Absenteeism of Healthcare Personnel in the COVID-19 Era: A Systematic Review of the Literature and Implications for the Post-Pandemic Seasons
Abstract
:1. Introduction
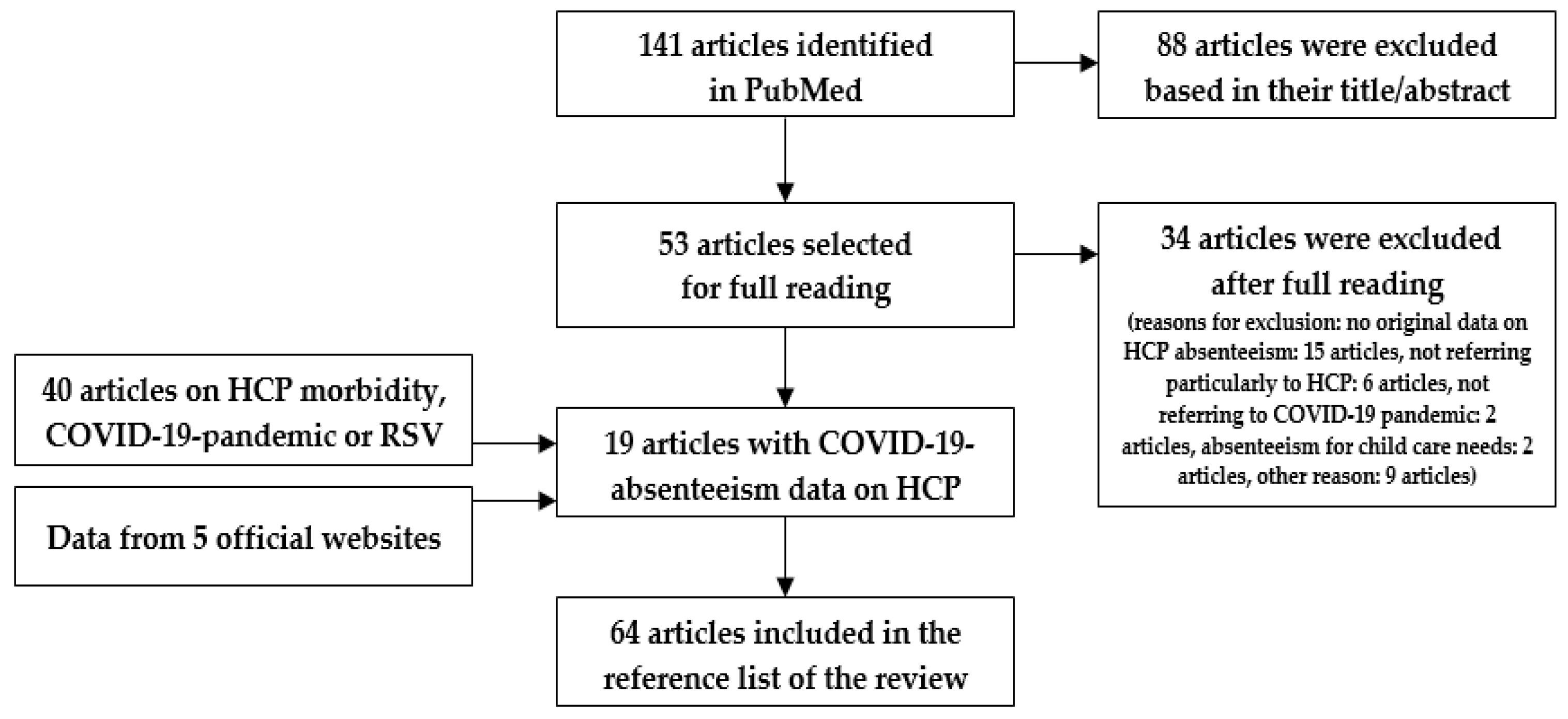
2. Methods
2.1. Search Methodology
2.2. Data Collection
2.3. Review Process
2.4. Supportive Data
2.5. Definitions
3. Results
3.1. Absenteeism in the First Year of the COVID-19 Pandemic
3.2. Impact of Infection Control Strategies on HCP Absenteeism
3.3. Vaccination against COVID-19 and Absenteeism of HCP
3.4. Comparison with Influenza-Associated Absenteeism among HCP
4. Discussion
4.1. Implications for the Upcoming Seasons
4.2. Vaccination Policies for HCP
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Durack, D.T.; Littman, R.J.; Benitez, R.M.; Mackowiak, P.A. Hellenic holocaust: A historical clinico-pathologic conference. Am. J. Med. 2000, 109, 391–397. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Impact of COVID-19 on Health and Care Workers: A Closer Look at Deaths. Available online: https://apps.who.int/iris/bitstream/handle/10665/345300/WHO-HWF-WorkingPaper-2021.1-eng.pdf (accessed on 5 November 2023).
