Development and Validation of a Risk-Prediction Nomogram for Chronic Low Back Pain Using a National Health Examination Survey: A Cross-Sectional Study
Abstract
1. Background
2. Methods
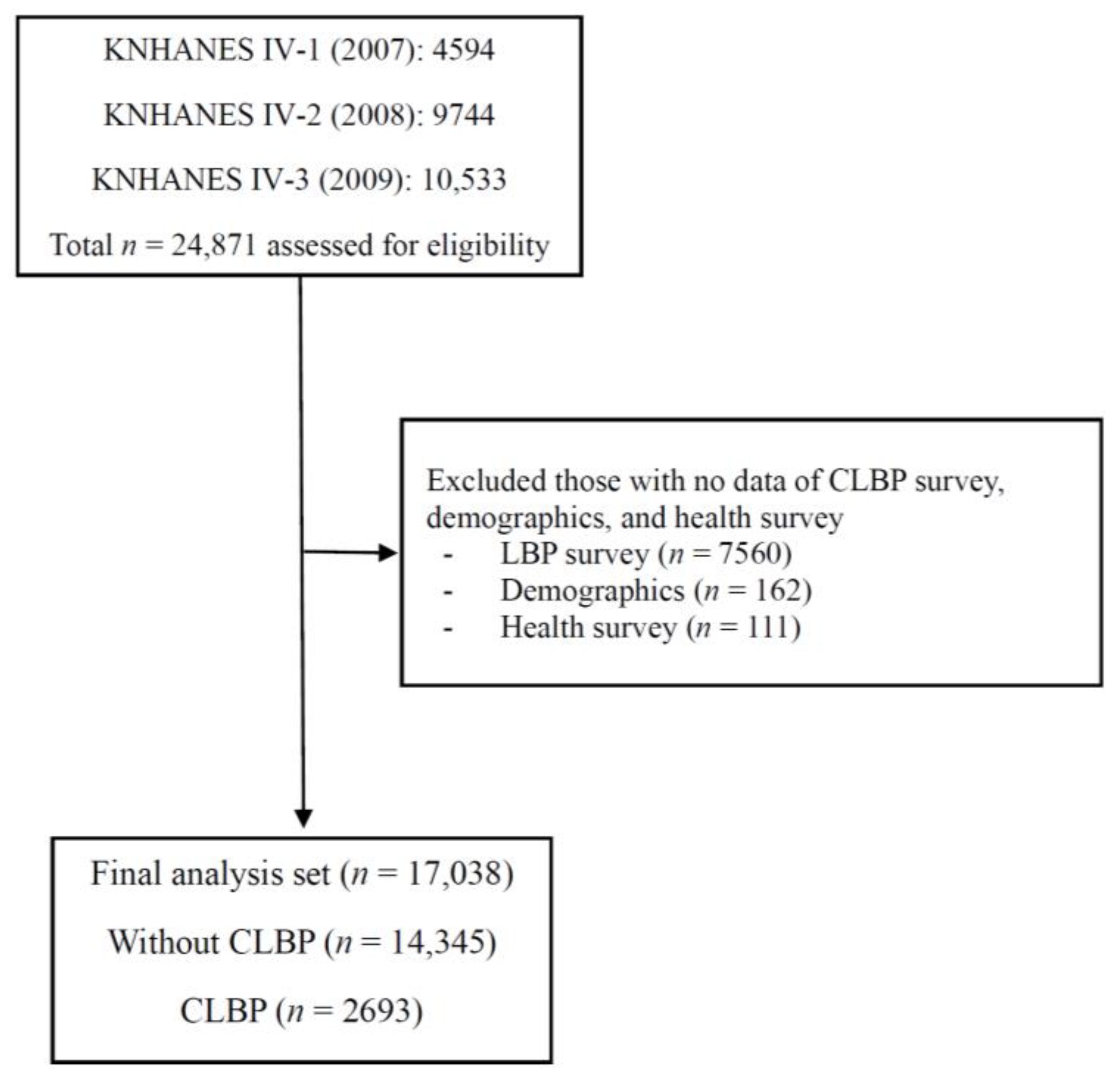
2.1. Study Design, Setting and Participants
2.2. Definitions of Chronic Low Back Pain
2.3. Data Sources, Measurements and Variables
2.4. Statistical Analysis
2.5. Ethics Approval and Consent to Participate
3. Results
3.1. Demographics of Participants
3.2. Risk Factors for the Prediction Model
3.3. Discrimination and Calibration of the Prediction Model
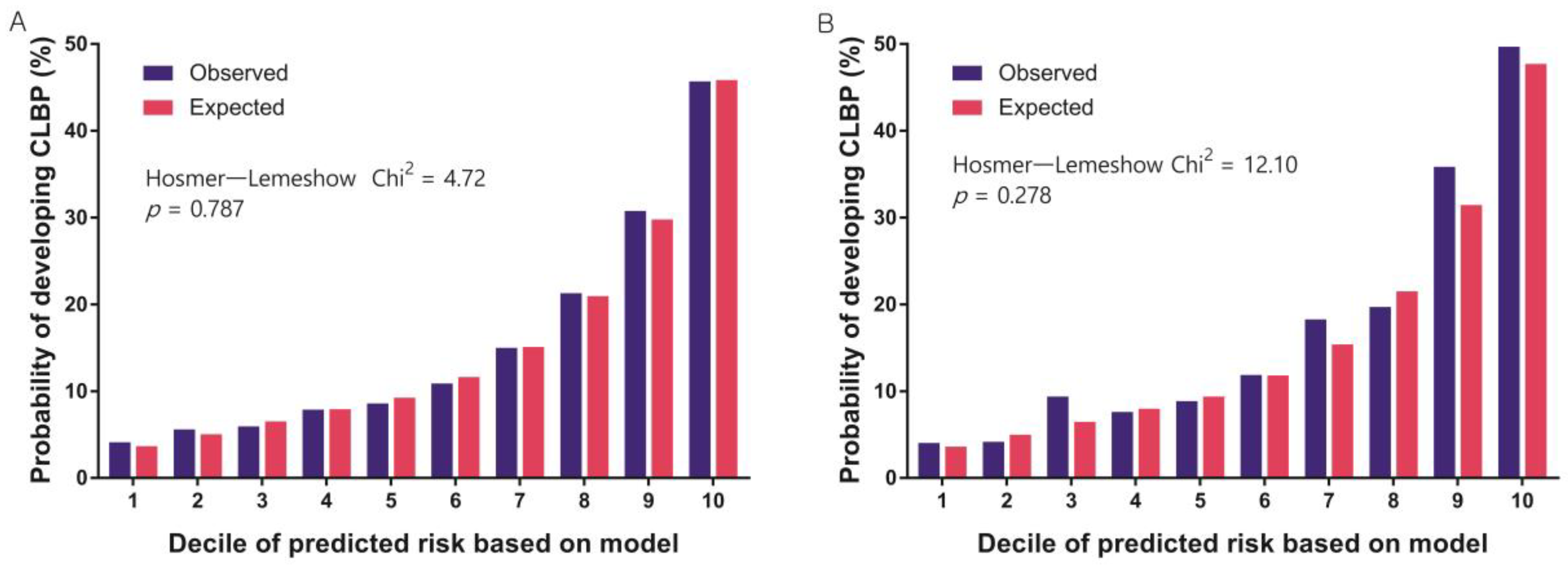
3.4. Nomogram for the Prediction Model
4. Discussion
Strengths and Limitations of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Balague, F.; Mannion, A.F.; Pellise, F.; Cedraschi, C. Non-specific low back pain. Lancet 2012, 379, 482–491. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.Y.; Song, K.S.; Cho, J.H.; Lee, J.H.; Kim, N.H. An Updated Overview of Low Back Pain Management. Asian Spine J. 2022, 16, 968–982. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.S.; Lee, K.C.; Dhake, R.P.; Longworth, S.; Sell, P. Ability of Spine Specialists to Identify Psychosocial Risk Factors as Obstacles to Recovery in Patients with Low Back Pain-Related Disorders. Asian Spine J. 2021, 15, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Ogon, I.; Iba, K.; Takashima, H.; Yoshimoto, M.; Morita, T.; Oshigiri, T.; Terashima, Y.; Emori, M.; Teramoto, A.; Takebayashi, T.; et al. Magnetic Resonance Spectroscopic Analysis of Multifidus Muscle Lipid Contents and Association with Nociceptive Pain in Chronic Low Back Pain. Asian Spine J. 2021, 15, 441–446. [Google Scholar] [CrossRef]
- Choi, J.Y.; Park, S.M.; Kim, H.J.; Yeom, J.S. Recent Updates on Minimally Invasive Spine Surgery: Techniques, Technologies, and Indications. Asian Spine J. 2022, 16, 1013–1021. [Google Scholar] [CrossRef] [PubMed]
