How COVID-19 Broke the Barriers Related to the Implementation of Telecare—Patients’ Experiences with a New form of Providing Health Services in Primary Health Care
Abstract
:1. Introduction
- Analysis of general parameters related to the use of GPs by Poles during the pandemic;
- Determining the attitudes of Poles towards teleconsultations and readiness to use them in the future;
- The identification of strengths and weaknesses in the use of ICT systems or other communication systems in the provision of GP services.
2. Materials and Methods
- 4.
- Technical and organizational aspects of the implementation of teleconsultations
- 5.
- Evaluation of difficulties in the implementation of selected elements of teleconsultations
- 6.
- Overall effectiveness of teleconsultations
- 7.
- Opinions on teleconsultations
- 8.
- Willingness to recommend teleconsultations
Study Group
3. Results
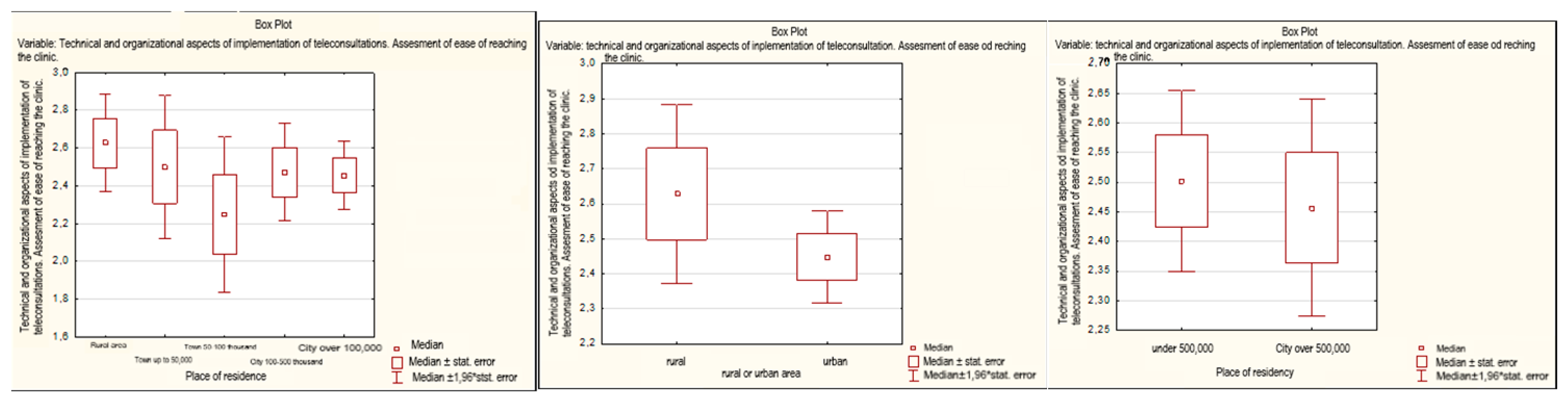
3.1. Technical Aspects of the Implementation of Teleconsultation
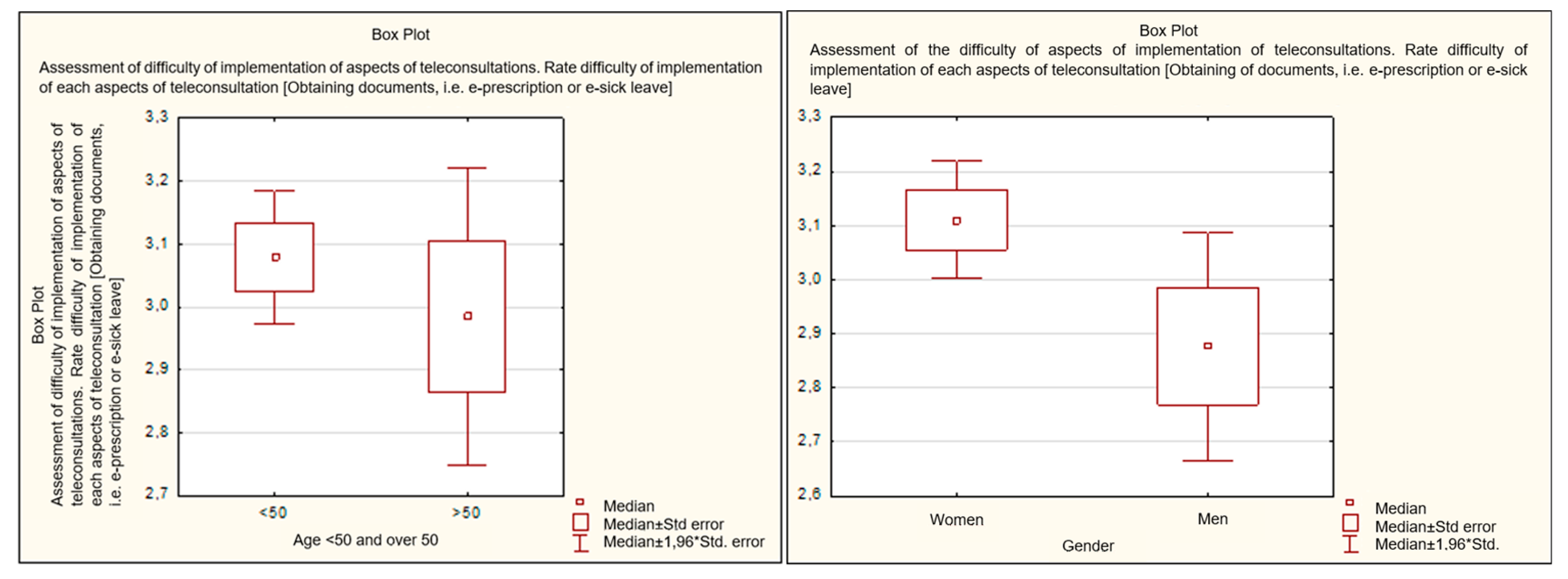
3.2. Evaluation of Difficulties in the Implementation of Selected Elements of Teleconsultations
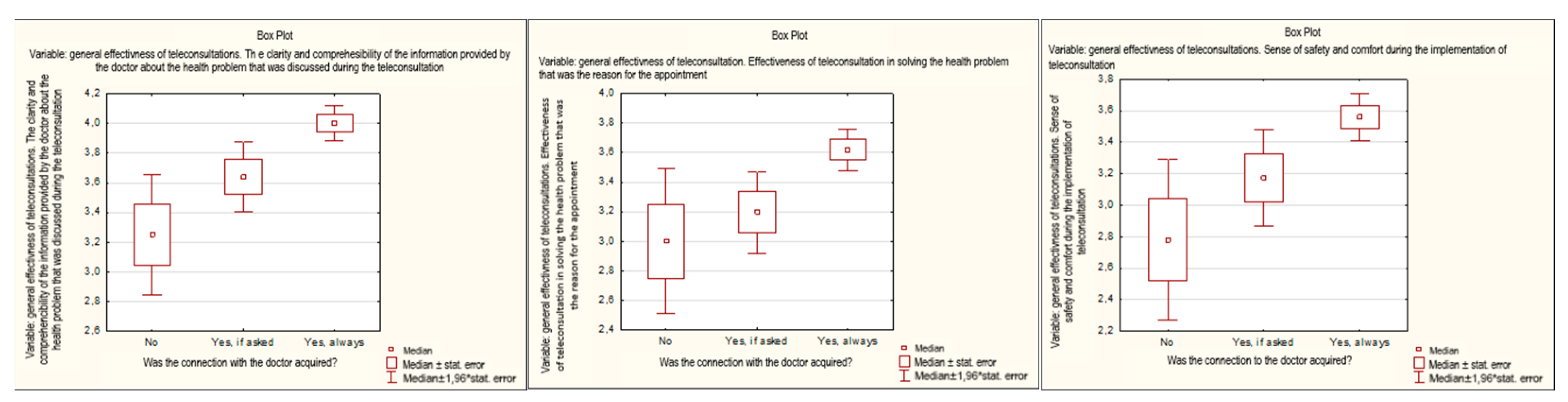
3.3. Overall Effectiveness of Teleconsultation
3.4. Opinions on Teleconsultation
3.5. Willingness to Recommend Teleconsultations
3.6. Advantages and Disadvantages of Teleconsultations
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Scantlebury, A.; Booth, A.; Hanley, B. Experiences, practices and barriers to accessing health information: A qualitative study. Int. J. Med. Inform. 2017, 103, 103–108. [Google Scholar] [PubMed]