- Maltezou, H.C.; Dedoukou, X.; Tseroni, M.; Tsonou, P.; Raftopoulos, V.; Papadima, K.; Mouratidou, E.; Poufta, S.; Panagiotakopoulos, G.; Hatzigeorgiou, D.; et al. SARS-CoV-2 infection in healthcare personnel with high-risk occupational exposure: Evaluation of 7-day exclusion from work policy. Clin. Infect. Dis. 2020, 71, 3182–3187. [Google Scholar] [CrossRef] [PubMed]
- Jinadatha, C.; Jones, L.D.; Choi, H.; Chatterjee, P.; Hwang, M.; Redmond, S.N.; Navas, M.E.; Zabarsky, T.F.; Bhullar, D.; Cadnum, J.L.; et al. Transmission of SARS-CoV-2 in inpatient and outpatient settings in a Veterans Affairs health care system. Open Forum Infect. Dis. 2021, 8, ofab328. [Google Scholar] [CrossRef] [PubMed]
- Groenewold, M.R.; Burrer, S.L.; Ahmed, F.; Uzicanin, A.; Free, H.; Luckhaupt, S.E. Increases in health-related workplace absenteeism among workers in essential critical infrastructure occupations during the COVID-19 pandemic—United States, March–April 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 853–858. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, E.; Roberts, N.J.; Uluturk, I.; Kaminski, P.; Barlow, J.W.; Zori, A.G.; Hébert-Dufresne, L.; Zusman, B.D. Adaptive staffing can mitigate essential worker disease and absenteeism in an emerging epidemic. Proc. Natl. Acad. Sci. USA 2021, 118, e2105337118. [Google Scholar] [CrossRef]
- Shah, R.; Wright, E.; Tambakis, G.; Holmes, J.; Thompson, A.; Connell, W.; Lust, M.; Niewiadomski, O.; Kamm, M.; Basnayake, C.; et al. Telehealth model of care for outpatient inflammatory bowel disease care in the setting of the COVID-19 pandemic. Intern. Med. J. 2021, 51, 1038–1042. [Google Scholar] [CrossRef]
- Falgarone, G.; Bousquet, G.; Wilmet, A.; Brizio, A.; Faure, V.; Guillouet, C.; Baudino, F.; Roque, I.; Mayol, S.; Pamoukdjian, F. A teleconsultation device, consult station, for remote primary care: Multisite prospective cohort study. J. Med. Internet Res. 2022, 24, e33507. [Google Scholar] [CrossRef]
- Ose, S.O.; Kaspersen, S.L.; Leinonen, T.; Verstappen, S.; de Rijk, A.; Spasova, S.; Hultqvist, S.; Nørup, I.; Pálsson, J.R.; Blume, A.; et al. Follow-up regimes for sick-listed employees: A comparison of nine north-western European countries. Health Policy 2022, 126, 619–631. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Dounias, G.; Rapisarda, V.; Ledda, C. Vaccination policies for healthcare personnel: Current challenges and future perspectives. Vaccine X 2022, 11, 100172. [Google Scholar] [CrossRef]
- Yaghoubi, M.; Salimi, M.; Meskarpour-Amiri, M. Systematic review of productivity loss among healthcare workers due to Covid-19. Int. Health Plan. Manag. 2022, 37, 94–111. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Challener, D.W.; Breeher, L.E.; Frain, J.; Swift, M.D.; Tosh, P.K.; O’Horo, J. Healthcare personnel absenteeism, presenteeism, and staffing challenges during epidemics. Infect. Control. Hosp. Epidemiol. 2021, 42, 388–391. [Google Scholar] [CrossRef] [PubMed]
- Alquézar-Arbé, A.; Piñera, P.; Jacob, J.; Martín, A.; Jiménez, S.; Llorens, P.; Martín-Sánchez, F.J.; Burillo-Putze, G.; García-Lamberechts, E.J.; Del Castillo, J.G.; et al. Impact of the COVID-19 pandemic on hospital emergency departments: Results of a survey of departments in 2020—The Spanish ENCOVUR study. Emergencias 2020, 32, 320–331. [Google Scholar] [PubMed]
