One-Stage Tricompartmental Hypoallergenic UKA for Tricompartmental Osteoarthritis: A Case Report
Abstract
1. Introduction
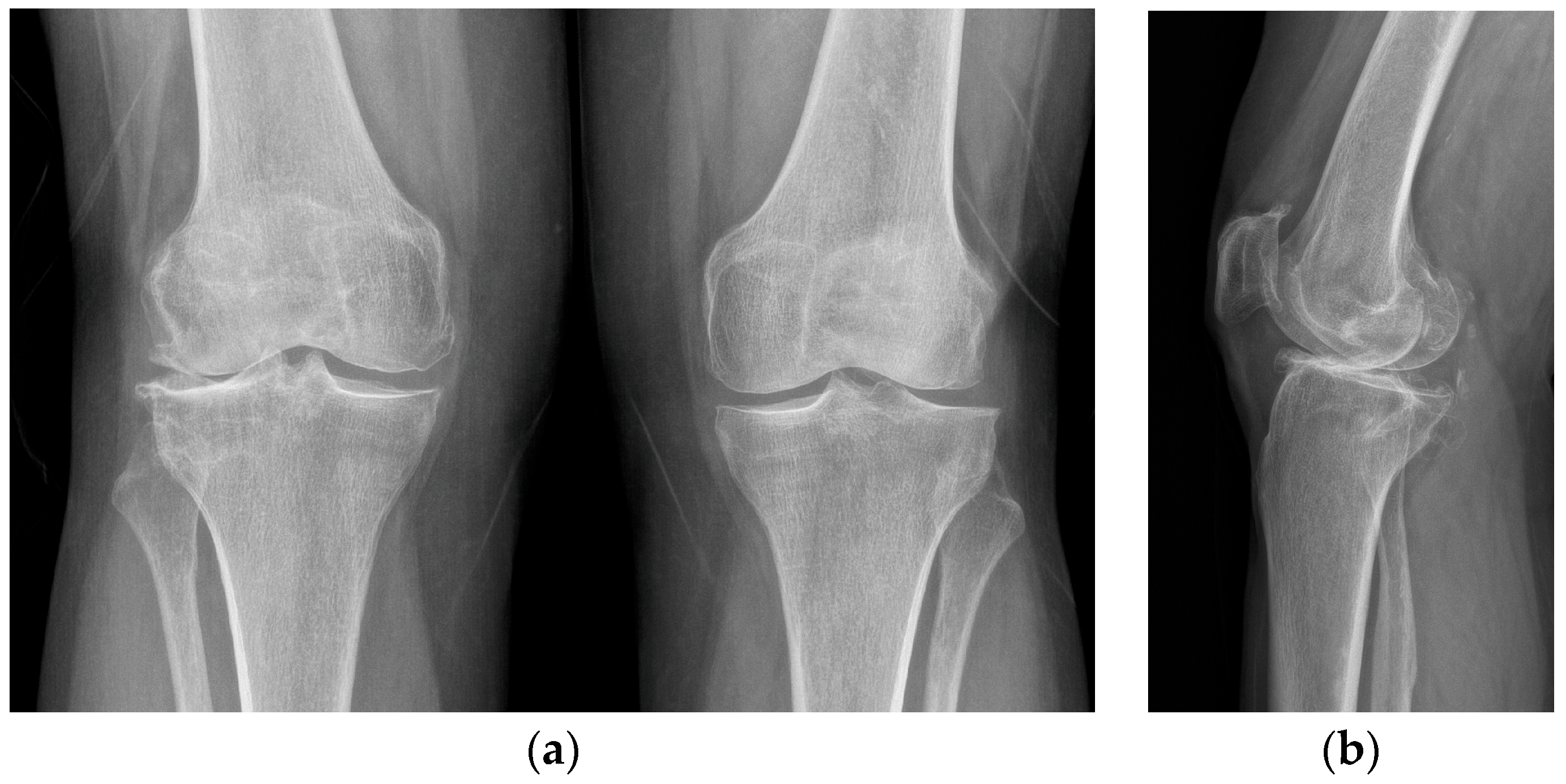
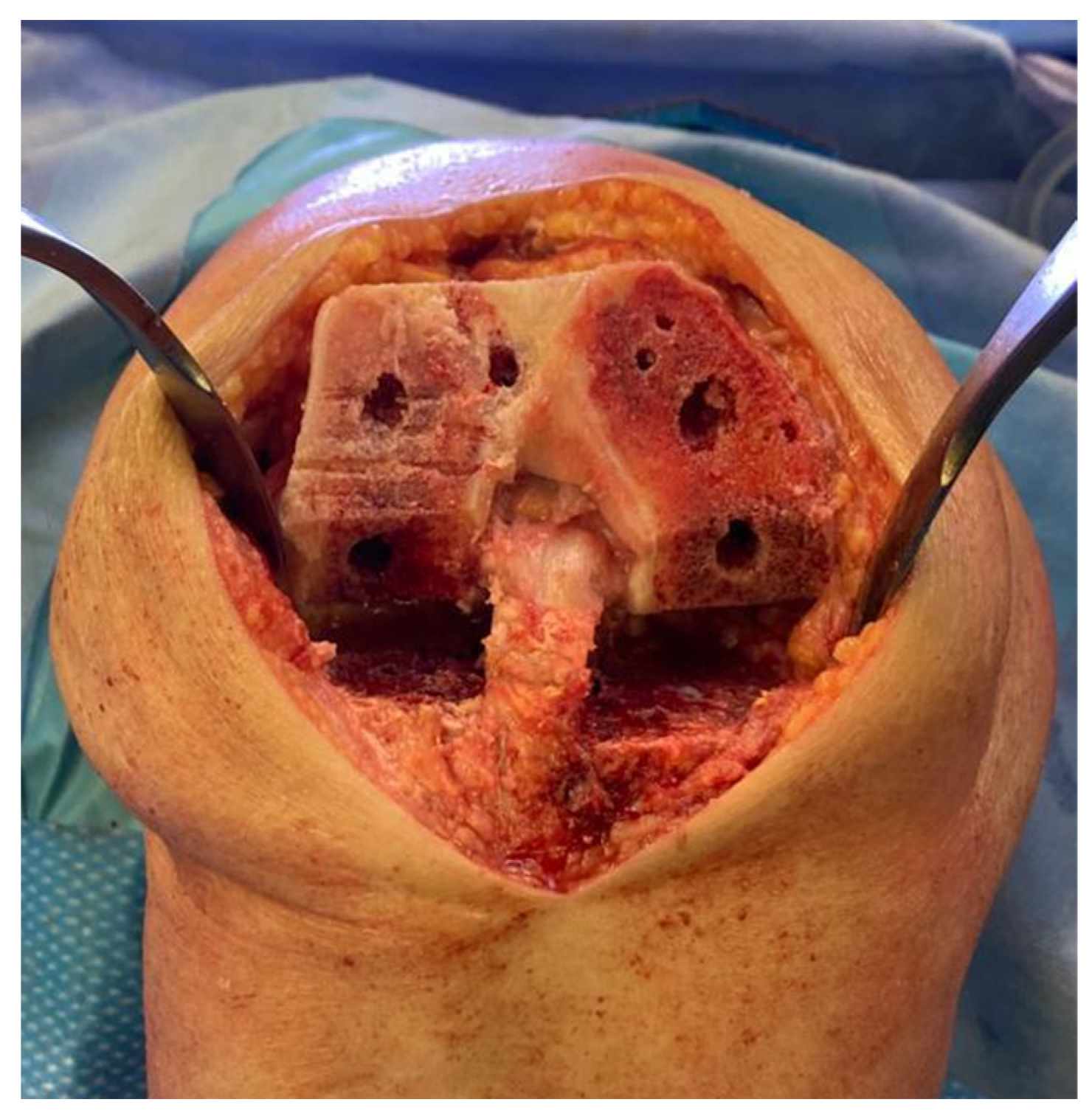
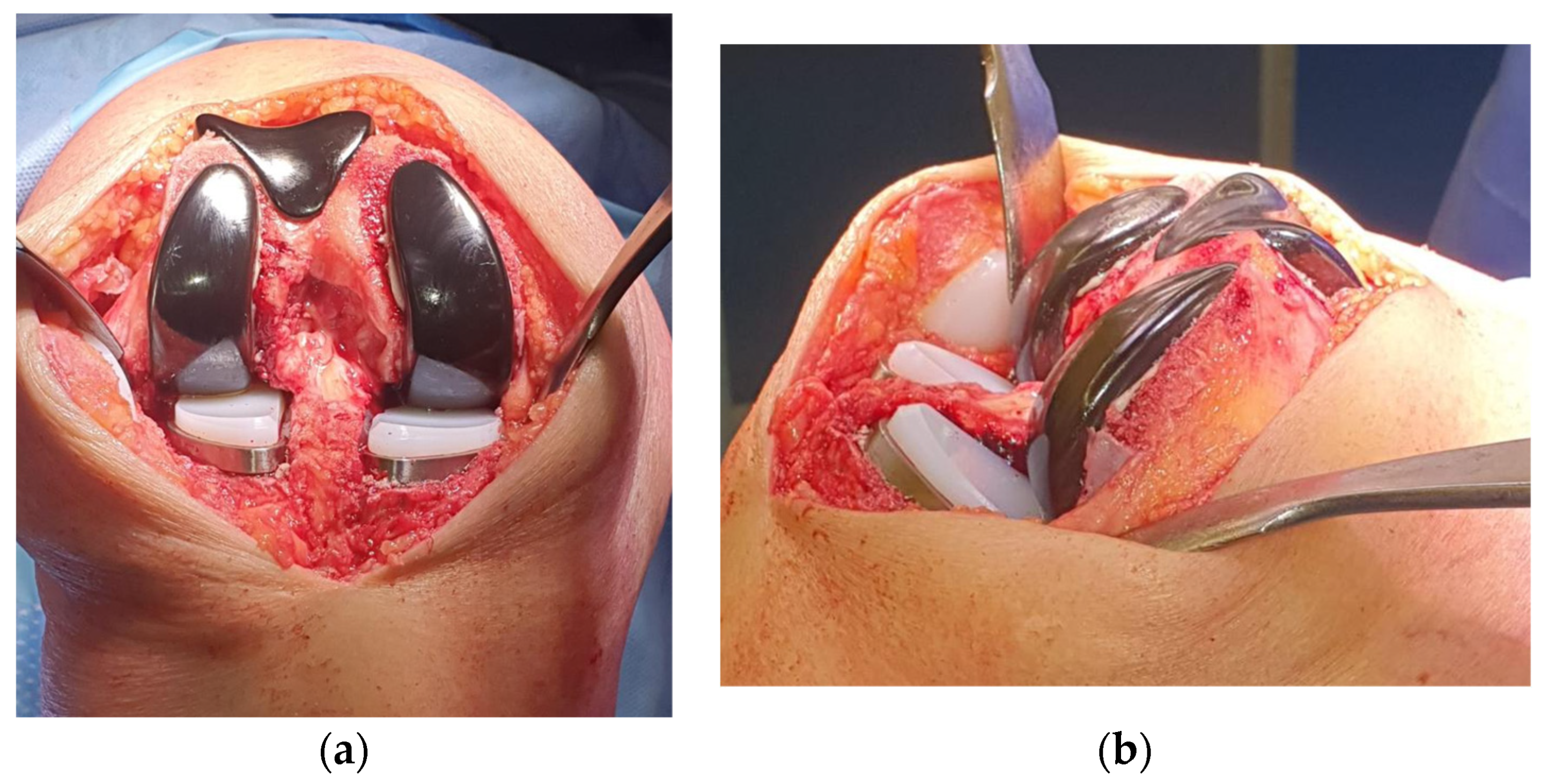
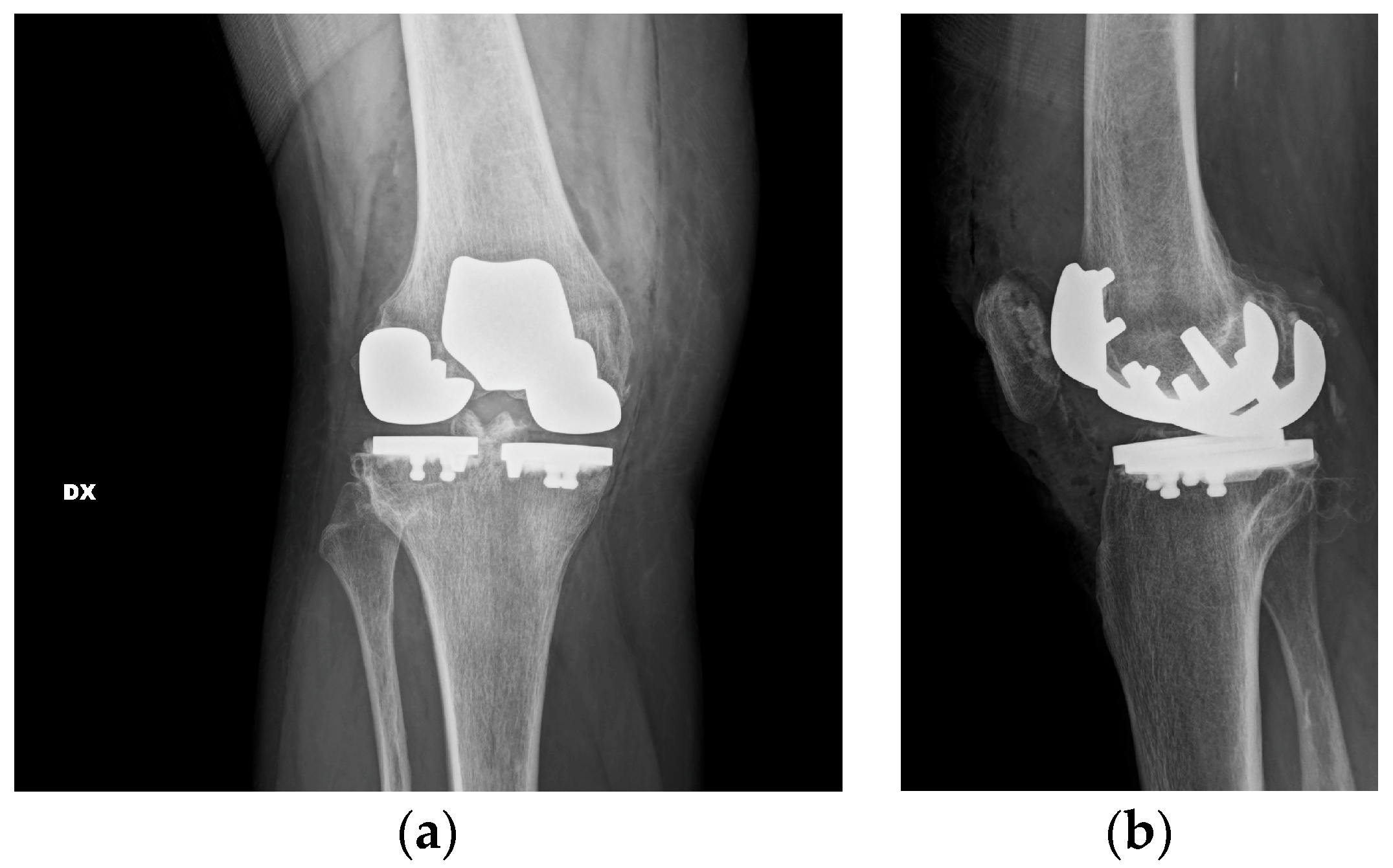
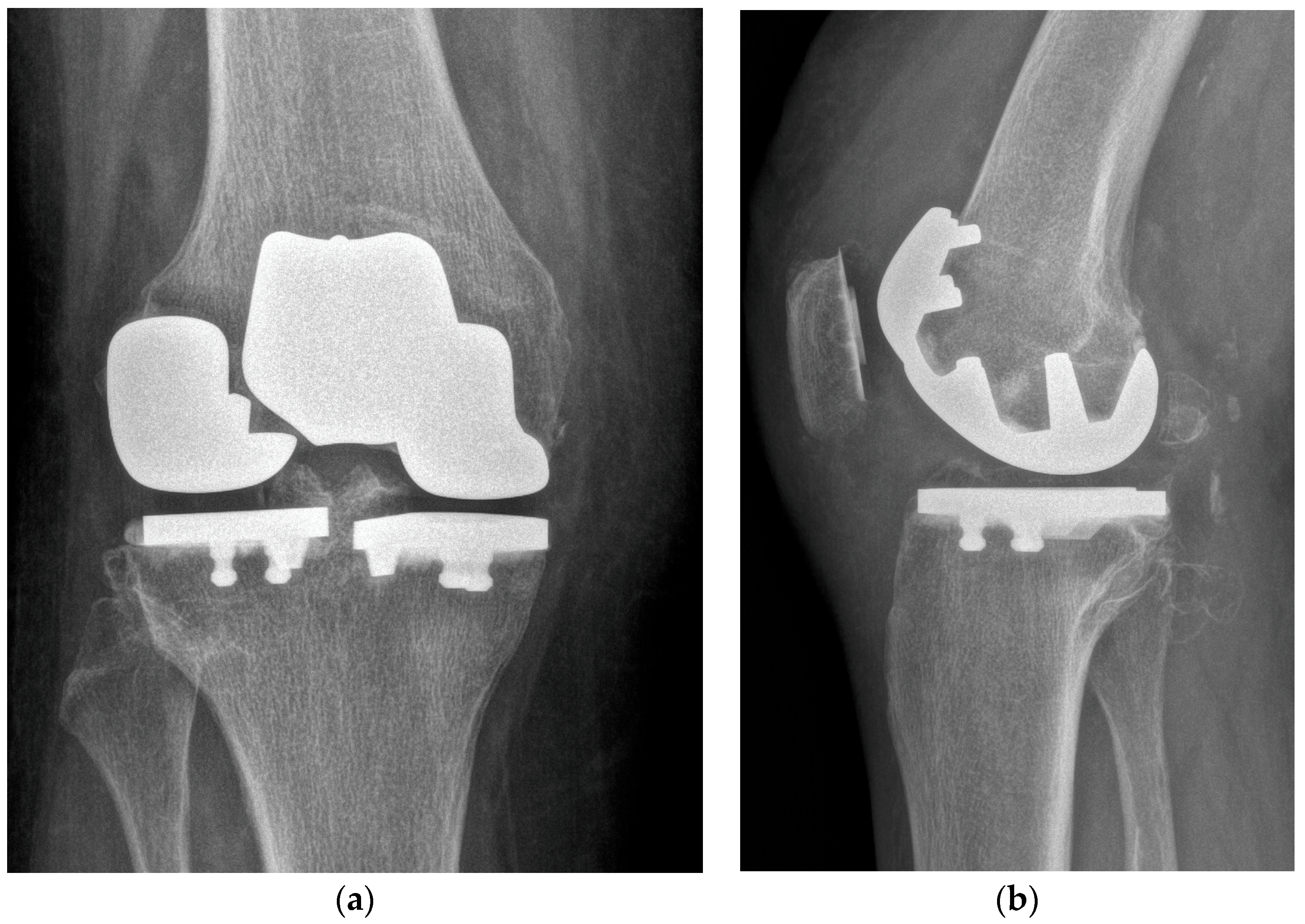
2. Case Description
3. Discussion
4. Future Directions, Clinical Implication and Lessons Learned
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mora, J.C.; Przkora, R.; Cruz-Almeida, Y. Knee Osteoarthritis: Pathophysiology and Current Treatment Modalities. J. Pain Res. 2018, 11, 2189–2196. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Jordan, J.M. Epidemiology of Osteoarthritis. Clin. Geriatr. Med. 2010, 26, 355–369. [Google Scholar] [CrossRef]
- Jang, S.; Lee, K.; Ju, J.H. Recent Updates of Diagnosis, Pathophysiology, and Treatment on Osteoarthritis of the Knee. Int. J. Mol. Sci. 2021, 22, 2619. [Google Scholar] [CrossRef]
- Sisó Almirall, A. Clinical Inertia in Osteoarthritis. Aten. Primaria 2012, 44, 72–73. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kolasinski, S.L.; Neogi, T.; Hochberg, M.C.; Oatis, C.; Guyatt, G.; Block, J.; Callahan, L.; Copenhaver, C.; Dodge, C.; Felson, D.; et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol. 2020, 72, 220–233. [Google Scholar] [CrossRef]
- Rozental, T.D.; Sculco, T.P. Intra-Articular Corticosteroids: An Updated Overview. Am. J. Orthop. 2000, 29, 18–23. [Google Scholar] [PubMed]