- Jung, S.O.; Son, Y.H.; Choi, E. E-health literacy in older adults: An evolutionary concept analysis. BMC Med. Inf. Decis. Mak. 2022, 22, 28. [Google Scholar] [CrossRef]
- World Health Organization. Classification of Digital Health Interventions v1.0: A Shared Language to Describe the Uses of Digital Technology for Health. WHO/RHR/18.06. 2018. Available online: https://apps.who.int/iris/bitstream/handle/10665/260480/WHO-RHR-18.06-eng.pdf (accessed on 10 December 2022). [CrossRef]
- Van Dyk, L.A. Review of Telehealth Service Implementation Frameworks. IJERPH 2014, 11, 1279–1298. [Google Scholar] [CrossRef] [PubMed]
- Salisbury, C.; Murphy, M.; Duncan, P. The Impact of Digital-First Consultations on Workload in General Practice: Modeling Study. J. Med. Internet Res. 2020, 22, e18203. [Google Scholar] [CrossRef] [PubMed]
- Rogalska, A.; Syrkiewicz-Świtała, M. Rola działań w zakresie e-zdrowia w obliczu pandemii COVID-19. E-Wydawnictwo. Prawnicza i Ekonomiczna Biblioteka Cyfrowa. Wydział Prawa, Administracji i Ekonomii Uniwersytetu Wrocławskiego 2021. [Google Scholar] [CrossRef]
- Keesara, S.; Jonas, A.; Schulman, K. Covid-19 and Health Care’s Digital Revolution. N. Engl. J. Med. 2020, 382, 82. [Google Scholar] [CrossRef] [PubMed]
- Kichloo, A.; Albosta, M.; Dettloff, K.; Wani, F.; El-Amir, Z.; Singh, J.; Aljadah, M.; Chakinala, R.C.; Kanugula, A.K.; Solanki, S.; et al. Telemedicine, the current COVID-19 pandemic and the future: A narrative review and perspectives moving forward in the USA. Fam. Med. Community Health 2020, 8, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Picardo, E.; Bau, M.; Anatrone, C.; Mondino, A.; Surace, A.; Gallo, F.; Danese, S.; Mitidieri, M. Oncophone20 study: Patients’ perception of telemedicine in the COVID-19 pandemic during follow-up visits for gynecological and breast cancers. Int. J. Gynaecol. Obstet. 2021, 155, 398–403. [Google Scholar] [PubMed]
- Lechien, J.R.; Radulesco, T.; Distinguin, L.; Chekkoury-Idrissi, Y.; Circiu, M.; EL Afia, F.; Michel, J.; Papon, J.F. Patient and otolaryngologist perceptions of telemedicine during COVID-19 pandemic. Eur. Arch. Otorhinolaryngol. 2021, 278, 4101–4105. [Google Scholar] [CrossRef] [PubMed]
- Narodowy Fundusz Zdrowia. Zarządzenie Prezesa NFZ Nr 39/2020/DSOZ Zmieniające Zarządzenie w Sprawie Warunków Zawarcia i Realizacji Umów o Udzielanie Świadczen Opieki Zdrowotnej w Zakresie Podstawowej Opieki Zdrowotnej. Available online: https://www.nfz.gov.pl/zarzadzenia-prezesa/zarzadzenia-prezesa-nfz/zarzadzenie-nr-392020dsoz,7150.html (accessed on 11 November 2022).
- Central Statistical Office. Outpatient Healthcare in 2021. Available online: https://stat.gov.pl/obszary-tematyczne/zdrowie/zdrowie/ambulatoryjna-opieka-zdrowotna-w-2021-roku,13,6.html (accessed on 27 January 2023).
- Gupta, S.; Sundaram, S.S. A Review of Telemedicine Practice Guidelines for COVID-19 and Global Emergencies. INQUIRY J. Med. Care Organ. Provis. Financ. 2022, 59, 469580211059989. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Consolidation Telemedicine Guide. 2022. Available online: https://www.who.int/publications-detail-redirect/9789240059184 (accessed on 11 November 2022).
