Abstract
Pay-for-performance (P4P) programs for diabetes care enable the provision of comprehensive and continuous health care to diabetic patients. However, patient outcomes may be affected by the patient’s educational attainment. The present retrospective cohort study aimed to examine the effects of the educational attainment of diabetic patients on participation in a P4P program in Taiwan and the risk of dialysis. The data were obtained from the National Health Insurance Research Database of Taiwan. Patients newly diagnosed with type 2 diabetes mellitus (T2DM) aged 45 years from 2002 to 2015 were enrolled and observed until the end of 2017. The effects of their educational attainment on their participation in a P4P program were examined using the Cox proportional hazards model, while the impact on their risk for dialysis was investigated using the Cox proportional hazards model. The probability of participation in the P4P program was significantly higher in subjects with a junior high school education or above than in those who were illiterate or had only attained an elementary school education. Subjects with higher educational attainment exhibited a lower risk for dialysis. Different educational levels had similar effects on reducing dialysis risk among diabetic participants in the P4P program.
1. Introduction
People today live in greater affluence, but their daily exercise is reduced. As a result, obesity is highly prevalent, and the incidence and prevalence of diabetes are rapidly increasing. According to the statistics of the International Diabetes Federation, there were 463 million people with diabetes worldwide in 2019, and it is estimated that the number of patients will rise to 700 million in 2045, constituting a 51% increase [1]. If diabetic patients do not control their blood glucose well, long-term hyperglycemia will lead to a series of complications, including nephropathy, retinopathy, neuropathy, cerebrovascular diseases, cardiovascular diseases, peripheral vascular diseases, ketoacidosis, hyperosmolar hyperglycemic state, and other problems [2]. Among them, about 30–46% of cases with type 2 diabetes are complicated by chronic kidney diseases; these patients ultimately require dialysis treatment [3]. The medical care burden derived from diabetes and its complications is also massive [4]. Diabetes is a chronic disease with high incidence and high medical costs; however, proper management and care can prevent or delay its complications [5,6]. Dialysis is one of the treatment strategies for end-stage renal disease (ESRD). Diabetic nephropathy is now the leading cause of ESRD in the U.S. [7]. Taiwan has the highest incidence and prevalence of dialysis globally [8], with more than 47% of dialysis cases caused by diabetes complications [9]. As the prevalence of diabetes continues to increase in Taiwan, ESRD has become a serious burden on the national healthcare system [10]. End-stage renal disease causes progressive organ damage elsewhere, leading to premature mortality. The excess mortality associated with type 2 diabetes occurs primarily in patients with chronic kidney disease [11]. Therefore, how to prevent and treat the progression of diabetic nephropathy is an important issue.
“Pay-for-performance” (P4P) is a new medical expense payment system concept aimed at improving medical care compliance through financial incentives; that is, it provides financial incentives to help hospitals and doctors provide a high-quality, low-cost, and holistic medical care model to achieve a specific medical care quality index. Pay-for-performance has been widely used in many developed countries, including the UK Quality and Outcomes Framework (QOF), the Australia Practice Incentives Program (PIP), and Taiwan’s diabetes pay-for-performance program. In Taiwan’s P4P program for diabetes, medical professionals from different disciplines constitute a shared care medical team that provides a complete care model comprising patient diagnosis, examinations, health education, and follow-up. In this system, doctors are rewarded based on the number of patients received and the status of four performance monitoring indicators, that is, the complete patient follow-up rate, which includes at least three scheduled follow-ups per year; the control rate of glycated hemoglobin; and the rate of achieving low-density lipoprotein goals [12]. P4P programs for diabetes provide appropriate care and effective use of medical resources by regularly delivering medical care. While the literature suggests that P4P programs have a limited impact on care quality [13,14], some studies suggest that P4P programs improve some process outcomes and the achievement of hemoglobin A1C, cholesterol, and blood pressure targets [15,16]. P4P programs for diabetes can reduce or delay the occurrence of complications, as well as reduce the number of times and days of hospitalization, thereby effectively controlling medical expenses [12,17,18].
People with relatively lower education are more likely to suffer from diabetes [19]. The prognosis of diabetes is found to be influenced by medical care access and quality for diabetic patients, management of blood biochemical parameters, and healthy patient behavior. The mode of medical care for diabetes has become complex. This has made preventative care more accessible to only the highly educated class of people, who find it easier to adopt appropriate and healthier behaviors [20]. Even in the literature, relatively higher education is positively correlated with better employment, higher income potential, and thus more healthcare opportunities [21]. That is, better-educated patients are less likely to suffer the adverse consequences of the disease, namely dialysis and mortality. Similarly, the research also confirms that, among diabetic patients, those with less education have poorer blood glucose control [22], and those with relatively low health literacy have a higher risk of stroke [23] and mortality [24,25].
While the prognosis of diabetic patients may be influenced by their educational level, patients who participate in pay-for-performance programs can receive medical care, health education, and follow-up treatment provided by professional medical teams. In this case, the subsequent influence of different educational levels on whether patients participate in a pay-for-performance program are worthy of further investigation. However, very few studies have focused on an in-depth analysis of the educational levels of diabetic patients. This study aims to compare the participation rates in a pay-for-performance program among diabetic patients with different educational levels and investigate the difference in dialysis risk among diabetic patients with varying educational levels and participation in the program.
2. Materials and Methods
2.1. Study Subjects
The main research population of this study was patients newly diagnosed with type 2 diabetes from 2002 to 2015. Data from 2000 to 2001 were taken as the washout period for newly diagnosed diabetes. These patients were subject to follow-up until the end of 2017. The study defined diabetic patients as those who had a primary or secondary diagnosis of diabetes in three outpatient visits within 365 consecutive days (ICD9: 250) or one hospitalization record and had taken diabetes-related drugs (the ATC CODE begins with A10) at least once [26,27]. Those who met the following criteria were excluded: (a) gestational diabetes, only those who sought medical care for primary and secondary diagnosis of diabetes within 270 days before delivery (ICD9: 648); (b) type 1 diabetes, defined as those who held a Major Illness/Injury Certificate for diabetes, or who had at least one outpatient diagnosis of insulin-dependent diabetes (250.x1, 250.x3) and one inpatient diagnosis of diabetic ketoacidosis (250.1x), or who had a diagnosis of insulin-dependent diabetes in at least three outpatient visits within 365 consecutive days; (c) patients who had kidney transplantation or dialysis before joining the pay-for-performance program or developing diabetes.
