Obesity-Related Factors in Adult Women with Early Menarche
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Sampling
2.2. Measurement
2.2.1. Obesity
2.2.2. Propensity Score Matching Variables
Age
Education Level
Marital Status
Employment Status
Personal Income
Chronic Disease
Experience of Childbirth and Breastfeeding
Whether Taking Oral Contraceptives
2.2.3. Variables Related to Obesity
Stress Recognition Rate
Sleeping Time
Monthly Drinking Rate
Current Smoking
Muscle Strength Exercise (per Week)
Aerobic Exercise Rate (per Week)
Nutrition State
2.3. Data Collection and Analysis
3. Results
3.1. Participants’ Characteristics
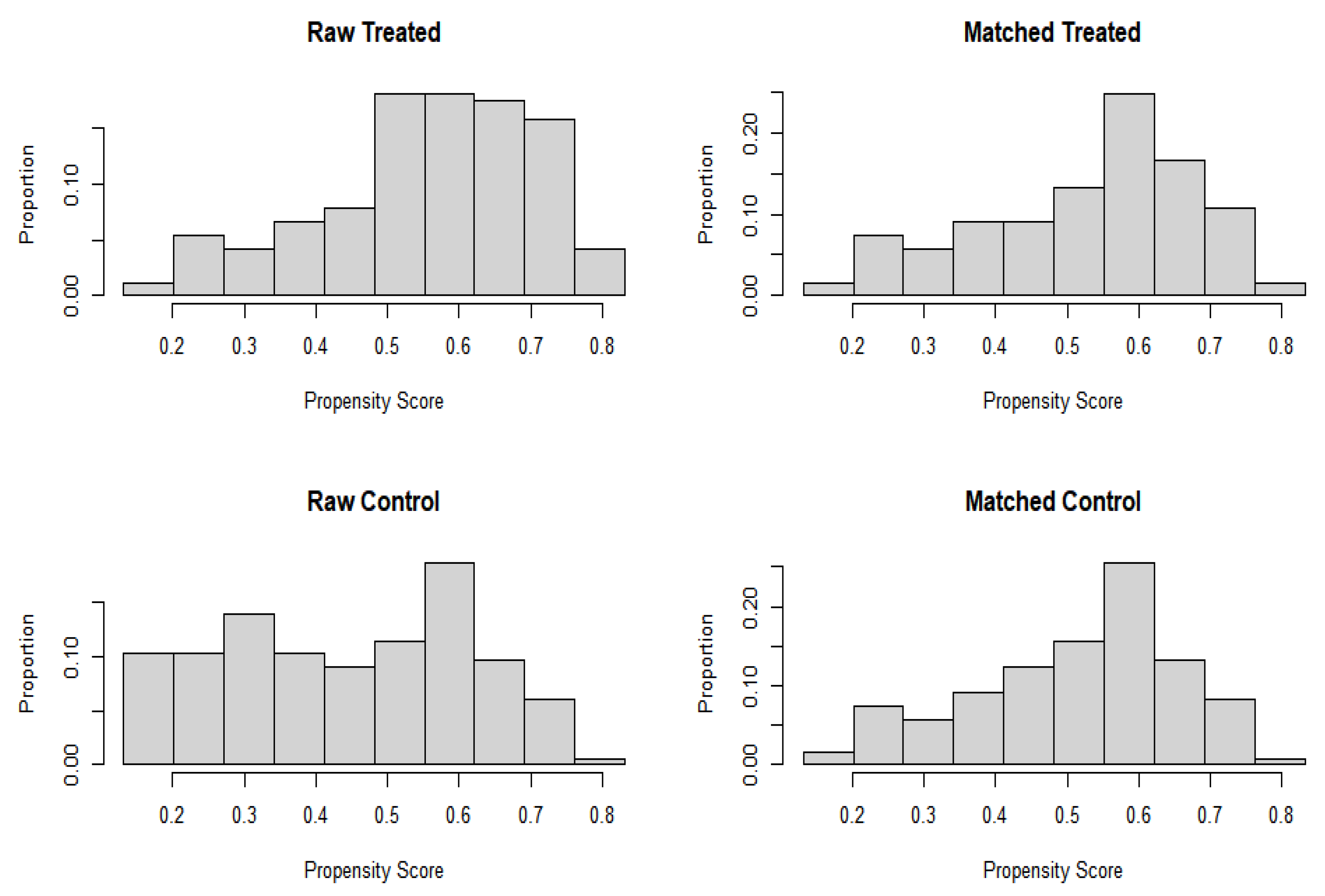
3.2. Participants’ Propensity Score Matching and Characteristic Comparison
3.3. Obesity-Associated Factors in Adult Women Who Experienced Early Menarche
4. Discussion
5. Conclusions
6. Limitations of the Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight Fact Sheet. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 3 November 2022).
