Abstract
Older people in low-population density regions tend to have fewer resources to engage in regular physical activity (PA) compared to their counterparts in urban areas. Moreover, PA assumes different dimensions, and the amount of PA related to each dimension may differ between women and men, predisposing them to different PA practices. Therefore, this cross-sectional study aims to describe the prevalence of barriers to PA, gender differences, and their associations with different PA dimensions. A total of 259 older adults (153 women and 106 men; age, 75.17 ± 8.05 years old) living in the community in the region of Guarda (Portugal) were interviewed face to face to record their sociodemographic characteristics, general health status (comorbidity index and self-reported health), PA behaviour, and barriers to PA. Women were more likely to report “low” income and living alone (p ≤ 0.05), while men reported a higher negative health status than women (p < 0.05). Two intrinsic (“Fear of injury” (40.1%) and “Need for rest” (26.3%)) and two extrinsic barriers (“Lack of nearby facilities” (30.5%) and “I don’t have transport” (25.6%)) were the most prevalent. For women, age, self-reported health, comorbidity index, and intrinsic and extrinsic barriers were similarly associated with the different PA dimensions. However, only self-reported health and extrinsic barriers were the variables associated with the different PA dimensions in men. Therefore, strategies to promote active ageing in low-population density regions should be focused on reducing intrinsic and extrinsic barriers based on gender and the PA dimension to be achieved.
1. Introduction
Physical activity (PA) promotion and the reduction of sedentary behaviour (SB) are crucial for protection from non-communicable diseases [1,2], cognitive decline [3], and mental illness [4], as well as reducing all-cause mortality [5] and improving health-related quality of life in the general population, including older adults [6,7]. These benefits are mirrored in PA recommendations, indicating that older adults should engage in at least 150–300 min of moderate-intensity aerobic PA, or at least 75–150 min of vigorous-intensity aerobic PA (or an equivalent combination of moderate- and vigorous-intensity activity) throughout the week, muscle-strengthening activities of moderate or higher intensity and involving all major muscle groups two or more days per week, and perform on three or more days per week multicomponent physical activities focusing on functional balance and strength at moderate or higher intensity, to improve functional fitness and prevent falls [8].
Nevertheless, despite the clear benefits of being active, women and men from all over the world become less active as they get older and do not meet the PA and SB recommendations [9]. Consequently, the promotion of PA in this age group has become a priority in healthy ageing policies [10]. However, to design successful strategies and programmes to promote PA, it is necessary to investigate and understand the perceived barriers experienced by older adults that contribute to decreased PA levels. Some studies have shown that lack of knowledge, skills, abilities, family support, family roles, perceived fears of PA (e.g., pain, injury, or risk of falls) and environmental barriers (e.g., access to facilities and transport or adverse climate conditions) are the main barriers to PA among community-dwelling older adults [11,12,13,14]. However, several factors, such as gender, age, or socioeconomic conditions, may shape how perceived barriers affect SB and PA levels [12,14,15,16]. For instance, previous studies showed gender differences [17,18], with older women reporting a higher prevalence of barriers to moderate to vigorous PA (MVPA) than older men. However, older women are typically more involved in household activities [19], and thus tend to participate more in light-intensity PA (LPA) [20,21]. Along this line, and in relation to LPA, a study conducted by Stalling et al. observed that women spent more time on active transport, home-based activities, and housework than men, while men allocated more time to leisure activities [22].
In view of the different patterns of PA and SB in older adults, it is important to identify the different barriers that older adults may perceive for each of the different PA domains, including the aforementioned factors of gender or age, in order to enable them to comply with the current recommendations of international organisations (i.e., reduce sedentary time to eight hours or less per day and replace it with physically-active behaviours, starting with LPA and progressively introducing MVPA [23]). In this context, LPA has emerged in recent years as a potentially effective strategy for older adults, given its plausibility and the benefits associated with its practice [21,24,25,26,27,28,29]. According to the results obtained by Dupré et al. [29], LPA should be included in future guidelines, since it allows minimum doses to be reached more easily and reduces SB in older adults, and, as their results suggest, the dose–effect curve may be stronger for LPA.
In this sense, the role of perceived barriers in predicting PA behaviour in older adults remains understudied, especially barriers related to LPA, as most research has investigated the barriers to MVPA [30,31]. This is even more critical in rural and inland areas, which are typically the most neglected and under-resourced regions. As recently stated by Rai et al., the different domains of PA ought to be examined to determine and identify any relationships that occur at that level [17], as, despite the potential of LPA, previous studies did not consider them [14].
Therefore, since public strategies to overcome barriers to PA need to be tailored to the specific characteristics and demands of the target population, we aimed to investigate the prevalence and gender differences of perceived barriers to PA among older adults living in low-population density areas, and their association with different dimensions of PA.
2. Materials and Methods
Data from the Gmove+ project were used for the analysis. Potential participants were recruited through a dissemination made at public health centres in collaboration with doctors and health professionals, as well as through poster announcements in public and commercial spaces, churches, and social networks in the district of Guarda (Portugal). Data collection was performed by a trained research team, tutored by the principal researcher of the project.
2.1. Participants
A total of 259 cases (153 women and 106 men) were included. Participants were recruited from the Guarda health care unit, the day care centres of the district, the physical exercise programmes of the municipality of Guarda, and through the dissemination and promotion of PA activities related to the project.
Exclusion criteria were: (i) aged under 65 years old; (ii) having a mobility impairment; (iii) having cognitive limitations that affect the comprehension or performance of the psychometric tests; and (iv) living in social and health care support centres. All participants were informed about the purpose of the project and signed an informed consent form prior to data collection. The Gmove+ project was approved by the Ethics Committee of the Local Health Unit of Guarda (Ref. 11136), in accordance with the Declaration of Helsinki.