It is reasonably assumed that most people’s educational level does not change much after age 45. Thus, diabetic patients aged 45–100 years were included in the study, although patients with missing values of research variables were excluded. In total, 1,307,963 diabetic patients were included (the selection process for the research subjects is shown in Figure 1).
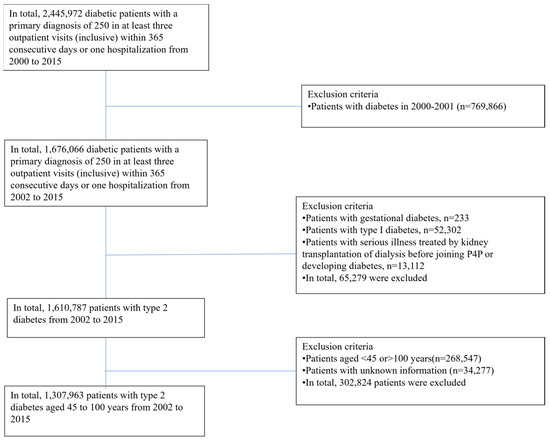
Figure 1.
Research subject selection.
2.2. Data Sources
This is a retrospective cohort study. The data sources included the National Health Insurance Research Database and the Cause of Death File, published from 2000 to 2017, provided by the Ministry of Health and Welfare. Individuals’ educational attainment was obtained from the Household Registration Files issued by the Ministry of the Interior.
2.3. Descriptions of Variables
The independent variable was educational level, which was divided into illiteracy or elementary school, junior high school, senior high school, university, and master’s degree or above, according to the educational level in the household registration document. The dependent variables were participation in the pay-for-performance program for diabetes (“yes” or “no”) and dialysis treatment (“yes” or “no”). Type 2 diabetic patients who had code “E4” in the treatment items in the outpatient medical record or code “C” as the payment category in the inpatient medical service fee calculation list were defined as participating in the program [25]. In this study, whether the patient had undergone dialysis due to chronic renal failure was based on whether dialysis was recorded in the Registry for Catastrophic Illness Patients. The Registry for Catastrophic Illness Patients includes 30 severe illnesses and injuries (e.g., chronic renal failure, malignant tumors, etc.) listed by Taiwan’s National Health Insurance Administration. Therefore, those with dialysis recorded in the Registry for Catastrophic Illness Patients were defined as dialysis patients.
The control variables included patient demographics, financial factors, environmental factors, health status, and healthcare provider characteristics. Patient demographics included gender, age, and marital status. Marital status was divided into unmarried, married, divorced, and widowed. The patient’s financial status was measured by their monthly salary, which was divided into six grades. The patients’ living area environments were divided into seven urbanization grades. Among them, Grade I indicated the highest level of urbanization, and Grade VII indicated the lowest level [28].
Patients’ health status was expressed by Deyo’s Charlson Comorbidity Index (CCI) and diabetes complications severity index (DCSI). The CCI modified by Deyo et al. was adopted, classifying comorbidities into 17 categories. The patients’ codes of primary and secondary diagnoses (ICD-9-CM) were converted into value weight scores to be added up to calculate CCI scores [29]. The severity of diabetic complications (diabetes complications severity index (DCSI)) was calculated by scoring the codes of primary and secondary diagnoses (ICD-9-CM) of the patients according to the presence and severity of complications and then adding the complication score values [2]. The scores of CCI and DCSI were calculated mainly based on the medical records of the research subjects in the first two years before the index date. We defined the starting point of the observation period as the index date. For patients participating in the program, the index date was the time of entering the program. For those not participating, the index date was the date of the new diagnosis of diabetes. Previous studies noted that hypertension and hyperlipidemia aggravate renal function and increase the risk of dialysis [30,31,32,33]. Therefore, “whether having hypertension” and “whether having hyperlipidemia” were added as control variables when investigating “whether having undergone dialysis”.
The characteristics of the healthcare provider were divided into two parts: diabetes treatment physician and diabetes treatment medical institution. The definition of “primary healthcare provider” varied according to whether the research subject participated in the pay-for-performance program. For patients who participated in the program, the primary healthcare providers were the doctors and institutions that helped the patient enter the program. For patients who did not participate, the institutions and doctors that the patient last visited for diabetes treatment as of the observation deadline were the primary healthcare providers. The service volume of the primary treatment physician for diabetes was calculated by the average annual service volume of the primary treatment physician for patients. According to the number of diabetic patients diagnosed and treated by the physician, the service volume of the physician was divided into low service volume (Q1), medium service volume (Q1–Q3), and high service volume (>Q3), according to quartiles for analysis [26]. The departments of primary treatment physicians for diabetes were divided into endocrinology, family medicine, internal medicine, and other departments. The primary diabetes treatment institutions were divided into four levels: medical centers, regional hospitals, local hospitals, and primary clinics. According to ownership, they were divided into public hospitals and non-public hospitals.
2.4. Statistical Analysis
In this study, SAS Version 9.4 (SAS Institute Inc., Cary, NC, USA) statistical software was used to perform descriptive statistics and inferential statistical analysis. All of the tests adopted two-tailed tests, and a p-value less than 0.05 was regarded as statistically significant. First, for descriptive statistics, whether participants participated in the program and whether dialysis occurred were presented by number, percentage, mean, and standard deviation for diabetic patients with different educational levels and control variables (including basic demographics of diabetic patients, financial factors, environmental factors, health status, and characteristics of primary healthcare providers). To explore the influence of educational level on diabetic patients’ participation in the program, a log-rank test was first used to check whether there were statistically significant differences in “whether participating in the pay-for-performance program for diabetes” among different educational levels and other independent variables.
Then, using the Cox proportional hazard model, under the control of patients’ basic demographics, financial factors, environmental factors, health status, and the characteristics of primary healthcare providers, the influence of educational level on diabetic patients’ participation in the program was investigated.