- Douglas, R.J. Corticosteroid Injection into the Osteoarthritic Knee: Drug Selection, Dose, and Injection Frequency. Int. J. Clin. Pract. 2012, 66, 699–704. [Google Scholar] [CrossRef]
- Bert, J.M.; Bert, T.M. Nonoperative Treatment of Unicompartmental Arthritis: From Bracing to Injection. Clin. Sports Med. 2014, 33, 1–10. [Google Scholar] [CrossRef]
- Uthman, I.; Raynauld, J.-P.; Haraoui, B. Intra-Articular Therapy in Osteoarthritis. Postgrad. Med. J. 2003, 79, 449–453. [Google Scholar] [CrossRef][Green Version]
- Richards, M.M.; Maxwell, J.S.; Weng, L.; Mathew, G.; Golzarian, J. Inflammatories to Products of Regenerative Medicine. Phys. Sportsmed. 2017, 44, 101–108. [Google Scholar] [CrossRef]
- Sánchez Romero, E.A.; Fernández-Carnero, J.; Calvo-Lobo, C.; Ochoa Sáez, V.; Burgos Caballero, V.; Pecos-Martín, D. Is a Combination of Exercise and Dry Needling Effective for Knee OA? Pain Med. 2020, 21, 349–363. [Google Scholar] [CrossRef] [PubMed]
- Geng, R.; Li, J.; Yu, C.; Zhang, C.; Chen, F.; Chen, J.; Ni, H.; Wang, J.; Kang, K.; Wei, Z.; et al. Knee Osteoarthritis: Current Status and Research Progress in Treatment (Review). Exp. Ther. Med. 2023, 26, 481. [Google Scholar] [CrossRef]