2.2. Sociodemographic Characteristics
Individual sociodemographic factors obtained from the face to face interview included: age, gender, education level according to the Portuguese Educational System [32] (<4th Grade, =4th Grade, and >4th Grade), income level (based on the Portuguese average salary scales and grouped into three subcategories: Low (<500 €), Average (500–750 €), and High (>750 €) income, and living arrangement (coded as Living with a partner or Living alone).
2.3. General Health Status
The Charlson comorbidity index was used to convert the comorbidities into a score ranging from 0 to 10 [33]. Additionally, the SF-36 questionnaire question “In general, how would you describe your health?” was used to assess self-reported health status [34]. Based on the self-reported health status, participants were classified as having a negative or positive health perception.
2.4. Yale Physical Activity Survey
The PA assessment was conducted using the Portuguese version of the Yale PA Survey (YPAS-PT) for older adults [35]. The YPAS-PT determines the type, amount, and pattern of PA for a typical week in the last month. Five activity dimensions (vigorous activity, leisurely walking, moving, standing, and sitting) were obtained by multiplying the partial scores obtained from the questionnaire items (resulting from the multiplication of a frequency score by a duration score for each dimension) by a weighting factor based on the relative intensity of each activity dimension [36,37]. The validity and reliability of this questionnaire have been previously reported [35].
2.5. Perceived Barriers to the PA Questionnaire
A Portuguese version of the Perceived Barriers to PA Questionnaire was applied to measure barriers to PA in older populations [38,39]. This 22-item survey employs a five-point Likert scale (“never”, “rarely”, “sometimes”, “often”, and “always”) to rate the frequency with which factors (barriers) interfere with PA practice decisions.
Based on the social-ecological model of recreational PA [40], additional questions about PA program facilities, public transportation, family, and professional assistance were added to the previous questionnaire to better reflect the Gmove+ project’s goal of promoting and disseminating PA programs in the community. Given the importance of introducing new items tailored to local sociocultural contexts, the content and face validity of the questionnaire was initially assessed by our research team, and questions were discussed with a sample of older adults before data collection. Also, standard steps for the adaptation of cultural psychometric scales were followed [41], and questionnaire adjustments were made to improve the participants’ comprehension. The final version of the questionnaire consisted of 29 items. The interviewers were previously trained to gather the information correctly.
2.6. Statistical Analysis
Descriptive statistics are shown as means ± standard deviation or as percentages (frequencies), and normality was tested using the Shapiro–Wilk test. Perceived barriers to PA latent factor validity were psychometrically tested, performing a Confirmatory Factor Analysis. Full Information robust Maximum Likelihood was used to handle the small amount of missing data at the item level (missing at random = 3%) as proposed by a previous study [42]. The hypothesized model was tested using Amos 23.0 following the previous recommendations [43]. The absolute fit of the models was evaluated using the chi-square by degrees of freedom ratio (χ2/df), and the Standardized Root Mean Square Residual (SRMSR), while the relative fit was assessed using the Normed Fit Index, the Tucker–Lewis Index, and the Comparative Fit Index. For these indices, values over 0.95 indicate a good fit, and values over 0.98 of a very good fit [44]. A value lower than 0.08 for SRMSR is considered acceptable [45]. The Root Mean Square Error of Approximation (RMSEA) was used for evaluating how well the implied model reproduced the variance-covariance matrix of the data, keeping in mind that RMSEA values as low as 0.08 are deemed adequate, and below 0.06 represent a good fit to the model [45]. Then, the extracted factors were used in a multiple regression analysis with stepwise variable selection to identify the PA predictors [42].
For gender comparisons, Pearson’s chi-squared (χ2), an independent sample t test, or the Mann–Whitney U test, respectively, were used. Moreover, stepwise regression analysis was performed. The PA dimensions (vigorous, leisurely walking, moving, standing, and sitting) were treated as dependent variables, while the intrinsic and extrinsic barriers to PA, age, comorbidities index and self-reported health status were treated as independent variables. In all regression models checked, the collinearity was evaluated by the Variance Inflation Factors test, and the goodness of fit model was verified by the Nagelkerke R square test. IBM SPSS Statistics v.24.0 (IBM Corp, Armonk, NY, USA) was used for statistical analysis and the statistical significance level was set at 0.05.
3. Results
Table 1 and Figure 1 present the results of the confirmatory factor analysis model used to confirm the questionnaire-based factors for perceived barriers to PA. Results from this model indicate that the index factor analysis fit the model well with the 2-factor structure and 15 of 29 items. The existence of intrinsic and extrinsic factors was considered based on the meaning of the items that compose each factor. On the main fit measures, the model showed appropriate scores.

Table 1.
Confirmatory factor analysis.
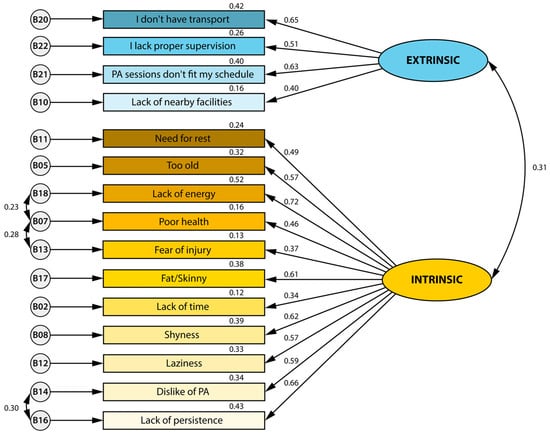
Figure 1.
Theoretical model of barriers to Physical Activity Questionnaire Portuguese version with the factor loading in each dimension.
Sociodemographics, health status, and indicators of PA levels are summarised in Table 2. Men and women were matched for age, with 70–79 years being the most frequent age range (43.1%). Most participants had completed the 4th grade of schooling, regardless of gender. Women were more likely to report “Low income” (45.8% vs. 28.3%) and to live alone (49.7% vs. 32.1%) than men (p ≤ 0.05). Regarding general health status, no gender differences were present in the comorbidity index. Both women (92.7%) and men (74.5%) claimed to have a positive self-reported health status. However, male participants reported a higher negative health status than women (p < 0.05). No gender differences were found in the PA dimensions.