- Mas Romero, M.; Avendaño Céspedes, A.; Tabernero Sahuquillo, M.T.; Cortés Zamora, E.B.; Gómez Ballesteros, C.; Sánchez-Flor Alfaro, V.; Bru, R.L.; Utiel, M.L.; Cifuentes, S.C.; Longobardo, L.M.P.; et al. COVID-19 outbreak in long-term care facilities from Spain. Many lessons to learn. PLoS ONE 2020, 15, e0241030. [Google Scholar] [CrossRef]
- Khorasanee, R.; Grundy, T.; Isted, A.; Breeze, R. The effects of COVID-19 on sickness of medical staff across departments: A single centre experience. Clin. Med. 2021, 21, e150–e154. [Google Scholar] [CrossRef]
- Nachtigall, I.; Bonsignore, M.; Hohenstein, S.; Bollmann, A.; Günther, R.; Kodde, C.; Englisch, M.; Ahmad-Nejad, P.; Schröder, A.; Glenz, C.; et al. Effect of gender, age and vaccine on reactogenicity and incapacity to work after COVID-19 vaccination: A survey among health care workers. BMC Infect. Dis. 2022, 22, 291. [Google Scholar] [CrossRef] [PubMed]
- Faramarzi, A.; Javan-Noughabi, J.; Tabatabaee, S.S.; Najafpoor, A.A.; Rezapour, A. The lost productivity cost of absenteeism due to COVID-19 in health care workers in Iran: A case study in the hospitals of Mashhad University of Medical Sciences. BMC Health Serv. Res. 2021, 21, 1169. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Panagopoulos, P.; Sourri, F.; Giannouchos, T.V.; Raftopoulos, V.; Gamaletsou, M.N.; Karapanou, A.; Koukou, D.-M.; Koutsidou, A.; Peskelidou, E.; et al. COVID-19 vaccination significantly reduces morbidity and absenteeism among healthcare personnel: A prospective multicenter study. Vaccine 2021, 39, 7021–7027. [Google Scholar] [CrossRef]
- Chrissian, A.A.; Oyoyo, U.E.; Patel, P.; Beeson, W.L.; Loo, L.K.; Tavakoli, S.; Dubov, A. Impact of COVID-19 vaccine-associated side effects on health care worker absenteeism and future booster vaccination. Vaccine 2022, 40, 3174–3181. [Google Scholar] [CrossRef]
- ten Doesschate, T.; van der Vaart, T.W.; Debisarun, P.A.; Taks, E.; Moorlag, S.J.C.F.M.; Paternotte, N.; Boersma, W.G.; Kuiper, V.P.; Roukens, A.H.E.; Rijinders, B.J.A.; et al. Bacillus Calmette-Guérin vaccine to reduce healthcare worker absenteeism in COVID-19 pandemic, a randomized controlled trial. Clin. Microbiol. Infect. 2022, 28, 1278–1285. [Google Scholar] [CrossRef]
- Parent-Lamarche, A.; Laforce, S. A moderated mediation analysis of New Work-related stressors, psychological distress, and absenteeism in health care during a pandemic: Is recognition the cure for preventing falling in battle? J. Occup. Environ. Med. 2022, 64, 839–847. [Google Scholar] [CrossRef]
- Pirdal, B.Z.; Toplu, F.S.; Esen, B.K.; Aydin, S.N.; Erginoz, E.; Can, G. An assessment on loss of workforce due to COVID-19 among healthcare personnel: A university hospital experience. Work 2022, 73, 59–67. [Google Scholar] [CrossRef]
- Garbin, A.J.Í.; Nascimento, C.C.M.P.; Zacharias, F.C.M.; Garbin, C.A.S.; Moimaz, S.A.S.; Saliba, N.A. Sickness absenteeism of primary health care professionals before and during the COVID-19 pandemic. Rev. Bras. Enferm. 2022, 75, e20220028. [Google Scholar] [CrossRef] [PubMed]
- Maltezou, H.C.; Gamaletsou, M.N.; Koukou, D.-M.; Giannouchos, T.V.; Sourri, F.; Syrimi, N.; Karapanou, A.; Lemonakis, N.; Peskelidou, E.; Papanastasiou, K.; et al. Association between COVID-19 vaccination status, time elapsed since the last vaccine dose, morbidity, and absenteeism among healthcare personnel: A prospective, multicenter study. Vaccine 2022, 40, 7660–7666. [Google Scholar] [CrossRef] [PubMed]