- Bouabida, K.; Lebouché, B.; Pomey, M.P. Telehealth and COVID-19 Pandemic: An Overview of the Telehealth Use, Advantages, Challenges, and Opportunities during COVID-19 Pandemic. Healthcare 2022, 10, 2293. [Google Scholar] [CrossRef] [PubMed]
- Grata-Borkowska, U.; Sobieski, M.; Drobnik, J.; Fabich, E.; Bujnowska-Fedak, M.M. Perception and Attitude toward Teleconsultations among Different Healthcare Professionals in the Era of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 11532. [Google Scholar] [CrossRef] [PubMed]
- Grata-Borkowska, U.; Sobieski, M.; Drobnik, J.; Fabich, E.; Bujnowska-Fedak, M.M. Use of Medical Teleconsultations During the COVID-19 Pandemic in Poland-Preliminary Results. In Proceedings of the 15th International Conference on Digital Society (ICDS 2021), Nice, France, 18–22 July 2021. [Google Scholar]
- Opinc, A.; Łukasik, Z.; Makowska, J. The attitude of Polish rheumatology patients towards telemedicine in the age of the COVID-19 pandemic. Reumatologia 2020, 58, 134–141. [Google Scholar]
- Kludacz-Alessandri, M.; Hawrysz, L.; Korneta, P.; Gierszewska, G.; Pomaranik, W.; Walczak, R. The impact of medical teleconsultations on general practitioner-patient communication during COVID-19: A case study from Poland. PLoS ONE 2021, 16, e0254960. [Google Scholar] [CrossRef]
- Stepaniuk, A.; Pawlukianiec, C.; Krawiel, M.; Lewoc, M.; Baran, A.; Flisiak, I. Great hopes or disappointment–a survey-based study on patients’ and doctors’ perception of telemedicine during the COVID-19 pandemic in Poland. Adv. Dermatol. Allergol. 2022, 39, 384–391. [Google Scholar]
- Frankowska, A.; Szymkowiak, M.; Walkowiak, D. Walkowiak. Teleconsultations Quality During the COVID-19 Pandemic in Poland in the Opinions of Generation Z Adults. Telemed. e-Health 2022, 28, 1843–1851. [Google Scholar] [CrossRef] [PubMed]
- Nitiema, P. Telehealth Before and During the COVID-19 Pandemic: Analysis of Health Care Workers’ Opinions. J. Med. Internet Res. 2022, 24, e29519. [Google Scholar] [CrossRef]
- Hincapié, M.A.; Gallego, J.C.; Gempeler, A.; Piñeros, J.A.; Nasner, D.; Escobar, M.F. Implementation and Usefulness of Telemedicine During the COVID-19 Pandemic: A Scoping Review. J. Prim. Care Community Health 2020, 11, 2150132720980612. [Google Scholar]
- Ftouni, R.; AlJardali, B.; Hamdanieh, M.; Ftouni, L.; Salem, N. Challenges of Telemedicine during the COVID-19 pandemic: A systematic review. BMC Med. Inf. Decis. Mak. 2022, 22, 207. [Google Scholar] [CrossRef]
- Narodowy Fundusz Zdrowia. Raport z Badania Satysfakacji Pacjentów Korzystających z Teleporad u Lekarza Podstawowej Opieki Zdrowotnej w Okresie Epidemii COVID-19. 2020. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwjMoIORrYP9AhWKjqQKHfldBroQFnoECA0QAQ&url=https%3A%2F%2Fwww.gov.pl%2Fattachment%2Fa702e12b-8b16-44f1-92b5-73aaef6c165c&usg=AOvVaw3h_roOXVcv9ZCTY7yXmn80 (accessed on 10 December 2022).
