Awareness and Sources of Knowledge about Obstructive Sleep Apnea: A Cross Sectional Survey Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Survey Development
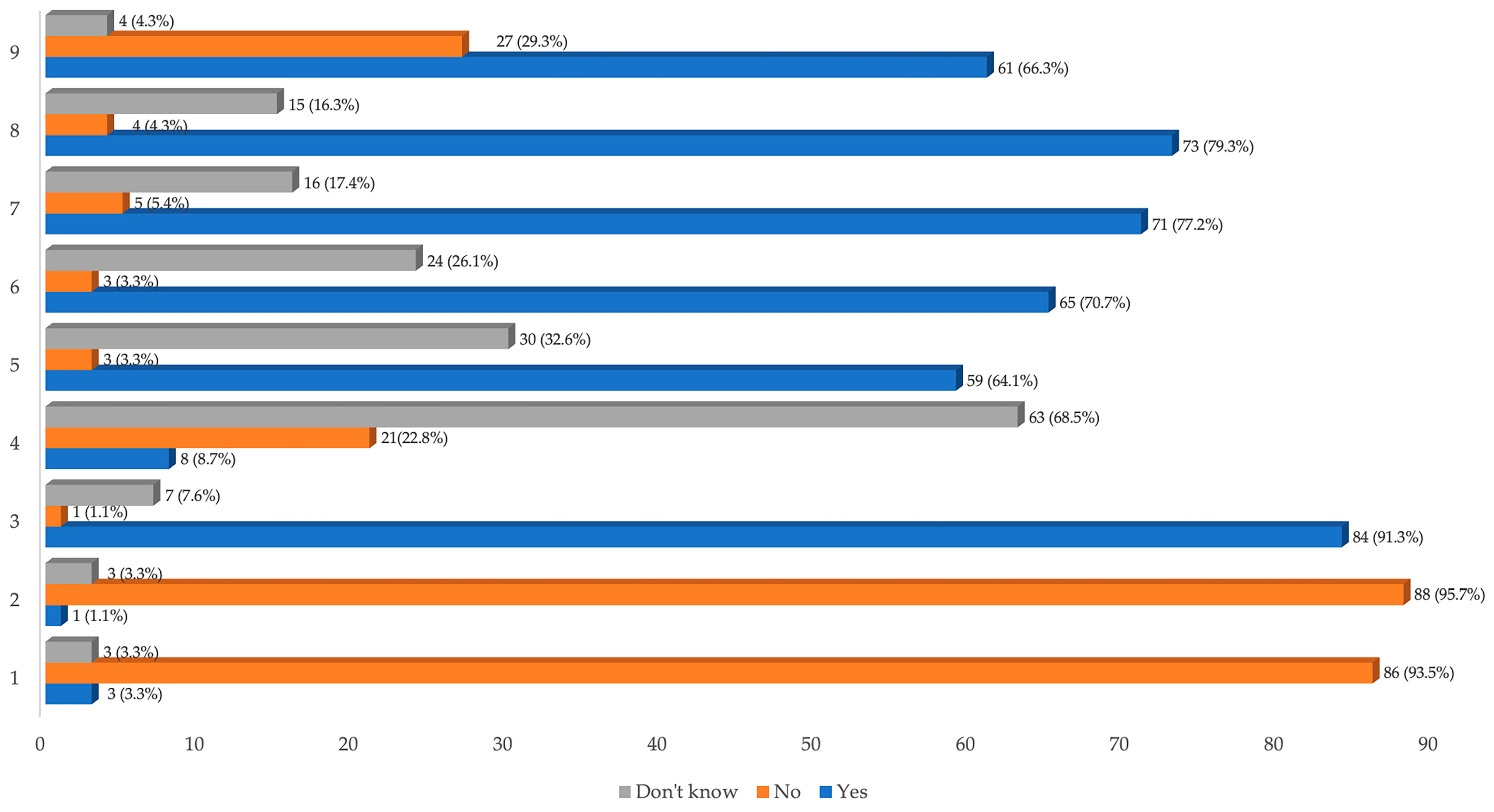
- Do you think snoring is a normal condition?