Table 2.
Sociodemographic, general health status, and levels of PA characteristics of the participants.
Results of the perceived barriers to PA questionnaire are presented in Figure 2. The results showed that “Fear of injury (40.1%), “Lack of nearby facilities” (30.5%), “Need for rest” (26.3%), and “I don’t have transport” (25.6%) were the most prevalent barriers to PA among all participants. Women presented similar values compared to men except for the barrier “Fear of injury” (45.8% vs. 33.0%; p < 0.01), reporting a higher percentage than men.
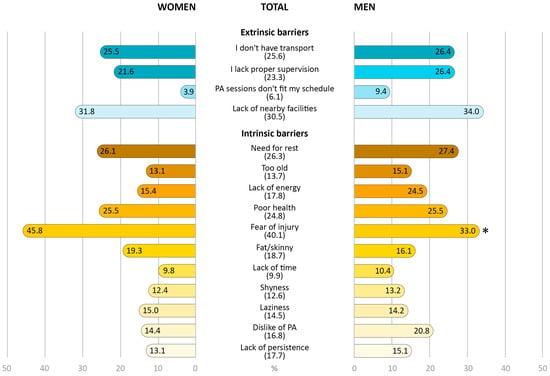
Figure 2.
Prevalence of total and gender-specific perceived barriers to PA. Extrinsic barriers are represented in blue, and intrinsic barriers in yellow. * differences in gender distribution. Data are presented as percentages (%) (n = 259).
Table 3 and Table 4 show the associations between the PA dimensions, intrinsic and extrinsic barriers to PA, health status, and age for women and men, respectively. For women (Table 3), model 2, which included the comorbidity index and self-reported health status, better explained (7%) the variance of vigorous index [F (1.150) = 6.390; R2 = 0.068; p = 0.002]. Meanwhile, the intrinsic factors (model 1) were the only factor with explanatory power (6%) for the leisure walk index [F (1.152) = 11.042; R2 = 0.062; p = 0.001]. Associations with moving index were suggested by three models, with model 3 (age, intrinsic factors, and extrinsic factors) demonstrating the best explanatory power [F (3.149) = 5.673; R2 = 0.084; p = 0.001]. Only two models suggested significant associations with the standing index, with model 2 having the best explanatory power [F (2.152) = 6.260; R2 = 0.065; p = 0.002]. In the associations with the sitting index, only age (model 1) showed a significant association with an explanatory power of 9% [F (1.152) = 16.552; R2 = 0.093; p < 0.001]. For men (Table 4), self-reported health status alone explains 3% of the vigorous index variance [F (1.99) = 4.365; R2 = 0.033; p = 0.039], 12% of the leisure walking index variance [F (1.100) = 14.230; R2 = 0.116; p < 0.001], 3% of the standing index variance [F (1.100) = 4.213; R2 = 0.031; p = 0.043], and 3% of the sitting index [F (1.100) = 2.936; R2 = 0.034; p = 0.034]. However, in the associations with the moving index, extrinsic factors presented 10% of explanatory power [F (1.100) = 11.531; R2 = 0.094; p = 0.001].

Table 3.
Association between PA dimensions and PA barriers, health status, and age for women (n = 153).

Table 4.
Association between PA dimensions and PA barriers, health status, and age for men (n = 106).
4. Discussion
The main findings of this study are that (i) two intrinsic (“Fear of injury” and “Need for rest”) and two extrinsic barriers (“Lack of nearby facilities” and “I don’t have transport”) were the most reported, with women being more likely to express “Fear of injury”; (ii) for women, all factors (age, self-reported health status, comorbidity index, and intrinsic and extrinsic barriers) were associated with the different PA dimensions; and (iii) only self-reported health and extrinsic barriers were the factors associated with the different PA dimensions in men.
4.1. Prevalence and Gender Differences of Perceived Barriers to PA
Regarding intrinsic barriers, “Fear of injury” is the most frequent barrier to PA among the older adults participating in this study (40.1%), being higher in women. According to the Special Eurobarometer 525 for Sport and Physical Activity, this is the fourth reason among the population aged 55 and over in Europe. In Portugal in particular, this barrier has increased by 10% since 2017. This is probably due to the Portuguese population ageing [46]. Also, at least one in four older people reported that the second reason is “Need to rest” (26.3%), closely followed by “Poor health” (24.8%), which is the most frequently reported according to the Eurobarometer reports in older populations [46]. These data are consistent with previous research [47,48,49] reporting that fear of injury, as well as fear of falling and health problems, are the main barriers in older populations. Indeed, a recent systematic review showed a consistent association between PA with increased fear of falling, but not with falls or fractures [50]. As the authors reinforce, it is necessary to promote PA-related health behaviours, as fear of falling influences mobility, increases social isolation, and decreases levels of self-efficacy, which are other potential barriers to PA and factors related to quality of life. In particular, for the Portuguese population, a recent study investigated PA barriers across multiple age groups and reported that, for older adults, health problems and a dislike of exercise or lack of motivation were the most prevalent [48], partially confirming our findings regarding the main barriers to PA. Moreover, other participant characteristics may explain these findings. For instance, reduced educational levels are likely to lead to lower health literacy, and thus less comprehension of the health benefits of regular PA [14,15,51].