- Frank, J.W.; Brooker, A.S.; DeMaio, S.E.; Kerr, M.S.; Maetzel, A.; Shannon, H.S.; Sullivan, T.J.; Norman, R.W.; Wells, R.P. Disability resulting from occupational low back pain. Part II: What do we know about secondary prevention? A review of the scientific evidence on prevention after disability begins. Spine 1996, 21, 2918–2929. [Google Scholar] [CrossRef] [PubMed]
- Nieminen, L.K.; Pyysalo, L.M.; Kankaanpaa, M.J. Prognostic factors for pain chronicity in low back pain: A systematic review. Pain Rep. 2021, 6, e919. [Google Scholar] [CrossRef] [PubMed]
- de Souza, I.M.B.; Sakaguchi, T.F.; Yuan, S.L.K.; Matsutani, L.A.; do Espirito-Santo, A.S.; Pereira, C.A.B.; Marques, A.P. Prevalence of low back pain in the elderly population: A systematic review. Clinics 2019, 74, e789. [Google Scholar] [CrossRef]
- Wong, C.K.; Mak, R.Y.; Kwok, T.S.; Tsang, J.S.; Leung, M.Y.; Funabashi, M.; Macedo, L.G.; Dennett, L.; Wong, A.Y. Prevalence, Incidence, and Factors Associated With Non-Specific Chronic Low Back Pain in Community-Dwelling Older Adults Aged 60 Years and Older: A Systematic Review and Meta-Analysis. J. Pain Off. J. Am. Pain Soc. 2022, 23, 509–534. [Google Scholar] [CrossRef] [PubMed]
- Park, S.M.; Kim, H.J.; Jeong, H.; Kim, H.; Chang, B.S.; Lee, C.K.; Yeom, J.S. Longer sitting time and low physical activity are closely associated with chronic low back pain in population over 50 years of age: A cross-sectional study using the sixth Korea National Health and Nutrition Examination Survey. Spine J. Off. J. North Am. Spine Soc. 2018, 18, 2051–2058. [Google Scholar] [CrossRef] [PubMed]
- Park, S.M.; Kim, H.J.; Jang, S.; Kim, H.; Chang, B.S.; Lee, C.K.; Yeom, J.S. Depression is Closely Associated With Chronic Low Back Pain in Patients Over 50 Years of Age: A Cross-sectional Study Using the Sixth Korea National Health and Nutrition Examination Survey (KNHANES VI-2). Spine 2018, 43, 1281–1288. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.; Jin, Y.S.; Lee, C.S.; Hwang, C.J.; Lee, S.Y.; Chung, S.G.; Choi, K.H. Relationship between the type and amount of physical activity and low back pain in Koreans aged 50 years and older. PM R J. Inj. Funct. Rehabil. 2014, 6, 893–899. [Google Scholar] [CrossRef] [PubMed]