- Are interruptions in breathing (apneas) during sleep, a normal condition?
- Can polysomnography be a valid tool for the diagnosis of OSA?
- Do you think that obstructive sleep apnea syndrome can lead to diabetes?
- Do you think that obstructive sleep apnea syndrome can lead to arterial hypertension?
- Do you think that obstructive sleep apnea syndrome can lead to myocardial infarction?
- Can obstructive sleep apnea lead to an increased risk of road accidents?
- To date, are there treatments that resolve the obstructive sleep apnea syndrome?
- Have you ever heard of CPAP?
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Benjafield, A.V.; Ayas, N.T.; Eastwood, P.R.; Heinzer, R.; Ip, M.S.M.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pépin, J.L.D.; et al. Estimation of the Global Prevalence and Burden of Obstructive Sleep Apnoea: A Literature-Based Analysis. Lancet Respir. Med. 2019, 7, 687–698. [Google Scholar] [CrossRef]
- Sateia, M.J. International Classification of Sleep Disorders-Third Edition Highlights and Modifications. Chest 2014, 146, 1387–1394. [Google Scholar] [CrossRef] [PubMed]
- Eckert, D.J.; Malhotra, A.; Jordan, A.S. Mechanisms of Apnea. Prog. Cardiovasc. Dis. 2009, 51, 313–323. [Google Scholar] [CrossRef] [PubMed]
- Eckert, D.J. Phenotypic Approaches to Obstructive Sleep Apnoea—New Pathways for Targeted Therapy. Sleep Med. Rev. 2018, 37, 45–59. [Google Scholar] [CrossRef]
- Turnbull, C.D.; Stradling, J.R. Endotyping, Phenotyping and Personalised Therapy in Obstructive Sleep Apnoea: Are We There Yet? Thorax 2023, 78, 726–732. [Google Scholar] [CrossRef] [PubMed]
- Bosi, M.; Incerti Parenti, S.; Sanna, A.; Plazzi, G.; De Vito, A.; Alessandri-Bonetti, G. Non-Continuous Positive Airway Pressure Treatment Options in Obstructive Sleep Apnoea: A Pathophysiological Perspective. Sleep Med. Rev. 2021, 60, 101521. [Google Scholar] [CrossRef]
- Incerti Parenti, S.; Bortolotti, F.; Alessandri-Bonetti, G. Oral Appliances for Obstructive Sleep Apnea. J. World Fed. Orthod. 2019, 8, 3–8. [Google Scholar] [CrossRef]
- Sowho, M.; Amatoury, J.; Kirkness, J.P.; Patil, S.P. Sleep and respiratory physiology in adults. Clin. Chest Med. 2014, 35, 469. [Google Scholar] [CrossRef]
- Mezzanotte, W.S.; Tangel, D.J.; White, D.P. Mechanisms of Control of Alae Nasi Muscle Activity. J. Appl. Physiol. 1992, 72, 925–933. [Google Scholar] [CrossRef]
- Fogel, R.B.; Trinder, J.; White, D.P.; Malhotra, A.; Raneri, J.; Schory, K.; Kleverlaan, D.; Pierce, R.J. The Effect of Sleep Onset on Upper Airway Muscle Activity in Patients with Sleep Apnoea versus Controls. J. Physiol. 2005, 564, 549–562. [Google Scholar] [CrossRef]
- Tangel, D.J.; Mezzanotte, W.S.; White, D.P. Influence of Sleep on Tensor Palatini EMG and Upper Airway Resistance in Normal Men. J. Appl. Physiol. 1991, 70, 2574–2581. [Google Scholar] [CrossRef] [PubMed]