Finally, regarding the difference in the influence of educational level on the occurrence of dialysis in patients participating or not in the program, a log-rank test was used to test whether different educational levels, participation in the program, and other variables had statistical differences in the incidence of dialysis. Univariate Poisson regression was used to test the difference in the number of patients undergoing dialysis per thousand person-years among diabetic patients with different educational levels and other factors. As for whether there was any interaction between educational level and participation status in the P4P program on the risk of dialysis, we first used the Mantel-Haenszel test. Then, we used the Cox proportional hazards model to explore the influence of educational level and whether patients participated in the program on the risk of dialysis. The results are presented as the hazard ratio (HR) with a 95% confidence interval.
3. Results
3.1. Differences in Participation in the Pay-for-Performance Program among Diabetic Patients with Different Educational Levels
The study included 1,307,963 diabetic patients over a 13 year period, of whom 37.04% participated in the pay-for-performance program. Participation rates varied by educational level, as shown in Table 1. Patients with a senior high school education had the highest participation rate (40.24%), while those with an educational level of illiteracy or elementary school had the lowest participation rate (34.72%).

Table 1.
Participation in the pay-for-performance program among type 2 diabetic patients with different educational levels and related factors.
The Cox proportional hazards model was used to explore the differences in participation and related factors, and the study found that patients with a junior high school education or higher were more likely to participate in the program compared to those with an education level of illiteracy or elementary school. Specifically, patients with a senior high school education had a 1.13 times higher probability of participating compared to patients with an education level of illiteracy or elementary school (95% CI: 1.13–1.14). Gender, age, marital status, monthly salary, urbanization degree of residential area, severity of comorbidities, severity of diabetic complications, service volume of the primary treatment physician and department of the physician, and level and ownership type of the primary treatment medical institution also affected participation in the program (p < 0.05). Male gender, higher severity of comorbidities and diabetic complications, primary clinics, higher service volume of the diabetic patient’s attending physician, and the physician being an endocrinologist were associated with a higher probability of participation. Patients aged between 45 and 65 years had a higher probability of participating with increasing age, but those aged over 75 years had a decreasing probability.
3.2. Educational Level Associated with the Dialysis Incidence Rate (Per Thousand Person-Years) of Diabetic Patients Participating and Not Participating in the Pay-for-Performance Program
This study included new patients with type 2 diabetes from 2002 to 2015 as research subjects and followed them up until the end of 2017. The longest observation time period was 16 years, and the average observation time period was 7.6 years. The longest time to join the P4P program was 16 years, and the average time to join the P4P program was 8.8 years. We used univariate Poisson regression to compare the incidence of dialysis among diabetic patients with different educational levels. Table 2 shows that the dialysis rate during the observation period was 1.87%, and the dialysis rate per 1000 person-years was 2.46. The incidence of dialysis among diabetic patients with an educational level of illiteracy or elementary school was 2.79 per 1000 person-years—significantly higher than that among diabetic patients with an educational level of university or above (1.55). The higher the education level, the lower the dialysis rate, with a statistically significant difference (p < 0.05). The dialysis rate among diabetic patients in the program was relatively low, 1.75 per 1000 person-years, which was significantly lower than that among diabetic patients not in the program (the dialysis rate was 3.00 per 1000 person-years).

Table 2.
Educational attainment and related factors associated with the occurrence of dialysis in patients with type 2 diabetes.
3.3. Educational Level Associated with the Risk of Dialysis in Diabetic Patients Participating and Not Participating in the Pay-for-Performance Program
The study used the Cox proportional hazards model to explore the influence of educational level on the risk of dialysis in diabetic patients participating and not participating in the P4P program. After controlling for other variables, the study found that a higher educational level was associated with a lower risk of dialysis in diabetic patients (Figure 2). Compared to illiteracy or elementary school, those with a higher educational level had a lower dialysis risk (Table 3, model A), and the risk was reduced by 43% in those with an educational level of university or master’s degree (HR = 0.57, 95% CI: 0.54–0.60). Participation in the pay-for-performance program was also associated with a lower dialysis risk (HR = 0.71, 95% CI: 0.69–0.73, Table 3). There was no significant difference in the influence of participation on the dialysis status of diabetic patients with different educational levels in terms of the interaction between educational level and whether the patients participated in the program (p > 0.05, Table 3, model B). In addition, male gender, younger age, unmarried patients, lower monthly salary, more severe comorbidities, more severe diabetic complications, no hypertension, no hyperlipidemia, lower service volume of the primary treatment physician, medical centers, and non-public hospitals were all associated with increased dialysis risk in diabetic patients (p < 0.05).
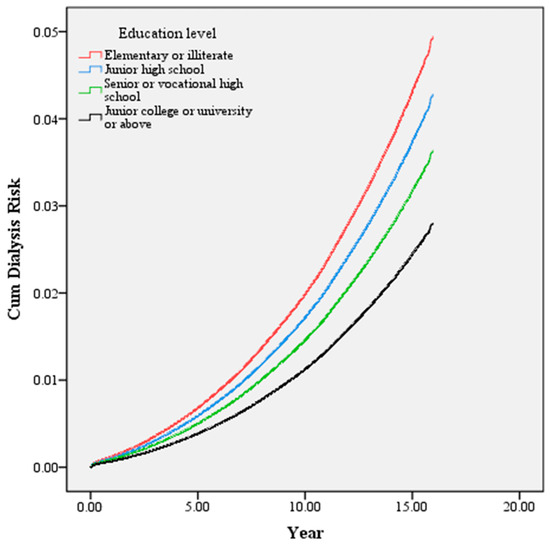
Figure 2.
Educational level associated with the dialysis risk of diabetic patients. Subjects with higher educational attainment exhibited a lower risk for dialysis.

Table 3.
Dialysis risk among type 2 diabetes with different educational attainment participating and not participating in the pay-for-performance program and related factors.
4. Discussion
In our study, 51% of diabetic patients were illiterate or had an elementary level of education. The incidence gap between those with the highest and lowest educational levels varied by age [34]. According to the 2005 National Health Interview Survey of the Health Promotion Administration in Taiwan, the prevalence of diabetes is 18.3% among those who are illiterate, 11.4% among those with an elementary education, 4.8% among those with a junior high school education, 2.5% among those with a senior high school education, and 1.5% among those with a university degree or higher [35]. Compared with those with university degrees and above, people with lower educational levels are significantly more likely to suffer from diabetes. Most patients with diabetes in Taiwan have low education levels. Consequently, this finding is consistent with the previous literature [36,37,38].