- Park, S.M.; Kim, G.U.; Kim, H.J.; Kim, H.; Chang, B.S.; Lee, C.K.; Yeom, J.S. Walking more than 90minutes/week was associated with a lower risk of self-reported low back pain in persons over 50years of age: A cross-sectional study using the Korean National Health and Nutrition Examination Surveys. Spine J. Off. J. North Am. Spine Soc. 2019, 19, 846–852. [Google Scholar] [CrossRef] [PubMed]
- Park, S.M.; Kim, G.U.; Kim, H.J.; Kim, H.; Chang, B.S.; Lee, C.K.; Yeom, J.S. Low handgrip strength is closely associated with chronic low back pain among women aged 50 years or older: A cross-sectional study using a national health survey. PLoS ONE 2018, 13, e0207759. [Google Scholar] [CrossRef] [PubMed]
- Waddell, G. 1987 Volvo award in clinical sciences. A new clinical model for the treatment of low-back pain. Spine 1987, 12, 632–644. [Google Scholar] [CrossRef] [PubMed]
- Shiri, R.; Coggon, D.; Falah-Hassani, K. Exercise for the Prevention of Low Back Pain: Systematic Review and Meta-Analysis of Controlled Trials. Am. J. Epidemiol. 2018, 187, 1093–1101. [Google Scholar] [CrossRef] [PubMed]
- Hassoon, A.; Bydon, M.; Kerezoudis, P.; Maloney, P.R.; Rinaldo, L.; Yeh, H.C. Chronic low-back pain in adult with diabetes: NHANES 2009-2010. J. Diabetes Its Complicat. 2017, 31, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Parreira, P.; Maher, C.G.; Steffens, D.; Hancock, M.J.; Ferreira, M.L. Risk factors for low back pain and sciatica: An umbrella review. Spine J. Off. J. North Am. Spine Soc. 2018, 18, 1715–1721. [Google Scholar] [CrossRef]
- Parreira, P.C.S.; Maher, C.G.; Ferreira, M.L.; Machado, G.C.; Blyth, F.M.; Naganathan, V.; Waite, L.M.; Seibel, M.J.; Handelsman, D.; Cumming, R.G. A longitudinal study of the influence of comorbidities and lifestyle factors on low back pain in older men. Pain 2017, 158, 1571–1576. [Google Scholar] [CrossRef]