- Korean Society for the Study of Obesity. Management of Obesity. 2014. Available online: http://general.kosso.or.kr/html/?pmode=BBBS0001300003&smode=view&seq=1214 (accessed on 3 November 2022).
- National Health Insurance Service. A Study on Improvement Plans for Insurers’ Obesity Management Projects to Improve Healthy Life Expectancy. 2017. Available online: http://lib.nhis.or.kr/search/detail/CATXAZ000000037289 (accessed on 3 November 2022).
- Ministry of the Interior and Safety. Comprehensive Plan for Obesity Prevention and Control. 2018. Available online: https://www.gov.kr/portal/ntnadmNews/1544415 (accessed on 3 November 2022).
- Korea Centers for Disease Control and Prevention. Seventh Korea National Health and Nutrition Examination Survey (KNHANES VII-3). 2019. Available online: http://www.mohw.go.kr/react/modules/download.jsp?BOARD_ID=140&CONT_SEQ=351319&FILE_SEQ=269105 (accessed on 3 November 2022).
- Prentice, P.; Viner, R.M. Pubertal timing and adult obesity and cardiometabolic risk in women and men: A systematic review and meta-analysis. Int. J. Obes. 2013, 37, 1036–1043. [Google Scholar] [CrossRef]
- LeBlanc, E.S.; Kapphahn, K.; Hedlin, H.; Desai, M.; Parikh, N.I.; Liu, S.; Parker, D.R.; Anderson, M.; Aroda, V.; Sullivan, S.; et al. Reproductive history and risk of type 2 diabetes mellitus in postmenopausal women: Findings from the women’s health initiative. Menopause 2017, 24, 64–72. [Google Scholar] [CrossRef]
- Thankamony, A.; Ong, K.K.; Ahmed, M.L.; Ness, A.R.; Holly, J.M.; Dunger, D.B. Higher levels of IGF-I and adrenal androgens at age 8 years are associated with earlier menarche in girls. J. Clin. Endocrinol. Metab. 2012, 97, E786–E790. [Google Scholar] [CrossRef]
- Lee, J.Y. Effect of early menarche on sexual experience among Korean high school girls. Child Health Nurs. Res. 2017, 23, 137–146. [Google Scholar] [CrossRef]
- Cheong, J.I.; Lee, C.H.; Park, J.H.; Ye, B.J.; Kwon, K.A.; Lee, Y.S.; Yoo, J.H. The effect of early menarche on the sexual behaviors of korean female adolescents. Ann. Pediatr. Endocrinol. Metab. 2015, 20, 130. [Google Scholar] [CrossRef]
- Kang, C.K.; Oh, W.O. Factors influencing self-esteem of girls with precocious puberty. J. East-West Nurs. Res. 2019, 25, 41–49. [Google Scholar] [CrossRef]
- Organization for Economic Cooperation and Development. Obesity Update. 2017. Available online: https://www.oecd.org/health/health-systems/obesity-update.htm (accessed on 3 November 2022).