- Teixeira Mendes, E.; Neto, D.G.P.V.; Ferreira, G.M.; Valença, I.N.; Lima, M.P.J.S.; de Freitas, M.F.M.B.; Donalisio, M.R.; Melo, M.C.; Lazari, C.; Goes, J.; et al. Impact of COVID-19 RT-PCR testing of asymptomatic health care workers on absenteeism and hospital transmission during the pandemic. Am. J. Infect. Control 2023, 51, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Khonyongwa, K.; Taori, S.; Soares, A.; Desai, N.; Sudhanva, M.; Bernal, W.; Schelenz, S.; Curran, L. Incidence and outcomes of healthcare-associated COVID-19 infections: Significance of delayed diagnosis and correlation with staff absence. J. Hosp. Infect. 2020, 106, 663–672. [Google Scholar] [CrossRef]
- Murphy, C.; Noonan, N.; O’Toole, E.; Plunkett, P.; Paula Colgan, M.; Canning, C.; Martin, Z.; Hennessy, M. COVID-19, when fourteen days are not enough—A case series of affected healthcare workers. Clin. Case Rep. 2021, 9, 1876–1881. [Google Scholar] [CrossRef]
- Ochoa-Leite, C.; Bento, J.; Rocha, D.R.; Vasques, I.; Cunha, R.; Oliveira, Á.; Rocha, L. Occupational management of healthcare workers exposed to COVID-19. Occup. Med. 2021, 71, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Grandi, J.L.; de Oliveira Silva, C.; Barbosa, D.A. Work absences among hospital cleaning staff during the SARS CoV 2 (COVID-19) pandemic. Rev. Bras. Med. Trab. 2022, 20, 45–54. [Google Scholar] [CrossRef]
- de Paiva, L.G.; Dos Santos, W.M.; de Lima Dalmolin, G. The impact of the SARS-CoV-2 pandemic on sickness absenteeism among hospital workers. Rev. Bras. Med. Trab. 2022, 20, 65–71. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Giannouchos, T.V.; Pavli, A.; Tsonou, P.; Dedoukou, X.; Tseroni, M.; Papadima, K.; Hatzigeorgiou, D.; Sipsas, N.V.; Souliotis, K. Costs associated with COVID-19 in healthcare personnel in Greece: A cost-of-illness analysis. J. Hosp. Infect. 2021, 114, 126–133. [Google Scholar] [CrossRef]
- Arbogast, J.W.; Moore-Schiltz, L.; Jarvis, W.R.; Harpster-Hagen, A.; Hughes, J.; Parker, A. Impact of a comprehensive workplace hand hygiene program on employer health care insurance claims and costs, absenteeism, and employee perceptions and practices. J. Occup. Environ. Med. 2016, 58, e231–e240. [Google Scholar] [CrossRef] [PubMed]
- Pham, T.M.; Tahir, H.; van de Wijgert, J.H.H.M.; Van der Roest, B.R.; Ellerbroek, P.; Bonten, M.J.M.; Bootsma, M.C.J.; Kretzschmar, M.E. Interventions to control nosocomial transmission of SARS-CoV-2: A modelling study. BMC Med. 2021, 19, 211. [Google Scholar] [CrossRef] [PubMed]
- Maltezou, H.C.; Basoulis, D.; Bonelis, K.; Gamaletsou, M.N.; Giannouchos, T.V.; Karantoni, E.; Karapanou, A.; Kounouklas, K.; Livanou, M.E.; Zotou, M.; et al. Effectiveness of full (booster) COVID-19 vaccination against severe outcomes and work absenteeism in hospitalized patients with COVID-19 during the Delta and Omicron waves in Greece. Vaccine 2023, 41, 2343–2348. [Google Scholar] [CrossRef] [PubMed]
- Ip, D.K.M.; Lau, E.H.Y.; Tam, Y.H.; So, H.C.; Cowling, B.J.; Kwok, H.K.H. Increases in absenteeism among health care workers in Hong Kong during influenza epidemics, 2004–2009. BMC Infect. Dis. 2015, 15, 586. [Google Scholar] [CrossRef]