This study found that the probability of participating in the program was significantly higher among diabetic patients with an educational level of junior high school, senior high school, or university or above than among those with an educational level of illiteracy or elementary school. At present, there is no research on the influence of educational level on the participation of diabetic patients in pay-for-performance programs. Nevertheless, we found that the higher the education level of a diabetic patient, the higher the participation rate. This may be because the doctors who participate in this program “potentially select” patients, that is, they may prefer those who are most likely to have better communication [39]. Diabetic patients with higher educational levels, for example, have higher health literacy, are easier to communicate with, have a better tendency toward self-care, are more likely to take preventive healthcare measures, and have a better health status [40,41,42,43]. Therefore, doctors tend to prioritize these groups in diabetes programs. Chen et al. and Kontopantelis et al. reported that the older the patient, the less likely a patient is to join such a program [44,45]. The results of this study are consistent with those of previous studies, finding the participation rate among those aged 45–55 years in the pay-for-performance program was the highest and then decreased with increasing age. This may be because fewer research subjects over 60 received a college education at the time in Taiwan. Thus, their educational levels are lower. In addition, the older the patient, the more comorbidities there will be, giving doctors a greater incentive to reverse-select [39]. This could explain why the rate of research subjects over 60 years old participating in the pay-for-performance program was low.
A total of 20–50% of diabetic patients develop diabetic nephropathy [46,47]. It takes an average of about 10–20 years for diabetic patients to develop from the first stage to the fourth stage of diabetic nephropathy and about 25 years to reach end-stage renal disease [48]. If the patient’s hyperglycemia and hypertension have not been properly controlled, the entire process can be shortened to 5 to 10 years. And 7–25% of newly diagnosed diabetic patients also have complications [49,50]. Newly diagnosed diabetes patients with complications have an increased risk of dialysis within 5 years. A previous study showed that 2.7–3.5% of type 2 diabetic patients with nephropathy progress to ESRD every year [51,52].
Research has found that educational level is highly correlated with the effectiveness of care for diabetic patients. The higher the educational level, the more knowledge there is about the disease, and the better the blood glucose control of diabetic patients [53,54]. Brown et al. contend that, among diabetic patients, individuals with lower socioeconomic status (family income, education, and occupation) are more likely to have poor healthcare results [55]. The results of this study showed that the higher the educational level, the lower the dialysis risk for diabetic patients. This result was consistent with the literature [56,57]. It may be that the occurrence and progression of diabetic nephropathy are not only related to the risk factors of hypertension, hyperglycemia, and urinary protein but also related to low medical knowledge of diabetic patients and insufficient access to medical care; those with low educational levels cannot effectively manage diabetes, which becomes a risk factor for diabetic nephropathy and dialysis requirements [58].
The results of this study showed that the diabetic patients participating in the pay-for-performance program had significantly lower dialysis risk. Pay-for-performance programs for diabetes combine multi-functional teams to provide perfect health education and care for diabetic patients. Substantial literature has proven that joining a diabetes pay-for-performance (P4P) program will improve blood sugar and glycated hemoglobin (HbA1c) levels. Hsu and Tai pointed out that diabetes patients who participate in a pay-for-performance program can effectively improve their blood sugar level [59]. Yuan et al. indicated that patients with diabetes who participate in a pay-for-performance program will improve their HbA1c level [60]. Hsieh et al. showed that joining the pay-for-performance program will reduce diabetes complications [18]. The time for joining a P4P program was far longer than in the study mentioned above; therefore, this study found that the participation of diabetic patients in the program prolonged the time it would have taken to enter the stage of terminal renal disease, thus lowering the risk of dialysis significantly compared with non-participants. This result was consistent with the literature [61,62].
In terms of the interaction between educational level and whether the patient participated in the program, the study found that the higher the educational level, the less likely the patient would need dialysis, but there was no statistically significant difference. The influence of educational level on the effectiveness of pay-for-performance (P4P) care can be divided into direct and indirect effects. Direct effects: The complexity of diabetes care (including diet, lifestyle behaviors, and medication) requires the patient’s understanding and cooperation to obtain good care outcomes. Diabetic patients with higher educational levels should better understand the diabetes medical care process and cooperate with treatment. Diabetes pay-for-performance programs comprise multifunctional healthcare teams formed by professional medical personnel, including physicians, nurses, nutritionists, and case managers. It is a complete patient-centered medical care model in which the medical team and patients cooperate with each other to provide extensive and continuous services that cover patient diagnosis, examination, health education, and patient tracking. The complete P4P medical care model will reduce the differential impact of different educational levels on dialysis risk, making the influence of educational level on the risk of dialysis similar for those staying in a P4P program. Indirect effects: Educational level affects health literacy, income, and lifestyle. Diabetic patients with higher educational levels have higher health literacy, better self-care tendencies, are more likely to take preventive health care measures, and have a better health status. Educational attainment affects income, which is essential to maintaining the quality of the complex diabetes care process. Second, low-income patients are more likely to have poor health behaviors such as smoking, physical inactivity, and bad dietary habits, thereby leading to poor outcomes in diabetes care [63]. Third, low-income patients are more likely to have multiple comorbidities and disabilities, resulting in poorer overall health [64]. Kim et al. pointed out that there is a significant interaction between receiving diabetes education courses and the educational level of people with diabetes in achieving optimal glycemic control [65]. Participation in diabetes education classes was positively associated with optimal glycemic control among patients with at least a high school education but negatively associated with optimal glycemic control among those with less than a junior high school education [65]. This is mainly because, although diabetes health education courses can improve nursing care and affect the medical outcomes of diabetes, the cognitive abilities of those receiving health education are different due to their different educational levels. However, our results are inconsistent because varying levels of education reduced the risk of dialysis among those with diabetes to a similar extent under a pay-for-performance program. This may be because P4P programs provide health education, regular follow-ups, and routine physical and biochemical examinations to provide comprehensive care, thus reducing the single impact of patients’ educational levels on health disparity.