- Ogilvie-Harris, D.J.; Fitsialos, D.P. Arthroscopic Management of the Degenerative Knee. Arthrosc. J. Arthrosc. Relat. Surg. Off. Publ. Arthrosc. Assoc. N. Am. Int. Arthrosc. Assoc. 1991, 7, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Moskowitz, R.W.; Nuki, G.; Abramson, S.; Altman, R.D.; Arden, N.; Bierma-Zeinstra, S.; Brandt, K.D.; Croft, P.; Doherty, M.; et al. OARSI Recommendations for the Management of Hip and Knee Osteoarthritis, Part I: Critical Appraisal of Existing Treatment Guidelines and Systematic Review of Current Research Evidence. Osteoarthr. Cartil. 2007, 15, 981–1000. [Google Scholar] [CrossRef]
- Rönn, K.; Reischl, N.; Gautier, E.; Jacobi, M. Current Surgical Treatment of Knee Osteoarthritis. Arthritis 2011, 2011, 454873. [Google Scholar] [CrossRef] [PubMed]
- Widuchowski, W.; Lukasik, P.; Kwiatkowski, G.; Faltus, R.; Szyluk, K.; Widuchowski, J.; Koczy, B. Isolated Full Thickness Chondral Injuries. Prevalance and Outcome of Treatment. A Retrospective Study of 5233 Knee Arthroscopies. Acta Chir. Orthop. Traumatol. Cech. 2008, 75, 382–386. [Google Scholar] [CrossRef] [PubMed]
- Garner, A.; Van Arkel, R.J.; Cobb, J. Classification of Combined Partial Knee Arthroplasty Aims. Bone Jt. 2019, 101, 922–928. [Google Scholar] [CrossRef]
- Stoddart, J.C.; Dandridge, O.; Garner, A.; Cobb, J.; Arkel, R.J. The compartmental distribution of knee osteoarthritis—A systematic review and meta-analysis. Osteoarthr. Cartil. 2021, 29, 445–455. [Google Scholar] [CrossRef]
- Rolston, L.; Moore, C. Conversion of Lateral Unicompartmental Arthroplasty to Anterior Cruciate Retaining Tricompartmental Knee Arthroplasty. Knee 2010, 17, 249–251. [Google Scholar] [CrossRef]