- Wiegand, L.; Zwillich, C.W.; Wiegand, D.; White, D.P. Changes in Upper Airway Muscle Activation and Ventilation during Phasic REM Sleep in Normal Men. J. Appl. Physiol. 1991, 71, 488–497. [Google Scholar] [CrossRef] [PubMed]
- Edwards, B.A.; White, D.P. Control of the Pharyngeal Musculature During Wakefulness and Sleep: Implications in Normal Controls and Sleep Apnea. Head Neck 2011, 33, S37. [Google Scholar] [CrossRef]
- Jordan, A.S.; McSharry, D.G.; Malhotra, A. Adult Obstructive Sleep Apnoea. Lancet 2014, 383, 736–747. [Google Scholar] [CrossRef]
- Heinzer, R.; Marti-Soler, H.; Haba-Rubio, J. Prevalence of Sleep Apnoea Syndrome in the Middle to Old Age General Population. Lancet Respir. Med. 2016, 4, e5–e6. [Google Scholar] [CrossRef]
- Lyons, M.M.; Bhatt, N.Y.; Pack, A.I.; Magalang, U.J. Global Burden of Sleep-Disordered Breathing and Its Implications. Respirology 2020, 25, 690–702. [Google Scholar] [CrossRef] [PubMed]
- Kapur, V.K.; Auckley, D.H.; Chowdhuri, S.; Kuhlmann, D.C.; Mehra, R.; Ramar, K.; Harrod, C.G. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2017, 13, 479–504. [Google Scholar] [CrossRef]
- Giles, T.L.; Lasserson, T.J.; Smith, B.J.; White, J.; Wright, J.; Cates, C.J. Continuous Positive Airways Pressure for Obstructive Sleep Apnoea in Adults. Cochrane Database Syst. Rev. 2006, 1, CD001106. [Google Scholar] [CrossRef]
- Mogell, K.; Blumenstock, N.; Mason, E.; Rohatgi, R.; Shah, S.; Schwartz, D. Definition of an Effective Oral Appliance for the Treatment of Obstructive Sleep Apnea and Snoring: An Update for 2019. J. Dent. Sleep Med. 2019, 6. [Google Scholar] [CrossRef]
- Armeni, P.; Borsoi, L.; Costa, F.; Donin, G.; Gupta, A. Cost-of-Illness Study of Obstructive Sleep Apnea Syndrome (OSAS) in Italy; Università Bocconi: Milan, Italy, 2019. [Google Scholar]
- Rapelli, G.; Pietrabissa, G.; Angeli, L.; Manzoni, G.M.; Tovaglieri, I.; Perger, E.; Garbarino, S.; Fanari, P.; Lombardi, C.; Castelnuovo, G. Study Protocol of a Randomized Controlled Trial of Motivational Interviewing-Based Intervention to Improve Adherence to Continuous Positive Airway Pressure in Patients with Obstructive Sleep Apnea Syndrome: The MotivAir Study. Front. Psychol. 2022, 13, 947296. [Google Scholar] [CrossRef]
- Borsoi, L.; Armeni, P.; Donin, G.; Costa, F.; Ferini-Strambi, L. The Invisible Costs of Obstructive Sleep Apnea (OSA): Systematic Review and Cost-of-Illness Analysis. PLoS ONE 2022, 17, e0268677. [Google Scholar] [CrossRef]
- Simmons, M.; Sayre, J.; Schotland, H.M.; Jeffe, D.B. Obstructive Sleep Apnea Knowledge Among Dentists and Physicians. J. Dent. Sleep Med. 2021, 8, 1–12. [Google Scholar] [CrossRef]