- Narasimha, S.; Madathil, K.C.; Agnisarman, S.; Rogers, H.; Welch, B.; Ashok, A.; Nair, A.; McElligott, J. Designing Telemedicine Systems for Geriatric Patients: A Review of the Usability Studies. Telemed. E-Health 2017, 23, 459–472. [Google Scholar] [CrossRef]
- Eberly, L.A.; Kallan, M.J.; Julien, H.M.; Haynes, N.; Khatana, S.A.M.; Nathan, A.S.; Snider, C.; Chokshi, N.P.; Eneanya, N.D.; Takvorian, S.U.; et al. Patient Characteristics Associated with Telemedicine Access for Primary and Specialty Ambulatory Care During the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2031640. [Google Scholar] [CrossRef] [PubMed]
- Imlach, F.; McKinlay, E.; Middleton, L.; Kennedy, J.; Pledger, M.; Russell, L.; Churchward, M.; Cumming, J.; McBride-Henry, K. Telehealth consultations in general practice during a pandemic lockdown: Survey and interviews on patient experiences and preferences. BMC Fam. Pract. 2020, 21, 269. [Google Scholar] [CrossRef] [PubMed]
- Chwistek, M. “Are You Wearing Your White Coat?”: Telemedicine in the Time of Pandemic. JAMA 2020, 324, 149. [Google Scholar] [CrossRef] [PubMed]
- Wade, V.A.; Karnon, J.; Elshaug, A.G.; Hiller, J.E. A systematic review of economic analyses of telehealth services using real time video communication. BMC Health Serv. Res. 2010, 10, 233. [Google Scholar] [CrossRef]
- Sutherland, A.E.; Stickland, J.; Wee, B. Can video consultations replace face-to-face interviews? Palliative medicine and the Covid-19 pandemic: Rapid review. BMJ Support Palliat. Care 2020, 10, 271–275. [Google Scholar] [CrossRef]
- Rahman, S.; Amit, S.; Kafy, A.A. Gender disparity in telehealth usage in Bangladesh during COVID-19. SSM Ment. Health 2022, 2, 100054. [Google Scholar] [CrossRef]
- Hasan, A.; Bhattacharya, S.; Kartikeyan, S. Gender Differences in Awareness and Use of Telemedicine amongst Allopathic Medicos. IJSR 2020, 9, 15. Available online: https://www.researchgate.net/publication/358387741_GENDER_DIFFERENCES_IN_AWARENESS_AND_USE_OF_TELEMEDICINE_AMONGST_ALLOPATHIC_MEDICOS (accessed on 14 December 2022).
- Goldstein, K.M.; Zullig, L.L.; Dedert, E.A.; Tabriz, A.A.; Brearly, T.W.; Raitz, G.; Sata, S.S.; Whited, J.D.; Bosworth, H.B.; Gordon, A.M.; et al. Telehealth Interventions Designed for Women: An Evidence Map. J. Gen. Intern. Med. 2018, 33, 2191–2200. [Google Scholar] [CrossRef]
- Mason, A.N.; Brown, M.; Mason, K. Telemedicine Patient Satisfaction Dimensions Moderated by Patient Demographics. Healthcare 2022, 10, 1029. [Google Scholar] [CrossRef]
- Bagchi, A.D.; Damas, K.; de Noguera, N.S.; Melamed, B.; Menifield, C.; Baveja, A.; Weber, P.; Swaminathan, S. Comfort with Telehealth Among Residents of an Underserved Urban Area. J. Prim. Care Community Health 2022, 13, 21501319221119692. [Google Scholar] [CrossRef]
- Guise, V.; Anderson, J.; Wiig, S. Patient safety risks associated with telecare: A systematic review and narrative synthesis of the literature. BMC Health Serv. Res. 2014, 14, 588. [Google Scholar] [CrossRef]
- Gordon, H.S.; Solanki, P.; Bokhour, B.G.; Gopal, R.K. “I’m Not Feeling Like I’m Part of the Conversation” Patients’ Perspectives on Communicating in Clinical Video Telehealth Visits. J. Gen. Intern. Med. 2020, 35, 1751–1758. [Google Scholar] [CrossRef]
- Locatelli, S.M.; LaVela, S.L.; Talbot, M.E.; Davies, M.L. How do patients respond when confronted with telephone access barriers to care? Health Expect. 2015, 18, 2154–2163. [Google Scholar]
| Feature | N = 408 |
|---|---|
| Age (years) | |
| Average | 35.52 |
| Standard deviation | 14.61 |
| Median | 27 |
| Minimum/Maximum | 17/87 |
| Age (N; %) | |
| Under 50 years of age | 342; 83.82% |
| Over 50 years of age | 66; 16.18% |
| Gender, (N;%) | |
| Women | 327; 80.15% |
| Men | 81; 19.85% |
| Place of residence (N;%) | |
| Rural area | 78; 19.12% |
| Town up to 50,000 residents | 42; 10.29% |
| City of 50–100 thousand inhabitants | 28; 6.86% |
| City of 100–500 thousand inhabitants | 87; 21.32% |