For extrinsic barriers, “Lack of nearby facilities” and “I don’t have transport” emerged as the main barriers to PA. Also, both barriers seem to be closely related. Previous studies in large cities showed how a greater supply of public transport allows people to move around more easily, in contrast to regions with low population density where the transport network is limited [12,14,15], and how the opportunity to practice systematic PA in the countryside is scarcer than in large centres due to the limited amount of infrastructure in the inland population [16]. Indeed, evidence referred to the “decentralisation of facilities” as a crucial facilitator of regular PA practice [12,52]. Furthermore, and in relation to extrinsic barriers, Gray et al. previously observed that socioeconomic status can influence barriers to PA. Those with lower socioeconomic status often report more barriers and, consequently, lower levels of PA practice, which is also influenced by age. [53]. This is partially in line with our results, which show that more than half of our participants have a low income (below the national minimum living wage), which may have an impact on barriers to PA.
Regarding gender differences, although there are some socioeconomic disparities between women and men, our data only report differences for the intrinsic barrier “Fear of injury”. Thus, although socioeconomic status is an independent factor acting as a barrier to PA [47], our sample does not seem to be influenced by it. Contrary to Lee [20], our study did not find that environmental (or extrinsic) factors specific to women represent worse conditions for their PA practice. Similarly, although men were more likely to report negative self-reported health status, our results did not observe differences in the “Poor health” barrier, contrary to previous studies [17,20,54]. Historically, older Portuguese women are less involved in regular PA, exercise, or sports activities [46,55,56], and are more sedentary than men [57,58]. However, perceived PA levels are normally overestimated in older women, largely conditioned by the fact that they are involved in more domestic tasks compared to men [59,60,61]. Likewise, there are gender differences in life trajectories related to social and health aspects [62]. In that sense, regular PA practice in older adults is positively related to education, exercise history, and self-efficacy [63,64], which tends to be lower in women of all ages and has been established as a barrier to PA [53,65]. This may be closely related to fear of injury, being the only barrier that showed gender differences in our sample, in agreement with Arazi et al. [47].
4.2. Correlation between PA Barriers and PA Dimensions
In the regression model, the comorbidity index, self-reported health status, and age variables were added to the model, as they showed correlations with intrinsic and extrinsic factors. Indeed, previous studies have reported that age, comorbidities, and self-rated health status were independent barriers to PA [14,49,66]. As initially hypothesised, the health-related factor was associated with different PA dimensions, but this was mainly observed in men. A potential explanation for these results is that they may increase their participation in regular physical activity if they feel good, regardless of age, and illness, among other factors. Unlike men, more factors correlated with different PA dimensions among women. These findings are consistent with previous research, which found that women are more easily affected by sociodemographic and health-related outcomes, resulting in low adherence to PA programmes [14,67].
Consistent with previous findings, which showed that poor health outcomes were positively and independently related to the odds of non-adherence to the recommended levels of MVPA [30], health-related issues were negatively correlated with the vigorous PA dimension in both genders. However, in women, possible comorbidities play a significant role in the vigorous PA engagement in this study. Although both women and men presented a reduced number of factors correlated to the leisure walking domain in our study, there were gender differences in the associations. Our results contradict a previous study that described a higher number of factors associated with leisure walking PA [68]. A possible explanation is that both genders have no difficulty achieving this PA dimension, classified as light–moderate PA, and it is more likely to be part of the daily life of this population. On the other hand, one possible reason for the gender differences in the associated factors for leisure PA is the fact that men tend to report engaging in more exercise for enjoyment than women, potentially because women tend to spend more time on household chores [48]. Extrinsic factors were correlated with the PA enrolled as the Moving index domain in both genders. In this regard, place of residence has been shown to be a determinant factor, notably for older people living in rural areas, where services or support are generally lacking compared to urban areas [41]. For women, in addition to extrinsic barriers, age and intrinsic barriers are other factors that explain the Moving index. Regarding the age factor, older adults are aware of their age-related physical limitations, leading to a lack of confidence in their abilities [30,69]. As noted above, women in this study had a higher prevalence of the “Fear of injury” barrier than men. It, therefore, seems reasonable that these two factors are determinants for our women, and not for their counterparts.
To our knowledge, the relationships between barriers to PA and the standing and sitting indices are the least investigated. Concerning the Standing index, a growing interest has emerged as studies show that increasing the volume of light to moderate PA in older individuals may positively affect their health status [70,71]. Based on our results, improving modifiable environmental conditions to reduce external barriers is a promising strategy to increase this PA dimension in older women. Also, the effect of age can be counteracted with awareness programs on the benefits of regular PA and the adaptation of facilities to the needs of this population. In contrast, self-reported health status was the factor most related to the standing domain in men. In fact, they were significantly more likely to report negative values for this factor. Therefore, modifying their perception of health status seems to be key in men, specifically to promote more time in the standing position and, in general, to increase their PA levels and reduce SB. Finally, sitting is the most common SB among older populations and is related to an increased risk of cardiovascular disease and all-cause mortality [72]. Age and self-reported health status were predictors for sitting time in our female and male participants, respectively. Ageing itself (reported by women) and its characteristics play a key role in the development of SB. Along with declining physical, mental, and cognitive health (reported by men), which limits their capacity and/or motivation for standing for long periods of time or performing PA, older adults describe additional leisure time associated with retirement, mostly occupied with typically sedentary leisure tasks (sewing, playing cards, playing chess, etc.) [73].
4.3. Confirmatory Factor Analysis Model
Our results showed that these two barriers are theoretically meaningful for PA engagement in this population. Extrinsic barriers refer to the infrastructure in the neighbourhoods and communities, while intrinsic barriers include personal motivations often associated with health, mood, and psychosocial factors [14,74].