- Mukora-Mutseyekwa, F.; Zeeb, H.; Nengomasha, L.; Adjei, N.F. Trends in prevalence and related risk factors of overweight and obesity among women of reproductive age in Zimbabwe, 2005–2015. Int. J. Environ. Res. Public Health. 2019, 16, 2758. [Google Scholar] [CrossRef] [PubMed]
- Roskam, A.J.R.; Kunst, A.E.; van Oyen, H.; Demarest, S.; Klumbiene, J.; Regidor, E.; Helmert, U.; Jusot, F.; Dzurova, D.; Mackenbach, J.P. Comparative appraisal of educational inequalities in overweight and obesity among adults in 19 European countries. Int. J. Epidemiol. 2010, 39, 392–404. [Google Scholar] [CrossRef] [PubMed]
- Rosiek, A.; Maciejewska, N.F.; Leksowski, K.; Rosiek-Kryszewska, A.; Leksowsk, L. Effect of television on obesity and excess of weight and consequences of health. Int. J. Environ. Res. Public Health. 2015, 12, 9408–9426. [Google Scholar] [CrossRef]
- Yoon, N.H.; Kwon, S.M. The effects of community environmental factors on obesity among Korean adults: A multilevel analysis. Epidemiol. Health. 2014, 36, e2014036. [Google Scholar] [CrossRef]
- Shlisky, J.D.; Hartman, T.J.; Kris-Etherton, P.M.; Rogers, C.J.; Sharkey, N.A.; Nickols-Richardson, S.M. Partial sleep deprivation and energy balance in adults: An emerging issue for consideration by dietetics practitioners. J. Acad. Nutr. Diet. 2012, 112, 1785–1797. [Google Scholar] [CrossRef] [PubMed]
- Kwak, J.W.; Jeon, C.H.; Kwak, M.H.; Kim, J.H.; Park, Y.S. Relationship between obesity and lifestyle factors in young Korean women: The seventh Korea national health and nutrition examination survey 2016. Korean J. Health Promot. 2019, 19, 9–15. [Google Scholar] [CrossRef]
- Pereira, M.A.; Kartashov, A.I.; Ebbeling, C.B.; Van Horn, L.; Slattery, M.L.; Jacobs, D.R.; Ludwig, D.S. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet 2005, 365, 36–42. [Google Scholar] [CrossRef]
- Tuovinen, E.L.; Saarni, S.E.; Männistö, S.; Borodulin, K.; Patja, K.; Kinnunen, T.H.; Kaprio, J.; Korhonen, T. Smoking status and abdominal obesity among normal- and overweight/obese adults: Population-based FINRISK study. Prev. Med. Rep. 2016, 4, 324–330. [Google Scholar] [CrossRef]
- Kim, Y.J.; Han, S.L. Associations between exposure to unhealthy food outlets within residential district and obesity: Using data from 2013 census on establishments and 2013–2014 Korea national health and nutrition examination survey. Korean J. Commun. Nutr. 2016, 21, 463–476. [Google Scholar] [CrossRef]
- Craig, L.C.; McNeill, G.; Macdiarmid, J.I.; Masson, L.F.; Holmes, B.A. Dietary patterns of school-age children in Scotland: Association with socioeconomic indicators, physical activity and obesity. Br. J. Nutr. 2010, 103, 319–334. [Google Scholar] [CrossRef] [PubMed]
- Drenowatz, C.; Eisenmann, J.C.; Pfeiffer, K.A.; Welk, G.; Heelan, K.; Gentile, D.; Walsh, D. Influence of socio-economic status on habitual physical activity and sedentary behavior in 8- to 11-year old children. BMC Public Health. 2010, 10, 241. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Baek, J.I. FUZZY matching using propensity score: IBM SPSS 22 Ver. J. Korean Data Inf. Sci. Soc. 2016, 27, 91–100. [Google Scholar] [CrossRef]
- Guo, S.; Frasher, M.W. Propensity Score Analysis: Statistical Methods and Applications, 2nd ed.; SAGE Publication: Los Angeles, CA, USA, 2014; pp. 1–409. [Google Scholar]
- Korea National Health and Nutrition Examination Survey. Seventh Korea National Health and Nutrition Examination Survey (KNHANES VII-3) 2018. 2017. Available online: https://www.seoulnutri.co.kr/food-db/49.do?curPage=1 (accessed on 3 November 2022).
- Hsieh, F.Y.; Bloch, D.A.; Larsen, M.D. A simple method of sample size calculation for linear and logistic regression. Stat. Med. 1998, 17, 1623–1634. [Google Scholar] [CrossRef]
- Son, Y.J.; Kim, G. The relationship between obesity, self-esteem and depressive symptoms of adult women in Korea. Korean J. Obes. 2012, 21, 89–98. Available online: https://www.koreamed.org/SearchBasic.php?RID=0134KJO/2012.21.2.89&DT=1 (accessed on 3 November 2022). [CrossRef]
- Korean Diabetes Association. Clinical Practice Guidelines for Diabetes 2013. 2014. Available online: https://www.diabetes.or.kr/pro/publication/view.php?number=46&sale_status=N (accessed on 3 November 2022).
