Abstract
Lung cancer is the most common cause of mortality from malignant tumors worldwide. The five-year survival rate for people with advanced stages varies considerably, from 35.4% to 6.9%. The angiogenic potential of bcl2 is not well known, nor is the way in which tumor cells with excessive bcl2 expression affect VEGF production. Hypothetically, given that tumor growth, progression and metastasis are dependent on angiogenesis, the antiapoptotic effect is expected to form a link between these two molecules. The aim of this study was to evaluate the relationship between bcl-2 and VEGF expression, clinicopathological features and survival in 216 patients with advanced NSCLC. Archival tumor tissues were examined by immunohistochemistry for the expression of bcl-2 and VEGF. Immunoreactivity for bcl-2 was observed in 41.4% of NSCLCs, 51% of squamous and 34.8% of adenocarcinomas-expressed Bcl-2. There was an inverse correlation of mononuclear stromal reaction and bcl-2 expression in adenocarcinoma (p < 0.0005). A total of 71.8% NSCLCs were VEGF positive, 56% of squamous and 82.2% of adenocarcinomas. High level of VEGF expression was significantly associated with histology type (p = 0.043), low histology grade (p = 0.014), clinical stage IV (p = 0.018), smoking history (p = 0.008) and EGFR mutations (p = 0.026). There was an inverse correlation in the expression of Bcl-2 and VEGF in NSCLC patients (p = 0.039, r = −0.163). Two-year survival of patients with unresectable NSCLC was 39.3%, and 50% of patients were alive at 17 months. Our results demonstrated no difference in survival for patients in advanced NSCLC grouped by bcl-2 and VEGF status. Additionally, we observed an inverse correlation in the expression of Bcl-2 and VEGF in NSCLC and mononuclear reaction and bcl-2 expression in adenocarcinomas.
1. Introduction
Lung cancer is the most common cause of morbidity and mortality from malignant tumors worldwide. Five-year survival rate for non-small cell lung cancer is approximately 26.3%. The five-year survival rate for people with more advanced stages of the disease varies considerably, from 35.4% in locally advanced to 6.9% in metastatic lung cancer, which depends not only on the stage, but also on the biological characteristics of the tumor [1]. The fundamental assumption of the modern age of lung cancer research is that diagnosis, prediction of prognosis and prediction of patient therapy can be improved by combining standard clinical parameters (performance status, tumor size, status of lymph nodes and distant metastases, differentiation, etc.), with genetic or biochemical properties of the tumor.
The best-studied markers, which today represent the standard in the diagnosis of LC, are TTF-1 and p63, with high specificity and sensitivity in differentiating squamous from primary and secondary adenocarcinomas [2,3].
The research results show, besides diagnostic, prognostic significance as well; p63 is a favorable prognostic factor in patients with squamous cell carcinoma [4], overexpression of TTF-1 prolongs the overall survival of adenocarcinoma patients both in the early and advanced stages of the disease [5], while Multivariate analysis by Svarton M and associates defines these immunohistochemical markers as the only significant parameters for progression-free survival and overall survival rates in patients with NSCLC treated with erlotinib [6].
The identification of new molecular markers, which could predict the response of the tumor to the applied treatment, can enable the optimization of the treatment for each patient.
Many genes and proteins involved in the regulation of the cell cycle, the process of angiogenesis and apoptosis have been defined as markers that have a significant role in the therapeutic response and clinical outcome in NSCLC patients [7,8,9]. Angiogenesis plays a pivotal role in tumor growth and metastatic spread, as such was validated as an independent prognostic factor [10].
One of the most important and strongest stimulators of tumor angiogenesis is VEGF. In the process of competition between proangiogenic and antiangiogenic factors, an angiogenic trigger occurs, which results in an increase in VEGF production. This complex signaling pathway allows VEGF to exert a number of effects in neoangiogenesis. Although VEGF expression is characteristic mainly of endothelial cells, high expression has been found in various tumor types including lung tumor cells.
This increased expression of VEGF in tumor tissue is the result of many factors, the most important of which is hypoxia, which stabilizes and increases the expression of the transcription factor HIF-1α (Hypoxia-inducible factor-1α), which stimulates the transcription of VEGF, which is secreted, diffuses through the tissue, reaches the endothelial cells and binds to specific receptors on their surface. Some studies show that genetic polymorphism of VEGF correlates with sensitivity, prognosis and therapeutic response of NSCLC patients [11,12].
Apoptosis is an important mechanism for maintaining the homeostasis of the organism. Bcl-2 (B-cell lymphoma 2) is the first discovered oncogene. It was initially discovered in B-cell lymphomas where in 85% of cases it is expressed as a result of translocation of the 14th and 18th chromosomes. This protein is a member of a gene family that also includes proapoptotic genes, and their mutual relationship determines whether proapoptotic or antiapoptotic signals will prevail in the cell [13,14].
Overexpression of the bcl-2 gene was also observed in certain solid tumors such as neoplasms of the colon (90%), gastrointestinal tract (60%), prostate carcinoma (30%), non-small cell lung carcinoma (20%) and melanoma [15,16]. In these tumors, the expression of Bcl-2 is a good prognostic indicator, which seems like a paradox considering that its main function is the inhibition of apoptosis [17,18]. On the other hand, Bcl-2 expression is associated with tumor progression, including the occurrence of liver metastases in colorectal carcinoma and lymphovascular invasion in triple-negative breast carcinoma [19,20,21,22].
The angiogenic potential of bcl2 is not well known, nor is the way in which tumor cells with excessive bcl2 expression affect VEGF production. Hypothetically, given that tumor growth, progression and metastasis are dependent on angiogenesis, the antiapoptotic effect is expected to form a link between these two molecules.
For this reason, the goal of our study is examined the expression of VEGF and Bcl-2 in unresectable non-small cell lung cancer, the association of the expression with the pathohistological characteristics of the tumor as well as the correlation with the clinical parameters of the examined patients.
2. Materials and Methods
This clinical-experimental, non-interventional study was conducted in the Center for Oncology and Radiology, the Service for Pathological-Anatomical Diagnostics and the Pulmonary Clinic of the University Clinical Center Kragujevac, in the period from 2017 to 2020.
2.1. Study Population
The study population included 216 patients with locally advanced and metastatic non-small cell lung cancer who were diagnosed and treated at the Kragujevac University Clinical Center in the period from 2016 to 2018. Patients with non-small cell squamous and adenocarcinoma of the lung who were classified into unresectable IIIa, IIIb and IV clinical stage based on clinical stage were included in the research. Staging was completed according to the AJCC (American Joint Committee on Cancer) and UICC (The Union for International Cancer Control) criteria, and the histological classification and grading of tumors according to WHO (World Health Organization) recommendations [23,24]. Patient survival was monitored for 24 months in day hospitals, at regular outpatient check-ups and by telephone contact.