- Gianino, M.M.; Kakaa, O.; Politano, G.; Scarmozzino, A.; Benso, A.; Zotti, C.M. Severe and moderate seasonal influenza epidemics among Italian healthcare workers: A comparison of the excess of absenteeism. Influenza Other Respir. Viruses 2021, 15, 81–90. [Google Scholar] [CrossRef]
- Gianino, M.M.; Politano, G.; Scarmozzino, A.; Stillo, M.; Amprino, V.; Di Carlo, S.; Benso, A.; Zotti, C.M. Cost of sickness absenteeism during seasonal influenza outbreaks of medium intensity among health care workers. Int. J. Environ. Res. Public Health 2019, 16, 747. [Google Scholar] [CrossRef]
- Gianino, M.M.; Politano, G.; Scarmozzino, A.; Charrier, L.; Testa, M.; Giacomelli, S.; Benso, A.; Zotti, C.M. Estimation of sickness absenteeism among Italian healthcare workers during seasonal influenza epidemics. PLoS ONE 2017, 12, e0182510. [Google Scholar] [CrossRef]
- Laris González, A.; Villa Guillén, M.; López Martínez, B.; Gamiño Arroyo, A.E.; Moreno Espinosa, S.; Jiménez Juárez, R.N.; Sánchez Huerta, J.L.; de la Rosa Zamboni, D. Influenza-like illness in healthcare personnel at a paediatric referral hospital: Clinical picture and impact of the disease. Influenza Other Respir. Viruses 2018, 12, 475–481. [Google Scholar] [CrossRef]
- Gaffney, A.W.; Himmelstein, D.U.; Woolhandler, S. Illness-Related Work Absence in mid-April was highest on record. JAMA Intern. Med. 2020, 180, 1699. [Google Scholar] [CrossRef]
- Australian Government. Department of Health and Aged Care. National 2022 Influenza Season Summary. Available online: https://www.health.gov.au/sites/default/files/2022-12/aisr-2022-national-influenza-season-summary.pdf (accessed on 5 November 2023).
- United Kingdom Health Security Agency. Weekly National Influenza and COVID-19 Surveillance Report Week 10 Report (Up to Week 9 Data). 09 March 2023. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1141346/Weekly_Flu_and_COVID-19_report_w10.pdf (accessed on 5 November 2023).
- Lee, S.S.; Viboud, C.; Petersen, E. Understanding the rebound of influenza in the post COVID-19 pandemic period holds important clues for epidemiology and control. Int. J. Infect. Dis. 2022, 122, 1002–1004. [Google Scholar] [CrossRef] [PubMed]
- Lofgren, E.; Naumova, E.N.; Gorski, J.; Naumov, Y.; Fefferman, N.H. How drivers of seasonality in respiratory infections may impact vaccine strategy: A case study in how COVID-19 may help us solve one of influenza’s biggest challenges. Clin. Infect. Dis. 2022, 75, ciac400. [Google Scholar] [CrossRef] [PubMed]
- Stein, R.T.; Zar, H.J. RSV through the COVID-19 pandemic: Burden, shifting epidemiology, and implications for the future. Pediatr. Pulmonol. 2023, 58, 1631–1639. [Google Scholar] [CrossRef] [PubMed]
- Drumright, L.; Frost, S.D.W.; Elliot, A.J.; Catchpole, M.; Pebody, R.G.; Atkins, M.; Harrison, J.; Parker, P.; Holmes, A. H Assessing the use of hospital staff influenza-like absence (ILA) for enhancing hospital preparedness and national surveillance. BMC Infect. Dis. 2015, 15, 110. [Google Scholar] [CrossRef]
- McKimm-Breschkin, J.L.; Hay, A.J.; Cao, B.; Cox, R.J.; Dunning, J.; Moen, A.C.; Olson, D.; Pizzorno, A.; Hayden, F.G. COVID-19, influenza and RSV: Surveillance-informed prevention and treatment—Meeting report from an ISIRV-WHO virtual conference. Antivir. Res. 2022, 197, 105227. [Google Scholar] [CrossRef]
