Abstract
Multimorbidity is defined as the presence of two or more chronic medical conditions in a person, whether physical, mental or long-term infectious diseases. This is especially common in older populations, affecting their quality of life and emotionally impacting their caregivers and family. Technology can allow for monitoring, managing, and motivating older adults in their self-care, as well as supporting their caregivers. However, when several conditions are present at once, it may be necessary to manage several types of technologies, or for technology to manage the interaction between conditions. This work aims to understand and describe the technologies that are used to support the management of multimorbidity for older adults. We conducted a systematic review of ten years of scientific literature from four online databases. We reviewed a corpus of 681 research papers, finally including 25 in our review. The technologies used most frequently by older adults with multimorbidity are mobile applications and websites, and they are mostly focused on communication and connectivity. We then propose opportunities for future research on addressing the challenges in the management of several simultaneous health conditions, potentially creating a better approach than managing each condition as if it were independent.
1. Introduction
The increase in the number of older adults, as well as the percentage of the population they represent, is a societal transformation that has created challenges for countries in various areas, particularly in the provision of health services [1]. Older adults with multimorbidity—the coexistence of two or more chronic health conditions [2]—represent a significant portion of the primary health care population [3,4]. Having multiple chronic conditions is associated with individual adverse outcomes, such as decreased quality of life [5], reduced physical functioning [5,6], and increased re-hospitalization and mortality rates [7]. Multimorbidity affects not only the person, but also their caregivers and family environment [8,9]. Furthermore, multimorbidity presents a challenge for healthcare professionals’ decision-making practices—e.g., a recent review explored technological support for physicians diagnosing patients with multimorbidity, finding computer-based simulation of clinical cases can be efficient in developing clinical reasoning for multimorbidity [10].
Managing multiple health conditions is challenging for patients, e.g., in the understanding and management of their diseases, e.g., attending multiple appointments and managing therapies or medications [11,12]. Patients must handle a large amount of information about each condition and represent their own interests [13], as well as be aware of any potential interactions between their conditions or between their medications. Furthermore, patients with multimorbidity may feel anxiety and distress towards their conditions, and sometimes cope through avoidance [14] so there may be challenging barriers to provide treatment as well as to implement interventions to support them.
Health technology encompasses a wide range of technology use for medicine, including e.g., drug development, telemedicine, and computer vision for medical images. In this paper, we focus on interactive health technologies geared towards an end user, i.e., technologies that enable a user (patient, caregiver, or healthcare professional) to interact with digital health information, supporting information exchange and self-care [15]. These technologies can be used by older adults to facilitate monitoring and management of their health conditions [16]. For example, mobile health technologies can provide patients with personalized and engaging solutions, at a low cost [17].
Interactive health technologies should be designed considering their users’ specific needs and constraints. User-centered design is an approach that involves users in design and development, with the aim of ensuring that their needs regarding technologies are met [15]. However, little emphasis has been placed on technology solutions aimed at older adults [18], especially those with multiple chronic diseases, as most digital solutions aimed at older adults support single-disease management, e.g., diabetes [19] or cardiovascular disease [20]. Recently, one study on the use of health technologies by adults with multimorbidity found that they use these technologies mainly to make medical decisions and communicate with health providers—however, older adults were found to be less likely to use them [21].
Although other systematic literature reviews have been carried out to account for the state of use of interactive health technologies by older adults, these do not focus on multimorbidity, concentrating instead on particular chronic diseases or conditions (e.g., [22,23,24]). However, managing multiple chronic conditions is not the same as managing them individually, as there may be complex inter-relations between the conditions, as well as within their management. We aim to study which interactive health technologies for older adults with multimorbidity have been proposed, to extract insights and lessons that may help guide development of these types of technologies in the future. For this purpose, this work presents a systematic review of the literature regarding technological solutions to address the needs of older adults with multiple chronic conditions. We aim to identify the type, support, and evaluation of technological tools that are used or proposed to support the health management of older adults with multimorbidity. Therefore, our research questions (RQ) are the following: RQ1: Which types of technologies have been developed to support the health management of older adults with multiple health conditions? RQ2: What are the expected health-related outcomes of technological interventions for older adults with multimorbidity? and RQ3: How are technologies for older adults with multiple health conditions evaluated?