To participate in the study patients were required to have the following criteria: at least 18 years of age, normal hepatic, renal and hematological function and an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1. Before entering the study, patients underwent a medical history evaluation and physical examination. Patients did not receive either chemotherapy or radiotherapy. Tumor measurements of lesions were assessed by imaging techniques such as computed tomography (CT) of the chest and abdomen, magnetic resonance imaging (MRI) of the brain. Tumor response was assessed according to the Response Evaluation Criteria in Solid Tumors guidelines Radiological assessments were performed by CT scans of the chest and abdomen after every two cycles of chemotherapy. Written informed consent was obtained from each patient prior to the start of the study.
The exclusion criteria were as follows: the existence of malignancy in other locations, histologically proven microcellular lung cancer, resectable NSCLC (I, II and resectable IIIa clinical stage), the patient’s general condition (ECOG performance status 3–4) and the decision of the Lung Oncology Council on treatment of patients using symptomatic therapy or only palliative radiation therapy due to comorbidities that exclude the use of chemotherapy. The confounding variables are the gender and age of the respondents, professional occupation, physical activity and data related to personal and family history.
2.2. Method
Tissue samples obtained by bronchoscopy and video-assisted thoracoscopic surgery were used in the research. Standard, histomorphological H&E method and immunohistochemistry were used as methods. Personal and demographic data of patients (gender, age, occupation, habits, comorbidities, family history, etc.), results of radiological diagnostics, data on applied treatment protocols as well as results of EGFR analysis obtained by PCR method in local reference laboratories were taken from the History of Diseases.
2.2.1. H&E Method
On routine, H&E-stained preparations of tumor samples, classic parameters of NSLC were determined by microscopic analysis: histological type, histological and nuclear grade, mitotic index, degree of necrosis and stromal-mononuclear reactions.
2.2.2. Immunohistochemical Method
The 3-micron-thick tissue sections, pre-fixed for 24 h in 10% neutral buffered formalin and embedded in paraffin blocks, were mounted on highly adherent slides, deparaffinized and rehydrated. After epitope release and endogenous peroxidase blocking, the tissue preparations were incubated with primary mouse monoclonal antibodies VEGF (clone VG1; dilution 1:100) and Bcl-2 (clone 100/D5, dilution 1:50), after washing with the secondary antibody, at room temperature according to the manufacturer’s recommendations (ThermoFisher Scientific, Waltham, MA, USA). The reaction was visualized with 3-diaminobenzidine tetrachloride (DAB), counterstained with Mayer’s hematoxylin, and final mounting and coverslipping with Canada balsam. The quality of the immunohistochemical reaction was monitored by simultaneous testing of internal and external, negative and positive tissue controls. The prepared immunohistochemical preparations were analyzed under a light microscope (Axioskop 40, Carl Zeiss, Oberkochen, Germany), and representative fields were photographed with a digital camera (AxioCam ICc1, Carl Zeiss, Oberkochen, Germany). All immunohistochemical stainings were performed with external control of the quality and specificity of staining, using positive and negative controls according to the propositions of NordiQC (Nordic Immunohistochemical Quality Control).
2.3. Immunohistochemical Detection of VEGF and Bcl-2 in NSCLC
Immunohistochemical analysis was performed independently by two researchers, without familiarization with the clinical data of the studied population. In the case of preparations with different obtained values, the final result was reached by consensus. Cytoplasmic expression of VEGFa was determined by a semiquantitative method, as a product of the percentage of positive tumor cells and the intensity of the reaction, according to the recommendations of Klein et al. [25]. Percentual expression, i.e., the number of VEGF positive per 100 counted tumor cells, was classified into four categories: 0—absence of immunoreactivity, 1 <30%, 2 31–60% and 3 >61% immunoreactivity, while the staining intensity was graded as follows: 0—no staining, 1—weak; 2—mild and 3—strong staining. By multiplying these values, VEGF expression in all NSLC samples was scored from 1 to 9. Specifically defined, the cutoff point to distinguish low from high VEGF expression was 25% of positive carcinoma cells [26].
Bcl-2 expression was determined as a percentage of positive tumor cells, not taking into account the intensity of the reaction. Sections were considered positive for Bcl-2 when ≥10% of tumor cells were stained in the cytoplasm [27].
Tumor proliferation index was determined as the number of nuclei expressing Ki-67 per 100 counted tumor cells, i.e., it is expressed as a percentage. Based on the obtained values, all NSLC were classified into two groups: those with low proliferative capacity, in which Ki-67 was less than 30%, and the group of NSLC with high Ki-67 index (greater than 30%).
2.4. Statistical Analysis
Complete statistical analysis of the data will be performed in the statistical computer program, PASW Statistics, version 26. All continuous variables will be presented as the median. Given the normality of the distribution, differences in the mean values of continuous variables were tested using the Mann-Whitney and Kruscal-Wallis tests for independent samples. Correlation between variables will be examined using Spearman’s correlation. Differences in survival were tested using the Kaplan-Mayaer curve and the Log-rank test. All analyzes will be evaluated at a statistical significance level of p ≤ 0.0524.
3. Results
3.1. Clinical Pathological Characteristics
There were 151 males and 65 females, with an average age of 64 years (range 36–80). The main patient characteristics are shown in Table 1.

Table 1.
Baseline Characteristics of the Study Population of Advance NSCLC Patients.
3.2. Association between the IHC Expression of Bcl-2 and Clinicopathological Features
Immunoreactivity for bcl-2 was observed in 41.4% of NSCLCs. Fifty-one percent of squamous cell carcinomas (SCCs) and 34.8% of adenocarcinomas (ACs) expressed Bcl-2. Immunostaining was localised predominantly in cytoplasm. High Bcl-2 expression was significantly associated with histology grade and stromal-mononuclear reaction (Figure 1). No statistically significant difference was identified between Bcl-2 expression and other clinical parameters, including gender, smoking status, TNM stage or lymph node metastasis (results not shown).