- Yang, M.; Wang, N.; Xu, X.; Zhang, Y.; Xu, G.; Chang, Y.; Li, Z. Facet joint parameters which may act as risk factors for chronic low back pain. J. Orthop. Surg. Res. 2020, 15, 185. [Google Scholar] [CrossRef]
- Thomas, E.; Silman, A.J.; Croft, P.R.; Papageorgiou, A.C.; Jayson, M.I.; Macfarlane, G.J. Predicting who develops chronic low back pain in primary care: A prospective study. BMJ 1999, 318, 1662–1667. [Google Scholar] [CrossRef]
- van den Hoogen, H.J.; Koes, B.W.; Deville, W.; van Eijk, J.T.; Bouter, L.M. The prognosis of low back pain in general practice. Spine 1997, 22, 1515–1521. [Google Scholar] [CrossRef] [PubMed]
- Kendall, N.A. Psychosocial approaches to the prevention of chronic pain: The low back paradigm. Baillieres Best Pract. Res. Clin. Rheumatol. 1999, 13, 545–554. [Google Scholar] [CrossRef] [PubMed]
- van der Windt, D.A.; Kuijpers, T.; Jellema, P.; van der Heijden, G.J.; Bouter, L.M. Do psychological factors predict outcome in both low-back pain and shoulder pain? Ann. Rheum. Dis. 2007, 66, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Heymans, M.W.; van Buuren, S.; Knol, D.L.; Anema, J.R.; van Mechelen, W.; de Vet, H.C. The prognosis of chronic low back pain is determined by changes in pain and disability in the initial period. Spine J. Off. J. North Am. Spine Soc. 2010, 10, 847–856. [Google Scholar] [CrossRef]
- Kwon, J.; Moon, S.; Park, S.; Park, S.; Park, S.; Suk, K.; Kim, H.; Lee, B. Lumbar Spinal Stenosis: Review Update 2022. Asian Spine J. 2022, 16, 789–798. [Google Scholar] [CrossRef] [PubMed]
- Kweon, S.; Kim, Y.; Jang, M.J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.H.; Oh, K. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef]
- Korea National Health and Nutrition Examination Survey. Available online: https://knhanes.kdca.go.kr/knhanes/eng/index.do (accessed on 21 July 2019).