- Garner, A.J.; Oxon, B.; Oxon, M.A.; Dist, P.; Dandridge, O.W.; Amis, A.A.; Eng, D.; Cobb, J.P.; Oxon, M.; Arkel, R.J. Van Partial and Combined Partial Knee Arthroplasty: Greater Anterior- Posterior Stability Than Posterior Cruciate e Retaining Total Knee Arthroplasty. J. Arthroplast. 2021, 36, 3765–3772.e4. [Google Scholar] [CrossRef]
- Romagnoli, S.; Petrillo, S.; Marullo, M. Knee Resurfacing with Double Unicompartimental Arthroplasty: Rationale, Biomechanics, Indications, Surgical Technique and Outcomes. J. Exp. Orthop. 2021, 8, 78. [Google Scholar] [CrossRef] [PubMed]
- Rossi, S.M.P.; Perticarini, L.; Clocchiatti, S.; Ghiara, M.; Benazzo, F. Mid- to Long-Term Follow-up of Combined Small Implants. Bone Jt. J. 2021, 103, 840–845. [Google Scholar] [CrossRef] [PubMed]
- Thienpont, E. Conversion of a Unicompartmental Knee Arthroplasty to a Total Knee Arthroplasty Can We Achieve A Primary Result ? Bone Jt. J. 2017, 99, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Riley, D.S.; Barber, M.S.; Kienle, G.S.; Aronson, J.K.; von Schoen-Angerer, T.; Tugwell, P.; Kiene, H.; Helfand, M.; Altman, D.G.; Sox, H.; et al. CARE Guidelines for Case Reports: Explanation and Elaboration Document. J. Clin. Epidemiol. 2017, 89, 218–235. [Google Scholar] [CrossRef]