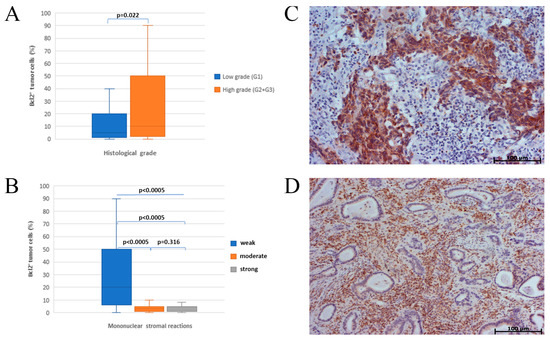
Figure 1.
Association of Bcl-2 expression with histological grade and mononuclear stromal reaction; (A) influence of histological grade on bcl-2 expression; histomorphological presentation of positive correlation of bcl-2 expression and histological grade (C); inverse correlation of mononuclear stromal reaction and bcl-2 expression in adenocarcinoma (B); histomorphological representation of the intensity of mononuclear stromal reaction and bcl-2 expression in adenocarcinoma (D).
3.3. Association between the IHC Expression of VEGF and Clinicopathologial Features
A total of 71.8% patients had positive immunohistochemical staining for VEGF. Fifty-six percent of squamous cell carcinomas (SCCs) and 82.2% of adenocarcinomas (ACs) expressed VEGF. High level of VEGF expression was significantly associated with histology type, histology grade, lymph node status, clinical stage and smoking history (Figure 2).
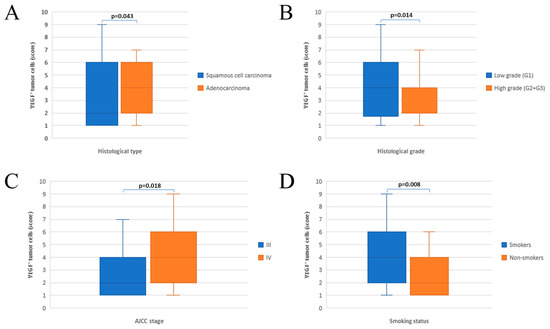
Figure 2.
Assotiation between the IHC expression of VEGF and clinicopathiological features (A) histological type; (B) histological grade; (C) stage disease; (D) smoking status.
3.4. Relationship between the Expression of VEGFa and Bcl-2
There was an inverse correlation (Figure 3) in the expression of Bcl-2 and VEGF (p = 0.039) in NSCLC patients.
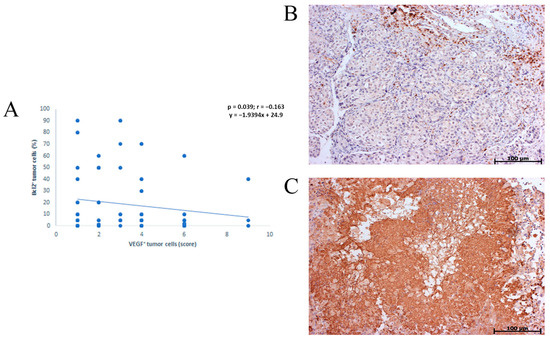
Figure 3.
Graphic and histomorphological presentation of inverse Correlation between Bcl-2 and VEGF expression in NSCLC. (A) graphic of inverse corelation; (B,C) histomorphological presentation.
3.5. Association of the Proliferation Index with the Expression of VEGFa and Bcl-2
A high Ki-67 proliferative index was observed in 79 patients NSCLC (71.8%) and was more common in adenocarcinomas than in squamous cell carcinomas. We found positive correlation between VEGF and the Ki-67 proliferation index in NSCLC patients. No correlation has been seen between Bcl-2 and the Ki-67 proliferation index in NSCLC patients, but there was a negative correlation in adenocarcinoma subgroups (Figure 4).
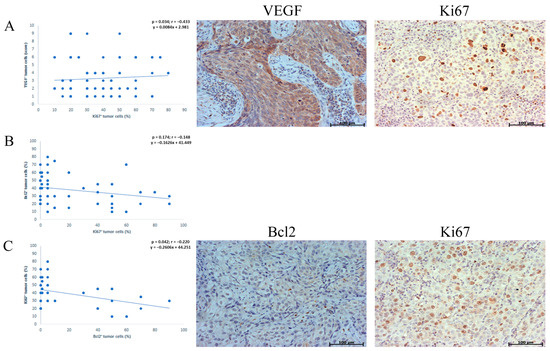
Figure 4.
Association of the proliferation index with the expression of VEGFa and Bcl-2. (A) graphic and histomorphological presentation of positive correlation between VEGF and the Ki-67 proliferation index in NSCLC patients; (B) relationship between Ki-67 proliferative index and bcl-2 expression in NSCLC patients (C) graphic and histomorphological presentation of inverse correlation between Bcl-2 and the Ki-67 proliferation index in adenocarcinomas.
3.6. Association of EGFR Status with Expression of VEGFa and Bcl-2
Wild-type EGFR was present in 86.3%, while 13.7% of adenocarcinoma had mutations on exons 19 and 21 (Table 2).

Table 2.
Percentage of adenocarcinoma mutations.
EGFR status significantly depends on the stage of the disease and age; younger patients more often had a mutated status, not related to histological grade and Bcl-2 expression. Mutation carriers are more often male and non-smokers. There is a significant association between EGFR status and VEGFa expression in the analyzed adenocarcinoma samples (Table 3).

Table 3.
Correlation between EGFR and VEGF and Bcl-2 in 102 cases of advanced lung adenocarcinoma.
3.7. Survival
Two-year survival of patients with unresectable NSCLC was 39.3%, and 50% of patients were alive at 17 months. Survival is statistically significantly affected by age and stage of the disease (results not shown), and without significance, survival is associated with the histological type of tumor, Ki-67 tumor proliferative capacity, VEGF and Bcl-2 expression (Figure 5).
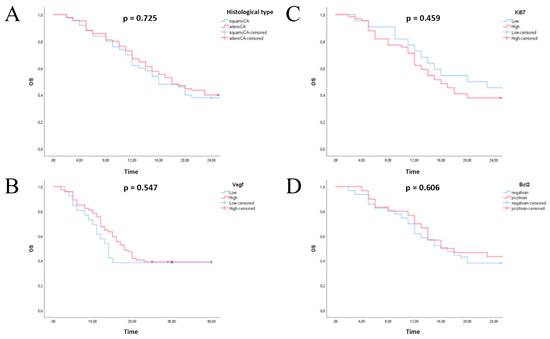
Figure 5.
Kaplan-Meier overall survival analysis of patients with non-small lung cell carcinoma. (A) histology type; (B) expression status of VEGF; (C) expression status of Ki67; (D) expression status of Bcl-2.