- Punnett, L.; Pruss-Utun, A.; Nelson, D.I.; Fingerhut, M.A.; Leigh, J.; Tak, S.; Phillips, S. Estimating the global burden of low back pain attributable to combined occupational exposures. Am. J. Ind. Med. 2005, 48, 459–469. [Google Scholar] [CrossRef] [PubMed]
- Steyerberg, E.W.; Harrell, F.E., Jr. Prediction models need appropriate internal, internal-external, and external validation. J. Clin. Epidemiol. 2016, 69, 245–247. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C.; Steyerberg, E.W. Events per variable (EPV) and the relative performance of different strategies for estimating the out-of-sample validity of logistic regression models. Stat. Methods Med. Res. 2017, 26, 796–808. [Google Scholar] [CrossRef] [PubMed]
- Khor, S.; Lavallee, D.; Cizik, A.M.; Bellabarba, C.; Chapman, J.R.; Howe, C.R.; Lu, D.; Mohit, A.A.; Oskouian, R.J.; Roh, J.R.; et al. Development and Validation of a Prediction Model for Pain and Functional Outcomes After Lumbar Spine Surgery. JAMA Surg. 2018, 153, 634–642. [Google Scholar] [CrossRef]
- D’Agostino, R.B.; Grundy, S.; Sullivan, L.M.; Wilson, P.; Group, C.H.D.R.P. Validation of the Framingham coronary heart disease prediction scores: Results of a multiple ethnic groups investigation. JAMA 2001, 286, 180–187. [Google Scholar] [CrossRef]
- Zlotnik, A.; Abraira, V. Nomograms in Stata. Available online: http://www.zlotnik.net/stata/nomograms/ (accessed on 3 April 2018).
- Kopec, J.A.; Sayre, E.C.; Esdaile, J.M. Predictors of back pain in a general population cohort. Spine 2004, 29, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Shiri, R.; Karppinen, J.; Leino-Arjas, P.; Solovieva, S.; Viikari-Juntura, E. The association between smoking and low back pain: A meta-analysis. Am. J. Med. 2010, 123, e7–e35. [Google Scholar] [CrossRef]
- Solovev, A.; Watanabe, Y.; Kitamura, K.; Takahashi, A.; Kobayashi, R.; Saito, T.; Takachi, R.; Kabasawa, K.; Oshiki, R.; Platonova, K.; et al. Total physical activity and risk of chronic low back and knee pain in middle-aged and elderly Japanese people: The Murakami cohort study. Eur. J. Pain 2020, 24, 863–872. [Google Scholar] [CrossRef] [PubMed]


| Variables | Without CLBP (n = 14,345) | CLBP (n = 2693) | p-Value |
|---|---|---|---|
| Age, year | 47.3 (± 16.1) | 59.1 (± 16.0) | <0.001 |
| Age, n (%) | |||
| 10–19 | 174 (1.2%) | 4 (0.1%) | <0.001 |
| 20–29 | 1932 (13.5%) | 142 (5.3%) | |
| 30–39 | 3143 (21.9%) | 269 (10.0%) | |
| 40–49 | 3052 (21.3%) | 310 (11.5%) | |
| 50–59 | 2423 (16.9%) | 439 (16.3%) | |
| 60–69 | 2038 (14.2%) | 698 (25.9%) | |
| 70–79 | 1296 (9.0%) | 665 (24.7%) | |
| 80–89 | 275 (1.9%) | 161 (6.0%) | |