4.4. Limitations, Strengths, and Future Directions
In general, the findings of this study revealed that results for women are consistent with the ecological model [30], which implies that, when compared to men, a greater variety of sociodemographic and health-related characteristics function as predictors of PA behaviours. However, our study presents some limitations. Firstly, results related to physical activity may have been affected by the subjective assessment of PA. This may have magnified or diminished real PA levels compared to more objective measures such as accelerometery. Additionally, the non-consideration of local sociocultural features (such as health literacy) by the assessment tools may also represent a limitation in the collection and interpretation of the results. Strengths of this research include an exploration of associations between LPA, SB, and barriers to PA, as the most recent guidelines recommend examining the factors that influence these PA behaviours, especially in older individuals. Moreover, the study was performed with older adults belonging to low-population density regions, mostly in rural contexts, revealing barriers to PA that were not identified in larger Portuguese studies. Thus, future research is recommended to address the issue of PA barriers using other approaches; to consider not only the barriers to different levels of PA, but also the existence of facilitators and beliefs about the benefits of regular PA, and, in many cases, to perform cross-cultural adaptation even for well-established questionnaires, as suggested by the literature.
4.5. Practical Applications
Identifying barriers and facilitators of PA considering geographical context should be the first strategy before developing community PA programs. Previous studies have identified a global trend, but identifying local differences can lead to more tailored and effective policies and guidelines to encourage an active lifestyle. Identifying the most common barriers that inhibit the regular practice of PA is crucial, since evidence suggests that gradually accumulating light to moderate levels of PA may positively impact the general health status of older people.
5. Conclusions
The achievement of the recommended levels of PA is influenced by several perceived barriers to PA, among other factors. As demonstrated by our findings, more specifically by the observed associations between barriers and light to moderate levels of PA, educating the population about the health benefits of achieving the recommended levels of PA is a priority. Likewise, decreasing extrinsic barriers (i.e., improving access to facilities and providing public transportation to fitness or sports centres) should be the priority in promoting PA, especially among older women living in low-population density regions. Furthermore, PA decentralisation policies should be implemented as prerequisites to increase population adherence for regular participation in PA.
Author Contributions
Conceptualization, C.V.-C., N.S., E.M., C.V. and V.P.L.; methodology, C.V.-C., N.S., E.M., C.V. and V.P.L.; formal analysis, A.R.C.-B., V.P.L., C.V.-C. and M.R.-A.; writing—original draft preparation, M.R.-A. and C.V.; writing—review and editing, C.V., E.M., A.B., M.R.-A., A.R.C.-B., N.S., V.P.L. and C.V.-C. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by PORTUGAL2020 and by the Fundação para a Ciência e a Tecnologia (FCT, I.P.), under project SAICT-POL/23811/2016 and through the Portuguese Foundation for Science and Technology, I.P., under project UID04045/2020. The Polytechnic of Guarda partly supported the research reported in this publication.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Local Health Unit of Guarda (Ref. 11136).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available on request.
Acknowledgments
M.R.-A. acknowledges the financial support received from the Spanish Ministry of Universities through the Grants for the Requalification of the Spanish University System under the Postdoctoral Margarita Salas Programme (RSUC.UDC.MS09), funded by the European Union–Next Generation. A.R.C.-B. and A.B. are part of the Highly Qualified Human Resources Project, reference number CENTRO-04-3559-FSE-000162.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Katzmarzyk, P.T.; Friedenreich, C.; Shiroma, E.J.; Lee, I.-M. Physical inactivity and non-communicable disease burden in low-income, middle-income and high-income countries. Br. J. Sports Med. 2022, 56, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; Ozemek, C.; Carbone, S.; Katzmarzyk, P.T.; Blair, S.N. Sedentary behavior, exercise, and cardiovascular health. Circ. Res. 2019, 124, 799–815. [Google Scholar] [CrossRef]
- Stubbs, B.; Chen, L.J.; Chang, C.Y.; Sun, W.J.; Ku, P.W. Accelerometer-assessed light physical activity is protective of future cognitive ability: A longitudinal study among community dwelling older adults. Exp. Gerontol. 2017, 91, 104–109. [Google Scholar] [CrossRef]
- Vancampfort, D.; Firth, J.; Schuch, F.B.; Rosenbaum, S.; Mugisha, J.; Hallgren, M.; Probst, M.; Ward, P.B.; Gaughran, F.; De Hert, M. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: A global systematic review and meta-analysis. World Psychiatry 2017, 16, 308–315. [Google Scholar] [CrossRef]