- Bach, C.M.; Nogler, M.; Steingruber, I.E.; Ogon, M.; Wimmer, C.; Göbel, G.; Krismer, M. Scoring Systems in Total Knee Arthroplasty. Clin. Orthop. Relat. Res. 2002, 399, 184–196. [Google Scholar] [CrossRef]
- Tegner, Y.; Lysholm, J. Rating Systems in the Evaluation of Knee Ligament Injuries. Clin. Orthop. Relat. Res. 1985, 198, 43–49. [Google Scholar] [CrossRef]
- Lombardi, A.V.; Berend, K.R.; Walter, C.A.; Aziz-Jacobo, J.; Cheney, N.A. Is Recovery Faster for Mobile-Bearing Unicompartmental than Total Knee Arthroplasty? Clin. Orthop. Relat. Res. 2009, 467, 1450–1457. [Google Scholar] [CrossRef]
- Schwab, P.-E.; Lavand’homme, P.; Yombi, J.C.; Thienpont, E. Lower Blood Loss after Unicompartmental than Total Knee Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 3494–3500. [Google Scholar] [CrossRef]
- Sánchez-Romero, E.A.; Battaglino, A.; Campanella, W.; Villafañe, J.H.; Turroni, S.; Bishop, M.D. Impact on Blood Tests of Lower Limb Joint Replacement for the Treatment of Osteoarthritis. Top. Geriatr. Rehabil. 2021, 37, 227–229. [Google Scholar] [CrossRef]
- Zaballa, E.; Ntani, G.; Harris, E.C.; Arden, N.K.; Cooper, C.; Walker-Bone, K. Return to Work and Employment Retention after Uni-Compartmental and Total Knee Replacement: Findings from the Clinical Outcomes in Arthroplasty Study. Knee 2023, 40, 245–255. [Google Scholar] [CrossRef]