Strengths and Limitations
There were some limitations in our study. First, because secondary databases were used in this study, it was impossible to obtain relevant data on all patients (such as BMI, smoking status, and biochemical data such as baseline blood glucose, HbA1c level, urine albumin, and serum creatinine), which may have influenced the subsequent dialysis risk of diabetic patients. However, in this study, the presence of diabetic complications, hypertension, hyperlipidemia, and other variables were used to represent the basic health status of patients so as to reduce bias. Second, this study aimed to show the correlation between the level of education and efficacy rather than the causal relationship between the level of education and efficacy. More data may be needed to explore the causal relationship, such as collecting more detailed information on health knowledge, attitudes, health behaviors, lifestyles, eating habits, etc., through questionnaires. Third, Taiwan’s health insurance system may be different from those of other countries, so the design of the pay-for-performance program may be unique. Therefore, extrapolation of the results of this study to other countries may be limited. To the best of the authors’ knowledge, this is the first study to consider the educational level of diabetic patients and whether the patients participated in a pay-for-performance program. It is also the first to explore the differences in care effectiveness (dialysis) of diabetic patients participating in a pay-for-performance program with different educational levels. Hence, the results of this study deserve more attention. In addition, this study used the National Health Insurance Research Database to represent the national population data, which is widely understood for general medical care use. It also covers a follow-up period of more than 10 years. Thus, the results are representative.
5. Conclusions
This study found that the higher the educational level of diabetic patients, the better their participation status in the pay-for-performance program and the lower their dialysis risk. However, there were similar effects on reducing the dialysis risk when participating in the P4P program. Diabetic patients with lower educational levels had a higher risk of dialysis. Still, if they joined the pay-for-performance program, regardless of their educational level, they could significantly reduce the risk of dialysis, so diabetic patients with lower educational levels should join P4P programs. Lower proportions of diabetic patients with lower educational levels joined the P4P program, so patients with lower educational levels need more attention and care. These results can provide a reference for the clinical health education of diabetic patients and related healthcare policy agencies in formulating policies for diabetes health education and treatment.
Author Contributions
Conceptualization, Y.-S.T., P.-T.K. and W.-C.T.; methodology, W.-C.T.; software, L.-T.C.; validation, P.-T.K. and W.-C.T.; formal analysis, Y.-S.T.; investigation, Y.-S.T.; resources, W.-C.T.; data curation, Y.-S.T., P.-T.K., L.-T.C. and W.-C.T.; writing—original draft preparation, Y.-S.T.; writing—review and editing, Y.-S.T., W.-C.T. and P.-T.K.; visualization, Y.-S.T.; supervision, W.-C.T. and P.-T.K.; project administration, Y.-S.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the Ministry of Science and Technology (MOST108-2410-H-468-017) and Asia University and China Medical University Hospital (CMU112-ASIA-13). The funders had no role in the study design, data collection, analysis, the decision to publish, or the preparation of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Dali JEN-AI Hospital (IRB No.: JAH 108-23).
Informed Consent Statement
Not applicable. Since patient identifications in the National Health Insurance Research Database have been scrambled and de-identified by the Taiwanese government for academic research use, informed consent was waived by the Research Ethics Committee of the Dali JEN-AI Hospital. The research was conducted in accordance with the 1964 Declaration of Helsinki and its amendments and was approved by the institutional review board of the Dali JEN-AI Hospital (IRB No. 108-23), Taiwan.
Data Availability Statement
Data are available from the Health and Welfare Data Science Center of the Ministry of Health and Welfare (MOHW) (https://www.mohw.gov.tw/mp-2.html (accessed on 1 May 2023)), Taiwan. All interested researchers can apply to use the database managed by the MOHW. Due to legal restrictions imposed by the Taiwanese government related to the Personal Information Protection Act, the database cannot be made publicly available. Raw data from the Health and Welfare Data Science Center cannot be obtained. These restrictions prohibit the authors from making the minimal dataset publicly available.
Acknowledgments
We appreciate using the National Health Insurance Research Database provided by the Science Center of the Ministry of Health and Welfare, Taiwan. We are also grateful to the Health Data Science Center, China Medical University Hospital, for providing administrative, technical, and funding support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Williams, R.; Karuranga, S.; Malanda, B.; Saeedi, P.; Basit, A.; Besançon, S.; Bommer, C.; Esteghamati, A.; Ogurtsova, K.; Colagiuri, S.; et al. Global and Regional Estimates and Projections of Diabetes-Related Health Expenditure: Results from the International Diabetes Federation Diabetes Atlas. Diabetes Res. Clin. Pract. 2020, 162, 108072. [Google Scholar] [CrossRef]
- Young, B.A.; Lin, E.; Von Korff, M.; Simon, G.; Ciechanowski, P.; Ludman, E.J.; Everson-Stewart, S.; Kinder, L.; Oliver, M.; Katon, W.J.; et al. Diabetes Complications Severity Index and Risk of Mortality, Hospitalization, and Healthcare Utilization. Am. J. Manag. Care 2008, 14, 15–23. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3810070/ (accessed on 28 October 2013).
- Tien, K.-J.; Lin, Z.-Z.; Chio, C.-C.; Wang, J.-J.; Chu, C.-C.; Sun, Y.-M.; Kan, W.-C.; Chien, C.-C. Epidemiology and Mortality of New-Onset Diabetes after Dialysis: Taiwan National Cohort Study. Diabetes Care 2013, 36, 3027–3032. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020; Centers for Disease Control and Prevention, US Department of Health and Human Services: Atlanta, GA, USA, 2020; pp. 12–15. Available online: https://www.cdc.gov/diabetes/data/statistics-report/coexisting-conditions-complications.html (accessed on 29 June 2022).
- Perkovic, V.; Heerspink, H.L.; Chalmers, J.; Woodward, M.; Jun, M.; Li, Q.; MacMahon, S.; Cooper, M.E.; Hamet, P.; Marre, M.; et al. Intensive Glucose Control Improves Kidney Outcomes in Patients with Type 2 Diabetes. Kidney Int. 2013, 83, 517–523. [Google Scholar] [CrossRef]
- Chang, P.-Y.; Chien, L.-N.; Lin, Y.-F.; Chiou, H.-Y.; Chiu, W.-T. Nonadherence of Oral Antihyperglycemic Medication Will Increase Risk of End-Stage Renal Disease. Medicine 2015, 94, e2051. [Google Scholar] [CrossRef]
- Hoogeveen, E.K. The Epidemiology of Diabetic Kidney Disease. Kidney Dial. 2022, 2, 433–442. [Google Scholar] [CrossRef]
- Saran, R.; Robinson, B.; Abbott, K.C.; Agodoa, L.Y.C.; Bragg-Gresham, J.; Balkrishnan, R.; Bhave, N.; Dietrich, X.; Ding, Z.; Eggers, P.W.; et al. US Renal Data System 2018 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am. J. Kidney Dis. 2019, 73, A7–A8. [Google Scholar] [CrossRef]
- Taiwan Society of Nephrology. 2021 Annual Report on Kidney Disease in Taiwan. Available online: https://www.tsn.org.tw/enVersion/TWRDS.aspx (accessed on 6 April 2021).