2. Systematic Literature Review Methodology
This work is a systematic literature review (SLR) of studies focused on technology for the health management of older adults with multiple chronic conditions. The SLR method involves collecting articles to organize, analyze, and identify the essential gaps to be addressed in future work [25]. Our work follows the systematic review steps of (1) question formulation; (2) locating studies; (3) study selection and evaluation; (4) analysis and synthesis; and (5) reporting and using results [26]. Each of these steps are described below. This work also follows PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [27] to ensure the review is replicable and systematically sound.
2.1. Question Formulation
We first defined the general concepts to formulate the research questions (see Table 1) by using the PICOC method (Population, Intervention, Comparison, Results, Context) [28] The population of interest in this study is older adults. According to the United Nations, older adults are those who are over 60 years old, although other definitions consider older adults to be over 65 [29,30]. The context is multimorbidity, i.e., those who have multiple health conditions. We are interested in studying interventions for the management of multimorbidity using technology, and we are interested in how the effects on health of these technologies are assessed. We did not focus on comparing technologies nor outcomes.

Table 1.
Search keywords aligned to PICOC.
2.2. Locating Studies
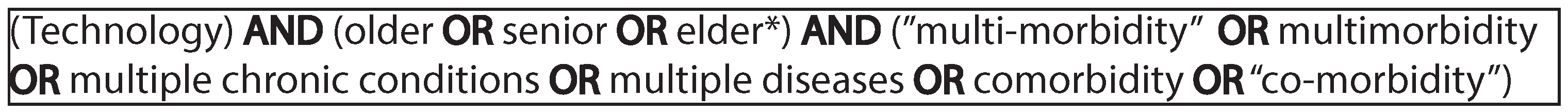
For the search, we considered studies published in ten years (from 2009 to 2019) in the following databases: ACM Digital Library, IEEE Xplore, ScienceDirect, and Pubmed. We believe that combining these four sources provides a comprehensive representation of research on technologies for older adults with multiple chronic conditions, both from a computer science and a health informatics perspective. The terms and synonyms used as the search string (stemming from the PICOC terms in Table 1) are presented in Figure 1. The Boolean operator “OR” is used to select alternative terms and synonyms and the Boolean operator “AND” is used to add terms to the string. We use quotation marks (“ ”) to search for an exact match of compound words. The asterisk operator (*) indicates that there may be more letters after the root word. The search strings were applied to titles and abstracts.
Figure 1.
Search String.
The initial search yielded 681 papers, out of which 161 were duplicate entries, resulting in 520 potential papers. After this step, we applied inclusion and exclusion criteria to further examine which articles were relevant for our search. This step is explained in the next section.
2.3. Study Selection and Evaluation
After obtaining the studies, as part of our study selection and evaluation, inclusion and exclusion criteria were applied to filter out research that was not relevant for our search. For this purpose, we included articles that fulfilled the following eligibility criteria: (1) published in peer-reviewed scientific journals or conferences, (2) written in English, (3) published between 2009 and 2019, (4) presenting technology (implementations, prototypes, or design concepts) specifically proposed for older adults with multiple chronic conditions. Exclusion criteria were as follows: (1) research about technologies aimed at a single chronic condition, (2) publications written in languages other than English, (3) abstracts, summaries, invited plenary sessions, letters to the editor, or reviews, or (4) if the article was not available for download. We did not assess the quality of the selected studies, opting to include all the studies that complied with our inclusion and exclusion criteria.