- Bhadelia, N.; Sonti, R.; McCarthy, J.W.; Vorenkamp, J.; Jia, H.; Saiman, L.; Furuya, E.Y. Impact of the 2009 Influenza A (H1N1) Pandemic on Healthcare Workers at a Tertiary Care Center in New York City. Infect. Control Hosp. Epidemiol. 2013, 34, 825–831. [Google Scholar] [CrossRef]
- Kuster, S.P.; Böni, J.; Kouyos, R.D.; Huber, M.; Schmutz, S.; Shah, C.; Bischoff-Ferrari, H.A.; Distler, O.; Battegay, E.; Giovanoli, P.; et al. Absenteeism and presenteeism in healthcare workers due to respiratory illness. Infect. Control Hosp. Epidemiol. 2021, 42, 268–273. [Google Scholar] [CrossRef]
- Johnson, D.H.; Osman, F.; Bean, J.; Stevens, L.; Shirley, D.; Keating, J.A.; Johnson, S.; Safdar, N. Barriers and facilitators to influenza-like illness absenteeism among healthcare workers in a tertiary-care healthcare system, 2017–2018 influenza season. Infect. Control Hosp. Epidemiol. 2021, 42, 1198–1205. [Google Scholar] [CrossRef]
- O’neil, C.A.; Kim, L.; Prill, M.M.; Talbot, H.K.; Whitaker, B.; Sakthivel, S.K.; Zhang, Y.; Zhang, J.; Tong, S.; Stone, N.; et al. Respiratory viral surveillance of healthcare personnel and patients at an adult long-term care facility. Infect. Control Hosp. Epidemiol. 2019, 40, 1309–1312. [Google Scholar] [CrossRef]
- Jiang, L.; McGeer, A.; McNeil, S.; Katz, K.; Loeb, M.; Muller, M.P.; Simor, A.; Powis, J.; Kohler, P.; Di Bella, J.M.; et al. Which healthcare workers work with acute respiratory illness? Evidence from Canadian acute-care hospitals during 4 influenza seasons: 2010–2011 to 2013–2014. Infect. Control Hosp. Epidemiol. 2019, 40, 889–896. [Google Scholar] [CrossRef]
- Frederick, J.; Brown, A.C.; Cummings, D.A.; Gaydos, C.A.; Gibert, C.L.; Gorse, G.J.; Los, J.G.; Nyquist, A.-C.; Perl, T.M.; Price, C.S.; et al. Protecting Healthcare Personnel in Outpatient Settings: The Influence of Mandatory Versus Nonmandatory Influenza Vaccination Policies on Workplace Absenteeism during Multiple Respiratory Virus Seasons. Infect. Control Hosp. Epidemiol. 2018, 39, 452–461. [Google Scholar] [CrossRef] [PubMed]
- Murti, M.; Otterstatter, M.; Orth, A.; Balshaw, R.; Halani, K.; Brown, P.D.; Hejazi, S.; Thompson, D.; Allison, S.; Bharmal, A.; et al. Measuring the impact of influenza vaccination on healthcare worker absenteeism in the context of a province-wide mandatory vaccinate-or-mask policy. Vaccine 2019, 37, 4001–4007. [Google Scholar] [CrossRef] [PubMed]
- Van Buynder, P.; Konrad, S.; Kersteins, F.; Preston, E.; Brown, P.; Keen, D.; Murray, N. Healthcare worker influenza immunization vaccinate or mask policy: Strategies for cost effective implementation and subsequent reductions in staff absenteeism due to illness. Vaccine 2015, 33, 1625–1628. [Google Scholar] [CrossRef]
- Shrestha, L.B.; Foster, C.; Rawlinson, W.; Tedla, N.; Bull, R.A. Evolution of the SARS-CoV-2 omicron variants BA.1 to BA.5: Implications for immune escape and transmission. Rev. Med. Virol. 2022, 32, e2381. [Google Scholar] [CrossRef] [PubMed]
- World Bank. New World Bank Country Classifications by Income Level: 2022–2023. Available online: https://blogs.worldbank.org/opendata/new-world-bank-country-classifications-income-level-2022-2023 (accessed on 5 November 2023).