- Lai, T.-S.; Hsu, C.-C.; Lin, M.-H.; Wu, V.-C.; Chen, Y.-M. Trends in the Incidence and Prevalence of End-Stage Kidney Disease Requiring Dialysis in Taiwan: 2010–2018. J. Formos. Med. Assoc. 2022, 121, S5–S11. [Google Scholar] [CrossRef]
- Afkarian, M.; Sachs, M.C.; Kestenbaum, B.; Hirsch, I.B.; Tuttle, K.R.; Himmelfarb, J.; De Boer, I.H. Kidney Disease and Increased Mortality Risk in Type 2 Diabetes. J. Am. Soc. Nephrol. 2013, 24, 302–308. [Google Scholar] [CrossRef]
- Chiou, S.-T.; Lin, H.-D.; Yu, N.-C.; Hseuh, H.-K.; Lin, L.-H.; Lin, L.-T.; Chen, T.-J.; Lai, M.-S. An Initial Assessment of the Feasibility and Effectiveness of Implementing Diabetes Shared Care System in Taiwan—Some Experiences from I-Lan County. Diabetes Res. Clin. Pract. 2001, 54, 67–73. [Google Scholar] [CrossRef]
- Ryan, A.M.; Krinsky, S.; Kontopantelis, E.; Doran, T. Long-Term Evidence for the Effect of Pay-for-Performance in Primary Care on Mortality in the UK: A Population Study. Lancet 2016, 388, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Van Herck, P.; De Smedt, D.; Annemans, L.; Remmen, R.; Rosenthal, M.B.; Sermeus, W. Systematic Review: Effects, Design choices, and Context of Pay-for-Performance in Health Care. BMC Health Serv. Res. 2010, 10, 247. [Google Scholar] [CrossRef] [PubMed]
- Oluwatowoju, I.; Abu, E.; Wild, S.H.; Byrne, C.D. Improvements in Glycaemic Control and Cholesterol Concentrations Associated with the Quality and Outcomes Framework: A Regional 2-Year Audit of Diabetes Care in the UK. Diabet. Med. 2010, 27, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Alshamsan, R.; Millett, C.; Majeed, A.; Khunti, K. Has Pay for Performance Improved the Management of Diabetes in the United Kingdom? Prim. Care Diabetes 2010, 4, 73–78. [Google Scholar] [CrossRef]
- Cheng, S.H.; Lee, T.T.; Chen, C.C. A Longitudinal Examination of a Pay-for-Performance Program for Diabetes Care: Evidence from a Natural Experiment. Med. Care 2012, 50, 109–116. [Google Scholar] [CrossRef]
- Hsieh, H.-M.; Lin, T.-H.; Lee, I.-C.; Huang, C.-J.; Shin, S.-J.; Chiu, H.-C. The Association between Participation in a Pay-for-Performance Program and Macrovascular Complications in Patients with Type 2 Diabetes in Taiwan: A Nationwide Population-Based Cohort Study. Prev. Med. 2016, 85, 53–59. [Google Scholar] [CrossRef]
- Choi, A.I.; Weekley, C.C.; Chen, S.-C.; Li, S.; Tamura, M.K.; Norris, K.C.; Shlipak, M.G. Association of Educational Attainment with Chronic Disease and Mortality: The Kidney Early Evaluation Program (KEEP). Am. J. Kidney Dis. 2011, 58, 228–234. [Google Scholar] [CrossRef]
- Hummer, R.A.; Lariscy, J.T. Educational Attainment and Adult Mortality. In International Handbook of Adult Mortality; Springer: Berlin/Heidelberg, Germany, 2011; pp. 241–261. [Google Scholar] [CrossRef]
- Ross, C.E.; Wu, C.-L. The Links between Education and Health. Am. Sociol. Rev. 1995, 60, 719. [Google Scholar] [CrossRef]
- Doshi, T.; Smalls, B.L.; Williams, J.S.; Wolfman, T.E.; Egede, L.E. Socioeconomic Status and Cardiovascular Risk Control in Adults with Diabetes. Am. J. Med. Sci. 2016, 352, 36–44. [Google Scholar] [CrossRef]
- Lai, Y.-J.; Hu, H.-Y.; Lee, Y.-L.; Ku, P.-W.; Yen, Y.-F.; Chu, D. A Retrospective Cohort Study on the Risk of Stroke in Relation to a Priori Health Knowledge Level among People with Type 2 Diabetes Mellitus in Taiwan. BMC Cardiovasc. Disord. 2017, 17, 130. [Google Scholar] [CrossRef]
- Saydah, S.H.; Imperatore, G.; Beckles, G.L. Socioeconomic Status and Mortality: Contribution of Health Care Access and Psychological Distress among Us Adults with Diagnosed Diabetes. Diabetes Care 2012, 36, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Saydah, S.; Lochner, K. Socioeconomic Status and Risk of Diabetes-Related Mortality in the U.S. Public Health Rep. 2010, 125, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.-C.; Kung, P.-T.; Chiu, L.-T.; Liao, Y.P.; Tsai, W.-C. Patients with Diabetes in Pay-for-Performance Programs Have Better Physician Continuity of Care and Survival. Am. J. Manag. Care 2017, 23, e57–e66. [Google Scholar] [PubMed]
- Chang, C.H.; Shau, W.Y.; Jiang, Y.D.; Li, H.Y.; Chang, T.J.; Sheu, W.H.; Kwok, C.F.; Ho, L.T.; Chuang, L.M. Type 2 Diabetes Prevalence and Incidence among Adults in Taiwan during 1999–2004: A National Health Insurance Data Set Study. Diabet. Med. 2010, 27, 636–643. [Google Scholar] [CrossRef]
- Liu, C.Y.; Hung, Y.T.; Chuang, Y.L.; Chen, Y.J.; Weng, W.S.; Liu, J.S.; Liang, K.Y. Incorporating Development Stratification of Taiwan Townships into Sampling Design of Large Scale Health Interview Survey. J. Health Manag. 2006, 4, 1–22. [Google Scholar] [CrossRef]