2.4. Analysis and Synthesis
The data extraction procedure we used has four phases of selection and a final phase of data aggregation. First, we performed an initial search and filtering, for which we used the search strings defined previously, stored the resulting documents in a repository, and removed the duplicates. Second, two authors (GC and VP) read the titles and abstracts of 10 randomly selected papers and applied the inclusion and exclusion criteria. A meeting resolved disagreements about the inclusion and exclusion criteria. After this calibration step, the same authors (GC and VP) read all the titles and abstracts of the selected papers, indicating which studies met these criteria. Articles with two inclusion or exclusion votes were automatically included or excluded. Articles that had one acceptance and one rejection vote were reviewed and resolved by a third reviewer (VH). Third, two authors (GC and VP) read the full text of each of the selected articles. Relevant information was extracted into a Google spreadsheet during this phase. Finally, the extracted data were compared, and disagreements were discussed in an online meeting.
2.5. Reporting and Using Results
The next section presents our results. We answer our three research questions in Section 3.1, Section 3.2 and Section 3.3. Section 4 discusses our findings, limitations, and insights, e.g., regarding opportunities to improve technological support for older adults with multimorbidity. In this way, we provide ways to use our results in future work.
3. Results
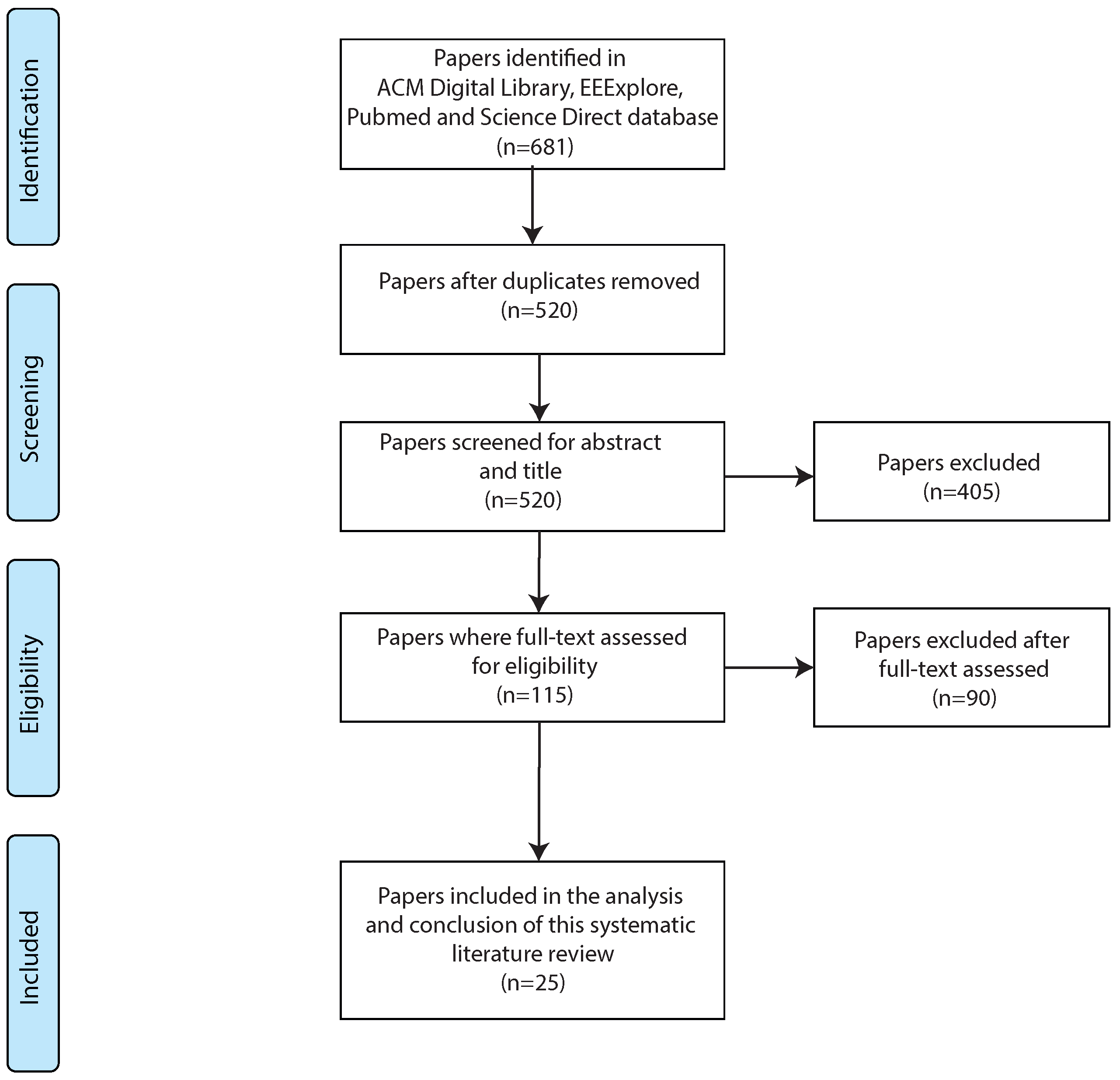