| City over 100 thousand inhabitants | 173; 42.40% |
| Education (N;%) | |
| Primary or junior high school | 4; 0.98% |
| Professional | 15; 3.68% |
| High school | 171; 41.91% |
| Higher education | 218; 53.43% |
| Marital Status (N;%) | |
| Married | 138; 33.82% |
| Widow/Widower | 4; 0.98% |
| Single | 255; 62.50% |
| Divorced/Separated | 11; 2.70% |
| Having offspring (N;%) | |
| Yes | 137; 33.58% |
| No | 271; 66.42% |
| Frequency of GP visits (N;%) | |
| 1–2× per year | 172; 42.16% |
| 3–6× per year | 170; 41.67% |
| 6–12× per year | 59; 14.46% |
| more than 12 times a year (i.e., more than once a month) | 7; 1.72% |
| Advantages and Disadvantages of Teleconsultations | The Most Frequently Indicated Response | Number | % |
|---|---|---|---|
| Advantages: | |||
| Teleconsultations provide easier access to doctors, a greater choice of specialists | Rather yes | 140 | 34.31% |
| Teleconsultations provide short waiting times for appointment | Rather yes | 164 | 40.39% |
| Teleconsultations provide greater mental comfort than when talking in the office | Rather not | 182 | 44.61% |
| Teleconsultation is convenient, no need to leave home, no travel costs | Definitely yes | 199 | 48.77% |
| Teleconsultations increase epidemiological safety | Definitely yes | 220 | 53.92% |
| Teleconsultation is the absence of the need to reschedule at work or to leave work in order to go to the clinic | Definitely yes | 192 | 47.06% |
| Disadvantages: | |||
| Teleconsultation is a hardware limitation, difficulty in accessing the clinic | Definitely yes | 144 | 35.29% |
| Lack of physical examination and related fears that the doctor will make the wrong diagnosis | Definitely yes | 297 | 72.79% |
| Unintelligible doctor’s recommendations, communication problems with the doctor | Rather not | 206 | 50.49% |
| Lack of information from the clinic at what time the doctor will call or appointment at different time than originally designated | Rather not | 124 | 30.39% |
| N | Mean | Std. Dev. | r (X, Y) | R2 | p | |
|---|---|---|---|---|---|---|
| I am ready to recommend teleconsultation to my friends and/or family as convenient | 407 | 2.77 | 1.41 | |||
| Clarity and comprehensibility of information shared by the doctor about related health issue | 3.87 | 1.07 | 0.49 | 0.24 | 0.00 | |
| Effectiveness of teleconsultation in solving the health problem which was the reason for the appointment | 3.49 | 1.28 | 0.55 | 0.30 | 0.00 | |
| Sense of safety and comfort during teleconsultation | 3.42 | 1.35 | 0.61 | 0.37 | 0.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciećko, W.; Labunets, K.; Wojnarowska, M.; Bosek, D.; Skwierawska, J.; Bandurski, T.; Bandurska, E. How COVID-19 Broke the Barriers Related to the Implementation of Telecare—Patients’ Experiences with a New form of Providing Health Services in Primary Health Care. Healthcare 2023, 11, 497. https://doi.org/10.3390/healthcare11040497
Ciećko W, Labunets K, Wojnarowska M, Bosek D, Skwierawska J, Bandurski T, Bandurska E. How COVID-19 Broke the Barriers Related to the Implementation of Telecare—Patients’ Experiences with a New form of Providing Health Services in Primary Health Care. Healthcare. 2023; 11(4):497. https://doi.org/10.3390/healthcare11040497
Chicago/Turabian StyleCiećko, Weronika, Kinga Labunets, Małgorzata Wojnarowska, Dominika Bosek, Justyna Skwierawska, Tomasz Bandurski, and Ewa Bandurska. 2023. "How COVID-19 Broke the Barriers Related to the Implementation of Telecare—Patients’ Experiences with a New form of Providing Health Services in Primary Health Care" Healthcare 11, no. 4: 497. https://doi.org/10.3390/healthcare11040497
APA StyleCiećko, W., Labunets, K., Wojnarowska, M., Bosek, D., Skwierawska, J., Bandurski, T., & Bandurska, E. (2023). How COVID-19 Broke the Barriers Related to the Implementation of Telecare—Patients’ Experiences with a New form of Providing Health Services in Primary Health Care. Healthcare, 11(4), 497. https://doi.org/10.3390/healthcare11040497