4. Discussion
Several experimental studies have shown a connection between bcl2 over expression and increased VEGF production, i.e., the influence of antiapoptotic bcl2 status on growth, progression, metastasis and intensification of angiogenesis [28,29,30]. However, in NSCLC, this relationship is not sufficiently clear, because it has been shown that the expression of bcl2, as a favorable prognostic factor, can be inversely correlated with VEGF [31,32] but also positively correlated with negative prognostic implication [33,34].
In our study, we examined the expression of VEGF and Bcl-2 in the tissue of 216 patients with locally advanced and metastatic NSCLC, association of IHC expression and clinicopathologial features, as well as correlation of IHC expression.
Stefanoup et al., reported that the expression of VEGF was 77.3% in NSCLC [35]. In this study, expression rate of VEGF protein was 71.8%.
The statistical analysis showed that positive expression of VEGF was higher in well differentiated cancer, in adenocarcinoma, lymph node metastasis and clinical stage of IV. The results in the present study is consistent with previous reports [36,37,38].
Usuda et al. showed in their research that VEGF expression is significantly higher in adenocarcinoma compared to squamous cell carcinomas, and that VEGF can be a positive regulator of pericytes and angiogenesis, thus affecting the proliferation of endothelial cells and maturation of blood vessels of tumor, which could result in a favorable outcome in well-differentiated lung cancer [39].
Lymphnodal metastases play an important role in tumor staging, which depends on the therapeutic modality, and as such represent an important prognostic predictor. In addition to being associated with tumor size, histological type and lymph node metastases are also associated with VEGF expression [40]. Liu et al. examined the expression of VEGF-C in NSCLC patients and showed that lymphovascular density is higher in VEGF-C positive tumors, which means that VEGF-C can affect both tumor growth and the occurrence of lymphnodal metastases [41]. The association between VEGF expression and lymphnodal metastases has also been shown in other solid tumors such as esophageal, prostate and stomach cancers [42,43,44].
We found statistically significant association between VEGF expression in current smokers and never smokers. In vitro findings are consistent with a pro-angiogenic effect of nicotine; increased angiogenesis in response to nicotine and the role of nicotine in tumorigenesis has not been demonstrated. There are some evidence indicate that prostacyclin is involved in angiogenesis and it is known that nicotine releases prostacyclin from human vascular endothelial cells. Also, nicotine induces basic fibroblast growth factor and platelet-derived growth factor release in endothelial cells and increases proliferation [45,46]. Heeschen C et al. have shown that nicotine increases endothelial cell number, reduces apoptosis and increases capillary network formation in vitro. The effects of nicotine on vascular structure are mediated by non-neuronal nicotine-sensitive acetylcholine receptors nAChR which have been shown to be present on endothelial cell which is associated with functional changes in tissue blood flow and accelerating tumor growth [47]. Conklin et al. show nicotine and cotinine cause an increase in VEGF expression in endothelial cells, indicating that cotinine may have an even more pronounced effect than nicotine because of the long half-life of cotinine [48]. Some studies suggested that nicotine causes a significant increase in serum VEGF levels [47,49,50,51]. Zhao H et al. showed that a low dose of nicotine promoted VEGF secretion by increasing HIF-1α-mediated VEGF transcription under hypoxic conditions [52].
The results of our study show a significant association between VEGF expression and EGFR (p = 0.026). In preclinical studies, mutations of EGFR correlated with VEGF in lung cancer, as it has been shown that EGFR-mutant NSCLC cells hasten the expression of VEGF more than wild-type NSCLC cells [53]. The reason for this is that EGFR-mutant NSCLC cells constitutively up-regulate HIF-1a in a hypoxia-independent manner and HIF-1a induces VEGF expression [54,55].
Some studies have shown that at the time of detection of resistance to the application of tyrosine kinase inhibitor (TKi), resistant cells had an elevated level of VEGF, thus suggesting the mutual connection of EGFR and VEGF signaling pathways. Based on this assumption, numerous clinical studies have shown benefit from dual EGFR-VEGF signaling inhibition, including longer time to disease progression and resistance to TKi [56,57,58].
In addition, we indicate that VEGF expression was significantly positively correlated with Ki-67 expression. These results indirectly show that high VEGF expression assumes a poorer prognosis of the disease.
Yoshihito Shibata et al., confirmed Bcl-2 expression in 29.1% of NSCLC and 44.4% of squamous cell carcinomas [27]. The results of this and other studies are similar to ours in terms of a higher number of squamous cell Bcl-2 positive tumors compared to the number of Bcl-2 positive NSCLC. Expression of Bcl-2 was related to histology grade and mononuclear stromal reactions (p = 0.022, p < 0.0005). Our results show that of bcl-2 over expression may represent tumor de-differentiation and more aggressive behaviour of NSCL tumors.
Petrisor et al. showed that Bcl-2 expression is lower in poorly differentiated colon cancers compared to low-grade tumors [59]. The assumption is that during tumor progression, Bcl-2 expression decreases due to its inhibitory effect on the progression of the cell cycle, thus leading to a reduction in the inhibition of apoptosis [60]. No survival difference was detected based on Bcl-2 status. Krug et al. also reported no difference in survival for patients in advanced NSCLC grouped by bcl-2 status [61].
The impact of bcl-2 protein expression on prognosis in NSCLC patients shows controversy. The meta-analysis by Zhang et al. shows the association of bcl-2 positivity and LONGER survival, while on the other hand some studies come to the conclusion that bcl-2 expression has no prognostic significance or is even associated with a poor prognostic outcome [62,63].
What could explain this are different antibodies used for immunohistochemical analysis, cut-off values, sample size and tumor heterogeneity. Bcl-2 expression may be more informative if put into context with the expression of other family members with pro-apoptotic functions. Published results suggest that the high expression of a pro-apoptotic Bax protein was associated with poor prognosis in esophageal, squamous cell carcinoma, Bak in bladder cancer and Mcl-1 protein defined as unfavorable prognostic marker for lung cancer [64,65,66,67].
According to Gurova et al., loss of apoptosis through p53 inactivation leads to genetic instability and tumor progression, whereas loss of apoptosis through bcl-2 overexpression creates genetically stable tumors that escape the selective pressure to inactivate p53 and are therefore less prone to progression, leading to a better prognostic outcome [68]. Haldar et al. show negative regulation of Bcl-2 expression by some p53 mutants that can result in a decrease in expression of Bcl-2 in advanced tumors with mutated p53 [69].