This section presents the results obtained from the systematic literature review. The selection and filtering process is presented in Figure 2. As shown, our initial search yielded a total of 681 items, which became 520 after the duplicates were removed. After reviewing title and abstract to eliminate studies that did not meet the inclusion/exclusion criteria, 405 articles that did not meet the criteria were removed from the corpus. Subsequently, 115 articles were assessed for eligibility through full-text analysis, and finally, 25 publications met the inclusion criteria.
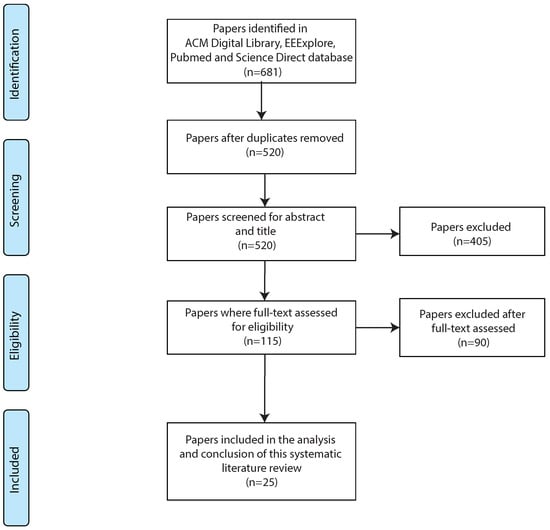
Figure 2.
Flow chart showing study selection.
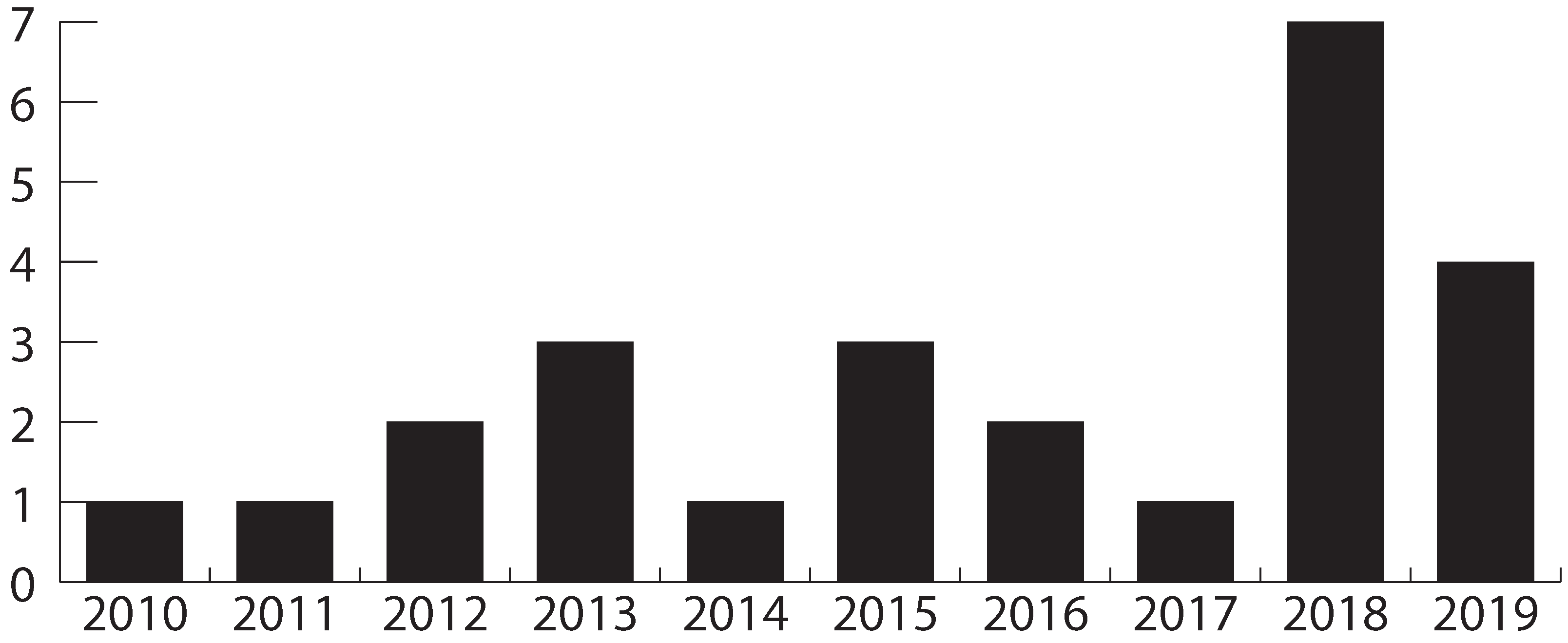
The selected studies were published between 2009 and 2019 (per our search criteria), with 44% of them being published after 2017. Figure 3 shows the distribution of articles published over time. Twelve of the selected articles (12/25, 48%) come from the area of medicine, while seven (7/25, 28%) are from computer science, and the rest (6/25, 24%) are from interdisciplinary work. Journals were the primary type of publication (20/25, 80%), followed by conferences (5/25, 20%). The selected studies are mostly authored by researchers from Europe (12/25, 48%), followed by the United States (11/25, 44%).
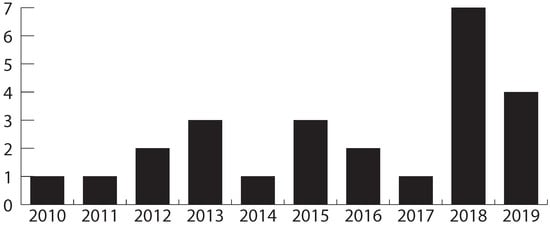
Figure 3.
Frequency of publications per year.
3.1. RQ1: Which Types of Technologies Have Been Developed to Support the Health Management of Older Adults with Multiple Health Conditions?
The types of interactive health technologies mentioned in the literature may be grouped into three categories (see Table 2). First, we have technologies that are based on applications and websites. Some of these technologies have focused on formative and organizational support [31,32], facilitating attendance at appointments [33], integration of care and coordination between health professionals and older adults [34,35,36,37,38], or medication management [39,40,41]. Smartphones, tablets, and computers have been used to implement these systems. This group, which is the most frequently mentioned, focuses on displaying and managing health information. The second group corresponds to wearable sensors; the technology focuses on measuring or detecting information that relates to the physical world, e.g., falls [42], foot movement [43], and biometric parameters [44], as well as teaching behaviors and integrating care into the home [45]. The last group includes devices composed of hand-held and digital parts. These devices focus on cognitive and sensory assistance [41].

Table 2.
Technologies to support health management of older adults with multiple chronic conditions (Y = yes).
In terms of how technology is tailored to support multimorbidity, we found that 8/25 (32.0%) papers presented technologies primarily oriented to the management of a single disease, but were evaluated in a context of older people with multimorbidity. The remaining research (17/25, 68.0%) developed or improved technology to support the management of multiple diseases in older people. These technologies are described in Table 3. For example, a health management system incorporated a social network component called Clinical Wall and the Clinical Decision Support (CDS) system to care for adults with multimorbidity [35], and a medication management application implemented medication information retrieval, doctor visit preparation, and information on when to seek assistance to support adults in reducing medication errors [39].