- Kyriakidis, T.; Asopa, V.; Baums, M.; Verdonk, R.; Totlis, T. Unicompartmental Knee Arthroplasty in Patients under the Age of 60 Years Provides Excellent Clinical Outcomes and 10-Year Implant Survival: A Systematic Review. Knee Surg. Sport. Traumatol. Arthrosc. 2023, 31, 922–932. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, H.; Matsumoto, K.; Akiyama, H. Functional Assessment of the Anterior Cruciate Ligament in Knee Osteoarthritis. J. Orthop. 2021, 23, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Garner, A.J.; Dandridge, O.W.; Amis, A.A.; Cobb, J.P.; van Arkel, R.J. Bi-Unicondylar Arthroplasty: A Biomechanics and Clinical Outcomes Study. Bone Jt. Res. 2021, 10, 723–733. [Google Scholar] [CrossRef] [PubMed]
- Romagnoli, S.; Marullo, M. Mid-Term Clinical, Functional, and Radiographic Outcomes of 105 Gender-Specific Patellofemoral Arthroplasties, With or Without the Association of Medial Unicompartmental Knee Arthroplasty. J. Arthroplast. 2018, 33, 688–695. [Google Scholar] [CrossRef]
- Pandit, H.; Mancuso, F.; Jenkins, C.; Jackson, W.F.M.; Price, A.J.; Dodd, C.A.F.; Murray, D.W. Lateral Unicompartmental Knee Replacement for the Treatment of Arthritis Progression after Medial Unicompartmental Replacement. Knee Surg. Sport. Traumatol. Arthrosc. 2017, 25, 669–674. [Google Scholar] [CrossRef] [PubMed]
- Saldanha, K.A.N.; Keys, G.W.; Svard, U.C.G.; White, S.H.; Rao, C. Revision of Oxford Medial Unicompartmental Knee Arthroplasty to Total Knee Arthroplasty—Results of a Multicentre Study. Knee 2007, 14, 275–279. [Google Scholar] [CrossRef]