- World Bank. Disproportionate Deaths among Health Care Workers from Ebola Could Lead to Sharp Rise in Maternal Mortality Last Seen 20 Years Ago—World Bank Report. Available online: https://www.worldbank.org/en/news/press-release/2015/07/08/disproportionate-deaths-among-health-care-workers-from-ebola-could-lead-to-sharp-rise-in-maternal-mortality-last-seen-20-years-ago---world-bank-report (accessed on 5 November 2023).
- Pereira, J.M.; Silva, C.; Freitas, D.; Salgado, A. Burnout among Portuguese radiographers during the COVID-19 pandemic. Radiography 2021, 27, 1118–1123. [Google Scholar] [CrossRef]
- Barros-Areal, A.F.; Albuquerque, C.P.; Silva, N.M.; Pinho, R.d.N.L.; Oliveira, A.P.R.A.; da Silva, D.L.M.; Gomes, C.M.; de Oliveira, F.A.R.; Kurizky, P.S.; Reis, A.P.M.G.; et al. Impact of COVID-19 on the mental health of public university hospital workers in Brazil: A cohort-based analysis of 32,691 workers. PLoS ONE 2022, 17, e0269318. [Google Scholar] [CrossRef] [PubMed]
- Fouad, M.M.; Zawilla, N.H.; Maged, L.A. Work performance among healthcare workers with post COVID-19 syndrome and its relation to antibody response. Infection 2023, 51, 839–849. [Google Scholar] [CrossRef]
- van den Broek, A.; van Hoorn, L.; Tooten, Y.; de Vroege, L. The moderating effect of the COVID-19 pandemic on the mental wellbeing of health care workers on sustainable employability: A scoping review. Front. Psychiatry 2023, 13, 1067228. [Google Scholar] [CrossRef]
- Bayham, J.; Fenichel, E.P. Impact of school closures for COVID-19 on the US health-care workforce and net mortality: A modelling study. Lancet Public Health 2020, 5, e271–e278. [Google Scholar] [CrossRef]
| Country/Study Design | Study Period | Setting | No of HCP | Absent HCP | Duration (Days) | Main Findings |
|---|---|---|---|---|---|---|
| Greece [3]/prospective observational cohort study | 13 March–3 May 2020 | hospitals, HCCs, laboratories | 3398 HCP exposed to SARS-CoV-2 | 41%; 74.8% post- HR exposure | 7 * | HR exposure associated with increased rate and duration of absenteeism |
| Ireland [28]/case series | first pandemic wave | 1 hospital | 456 HCP with COVID-19 | NS | NS | 203 HCP (44.5%) absent for several weeks |
| Spain [14]/cross-sectional study | March–April 2020 | 246 EDs of hospitals | NS | >5% | NS | Physicians, nurses, other emergency staff: in sick leave 20%, 19%, and 16% of the time |
| UK [16]/retrospective cross-sectional survey | 16 March–26 April 2020 | 1 hospital | 328 physicians | 39% | 7 † | Sickness absence rate: 9.1% c/w 1.5% in January 2020; variations between departments |
| Turkey [23]/cross-sectional survey | 11 March 2020–11 March 2021 | 1 hospital | 3967 HCP | 24.7% | 13.5 † | Absenteeism rate: 1.4%; higher absenteeism: age >40 y.o., HR exposure, SARS-CoV-2 positivity |
| Brazil [24]/cross-sectional survey | 2019–2020 | primary HCCs | 977 primary HCP | 85.67% | 9.88 * | 64.79% of HCP absent in 2019 c/w 85.67% in 2020; more respiratory diseases in 2020 |
| Portugal [29]/epidemiological survey | 11 March–15 December 2020 | oncology hospital | 2300 HCP | 6.7% | 33 * before c/w 20 * after 14 October | On 14 October new return-to-work strategy for HCP based on clinical and laboratory criteria |
| Spain [15]/epidemiological study | 6 March–5 April 2020 | LTCF | 190 employees | 24.6% | 19.2 * | Severe COVID-19 outbreak: 33.6% attack rate among 198 residents, 69 new employees, 276,281 Euros total cost (35.1% due to absenteeism and staff replacement) |
| UK [27]/observational study | 1 March–18 April 2020 | 1 hospital | NS | NS | NS | Incidence of HA-COVID-19 correlated with HCP absence due to COVID-19 |