- Ekelund, U.; Tarp, J.; Steene-Johannessen, J.; Hansen, B.H.; Jefferis, B.; Fagerland, M.W.; Whincup, P.; Diaz, K.M.; Hooker, S.P.; Chernofsky, A.; et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: Systematic review and harmonised meta-analysis. BMJ 2019, 366, l4570. [Google Scholar] [CrossRef]
- Cunningham, C.; O’ Sullivan, R.; Caserotti, P.; Tully, M.A. Consequences of physical inactivity in older adults: A systematic review of reviews and meta-analyses. Scand. J. Med. Sci. Sports 2020, 30, 816–827. [Google Scholar] [CrossRef] [PubMed]
- Marquez, D.X.; Aguiñaga, S.; Vásquez, P.M.; Conroy, D.E.; Erickson, K.I.; Hillman, C.; Stillman, C.M.; Ballard, R.M.; Sheppard, B.B.; Petruzzello, S.J.; et al. A systematic review of physical activity and quality of life and well-being. Transl. Behav. Med. 2020, 10, 1098–1109. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet. Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Agostino, D.; Daskalopoulou, C.; Wu, Y.-T.; Koukounari, A.; Haro, J.M.; Tyrovolas, S.; Panagiotakos, D.B.; Prince, M.; Prina, A.M. The impact of physical activity on healthy ageing trajectories: Evidence from eight cohort studies. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 92. [Google Scholar] [CrossRef] [PubMed]
- Spiteri, K.; Broom, D.; Bekhet, A.H.; De Caro, J.X.; Laventure, B.; Grafton, K. Barriers and Motivators of Physical Activity Participation in Middle-aged and Older-adults—A Systematic Review. J. Aging Phys. Act. 2019, 27, 929–944. [Google Scholar] [CrossRef]
- Baert, V.; Gorus, E.; Mets, T.; Geerts, C.; Bautmans, I. Motivators and barriers for physical activity in the oldest old: A systematic review. Ageing Res. Rev. 2011, 10, 464–474. [Google Scholar] [CrossRef]
- Franco, M.R.; Tong, A.; Howard, K.; Sherrington, C.; Ferreira, P.H.; Pinto, R.Z.; Ferreira, M.L. Older people’s perspectives on participation in physical activity: A systematic review and thematic synthesis of qualitative literature. Br. J. Sports Med. 2015, 49, 1268–1276. [Google Scholar] [CrossRef] [PubMed]
- Bethancourt, H.J.; Rosenberg, D.E.; Beatty, T.; Arterburn, D.E. Barriers to and facilitators of physical activity program use among older adults. Clin. Med. Res. 2014, 12, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Moschny, A.; Platen, P.; Klaaßen-Mielke, R.; Trampisch, U.; Hinrichs, T. Barriers to physical activity in older adults in Germany: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 121. [Google Scholar] [CrossRef]
- Omelan, A.; Podstawski, R.; Wziatek, B.; Merino-Marbán, R.; Romero-Ramos, O. Physical activity levels of rural and urban seniors in the region of Warmia and Mazury in Poland. Balt. J. Health Phys. Act. 2017, 2017, 74–88. [Google Scholar] [CrossRef]
- Rai, R.; Jongenelis, M.I.; Jackson, B.; Newton, R.U.; Pettigrew, S. Exploring Factors Associated with Physical Activity in Older Adults: An Ecological Approach. J. Aging Phys. Act. 2019, 27, 343–353. [Google Scholar] [CrossRef] [PubMed]
- van Uffelen, J.G.Z.; Khan, A.; Burton, N.W. Gender differences in physical activity motivators and context preferences: A population-based study in people in their sixties. BMC Public Health 2017, 17, 624. [Google Scholar] [CrossRef]
- Adjei, N.K.; Brand, T. Investigating the associations between productive housework activities, sleep hours and self-reported health among elderly men and women in western industrialised countries. BMC Public Health 2018, 18, 110. [Google Scholar] [CrossRef]
- Lee, Y.S. Gender differences in physical activity and walking among older adults. J. Women Aging 2005, 17, 55–70. [Google Scholar] [CrossRef]
- Cabanas-Sánchez, V.; Esteban-Cornejo, I.; Migueles, J.H.; Banegas, J.R.; Graciani, A.; Rodríguez-Artalejo, F.; Martínez-Gómez, D. Twenty four-hour activity cycle in older adults using wrist-worn accelerometers: The seniors-ENRICA-2 study. Scand. J. Med. Sci. Sports 2020, 30, 700–708. [Google Scholar] [CrossRef]
- Stalling, I.; Albrecht, B.M.; Doerwald, F.; Bammann, K. Time allocation to active domains, physical activity, and health indicators in older adults: Cross-sectional results from the OUTDOOR ACTIVE study. BMC Public Health 2020, 20, 1580. [Google Scholar] [CrossRef] [PubMed]
- Ross, R.; Chaput, J.P.; Giangregorio, L.M.; Janssen, I.; Saunders, T.J.; Kho, M.E.; Poitras, V.J.; Tomasone, J.R.; El-Kotob, R.; McLaughlin, E.C.; et al. Canadian 24-Hour Movement Guidelines for Adults aged 18-64 years and Adults aged 65 years or older: An integration of physical activity, sedentary behaviour, and sleep. Appl. Physiol. Nutr. Metab. 2020, 45, S57–S102. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Yang, P.S.; Park, B.E.; Kang, T.S.; Lim, S.H.; Cho, S.; Lee, S.Y.; Chung, Y.H.; Lee, M.Y.; Kim, D.; et al. Association of Light-Intensity Physical Activity with Mortality in the Older Population: A Nationwide Cohort Study. Front. Cardiovasc. Med. 2022, 9, 859277. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Qiang, F. Psychosocial Mediation of Light-Moderate Physical Activity and Cognitive Performance among Adults Aged 60+ in China. Behav. Sci. 2022, 12, 175. [Google Scholar] [CrossRef]
- McMullan, I.I.; Bunting, B.P.; McDonough, S.M.; Tully, M.A.; Casson, K. The association between light intensity physical activity with gait speed in older adults (≥ 50 years). A longitudinal analysis using the English Longitudinal Study of Ageing (ELSA). Aging Clin. Exp. Res. 2020, 32, 2279–2285. [Google Scholar] [CrossRef]