An inverse correlation was found between expression of Bcl-2 and VEGF. Michael I. Koukourakis et al. and Fontanini et al. show inverse relationship between vascular grade and bcl-2 expression but in operable NSCLC [70,71]. It has been shown that p53 oncoprotein can regulate neovascularisation through induction of thrombospondin-1, an inhibitor of angiogenesis. On the other hand, bcl-2 may inhibit p53 function that can be associated with increased tumoral angiogenesis. Therefore, bcl-2 may regulate angiogenesis either by stimulating the release of inhibitors of angiogenesis or by suppression of angiogenic factors via a pathway distinct from that of p53.
5. Conclusions
In conclusion, the present study demonstrated no difference in survival for patients in advanced NSCLC grouped by bcl-2 and VEGF status. Additionally, we observed a inversely correlation in the expression of Bcl-2 and VEGF in NSCLC patients and inverse correlation of mononuclear stromal reaction and bcl-2 expression in adenocarcinomas.
Author Contributions
Conceptualization, M.M., M.P. and S.M.; methodology, M.M.; software, M.M. and M.Z.M.; validation, M.M., S.M., M.Z.M. and M.P.; formal analysis, M.P., M.Z.M. and A.D.; investigation, M.M., R.V., A.I. and D.J.; resources, S.M.; data curation, S.M., A.I. and R.V.; writing—original draft preparation, M.M.; writing—review and editing M.M., S.M. and T.N.; visualization, M.M.; supervision, S.M. and M.P.; project administration, M.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of University Clinical Center Kragujevac, Serbia, decision number: 01-12751/2016.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
This study was supported by the Scientific Committee of Faculty of Medical Sciences, University of Kragujevac “Expression of tumor markers as an indicator of chemosensitivity and prognosis in locally advanced non-small cell lung cancer” (JP No. 10-16).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Howlader, N.N.A.; Krapcho, M.; Miller, D.; Brest, A.; Yu, M.; Ruhl, J.; Tatalovich, Z.; Mariotto, A.; Lewis, D.R.; Chen, H.S.; et al. (Eds.) SEER Cancer Statistics Review, 1975–2017; National Cancer Institute: Bethesda, MD, USA, 2020. Available online: https://seer.cancer.gov/csr/1975_2017/ (accessed on 1 April 2020).
- Gurguş, D.; Grigoraş, M.L.; Motoc, A.G.M.; Zamfir, C.L.; Cornianu, M.; Faur, C.I.; Pop, D.L.; Folescu, R. Clinical relevance and accuracy of p63 and TTF-1 for better approach of small cell lung carcinoma versus poorly differentiated nonkeratinizing squamous cell carcinoma. Rom. J. Morphol Embryol. 2019, 60, 139–143. [Google Scholar] [PubMed]
- Moldvay, J.; Jackel, M.; Bogos, K.; Soltész, I.; Agócs, L.; Kovács, G.; Schaff, Z. The role of TTF-1 in differentiating primary and metastatic lung adenocarcinomas. Pathol. Oncol. Res. 2004, 10, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Fan, M.; Dai, L.; Kang, X.; Liu, Y.; Sun, Y.; Xiong, H.; Liang, Z.; Yan, W.; Chen, K. Expression of p63 and CK5/6 in early-stage lung squamous cell carcinoma is not only an early diagnostic indicator but also correlates with a good prognosis. Thorac. Cancer 2015, 6, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Kim, H.S.; Kim, B.J.; Han, B.; Choi, D.R.; Kwon, J.H. Prognostic Impact of TTF-1 Expression in Non-Squamous Non-Small-Cell Lung Cancer: A Meta-Analysis. J. Cancer 2018, 9, 4279–4286. [Google Scholar] [CrossRef] [PubMed]
- Svaton, M.; Fiala, O.; Krakorova, G.; Blazek, J.; Hurdalkova, K.; Barinova, M.; Mukensnabl, P.; Pesek, M. Thyroid transcription factor 1 and p63 expression is associated with survival outcome in patients with non-small cell lung cancer treated with erlotinib. Oncol. Lett. 2020, 20, 1376–1382. [Google Scholar]
- Zhu, L.; Yu, H.; Liu, S.Y.; Xiao, X.S.; Dong, W.H.; Chen, Y.N.; Xu, W.; Zhu, T. Prognostic value of tissue inhibitor of metalloproteinase-2 expression in patients with non-small cell lung cancer: A systematic review and meta-analysis. PLoS ONE 2015, 10, e0124230. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.N.; Wang, D.S.; Chen, Y.Q.; Zhao, C.L.; Gong, B.L.; Jiang, A.B.; Jia, W.; Hu, F.D. Expression of survivin and patients survival in non-small cell lung cancer: A meta-analysis of the published studies. Mol. Biol. Rep. 2013, 40, 917–924. [Google Scholar] [CrossRef]
- Farhat, F.S.; Tfayli, A.; Fakhruddin, N.; Mahfouz, R.; Otrock, Z.K.; Alameddine, R.S.; Awada, A.H.; Shamseddine, A. Expression, prognostic and predictive impact of VEGF and bFGF in non-small cell lung cancer. Crit. Rev. Oncol. Hematol. 2012, 84, 149–160. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef]
- Guo, X.; Chen, Y.; Xu, Z.; Xu, Z.; Qian, Y.; Yu, X. Prognostic significance of VEGF-C expression in correlation with COX-2, lymphatic microvessel density, and clinicopathologic characteristics in human non-small cell lung cancer. Acta Biochim. Biophys. Sin. 2009, 41, 217–222. [Google Scholar] [CrossRef]
- Bonnesen, B.; Pappot, H.; Holmstav, J.; Skov, B.G. Vascular endothelial growth factor A and vascular endothelial growth factor receptor 2 expression in non-small cell lung cancer patients: Relation to prognosis. Lung Cancer 2009, 66, 314–318. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, A.B.; Gottlieb, R.A. Bcl-2 family members and apoptosis, taken to heart. Am. J. Physiol. Cell Physiol. 2007, 292, C45–C51. [Google Scholar] [CrossRef] [PubMed]