- Deyo, R.A.; Cherkin, D.C.; Ciol, M.A. Adapting a Clinical Comorbidity Index for Use with ICD-9-cm Administrative Databases. J. Clin. Epidemiol. 1992, 45, 613–619. [Google Scholar] [CrossRef]
- Berthoux, F.; Mohey, H.; Laurent, B.; Mariat, C.; Afiani, A.; Thibaudin, L. Predicting the Risk for Dialysis or Death in IgA Nephropathy. J. Am. Soc. Nephrol. 2011, 22, 752–761. [Google Scholar] [CrossRef]
- Bakris, G.L.; Weir, M.R.; Shanifar, S.; Zhang, Z.; Douglas, J.; van Dijk, D.J.; Brenner, B.M.; RENAAL Study Group. Effects of Blood Pressure Level on Progression of Diabetic Nephropathy: Results from the RENAAL Study. Arch. Intern. Med. 2003, 163, 1555–1565. [Google Scholar] [CrossRef]
- Sandhu, S.; Wiebe, N.; Fried, L.F.; Tonelli, M. Statins for Improving Renal Outcomes: A Meta-Analysis. J. Am. Soc. Nephrol. 2006, 17, 2006. [Google Scholar] [CrossRef]
- Mühlfeld, A.S.; Spencer, M.W.; Hudkins, K.L.; Kirk, E.; Leboeuf, R.C.; Alpers, C.E. Hyperlipidemia Aggravates Renal Disease in B6.ROP Os/+ mice. Kidney Int. 2004, 66, 1393–1402. [Google Scholar] [CrossRef]
- Fleischer, N.L.; Henderson, A.K.; Wu, Y.-H.; Liese, A.D.; McLain, A.C. Disparities in Diabetes by Education and Race/Ethnicity in the U.S., 1973–2012. Am. J. Prev. Med. 2016, 51, 947–957. [Google Scholar] [CrossRef] [PubMed]
- Health Promotion Administration. Diabetes Prevalence. 2017. Available online: https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=1126&pid=1765 (accessed on 24 January 2017).
- Agardh, E.; Allebeck, P.; Hallqvist, J.; Moradi, T.; Sidorchuk, A. Type 2 Diabetes Incidence and Socio-Economic Position: A Systematic Review and Meta-Analysis. Leuk. Res. 2011, 40, 804–818. [Google Scholar] [CrossRef]
- Borrell, L.N.; Dallo, F.J.; White, K. Education and Diabetes in a Racially and Ethnically Diverse Population. Am. J. Public Health 2006, 96, 1637–1642. [Google Scholar] [CrossRef] [PubMed]
- Sacerdote, C.; Ricceri, F.; Rolandsson, O.; Baldi, I.; Chirlaque, M.-D.; Feskens, E.; Bendinelli, B.; Ardanaz, E.; Arriola, L.; Balkau, B.; et al. Lower Educational Level Is a Predictor of Incident Type 2 Diabetes in European Countries: The Epic-Interact Study. Int. J. Epidemiol. 2012, 41, 1162–1173. [Google Scholar] [CrossRef] [PubMed]
- Chang, R.-E.; Lin, S.-P.; Aron, D.C. A Pay-for-Performance Program in Taiwan Improved Care for Some Diabetes Patients, but Doctors May Have Excluded Sicker Ones. Health Aff. 2012, 31, 93–102. [Google Scholar] [CrossRef]
- Do, Y.K.; Eggleston, K.N. Educational Disparities in Quality of Diabetes Care in a Universal Health Insurance System: Evidence from the 2005 Korea National Health and Nutrition Examination Survey. Int. J. Qual. Health Care 2011, 23, 397–404. [Google Scholar] [CrossRef]
- Duong, V.T.; Lin, I.-F.; Sorensen, K.; Pelikan, J.M.; Broucke, S.V.D.; Lin, Y.-C.; Chang, P.W. Health Literacy in Taiwan: A Population-Based Study. Asia Pac. J. Public Health 2015, 27, 871–880. [Google Scholar] [CrossRef]
- Huang, C.-H.; Talley, P.C.; Lin, C.-W.; Huang, R.-Y.; Liu, I.-T.; Chiang, I.-H.; Lu, I.-C.; Lai, Y.-C.; Kuo, K.-M. Factors Associated with Low Health Literacy among Community-Dwelling Women in Taiwan. Women Health 2020, 60, 487–501. [Google Scholar] [CrossRef]
- Wei, M.-H. The Associations between Health Literacy, Reasons for Seeking Health Information, and Information Sources Utilized by Taiwanese Adults. Health Educ. J. 2014, 73, 423–434. [Google Scholar] [CrossRef]
- Chen, T.; Chung, K.; Lin, I.; Lai, M. The Unintended Consequence of Diabetes Mellitus Pay-for-Performance (P4p) Program in Taiwan: Are Patients with More Comorbidities or More Severe Conditions Likely to Be Excluded from the P4p Program? Health Serv. Res. 2011, 46, 47–60. [Google Scholar] [CrossRef]
- Kontopantelis, E.; Springate, D.A.; Ashcroft, D.M.; Valderas, J.M.; van der Veer, S.N.; Reeves, D.; Guthrie, B.; Doran, T. Associations between Exemption and Survival Outcomes in the UK’s Primary Care Pay-for-Performance Programme: A Retrospective Cohort Study. BMJ Qual. Saf. 2016, 25, 657–670. [Google Scholar] [CrossRef] [PubMed]
- Shahbazian, H.; Rezaii, I. Diabetic Kidney Disease; Review of the Current Knowledge. J. Renal Inj. Prev. 2013, 2, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Selby, N.M.; Taal, M.W. An Updated Overview of Diabetic Nephropathy: Diagnosis, Prognosis, Treatment Goals and Latest Guidelines. Diabetes Obes. Metab. 2020, 22, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Roshan, B.; Stanton, R.C. A Story of Microalbuminuria and Diabetic Nephropathy. J. Nephropathol. 2013, 2, 234–240. [Google Scholar] [CrossRef]