- Dillow, K.; Essick, G.; Sanders, A.; Sheats, R.; Brame, J. Patient Response to Sleep Apnea Screening in a Dental Practice. J. Public Health Dent. 2017, 77, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Saglam-Aydinatay, B.; Uysal, S.; Taner, T. Facilitators and Barriers to Referral Compliance among Dental Patients with Increased Risk of Obstructive Sleep Apnea. Acta Odontol. Scand. 2018, 76, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Sia, C.H.; Hong, Y.; Tan, L.W.L.; van Dam, R.M.; Lee, C.H.; Tan, A. Awareness and Knowledge of Obstructive Sleep Apnea among the General Population. Sleep Med. 2017, 36, 10–17. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Sleep Medicine. The International Classification of Sleep Disorders, 3rd ed.; ICSD-3: Diagnostic and Coding Manual; American Academy of Sleep Medicine: Westchester, IL, USA, 2014. [Google Scholar]
- Şentürk, H.; Eryilmaz, M.A.; Vatansev, H.; Pekgör, S. Evaluation of Knowledge Level Related to Obstructive Sleep Apnea Syndrome. Niger. J. Clin. Pract. 2019, 22, 1722–1727. [Google Scholar] [CrossRef]
- Henzell, M.; Knight, A.; Antoun, J.S.; Farella, M. Social Media Use by Orthodontic Patients. N. Z. Dent. J. 2013, 109, 130–133. [Google Scholar]
- Scarpelli, S.; Alfonsi, V.; Mangiaruga, A.; Musetti, A.; Quattropani, M.C.; Lenzo, V.; Freda, M.F.; Lemmo, D.; Vegni, E.; Borghi, L.; et al. Pandemic Nightmares: Effects on Dream Activity of the COVID-19 Lockdown in Italy. J. Sleep Res. 2021, 30, e13300. [Google Scholar] [CrossRef]
- Paiva, T.; Reis, C.; Feliciano, A.; Canas-Simião, H.; Machado, M.A.; Gaspar, T.; Tomé, G.; Branquinho, C.; Silva, M.R.; Ramiro, L.; et al. Sleep and Awakening Quality during COVID-19 Confinement: Complexity and Relevance for Health and Behavior. Int. J. Environ. Res. Public Health 2021, 18, 3506. [Google Scholar] [CrossRef]
- Ruiz-Herrera, N.; Díaz-Román, A.; Guillén-Riquelme, A.; Quevedo-Blasco, R. Sleep Patterns during the COVID-19 Lockdown in Spain. Int. J. Environ. Res. Public Health 2023, 20, 4841. [Google Scholar] [CrossRef]
- Mehrtash, M.; Bakker, J.P.; Ayas, N. Predictors of Continuous Positive Airway Pressure Adherence in Patients with Obstructive Sleep Apnea. Lung 2019, 197, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Bortolotti, F.; Corazza, G.; Bartolucci, M.L.; Incerti Parenti, S.; Paganelli, C.; Alessandri-Bonetti, G. Dropout and Adherence of Obstructive Sleep Apnoea Patients to Mandibular Advancement Device Therapy: A Systematic Review of Randomised Controlled Trials with Meta-Analysis and Meta-Regression. J. Oral Rehabil. 2022, 49, 553–572. [Google Scholar] [CrossRef] [PubMed]
- Fox, S. Health Topics. Pew Internet and American Life Project. 2011. Available online: https://www.pewresearch.org/internet/2011/02/01/health-topics-2/ (accessed on 1 March 2023).
- Fox, S.; Rainie, L. The Online Health Care Revolution: How the Web Helps Americans Take Better Care of Themselves: Pew Charitable Trusts: Washington, DC, USA. 2000. Available online: https://www.pewresearch.org/internet/2000/11/26/the-online-health-care-revolution/ (accessed on 1 March 2023).
- Weedmark, D. Why Is Audiovisual Media Considered a Powerful Tool and Means of Communication? Available online: https://smallbusiness.chron.com/audiovisual-media-considered-powerful-tool-means-communication-33541.html (accessed on 30 September 2023).