- Palumbo, B.T.; Henderson, E.R.; Edwards, P.K.; Burris, R.B.; Gutiérrez, S.; Raterman, S.J. Initial Experience of the Journey-Deuce Bicompartmental Knee Prosthesis: A Review of 36 Cases. J. Arthroplast. 2011, 26, 40–45. [Google Scholar] [CrossRef]
- Peersman, G.; Jak, W.; Vandenlangenbergh, T.; Jans, C.; Cartier, P.; Fennema, P. Cost-Effectiveness of Unicondylar versus Total Knee Arthroplasty: A Markov Model Analysis. Knee 2014, 21, S37–S42. [Google Scholar] [CrossRef]

| Title | Author | Contribution |
|---|---|---|
| Knee resurfacing with double unicompartmental arthroplasty: rationale, biomechanics, indications, surgical technique and outcomes [21]. | Romagnoli, S., Petrillo, S. and Marullo Matteo | Recreating normal knee kinematics and function. Excellent clinical results, with a gait pattern and knee function closer to the native one compared to TKA; 94.2% of overall survival rate at 9.4 years of follow-up |
| Mid- to long-term follow-up of combined small implants [22]. | Rossi, S.M.P., Perticarini, L., Clocchiatti, S., Ghiara, M., Benazzo, F. | Excellent clinical and radiological outcomes 91.5% survival rate at mid- to long-term follow-up |
| Bi-unicondylar arthroplasty: A biomechanics and clinical outcomes study [33]. | Garner, A. J., Dandridge, O. W., Amis, A. A., Cobb, J. P., van Arkel, R. J. | Bi-UKA restores a more normal gait than TKA. Patients are highly satisfied and report excellent quality of life following Bi-UKA. Bi-UKA subjects reported higher OKS and EQ-5D. |