- White, E. Mechanisms of apoptosis regulation by viral oncogenes in infection and tumorigenesis. Cell Death Differ. 2006, 13, 1371–1377. [Google Scholar] [CrossRef]
- Reed, J.C.; Miyashita, T.; Takayama, S.; Wang, H.G.; Sato, T.; Krajewski, S.; Aimé-Sempé, C.; Bodrug, S.; Kitada, S.; Hanada, M. BCL-2 family proteins: Regulators of cell death involved in the pathogenesis of cancer and resistance to therapy. J. Cell. Biochem. 1996, 60, 23–32. [Google Scholar] [CrossRef]
- Hartman, M.L.; Czyz, M. Anti-apoptotic proteins on guard of melanoma cell survival. Cancer Lett. 2013, 331, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Vairo, G.; Innes, K.M.; Adams, J.M. Bcl-2 has a cell cycle inhibitory function separable from its enhancement of cell survival. Oncogene 1996, 13, 1511–1519. [Google Scholar] [PubMed]
- Pietenpol, J.A.; Papadopoulos, N.; Markowitz, S.; Willson, J.K.; Kinzler, K.W.; Vogelstein, B. Paradoxical inhibition of solid tumor cell growth by bcl-2. Cancer Res. 1994, 54, 3714–3717. [Google Scholar]
- Oliver, L.; Cordel, S.; Barbieux, I.; LeCabellec, M.T.; Meflah, K.; Grégoire, M.; Vallette, F.M. Resistance to apoptosis is increased during metastatic dissemination of colon cancer. Clin. Exp. Metastasis 2002, 19, 175–180. [Google Scholar] [CrossRef]
- Melucci, E.; Cosimelli, M.; Carpanese, L.; Pizzi, G.; Izzo, F.; Fiore, F.; Golfieri, R.; Giampalma, E.; Sperduti, I.; Ercolani, C.; et al. Decrease of survivin, p53 and Bcl-2 expression in chemorefractory colorectal liver metastases may be predictive of radiosensivity radiosensivity after radioembolization with yttrium-90 resin microspheres. J. Exp. Clin. Cancer Res. 2013, 32, 13. [Google Scholar] [CrossRef]
- Neri, A.; Marrelli, D.; Roviello, F.; DeMarco, G.; Mariani, F.; DeStefano, A.; Megha, T.; Caruso, S.; Corso, G.; Cioppa, T.; et al. Bcl-2 expression correlates with lymphovascular invasion and long-term prognosis in breast cancer. Breast Cancer Res. Treat. 2006, 99, 77–83. [Google Scholar] [CrossRef]
- Tawfik, K.; Kimler, B.F.; Davis, M.K.; Fan, F.; Tawfik, O. Prognostic significance of Bcl-2 in invasive mammary carcinomas: A comparative clinicopathologic study between “triple-negative” and non-”triple-negative” tumors. Hum. Pathol. 2012, 43, 23–30. [Google Scholar] [CrossRef] [PubMed]
- WHO. Classification of Tumours Editorial Board. In Thoracic Tumours, 5th ed.; Lyon, F., Ed.; International Agency for Research on Cancer: Lyon, France, 2021; Available online: https://tumourclassification.iarc.who.int/ (accessed on 1 May 2021).
- Mahul, B.; Amin, S.B.E.; Frederick, L.; Greene, D.R.; Byrd, R.K.; Brookland, M.K.W.; Jeffrey, E.G.; Carolyn, C.; Kenneth, R.H.; Daniel, C.; et al. AJCC Cancer Staging Manual, 8th ed.; Springer: Berlin/Heidelberg, Germany, 2017; pp. 819–831. [Google Scholar]
- Klein, M.; Vignaud, J.M.; Hennequin, V.; Toussaint, B.; Bresler, L.; Plénat, F.; Leclère, J.; Duprez, A.; Weryha, G. Increased expression of the vascular endothelial growth factor is a pejorative prognosis marker in papillary thyroid carcinoma. J. Clin. Endocrinol. Metab. 2001, 86, 656–658. [Google Scholar] [CrossRef] [PubMed]
- Yano, T.; Tanikawa, S.; Fujie, T.; Masutani, M.; Horie, T. Vascular endothelial growth factor expression and neovascularisation in non-small cell lung cancer. Eur. J. Cancer 2000, 36, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Shibata, Y.; Hidaka, S.; Tagawa, Y.; Nagayasu, T. Bcl-2 protein expression correlates with better prognosis in patients with advanced non-small cell lung cancer. Anticancer Res. 2004, 24, 1925–1928. [Google Scholar] [PubMed]
- Beierle, E.A.; Strande, L.F.; Chen, M.K. VEGF upregulates Bcl-2 expression and is associated with decreased apoptosis in neuroblastoma cells. J. Pediatr. Surg. 2002, 37, 467–471. [Google Scholar] [CrossRef]
- Fernandez, A.; Udagawa, T.; Schwesinger, C.; Beecken, W.; Achilles-Gerte, E.; McDonnell, T.; D’Amato, R. Angiogenic potential of prostate carcinoma cells overexpressing bcl-2. J. Natl. Cancer Inst. 2001, 93, 208–213. [Google Scholar] [CrossRef]
- Biroccio, A.; Candiloro, A.; Mottolese, M.; Sapora, O.; Albini, A.; Zupi, G.; Del Bufalo, D. Bcl-2 overexpression and hypoxia synergistically act to modulate vascular endothelial growth factor. FASEB J. 2000, 14, 652–660. [Google Scholar] [CrossRef]
- Bairey, O.; Zimra, Y.; Shaklai, M.; Rabizadeh, E. Bcl-2 expression correlates positively with serum basic fibroblast growth factor (bFGF) and negatively with cellular vascular endothelial growth factor (VEGF) in patients with chronic lymphocytic leukaemia. Br. J. Haematol. 2001, 113, 400–406. [Google Scholar] [CrossRef]
- Jinyoung, Y.J.H.J.; Hyun, J.C.; Seok, J.K.; Chang, S.K. Expression of bcl-2, p53 and VEGF in Non-Small Cell Lung Carcinomas: Their Relation with the Microvascular Density and Prognosis. Korean J. Pathol. 2005, 39, 74–80. [Google Scholar]
- Ahmed, M.B.; Nabih, E.S.; Louka, M.L.; Abdel Motaleb, F.I.; El Sayed, M.A.; Elwakiel, H.M. Evaluation of nestin in lung adenocarcinoma: Relation to VEGF and Bcl-2. Biomarkers 2014, 19, 29–33. [Google Scholar] [CrossRef]