- Knight, J.A.; Wong, J.; Blackmore, K.M.; Raboud, J.M.; Vieth, R. Vitamin D association with estradiol and progesterone in young women. Cancer Causes Control. 2010, 21, 479–483. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.K. Age at Menarche and BMI at Early Adulthood: Mendelian Randomization. Ph.D. Thesis, Graduate School of Seoul National University, Seoul, Republic of Korea, 2018. [Google Scholar]
- Lieberotha, S.; Gadea, E.; Kyvik, K.O.; Backer, V.; Thomsen, S.F. Early menarche is associated with increased risk of asthma: Prospective population-based study of twins. Respir. Med. 2015, 109, 565–571. [Google Scholar] [CrossRef]
- Won, J.C.; Hong, J.W.; Noh, J.H.; Kim, D.J. Association between age at menarche and risk factors for cardiovascular diseases in Korean women: The 2010 to 2013 Korea national health and nutrition examination survey. Medicine 2016, 95, 3580–3589. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, A.; Jungbluth Rodriguez, K.; Sabag, A.; Mavros, Y.; Parker, H.M.; Keating, S.E.; Johnson, N.A. Effect of aerobic exercise on waist circumference in adults with overweight or obesity: A systematic review and meta-analysis. Obes. Rev. 2022, 23, e13446. [Google Scholar] [CrossRef] [PubMed]
- Verheggen, R.; Maessen, M.; Green, D.J.; Hermus, A.; Hopman, M.; Thijssen, D. A systematic review and meta-analysis on the effects of exercise training versus hypocaloric diet: Distinct effects on body weight and visceral adipose tissue. Obes. Rev. 2016, 17, 664–690. [Google Scholar] [CrossRef] [PubMed]
- Nwaezuoke, C.A.; Gbonjubola, Y.T. Aerobic exercise as a non-medicinal option in the management of primary dysmenorrhea: A critical review. Adesh Univ. J. Med. Sci. Res. 2022, 4, 3–9. [Google Scholar] [CrossRef]
- World Health Organization. Guidelines on Physical Activity and Sedentary Behaviour. 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/336656/9789240015128-eng.pdf (accessed on 3 November 2022).
- Blakeley, C.E.; Van Rompay, M.I.; Schultz, N.S.; Sacheck, J.M. Relationship between muscle strength and dyslipidemia, serum 25(OH)D, and weight status among diverse schoolchildren: A cross-sectional analysis. BMC Pediatr. 2018, 18, 23. [Google Scholar] [CrossRef]
- Costa, T.; Murara, P.; Vancini, R.L.; de Lira, C.A.B.; Andrade, M.S. Influence of biological maturity on the muscular strength of young male and female swimmers. J. Hum. Kinet. 2021, 78, 67–77. [Google Scholar] [CrossRef]

| Variables | Before Propensity Score Matching | After Propensity Score Matching | ||||
|---|---|---|---|---|---|---|
| Mean of Obese Group (n = 165) | Mean of Non-Obese Group (n = 166) | Standardized Mean Difference | Mean of Obese Group (n = 121) | Mean of Non-Obese Group (n = 119) | Standardized Mean Difference | |
| Age | 1.68 | 1.78 | 0.76 | 1.69 | 1.69 | 0.76 |
| Education level | 1.67 | 1.55 | 0.50 | 1.62 | 1.60 | 0.49 |
| Marital status | 1.59 | 1.43 | 0.50 | 1.54 | 1.50 | 0.50 |
| Occupation | 1.39 | 1,39 | 0.49 | 1,45 | 1,38 | 0.48 |
| Personal income | 2.54 | 2.34 | 1.16 | 2.46 | 2.44 | 1.18 |