- Osman, W.; Mohamed, F.; Elhassan, M.; Shoufan, A. Is YouTube a Reliable Source of Health-Related Information? A Systematic Review. BMC Med. Educ. 2022, 22, 382. [Google Scholar] [CrossRef] [PubMed]
- Incerti Parenti, S.; Gamberini, S.; Fiordelli, A.; Bortolotti, F.; Laffranchi, L.; Alessandri-Bonetti, G. Online Information on Mandibular Advancement Device for the Treatment of Obstructive Sleep Apnea: A Content, Quality and Readability Analysis. J. Oral Rehabil. 2023, 50, 210–216. [Google Scholar] [CrossRef]
- Incerti-Parenti, S.; Bartolucci, M.L.; Biondi, E.; Fiordelli, A.; Paganelli, C.; Alessandri-Bonetti, G. Online Audio-Visual Information on the Treatment of OSA with Mandibular Advancement Devices: Analysis of Quality, Reliability and Contents. Appl. Sci. 2023, 13, 5727. [Google Scholar] [CrossRef]
- Lichtblau, M.; Bratton, D.; Giroud, P.; Weiler, T.; Bloch, K.E.; Brack, T. Risk of Sleepiness-Related Accidents in Switzerland: Results of an Online Sleep Apnea Risk Questionnaire and Awareness Campaigns. Front. Med. 2017, 4, 34. [Google Scholar] [CrossRef]

| Gender | Male | n = 67 | 72.8% |
| Female | n = 25 | 27.2% | |
| Country of Origin | Italy | n = 88 | 95.7% |
| EU Country | n = 3 | 3.3% | |
| Not EU Country | n = 1 | 1.1% | |
| Level of Education | Primary School | n = 1 | 1.1% |
| Middle School Graduation | n = 16 | 17.4% | |
| High School Diploma | n = 38 | 41.3% | |
| University Degree | n = 37 | 40.2% | |
| Occupation | Student | n = 0 | 0 |
| Government Employee | n = 20 | 21.7% | |
| Freelance | n = 15 | 16.3% | |
| Private Employee | n = 18 | 19.6% | |
| Unemployed | n = 0 | 0 | |
| Retired | n = 33 | 35.9% | |
| Other | n = 6 | 6.5% | |
| Marital Status | Single | n = 15 | 16.3% |
| Divorced | n = 8 | 8.7% | |
| Married | n = 60 | 65.2% | |
| Engaged in a stable relationship | n = 9 | 9.8% |
| Score (Number of Correct Answers) | Prevalence % |
|---|---|
| 9 | 0% (n = 0) |
| 8 | 5.43% (n = 5) |
| 7 | 34.78% (n = 32) |
| 6 | 27.17% (n = 25) |
| 5 | 11.96% (n = 11) |
| 4 | 10.87% (n = 10) |
| 3 | 7.61% (n = 7) |
| 2 | 2.17% (n = 2) |
| 1 | 0% (n = 0) |
| 0 | 0% (n = 0) |
| Χ2= | p= | |
| Gender | 0.949 | 0.330 |
| Marital status | 0.174 | 0.677 |
| Source of Knowledge | 1.978 | 0.852 |
| Level of Education | 14.465 | 0.002 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bartolucci, M.L.; Incerti Parenti, S.; Bortolotti, F.; Gorini, T.; Alessandri-Bonetti, G. Awareness and Sources of Knowledge about Obstructive Sleep Apnea: A Cross Sectional Survey Study. Healthcare 2023, 11, 3052. https://doi.org/10.3390/healthcare11233052
Bartolucci ML, Incerti Parenti S, Bortolotti F, Gorini T, Alessandri-Bonetti G. Awareness and Sources of Knowledge about Obstructive Sleep Apnea: A Cross Sectional Survey Study. Healthcare. 2023; 11(23):3052. https://doi.org/10.3390/healthcare11233052
Chicago/Turabian StyleBartolucci, Maria Lavinia, Serena Incerti Parenti, Francesco Bortolotti, Tommaso Gorini, and Giulio Alessandri-Bonetti. 2023. "Awareness and Sources of Knowledge about Obstructive Sleep Apnea: A Cross Sectional Survey Study" Healthcare 11, no. 23: 3052. https://doi.org/10.3390/healthcare11233052
APA StyleBartolucci, M. L., Incerti Parenti, S., Bortolotti, F., Gorini, T., & Alessandri-Bonetti, G. (2023). Awareness and Sources of Knowledge about Obstructive Sleep Apnea: A Cross Sectional Survey Study. Healthcare, 11(23), 3052. https://doi.org/10.3390/healthcare11233052