| Brazil [30]/retrospective cohort study | 24 March–31 December 2020 | 1 hospital | NS | 199 cleaning staff with 689 medical certificates | 5.82 * | 44.2% with suspected/confirmed COVID-19; longer absence in suspected COVID-19 c/w other causes (mean 5.82 vs. 3.82 days) |
| Brazil [31]/cross-sectional survey | September 2014–December 2020 | 1 hospital | 1229 HCP | NS | NS | Mean sickness absenteeism was 5.10% during the COVID-19 pandemic c/w 2.97% pre-pandemic; ×2.03 increased sickness absence duration and ×2.49 increased daily cost during the pandemic |
| Iran [18]/cross-sectional survey | 19 February–21 September 2020 | 25 hospitals | 22,000 HCP | 8.9% | 16.44 * | Negative association between absenteeism with being a physician and work experience |
| Canada [22]/cross-sectional survey | 18 October 2021–27 January 2022 | Quebec healthcare sector | 1128 new-work HCP | NS | 18.08 * | Increased COVID-19-associated workload and fear of COVID-19 were indirectly associated with higher level of absenteeism |
| Brazil [26]/time-series analysis | March–August 2020 | 1 hospital | 429 asymptomatic HCP | 17.3% | NS | SARS-CoV-2 PCR testing of HCP was associated with reduced absenteeism; duration of absence increased by 473% in 2020 c/w 2019 |
| Greece [19]/prospective observational study | 4 January–18 April 2021 | 5 hospitals | 7445 HCP | 11.3% among unvaccinated c/w 4.7% among vaccinated HCP | 11.9 * in unvaccinated c/w 6.9 * in vaccinated | 66.42% vaccine effectiveness of 2 doses of Pfizer mRNA vaccine against absenteeism |
| Greece [25]/prospective observational study | 14 November 2021–17 April 2022 | 5 hospitals | 7592 HCP | 28.7% | 8.1 * in fully vaccinated c/w 9.7 * in non-fully vaccinated | Fully vaccinated had shorter absenteeism c/w with non-fully vaccinated (OR: 0.56); >17.1 weeks from last vaccine dose associated with longer absence |
| USA [20]/cross-sectional survey | February–April 2021 | 2 healthcare Systems | 2103 vaccinated HCP | 18.1% | 93% for 1–2 days | Generalized symptoms, being a nurse and Moderna vaccine recipient were associated with increased risk for work absence |
| Germany [32]/cross-sectional survey | 19 May–21 June 2021 | 89 hospitals | 8375 HCP | 23% | NS | Being a male, older age, and BNT162b vaccine recipient were associated with lower risk for work absence |
| Netherlands [21]/randomized trial | 24 March 2020 27 March 2021 | 9 hospitals | 1511 HCP exposed to COVID-19 patients | BCG group: 2.8% placebo: 2.7% | NS | BCG vaccine had no effect on absenteeism |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maltezou, H.C.; Ledda, C.; Sipsas, N.V. Absenteeism of Healthcare Personnel in the COVID-19 Era: A Systematic Review of the Literature and Implications for the Post-Pandemic Seasons. Healthcare 2023, 11, 2950. https://doi.org/10.3390/healthcare11222950
Maltezou HC, Ledda C, Sipsas NV. Absenteeism of Healthcare Personnel in the COVID-19 Era: A Systematic Review of the Literature and Implications for the Post-Pandemic Seasons. Healthcare. 2023; 11(22):2950. https://doi.org/10.3390/healthcare11222950
Chicago/Turabian StyleMaltezou, Helena C., Caterina Ledda, and Nikolaos V. Sipsas. 2023. "Absenteeism of Healthcare Personnel in the COVID-19 Era: A Systematic Review of the Literature and Implications for the Post-Pandemic Seasons" Healthcare 11, no. 22: 2950. https://doi.org/10.3390/healthcare11222950
APA StyleMaltezou, H. C., Ledda, C., & Sipsas, N. V. (2023). Absenteeism of Healthcare Personnel in the COVID-19 Era: A Systematic Review of the Literature and Implications for the Post-Pandemic Seasons. Healthcare, 11(22), 2950. https://doi.org/10.3390/healthcare11222950