| Family income | 2.96 | 2.79 | 0.99 | 2.90 | 2.90 | 0.98 |
| Chronic disease | 0.20 | 0.45 | 0.50 | 0.26 | 0.28 | 0.45 |
| Labor delivery | 1.64 | 1.51 | 0.50 | 1.60 | 1.58 | 0.49 |
| Breast feeding | 1.70 | 1.60 | 0.49 | 1.67 | 1.67 | 0.47 |
| Contraceptive pill | 1.91 | 1.87 | 0.33 | 1.88 | 1.89 | 0.31 |
| Variables | Category | Obese Group (n = 121) | Non-Obese Group (n = 119) | χ2 (p) | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Age (years) | Under 30 | 59 | 24.6 | 62 | 25.8 | 0.83 (0.660) |
| 30–39 | 39 | 16.3 | 32 | 13.3 | ||
| Over 39 | 23 | 9.6 | 25 | 10.4 | ||
| Education level | Under middle school | 50 | 20.8 | 44 | 18.3 | 0.48 (0.490) |
| Middle school or more | 71 | 29.6 | 75 | 31.3 | ||
| Marital status | Yes | 59 | 24.6 | 55 | 22.9 | 0.16 (0.693) |
| None | 62 | 25.8 | 64 | 26.7 | ||
| Occupation | Yes | 72 | 30.0 | 66 | 27.5 | 0.48 (0.490) |
| None | 49 | 20.4 | 53 | 22.1 | ||
| Personal income | Low | 34 | 14.2 | 31 | 12.9 | 0.31 (0.958) |
| Middle | 28 | 11.7 | 31 | 12.9 | ||
| High | 26 | 10.8 | 25 | 10.4 | ||
| Family income | Low | 10 | 4.2 | 11 | 4.6 | 0.38 (0.278) |
| Middle-low | 35 | 14.6 | 25 | 10.4 | ||
| Middle-high | 33 | 13.8 | 45 | 18.8 | ||
| High | 43 | 17.9 | 38 | 15.8 | ||
| Chronic disease | Yes | 88 | 36.7 | 88 | 36.7 | 0.05 (0.830) |
| None | 33 | 13.8 | 31 | 12.9 | ||
| Labor delivery | Yes | 49 | 20.4 | 47 | 19.6 | 0.03 (0.874) |
| None | 72 | 30.0 | 72 | 30.0 | ||
| Breast feeding | Yes | 40 | 16.7 | 39 | 16.3 | 0.00 (0.963) |
| None | 81 | 33.8 | 80 | 33.3 | ||
| Contraceptive pill | Yes | 15 | 6.3 | 13 | 5.4 | 0.13 (0.722) |
| None | 106 | 44.2 | 106 | 88.3 | ||
| Variables | B | SE | p | Exp (B) | 95% CI of Exp (B) | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Stress cognition rate | 0.06 | 0.28 | 0.830 | 1.06 | 0.61 | 1.84 |
| Sleeping time during week | 0.15 | 0.28 | 0.591 | 1.16 | 0.67 | 2.02 |
| Alcohol consumption rate | 0.25 | 0.28 | 0.375 | 1.28 | 0.73 | 2.24 |
| Smoking | −0.27 | 0.22 | 0.229 | 0.76 | 0.48 | 1.18 |
| Aerobic exercise | −0.62 | 0.28 | 0.028 | 0.53 | 0.30 | 0.93 |
| Muscle-strengthening exercise | −1.09 | 0.33 | 0.001 | 0.33 | 0.17 | 0.64 |
| High-fat diet | −0.33 | 0.32 | 0.302 | 0.71 | 0.38 | 1.34 |
| High-carbohydrate diet | 0.13 | 0.35 | 0.695 | 1.14 | 0.57 | 2.28 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, H.; Han, J.-W. Obesity-Related Factors in Adult Women with Early Menarche. Healthcare 2023, 11, 557. https://doi.org/10.3390/healthcare11040557
Cho H, Han J-W. Obesity-Related Factors in Adult Women with Early Menarche. Healthcare. 2023; 11(4):557. https://doi.org/10.3390/healthcare11040557
Chicago/Turabian StyleCho, Hunha, and Jeong-Won Han. 2023. "Obesity-Related Factors in Adult Women with Early Menarche" Healthcare 11, no. 4: 557. https://doi.org/10.3390/healthcare11040557
APA StyleCho, H., & Han, J.-W. (2023). Obesity-Related Factors in Adult Women with Early Menarche. Healthcare, 11(4), 557. https://doi.org/10.3390/healthcare11040557