- Rees-Punia, E.; Deubler, E.; Campbell, P.; Gapstur, S.M.; Patel, A. Light-Intensity Physical Activity in a Large Prospective Cohort of Older US Adults: A 21-Year Follow-Up of Mortality. Gerontology 2020, 66, 259–265. [Google Scholar] [CrossRef]
- Welch, W.A.; Strath, S.J.; Brondino, M.; Walker, R.; Swartz, A.M. Duration-Response of Light-Intensity Physical Activity and Glucose Dynamics in Older Adults. J. Phys. Act. Health 2019, 16, 37–42. [Google Scholar] [CrossRef]
- Volders, E.; de Groot, R.H.M.; Bolman, C.A.W.; Lechner, L. The longitudinal associations between change in physical activity and cognitive functioning in older adults with chronic illness (es). BMC Geriatr. 2021, 21, 478. [Google Scholar] [CrossRef] [PubMed]
- Cerin, E.; Leslie, E.; Sugiyama, T.; Owen, N. Perceived barriers to leisure-time physical activity in adults: An ecological perspective. J. Phys. Act. Health 2010, 7, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Gorman, E.; Hanson, H.M.; Yang, P.H.; Khan, K.M.; Liu-Ambrose, T.; Ashe, M.C. Accelerometry analysis of physical activity and sedentary behavior in older adults: A systematic review and data analysis. Eur. Rev. Aging Phys. Act. 2014, 11, 35–49. [Google Scholar] [CrossRef]
- Fernandes, D. A avaliação das aprendizagens no Sistema Educativo Português. Educ. Pesqui. 2007, 33, 581–600. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, P.L. Development of the Portuguese version of MOS SF-36. Part II--Validation tests. Acta Med. Port. 2000, 13, 119–127. [Google Scholar]
- Machado, M.; Tavares, C.; Moniz-Pereira, V.; André, H.; Ramalho, F.; Veloso, A.; Carnide, F. Validation of YPAS-PT—The Yale Physical Activity Survey for Portuguese Older People. Sci. J. Public Health 2016, 4, 72. [Google Scholar] [CrossRef][Green Version]
- Dipietro, L.; Caspersen, C.J.; Ostfeld, A.M.; Nadel, E.R. A survey for assessing physical activity among older adults. Med. Sci. Sports Exerc. 1993, 25, 628–642. [Google Scholar] [CrossRef]
- Young, D.R.; Jee, S.H.; Appel, L.J. A comparison of the Yale Physical Activity Survey with other physical activity measures. Med. Sci. Sports Exerc. 2001, 33, 955–961. [Google Scholar] [CrossRef] [PubMed]
- Booth, M.L.; Bauman, A.; Owen, N. Perceived Barriers to Physical Activity among Older Australians. J. Aging Phys. Act. 2002, 10, 271–280. [Google Scholar] [CrossRef]
- Nascimento, C.M.C.; Gobbi, S.; Sussumu Hirayama, M.; Colim Brazão, M. Nível De Atividade Física E As Principais Barreiras Percebidas Por Idosos De Rio Claro. J. Phys. Educ. 2008, 19, 109–118. [Google Scholar] [CrossRef]
- Sallis, J.F.; Cervero, R.B.; Ascher, W.; Henderson, K.A.; Kraft, M.K.; Kerr, J. An ecological approach to creating active living communities. Annu. Rev. Public Health 2006, 27, 297–322. [Google Scholar] [CrossRef]
- Gjersing, L.; Caplehorn, J.R.; Clausen, T. Cross-cultural adaptation of research instruments: Language, setting, time and statistical considerations. BMC Med. Res. Methodol. 2010, 10, 13. [Google Scholar] [CrossRef]
- Enders, C.K.; Bandalos, D.L. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Struct. Equ. Model. 2001, 8, 430–457. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; Guilford Press: New York, NY, USA, 2016; Description: xvii; 534p. [Google Scholar]
- Byrne, B.M. Structural Equation Modeling with AMOS; Psychology Press: New York, NY, USA, 2000; ISBN 9781410600219. [Google Scholar]
- Hooper, D.; Coughlan, J.; Mullen, M.R. Structural equation modelling: Guidelines for determining model fit. Electron. J. Bus. Res. Methods 2008, 6, 53–60. [Google Scholar]
- European Commission. European Commission Special Eurobarometer 525 for Sport and Physical Activity; European Union: Brussels, Belgium, 2022; ISBN 978-92-76-56432-4. [Google Scholar]
- Arazi, H.; Izadi, M.; Kabirian, H. Interactive effect of socio-eco-demographic characteristics and perceived physical activity barriers on physical activity level among older adults. Eur. Rev. Aging Phys. Act. 2022, 19, 8. [Google Scholar] [CrossRef] [PubMed]
- Guedes-Estevez, E.; Costa, A.R.; Moura-Ferreira, P.; Lunet, N.; Morais, S. Regular physical activity-related awareness and knowledge in Portugal: Results from a population-based survey. Porto Biomed. J. 2021, 6, e130. [Google Scholar] [CrossRef] [PubMed]
- Mathews, A.E.; Laditka, S.B.; Laditka, J.N.; Wilcox, S.; Corwin, S.J.; Liu, R.; Friedman, D.B.; Hunter, R.; Tseng, W.; Logsdon, R.G. Older adults’ perceived physical activity enablers and barriers: A multicultural perspective Mathews A.E. J. Aging Phys. Act. 2010, 18, 119–140. [Google Scholar] [CrossRef] [PubMed]
- Ramsey, K.A.; Zhou, W.; Rojer, A.G.M.; Reijnierse, E.M.; Maier, A.B. Associations of objectively measured physical activity and sedentary behaviour with fall-related outcomes in older adults: A systematic review. Ann. Phys. Rehabil. Med. 2022, 65, 101571. [Google Scholar] [CrossRef]
- Wongsila, S.; Chernbumroong, S.; Sureephong, P. Systematic reviews of elderly exercise barriers. In Proceedings of the 2022 Joint International Conference on Digital Arts, Media and Technology with ECTI Northern Section Conference on Elec-trical, Electronics, Computer and Telecommunications Engineering (ECTI DAMT & NCON), Chiang Rai, Thailand, 26–28 January 2022; pp. 460–462. [Google Scholar]
- Harrison, E.A.; Lord, L.M.; Asongwed, E.; Jackson, P.; Johnson-Largent, T.; Jean Baptiste, A.M.; Harris, B.M.; Jeffery, T. Perceptions, Opinions, Beliefs, and Attitudes About Physical Activity and Exercise in Urban-Community-Residing Older Adults. J. Prim. Care Community Health 2020, 11, 2150132720924137. [Google Scholar] [CrossRef]