- Tian, J.; Hu, L.; Li, X.; Geng, J.; Dai, M.; Bai, X. MicroRNA-130b promotes lung cancer progression via PPARγ/VEGF-A/BCL-2-mediated suppression of apoptosis. J. Exp. Clin. Cancer Res. 2016, 35, 105. [Google Scholar] [CrossRef] [PubMed]
- Stefanou, D.; Goussia, A.C.; Arkoumani, E.; Agnantis, N.J. Expression of vascular endothelial growth factor and the adhesion molecule E-cadherin in non-small cell lung cancer. Anticancer Res. 2003, 23, 4715–4720. [Google Scholar] [PubMed]
- Lin, Q.; Guo, L.; Lin, G.; Chen, Z.; Chen, T.; Lin, J.; Zhang, B.; Gu, X. Clinical and prognostic significance of OPN and VEGF expression in patients with non-small-cell lung cancer. Cancer Epidemiol. 2015, 39, 539–544. [Google Scholar] [CrossRef] [PubMed]
- Ding, M.; Liu, L.; Hu, C.; Liu, Y.; Qiao, Y.; Jiang, X. Expression of VEGFR2 and NRP-1 in non-small cell lung cancer and their clinical significance. Chin. J. Cancer Res. 2014, 26, 669–677. [Google Scholar]
- Wei, D.; Xin, Y.; Rong, Y.; Hao, Y. Correlation between the Expression of VEGF and Ki67 and Lymph Node Metastasis in Non-small-Cell Lung Cancer: A Systematic Review and Meta-Analysis. Evid. Based Complement. Alternat. Med. 2022, 2022, 9693746. [Google Scholar] [CrossRef]
- Usuda, K.; Iwai, S.; Funasaki, A.; Sekimura, A.; Motono, N.; Ueda, Y.; Shimazaki, M.; Uramoto, H. Expression and Prognostic Impact of VEGF, CD31 and αSMA in Resected Primary Lung Cancers. Anticancer Res. 2018, 38, 4057–4063. [Google Scholar] [CrossRef]
- Dai, M.; Hua, C.; Wang, M.; Gao, L.; Jiang, L.; Liu, Y. Targeting regulation of VEGF by BPTF in Non-Small Cell Lung Cancer and its potential clinical significance. Eur. J. Med. Res. 2022, 27, 299. [Google Scholar] [CrossRef]
- Liu, J.; Liu, C.; Qiu, L.; Li, J.; Zhang, P.; Sun, Y. Overexpression of both platelet-derived growth factor-BB and vascular endothelial growth factor-C and its association with lymphangiogenesis in primary human non-small cell lung cancer. Diagn Pathol 2014, 9, 128. [Google Scholar] [CrossRef]
- Yang, Z.; Wang, Y.G.; Su, K. VEGF-C and VEGF-D expression and its correlation with lymph node metastasis in esophageal squamous cell cancer tissue. Asian Pac. J. Cancer Prev. 2015, 16, 271–274. [Google Scholar] [CrossRef]
- Kostis, G.; Ioannis, L.; Helen, K.; Helen, P. The expression of vascular endothelial growth factor-C correlates with lymphatic microvessel density and lymph node metastasis in prostate carcinoma: An immunohistochemical study. Urol. Ann. 2014, 6, 224–230. [Google Scholar] [CrossRef]
- Kruszyna, Ł.; Murawa, D.; Jagodziński, P.P.; Oszkinis, G.; Krasiński, Z. The Expression and Prognostic Significance of VEGF and CXCR4 in Gastric Cancer: Correlation with Angiogenesis, Lymphangiogenesis and Progression. Curr. Issues Mol. Biol. 2022, 44, 3075–3088. [Google Scholar] [CrossRef] [PubMed]
- Cucina, A.; Sapienza, P.; Borrelli, V.; Corvino, V.; Foresi, G.; Randone, B.; Cavallaro, A.; Santoro-D’Angelo, L. Nicotine reorganizes cytoskeleton of vascular endothelial cell through platelet-derived growth factor BB. J. Surg. Res. 2000, 92, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Cucina, A.; Corvino, V.; Sapienza, P.; Borrelli, V.; Lucarelli, M.; Scarpa, S.; Strom, R.; Santoro-D’Angelo, L.; Cavallaro, A. Nicotine regulates basic fibroblastic growth factor and transforming growth factor beta1 production in endothelial cells. Biochem. Biophys. Res. Commun. 1999, 257, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Heeschen, C.; Jang, J.J.; Weis, M.; Pathak, A.; Kaji, S.; Hu, R.S.; Tsao, P.S.; Johnson, F.L.; Cooke, J.P. Nicotine stimulates angiogenesis and promotes tumor growth and atherosclerosis. Nat. Med. 2001, 7, 833–839. [Google Scholar] [CrossRef]
- Conklin, B.S.; Zhao, W.; Zhong, D.S.; Chen, C. Nicotine and cotinine up-regulate vascular endothelial growth factor expression in endothelial cells. Am. J. Pathol. 2002, 160, 413–418. [Google Scholar] [CrossRef]
- Wasada, T.; Kawahara, R.; Katsumori, K.; Naruse, M.; Omori, Y. Plasma concentration of immunoreactive vascular endothelial growth factor and its relation to smoking. Metabolism 1998, 47, 27–30. [Google Scholar] [CrossRef]
- Takigawa, N.; Segawa, Y.; Fujimoto, N.; Hotta, K.; Eguchi, K. Elevated vascular endothelial growth factor levels in sera of patients with lung cancer. Anticancer Res. 1998, 18, 1251–1254. [Google Scholar]
- Ugur, M.G.; Kutlu, R.; Kilinc, I. The effects of smoking on vascular endothelial growth factor and inflammation markers: A case-control study. Clin. Respir. J. 2018, 12, 1912–1918. [Google Scholar] [CrossRef]
- Zhao, H.; Wu, L.; Wang, Y.; Zhou, J.; Li, R.; Zhou, J.; Wang, Z.; Xu, C. Nicotine promotes vascular endothelial growth factor secretion by human trophoblast cells under hypoxic conditions and improves the proliferation and tube formation capacity of human umbilical endothelial cells. Reprod. Biomed. Online 2017, 34, 406–413. [Google Scholar] [CrossRef]
- Naumov, G.N.; Nilsson, M.B.; Cascone, T.; Briggs, A.; Straume, O.; Akslen, L.A.; Lifshits, E.; Byers, L.A.; Xu, L.; Wu, H.K.; et al. Combined vascular endothelial growth factor receptor and epidermal growth factor receptor (EGFR) blockade inhibits tumor growth in xenograft models of EGFR inhibitor resistance. Clin. Cancer Res. 2009, 15, 3484–3494. [Google Scholar] [CrossRef]