| ≥90 | 12 (0.1%) | 5 (0.2%) | |
| Gender, n (%) | |||
| Male | 6444 (44.9%) | 758 (28.1%) | <0.001 |
| Female | 7901 (55.1%) | 1935 (71.9%) | |
| Height, cm | 162.4 (± 9.1) | 157.3 (± 9.3) | <0.001 |
| Weight, kg | 62.5 (± 11.5) | 59.0 (± 10.3) | <0.001 |
| BMI, kg/m2 | 23.6 (± 3.4) | 23.8 (± 3.3) | 0.002 |
| Obesity, n (%) * | |||
| Underweight (<18.5) | 683 (4.8%) | 106 (4.0%) | 0.001 |
| Normal (18.5–24.9) | 9080 (64.1%) | 1644 (61.6%) | |
| Obese (>25) | 4403 (31.1%) | 918 (34.4%) | |
| Smoking status, n (%) | |||
| Non/Ex-smoker | 11,018 (76.9%) | 2304 (85.7%) | <0.001 |
| Current smoker | 3318 (23.1%) | 274 (14.3%) | |
| Alcohol consumption, n (%) | |||
| None | 6453 (45.0%) | 1688 (62.7%) | <0.001 |
| ≥1 drink/month | 7892 (55.0%) | 1005 (37.3%) | |
| Occupation, n (%) | |||
| Unemployed (student, housewife, etc.) | 5791 (40.4%) | 1375 (51.1%) | <0.001 |
| Office work | 2891 (20.2%) | 187 (6.9%) | |
| Sales and services | 1893 (13.2%) | 221 (8.2%) | |
| Agriculture, forestry and fishery | 1102 (7.7%) | 524 (19.5%) | |
| Machine fitting and simple labor | 2668 (18.6%) | 386 (14.3%) | |
| Household income, n (%) † | |||
| Low | 2572 (18.4%) | 976 (36.9%) | <0.001 |
| Low-moderate | 3510 (25.1%) | 645 (24.4%) | |
| Moderate-high | 3881 (27.8%) | 554 (20.9%) | |
| High | 4008 (28.7%) | 471 (17.8%) | |
| Education level, n (%) ‡ | |||
| ≤6 years | 3462 (24.1%) | 1503 (55.8%) | <0.001 |
| 7–9 years | 1594 (11.1%) | 316 (11.7%) | |
| 10–12 years | 5289 (36.9%) | 563 (20.9%) | |
| ≥13 years | 4000 (27.9%) | 311 (11.5%) | |
| Physical activity, n (%) § | |||
| Walk | 6570 (46.0%) | 1263 (47.1%) | 0.32 |
| Middle PA | 1903 (13.3%) | 514 (19.1%) | <0.001 |
| High PA | 2276 (15.9%) | 408 (15.2%) | 0.34 |
| Depressive symptom, n (%) || | 1987 (13.9%) | 698 (25.9%) | <0.001 |
| Comorbidities, n (%) | |||
| Hypertension | 2591 (18.1%) | 879 (32.6%) | <0.001 |
| Dyslipidemia | 968 (6.7%) | 305 (11.3%) | <0.001 |
| Stroke | 261 (1.8%) | 134 (5.0%) | <0.001 |
| Ischemic heart disease | 258 (1.8%) | 133 (4.9%) | <0.001 |
| Knee osteoarthritis | 2119 (14.8%) | 1052 (39.1%) | <0.001 |
| Asthma | 512 (3.6%) | 215 (8.0%) | <0.001 |
| COPD | 114 (0.8%) | 57 (2.1%) | <0.001 |
| Diabetes | 1004 (7.0%) | 310 (11.5%) | <0.001 |
| Chronic kidney disease | 48 (0.3%) | 17 (0.6%) | 0.022 |
| Liver cirrhosis | 23 (0.2%) | 10 (0.4%) | 0.022 |
| Cancer ¶ | 356 (2.5%) | 145 (5.4%) | <0.001 |
| Variables | Coefficient | Odds Radio | 95% CI | p-Value | |
|---|---|---|---|---|---|
| Age group | |||||
| 10–19 | reference | ||||
| 20–29 | 0.8090 | 2.246 | 0.810 | 6.224 | 0.120 |
| 30–39 | 0.9342 | 2.545 | 0.926 | 6.996 | 0.070 |