- Gray, P.M.; Murphy, M.H.; Gallagher, A.M.; Simpson, E.E.A. Motives and Barriers to Physical Activity Among Older Adults of Different Socioeconomic Status. J. Aging Phys. Act. 2016, 24, 419–429. [Google Scholar] [CrossRef] [PubMed]
- Gobbi, S.; Sebastiao, E.; Papini, C.B.; Nakamura, P.M.; Valdanha Netto, A.; Gobbi, L.T.B.; Kokubun, E. Physical inactivity and related barriers: A study in a community dwelling of older brazilians. J. Aging Res. 2012, 2012, 685190. [Google Scholar] [CrossRef]
- Sjöström, M.; Oja, P.; Hagströmer, M.; Smith, B.J.; Bauman, A. Health-enhancing physical activity across European Union countries: The Eurobarometer study. J. Public Health 2006, 14, 291–300. [Google Scholar] [CrossRef]
- Shinn, C.; Salgado, R.; Rodrigues, D. National programme for promotion of physical activity: The situation in Portugal. Cienc. Saude Coletiva 2020, 25, 1339–1348. [Google Scholar] [CrossRef]
- Rodrigues, V.; Mota-Pinto, A.; De Sousa, B.; Botelho, A.; Alves, C.; De Oliveira, C.R. The aging profile of the Portuguese population: A principal component analysis. J. Community Health 2014, 39, 747–752. [Google Scholar] [CrossRef][Green Version]
- Santos, R.; Nunes, A.; Ribeiro, J.C.; Santos, P.; Duarte, J.A.R.; Mota, J. Obesidade, síndrome metabólica e atividade física: Estudo exploratório realizado com adultos de ambos os sexos, da Ilha de S. Miguel, Região Autônoma dos Açores, Portugal. Rev. Bras. Educ. Física Esporte 2005, 19, 317–328. [Google Scholar] [CrossRef]
- Guerreiro, M.; Pereira, I. Women’s Occupational Patterns and Work-Family Arrangements: Do National and Organisational Policies Matter. In Women, Men, Work and Family in Europe; Springer: Berlin/Heidelberg, Germany, 2007; pp. 190–209. ISBN 978-1-349-54127-0. [Google Scholar]
- Cunha, M.; André, S.; Aparício, G.; Santos, E.; Nunes, C. Organization of housework in heterosexual couples: Systematic review of the literature. Procedia-Social Behav. Sci. 2016, 217, 459–468. [Google Scholar] [CrossRef][Green Version]
- Voicu, M.; Voicu, B.; Strapcova, K. Housework and gender inequality in European countries. Eur. Sociol. Rev. 2009, 25, 365–377. [Google Scholar] [CrossRef]
- Gross, S.M.; Gary, T.L.; Browne, D.C.; LaVeist, T.A. Gender differences in body image and health perceptions among graduating seniors from a historically black college. J. Natl. Med. Assoc. 2005, 97, 1608–1619. [Google Scholar]
- Rhodes, R.E.; Martin, A.D.; Taunton, J.E.; Rhodes, E.C.; Donnelly, M.; Elliot, J. Factors associated with exercise adherence among older adults. An individual perspective. Sport. Med. 1999, 28, 397–411. [Google Scholar] [CrossRef]
- McAuley, E.; Blissmer, B. Self-efficacy determinants and consequences of physical activity. Exerc. Sport Sci. Rev. 2000, 28, 85–88. [Google Scholar] [CrossRef]
- Bunn, F.; Dickinson, A.; Barnett-Page, E.; Mcinnes, E.; Horton, K. A systematic review of older people’s perceptions of facilitators and barriers to participation in falls-prevention interventions. Ageing Soc. 2008, 28, 449–472. [Google Scholar] [CrossRef]
- You, E.; Lautenschlager, N.T.; Wan, C.S.; Goh, A.M.Y.; Curran, E.; Chong, T.W.H.; Anstey, K.J.; Hanna, F.; Ellis, K.A. Ethnic Differences in Barriers and Enablers to Physical Activity Among Older Adults. Front. Public Health 2021, 9, 1309. [Google Scholar] [CrossRef]
- Guthold, R.; Ono, T.; Strong, K.L.; Chatterji, S.; Morabia, A. Worldwide Variability in Physical Inactivity. Am. J. Prev. Med. 2008, 34, 486–494. [Google Scholar] [CrossRef]
- Aoyagi, Y.; Park, H.; Watanabe, E.; Park, S.; Shephard, R.J. Habitual physical activity and physical fitness in older Japanese adults: The nakanojo study. Gerontology 2009, 55, 523–531. [Google Scholar] [CrossRef] [PubMed]
- Mcauley, E.; Szabo, A.; Gothe, N.; Olson, E.A. Self-Efficacy: Implications for Physical Activity, Function, and Functional Limitations in Older Adults. Am. J. Lifestyle Med. 2011, 5, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Jefferis, B.J.; Parsons, T.J.; Sartini, C.; Ash, S.; Lennon, L.T.; Papacosta, O.; Morris, R.W.; Wannamethee, S.G.; Lee, I.M.; Whincup, P.H. Objectively measured physical activity, sedentary behaviour and all-cause mortality in older men: Does volume of activity matter more than pattern of accumulation? Br. J. Sports Med. 2019, 53, 1013–1020. [Google Scholar] [CrossRef]
- Musich, S.; Wang, S.S.; Hawkins, K.; Greame, C. The Frequency and Health Benefits of Physical Activity for Older Adults. Popul. Health Manag. 2017, 20, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Stamatakis, E.; Gale, J.; Bauman, A.; Ekelund, U.; Hamer, M.; Ding, D. Sitting time, physical activity, and risk of mortality in adults. J. Am. Coll. Cardiol. 2019, 73, 2062–2072. [Google Scholar] [CrossRef]
- Compernolle, S.; De Cocker, K.; Cardon, G.; De Bourdeaudhuij, I.; Van Dyck, D. Older Adults’ Perceptions of Sedentary Behavior: A Systematic Review and Thematic Synthesis of Qualitative Studies. Gerontologist 2020, 60, e572–e582. [Google Scholar] [CrossRef]
- Bauman, A.E.; Reis, R.S.; Sallis, J.F.; Wells, J.C.; Loos, R.J.F.; Martin, B.W. Correlates of physical activity: Why are some people physically active and others not? Lancet 2012, 380, 258–271. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).