- Xu, L.; Nilsson, M.B.; Saintigny, P.; Cascone, T.; Herynk, M.H.; Du, Z.; Nikolinakos, P.G.; Yang, Y.; Prudkin, L.; Liu, D.; et al. Epidermal growth factor receptor regulates MET levels and invasiveness through hypoxia-inducible factor-1alpha in non-small cell lung cancer cells. Oncogene 2010, 29, 2616–2627. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.S.; Park, S.H. Immunohistochemical Expression and Prognostic Value of VEGF, HIF-1alpha, EGFR in Non-Small Cell Lung Cancer. Tuberc. Respir. Dis. 2010, 68, 22–28. [Google Scholar] [CrossRef]
- Le, X.; Nilsson, M.; Goldman, J.; Reck, M.; Nakagawa, K.; Kato, T.; Ares, L.P.; Frimodt-Moller, B.; Wolff, K.; Visseren-Grul, C.; et al. Dual EGFR-VEGF Pathway Inhibition: A Promising Strategy for Patients With EGFR-Mutant NSCLC. J. Thorac. Oncol. 2021, 16, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Johnson, B.E.; Kabbinavar, F.; Fehrenbacher, L.; Hainsworth, J.; Kasubhai, S.; Kressel, B.; Lin, C.Y.; Marsland, T.; Patel, T.; Polikoff, J.; et al. ATLAS: Randomized, double-blind, placebo-controlled, phase IIIB trial comparing bevacizumab therapy with or without erlotinib, after completion of chemotherapy, with bevacizumab for first-line treatment of advanced non-small-cell lung cancer. J. Clin. Oncol. 2013, 31, 3926–3934. [Google Scholar] [CrossRef] [PubMed]
- Stinchcombe, T.E.; Jänne, P.A.; Wang, X.; Bertino, E.M.; Weiss, J.; Bazhenova, L.; Gu, L.; Lau, C.; Paweletz, C.; Jaslowski, A.; et al. Effect of Erlotinib Plus Bevacizumab vs Erlotinib Alone on Progression-Free Survival in Patients with Advanced EGFR-Mutant Non-Small Cell Lung Cancer: A Phase 2 Randomized Clinical Trial. JAMA Oncol. 2019, 5, 1448–1455. [Google Scholar] [CrossRef]
- Petrişor, O.; Giuşcă, S.E.; Sajin, M.; Dobrescu, G.; Căruntu, I.D. Ki-67, p53 and bcl-2 analysis in colonic versus rectal adenocarcinoma. Rom. J. Morphol. Embryol. 2008, 49, 163–171. [Google Scholar]
- Kirkin, V.; Joos, S.; Zörnig, M. The role of Bcl-2 family members in tumorigenesis. Biochim. Biophys. Acta 2004, 1644, 229–249. [Google Scholar] [CrossRef]
- Krug, L.M.; Miller, V.A.; Filippa, D.A.; Venkatraman, E.; Ng, K.K.; Kris, M.G. Bcl-2 and bax expression in advanced non-small cell lung cancer: Lack of correlation with chemotherapy response or survival in patients treated with docetaxel plus vinorelbine. Lung Cancer 2003, 39, 139–143. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, S.; Wang, L.; Wang, R.; Chen, S.; Pan, B.; Sun, Y.; Chen, H. Prognostic value of Bcl-2 expression in patients with non-small-cell lung cancer: A meta-analysis and systemic review. OncoTargets Ther. 2015, 8, 3361–3369. [Google Scholar] [CrossRef]
- Lee, H.W.; Choi, Y.W.; Han, J.H.; Kim, J.H.; Jung, J.H.; Jeong, S.H.; Kang, S.Y.; Choi, J.H.; Oh, Y.T.; Park, K.J.; et al. Expression of excision repair cross-complementation group 1 protein predicts poor outcome in advanced non-small cell lung cancer patients treated with platinum-based doublet chemotherapy. Lung Cancer 2009, 65, 377–382. [Google Scholar] [CrossRef]
- Haitel, A.; Posch, B.; El-Baz, M.; Mokhtar, A.A.; Susani, M.; Ghoneim, M.A.; Marberger, M. Bilharzial related, organ confined, muscle invasive bladder cancer: Prognostic value of apoptosis markers, proliferation markers, p53, E-cadherin, epidermal growth factor receptor and c-erbB-2. J. Urol. 2001, 165, 1481–1487. [Google Scholar] [CrossRef] [PubMed]
- Kurabayashi, A.; Furihata, M.; Matsumoto, M.; Ohtsuki, Y.; Sasaguri, S.; Ogoshi, S. Expression of Bax and apoptosis-related proteins in human esophageal squamous cell carcinoma including dysplasia. Mod. Pathol. 2001, 14, 741–747. [Google Scholar] [CrossRef] [PubMed]
- Takayama, T.; Nagao, M.; Sawada, H.; Yamada, Y.; Emoto, K.; Fujimoto, H.; Ueno, M.; Hirao, S.; Nakajima, Y. Bcl-X expression in esophageal squamous cell carcinoma: Association with tumor progression and prognosis. J. Surg. Oncol. 2001, 78, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Eerola, A.-K.; Ruokolainen, H.; Soini, Y.; Raunio, H.; Pääkkö, P. Accelerated apoptosis and low Bcl-2 expression associated with neuroendocrine differentiation predict shortened survival in operated large cell carcinoma of the lung. Pathol. Oncol. Res. 1999, 5, 179–186. [Google Scholar] [CrossRef]
- Gurova, K.V.; Gudkov, A.V. Paradoxical role of apoptosis in tumor progression. J. Cell. Biochem. 2003, 88, 128–137. [Google Scholar] [CrossRef]
- Haldar, S.; Negrini, M.; Monne, M.; Sabbioni, S.; Croce, C.M. Down-regulation of bcl-2 by p53 in breast cancer cells. Cancer Res. 1994, 54, 2095–2097. [Google Scholar]
- Koukourakis, M.I.; Giatromanolaki, A.; O’Byrne, K.J.; Whitehouse, R.M.; Talbot, D.C.; Gatter, K.C.; Harris, A.L. Potential role of bcl-2 as a suppressor of tumour angiogenesis in non-small-cell lung cancer. Int. J. Cancer 1997, 74, 565–570. [Google Scholar] [CrossRef]
- Fontanini, G.; Boldrini, L.; Vignati, S.; Chinè, S.; Basolo, F.; Silvestri, V.; Lucchi, M.; Mussi, A.; Angeletti, C.A.; Bevilacqua, G. Bcl-2 and p53 regulate vascular endothelial growth factor (VEGF)-mediated angiogenesis in non-small cell lung carcinoma. Eur. J. Cancer 1998, 34, 718–723. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).