using Andersen’s Behavioral Model. Healthcare. 2023; 11(5):656. https://doi.org/10.3390/healthcare11050656
Chicago/Turabian StyleKim, Ye-Soon, and Seung Hee Ho. 2023. "Factors Associated with Lack of Health Screening among People with Disabilities Using Andersen’s Behavioral Model" Healthcare 11, no. 5: 656. https://doi.org/10.3390/healthcare11050656
APA StyleKim, Y.-S., & Ho, S. H. (2023). Factors Associated with Lack of Health Screening among People with Disabilities Using Andersen’s Behavioral Model. Healthcare, 11(5), 656. https://doi.org/10.3390/healthcare11050656