| Mid-merm Clinical, Functional, and Radiographic Outcomes of 105 Gender-specific Patellofemoral Arthroplasties, With or Without the Association of Medial Unicompartmental Knee Arthroplasty [34]. | Romagnoli S., Marullo M. | Improvement in knee joint range of motion, clinical and functional Knee Society Score at mid-term follow-up; 95.2% survival rate at 5.5 years follow-up. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parente, A.; Medetti, M.; Basile, G.; Parente, F. One-Stage Tricompartmental Hypoallergenic UKA for Tricompartmental Osteoarthritis: A Case Report. Healthcare 2023, 11, 2999. https://doi.org/10.3390/healthcare11222999
Parente A, Medetti M, Basile G, Parente F. One-Stage Tricompartmental Hypoallergenic UKA for Tricompartmental Osteoarthritis: A Case Report. Healthcare. 2023; 11(22):2999. https://doi.org/10.3390/healthcare11222999
Chicago/Turabian StyleParente, Andrea, Marta Medetti, Giuseppe Basile, and Franco Parente. 2023. "One-Stage Tricompartmental Hypoallergenic UKA for Tricompartmental Osteoarthritis: A Case Report" Healthcare 11, no. 22: 2999. https://doi.org/10.3390/healthcare11222999
APA StyleParente, A., Medetti, M., Basile, G., & Parente, F. (2023). One-Stage Tricompartmental Hypoallergenic UKA for Tricompartmental Osteoarthritis: A Case Report. Healthcare, 11(22), 2999. https://doi.org/10.3390/healthcare11222999