- Samsu, N. Diabetic Nephropathy: Challenges in Pathogenesis, Diagnosis, and Treatment. BioMed Res. Int. 2021, 2021, 1–17. [Google Scholar] [CrossRef]
- Shih, H.-M.; Tsai, W.-C.; Wu, P.-Y.; Chiu, L.-T.; Kung, P.-T. Risk of Rapid Progression to Dialysis in Patients with Type 2 Diabetes Mellitus with and without Diabetes-Related Complications at Diagnosis. Sci. Rep. 2023, 13, 1–12. [Google Scholar] [CrossRef]
- So, W.Y.; Kong, A.P.; Ma, R.C.; Ozaki, R.; Szeto, C.C.; Chan, N.N.; Ng, V.; Ho, C.S.; Lam, C.W.; Chow, C.C.; et al. Glomerular Filtration Rate, Cardiorenal End Points, and All-Cause Mortality in Type 2 Diabetic Patients. Diabetes Care 2006, 29, 2046–2052. [Google Scholar] [CrossRef]
- Andrésdóttir, G.; Jensen, M.L.; Carstensen, B.; Parving, H.-H.; Rossing, K.; Hansen, T.W.; Rossing, P. Improved Survival and Renal Prognosis of Patients with Type 2 Diabetes and Nephropathy with Improved Control of Risk Factors. Diabetes Care 2014, 37, 1660–1667. [Google Scholar] [CrossRef]
- Poulimeneas, D.; Grammatikopoulou, M.G.; Bougioukli, V.; Iosifidou, P.; Vasiloglou, M.F.; Gerama, M.-A.; Mitsos, D.; Chrysanthakopoulou, I.; Tsigga, M.; Kazakos, K. Diabetes Knowledge among Greek Type 2 Diabetes Mellitus Patients. Endocrinol. Nutr.(Ed. Impr.) 2016, 63, 320–326. [Google Scholar] [CrossRef]
- Bains, S.S.; Egede, L.E.; Thurston, M.M.; Bourg, C.A.; Phillips, B.B.; Huston, S.A.; Osborn, C.Y.; Pereira, K.; Johnson, C.; Vorderstrasse, A.; et al. Associations Between Health Literacy, Diabetes Knowledge, Self-Care Behaviors, and Glycemic Control in a Low Income Population with Type 2 Diabetes. Diabetes Technol. Ther. 2011, 13, 335–341. [Google Scholar] [CrossRef]
- Brown, A.F.; Ettner, S.L.; Piette, J.; Weinberger, M.; Gregg, E.; Shapiro, M.F.; Karter, A.J.; Safford, M.; Waitzfelder, B.; Prata, P.A.; et al. Socioeconomic Position and Health among Persons with Diabetes Mellitus: A Conceptual Framework and Review of the Literature. Epidemiol. Rev. 2004, 26, 63–77. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.; Liu, J.; Tao, S.; Hong, H.G.; Li, Y.; Fu, P. Associations between Socioeconomic Status and Chronic Kidney Disease: A Meta-Analysis. J. Epidemiol. Community Health 2018, 72, 270–279. [Google Scholar] [CrossRef] [PubMed]
- Tripathy, S.; Cai, X.; Adhikari, A.; Kershaw, K.; Peralta, C.A.; Kramer, H.; Jacobs, D.R.; Gutierrez, O.M.; Carnethon, M.R.; Isakova, T. Association of Educational Attainment with Incidence of Ckd in Young Adults. Kidney Int. Rep. 2020, 5, 2256–2263. [Google Scholar] [CrossRef] [PubMed]
- Duru, O.K.; Middleton, T.; Tewari, M.K.; Norris, K. The Landscape of Diabetic Kidney Disease in the United States. Curr. Diabetes Rep. 2018, 18, 14. [Google Scholar] [CrossRef]
- Hsu, C.-C.; Tai, T.-Y. Long-Term Glycemic Control By a Diabetes Case-Management Program and the Challenges of Diabetes Care in Taiwan. Diabetes Res. Clin. Pract. 2014, 106, S328–S332. [Google Scholar] [CrossRef]
- Yuan, S.-P.; Huang, C.-N.; Liao, H.-C.; Lin, Y.-T.; Wang, Y.-H. Glycemic Control Outcomes by Gender in the Pay-for-Performance System: A Retrospective Database Analysis in Patients with Type 2 Diabetes Mellitus. Int. J. Endocrinol. 2014, 2014, 1–11. [Google Scholar] [CrossRef]
- Liao, P.-J.; Lin, T.-Y.; Wang, T.-C.; Ting, M.-K.; Wu, I.-W.; Huang, H.-T.; Wang, F.-C.; Chang, H.-C.; Hsu, K.-H. Long-Term and Interactive Effects of Pay-for-Performance Interventions among Diabetic Nephropathy Patients at the Early Chronic Kidney Disease Stage. Medicine 2016, 95, e3282. [Google Scholar] [CrossRef]
- Lin, M.-T.; Hsu, C.-N.; Lee, C.-T.; Cheng, S.-H. Effect of a Pay-for-Performance Program on Renal Outcomes among Patients with Early-Stage Chronic Kidney Disease in Taiwan. Int. J. Health Policy Manag. 2021, 11, 1307–1315. [Google Scholar] [CrossRef]
- Dubay, L.C.; Lebrun, L.A. Health, Behavior, and Health Care Disparities: Disentangling the Effects of Income and Race in the United States. Int. J. Health Serv. 2012, 42, 607–625. [Google Scholar] [CrossRef]
- McCall, D.T.; Sauaia, A.; Hamman, R.F.; Reusch, J.E.; Barton, P. Are Low-Income Elderly Patients at Risk for Poor Diabetes Care? Diabetes Care 2004, 27, 1060–1065. [Google Scholar] [CrossRef]
- Kim, S.H. Educational Attainment Moderates the Associations of Diabetes Education with Health Outcomes. Int. J. Nurs. Pract. 2016, 22, 444–450. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).