| 40–49 | 0.9534 | 2.595 | 0.945 | 7.122 | 0.064 |
| 50–59 | 1.1288 | 3.092 | 1.125 | 8.501 | 0.029 |
| 60–69 | 1.5562 | 4.741 | 1.722 | 13.049 | 0.003 |
| 70–79 | 1.8467 | 6.339 | 2.297 | 17.494 | <0.001 |
| 80–89 | 1.9834 | 7.268 | 2.580 | 20.473 | <0.001 |
| ≥90 | 1.2191 | 3.384 | 0.625 | 18.334 | 0.157 |
| Gender | |||||
| Male | reference | ||||
| Female | 0.6023 | 1.826 | 1.623 | 2.055 | <0.001 |
| Occupation | |||||
| Unemployed (Student, housewife, etc.) | reference | ||||
| Office work | −0.2717 | 0.762 | 0.620 | 0.937 | 0.010 |
| Sales and services | −0.1310 | 0.877 | 0.730 | 1.054 | 0.161 |
| Agriculture, forestry and fishery | 0.5694 | 1.767 | 1.516 | 2.060 | <0.001 |
| Machine fitting and simple labor | 0.0195 | 1.002 | 0.859 | 1.169 | 0.980 |
| Education level * | |||||
| ≤6 years | reference | ||||
| 7–9 years | −0.1874 | 0.829 | 0.700 | 0.981 | 0.029 |
| 10–12 years | −0.3344 | 0.716 | 0.607 | 0.844 | <0.001 |
| ≥13 years | −0.4863 | 0.615 | 0.499 | 0.757 | <0.001 |
| Middle PA † | 0.4069 | 1.502 | 1.315 | 1.716 | <0.001 |
| Depressive symptom ‡ | 0.4907 | 1.633 | 1.448 | 1.843 | <0.001 |
| Comorbidities | |||||
| Stroke | 0.4657 | 1.593 | 1.223 | 2.075 | 0.001 |
| Ischemic heart disease | 0.4271 | 1.533 | 1.184 | 1.984 | 0.001 |
| Knee osteoarthritis | 0.5326 | 1.703 | 1.514 | 1.916 | <0.001 |
| Asthma | 0.2921 | 1.339 | 1.090 | 1.646 | 0.005 |
| COPD | 0.6031 | 1.828 | 1.228 | 2.720 | 0.003 |
| Cancer § | 0.3648 | 1.440 | 1.133 | 1.831 | 0.003 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.G.; Park, S.-M.; Kim, H.-J.; Yeom, J.S. Development and Validation of a Risk-Prediction Nomogram for Chronic Low Back Pain Using a National Health Examination Survey: A Cross-Sectional Study. Healthcare 2023, 11, 468. https://doi.org/10.3390/healthcare11040468
Kim JG, Park S-M, Kim H-J, Yeom JS. Development and Validation of a Risk-Prediction Nomogram for Chronic Low Back Pain Using a National Health Examination Survey: A Cross-Sectional Study. Healthcare. 2023; 11(4):468. https://doi.org/10.3390/healthcare11040468
Chicago/Turabian StyleKim, Jung Guel, Sang-Min Park, Ho-Joong Kim, and Jin S. Yeom. 2023. "Development and Validation of a Risk-Prediction Nomogram for Chronic Low Back Pain Using a National Health Examination Survey: A Cross-Sectional Study" Healthcare 11, no. 4: 468. https://doi.org/10.3390/healthcare11040468
APA StyleKim, J. G., Park, S.-M., Kim, H.-J., & Yeom, J. S. (2023). Development and Validation of a Risk-Prediction Nomogram for Chronic Low Back Pain Using a National Health Examination Survey: A Cross-Sectional Study. Healthcare, 11(4), 468. https://doi.org/10.3390/healthcare11040468