Table 3.
Technology tailored to multimorbidity (17 studies).
We classified multimorbidity support in five types of areas in which the technology helped or guided older adults (see Table 2). Of the 17 articles with specific support for older adults with multimorbidity, two (2/17, 11.8%) focused on medical records [42,44], six (6/17, 35.3%) on facilitating communication with others [34,35,36,37,38], nine (9/17, 53.0%) examined technology as treatment guides [31,32,33,34,36,38,47,48,50], one (1/17, 5.9%) on providing access to health information (information access) [35] and three (3/17, 17.6%) on guiding medication management [39,40,41]. Two of the articles provided two types of support (communication and information access [35], and communication and treatment [38]). It is important to note that the provided support is not only related to the older adults, as some of the studies also focused on their caregivers (e.g., [38,55]).
Regarding the relationship between the type of technology and the support for multimorbidity, the researchers choose technologies that are appropriate for the intended multimorbidity support. For example, all the communication technologies, i.e., those that aim to help older adults to communicate and obtain information about their health (e.g., videoconferencing applications), are implemented through mobile applications (3/5, 60%) or websites (2/5, 40%), and all of those that aim to update medical records and health data are based on wearable sensors (2/2, 100%).
3.2. RQ2: What Are the Expected Health-Related Outcomes of Technological Interventions for Older Adults with Multimorbidity?
We wanted to know which health improvements or outcomes are the goals of the interventions described in the selected papers. The studies focused primarily on five dimensions of health: (1) physical, (2) mental, (3) social, (4) emotional, and (5) environmental (see Table 4). The largest number of studies referred to improved social interaction (11/25, 44.0%) and mental well-being (11/25, 44.0%); the first aspect refers to communication with family, friends, or medical staff. Mental well-being is especially important for older adults because it can affect health and quality of life. Following is the aim of improving physical aspects, i.e., functional improvements, with nine articles (9/25, 36.0%). Finally, some studies focused on emotional (3/25, 12.0%) and environmental well-being (1/25, 4.0%). Some studies focused on improving more than one health dimension [31,36,39,44,45,48,51,52,53].

Table 4.
Considered aspects of older adults’ health when using technology for multimorbidity support.
Although we aimed to study the effects of the technological interventions on health, the selected papers did not measure this as an outcome, rather focusing on which aspect of health is supported by technology. Therefore, it was not possible to accurately describe health-related effects of the interventions.
3.3. RQ3: How Are Technologies for Older Adults with Multiple Health Conditions Evaluated?
Regarding the assessment methodology used to evaluate the proposed technologies, this review considered three main aspects for the analysis: the methodological approach, the sample size, and the age of the participants (see Table 5).

Table 5.
Methods used to evaluate interventions. Articles [31,44,47] are proposals and therefore were not evaluated.
The observed studies were almost evenly distributed between qualitative (9/25, 36.0%) and quantitative methods (10/25, 40.0%). Three studies used mixed methods (3/25, 12.0%), and three studies (3/25, 12.0%) did not carry out an evaluation, as they were system designs or research proposals.
Regarding study design, only one study was part of a randomized control trial (RCT) [41], while another was initially designed as such but randomization failed and the study was considered to be a prospective cohort study [52]. One study was a pre/post pilot study [32]. Several papers present interview or focus groups studies [33,34,36,37,40,45,50,53], with some also including co-design workshops or participatory design [39,49,51], with the goal of understanding some experience—e.g., how older adults perceive care and case management [34], how care navigation is experienced [33], the self-management of medication [40]—or with the goal of understanding usability and interface preferences, e.g., [36]. Other studies share the latter aim but employ surveys and questionnaires, e.g., the Technology Acceptance Model (TAM) [35], as well as others [43,46,48,54,55]. The final two studies used data from system use or testing to understand system effectiveness [38,42]. Therefore, most studies are not experiments nor quasi experiments, but rather evaluations of technology or explorations of user needs or experiences.
Almost all of the studies that had participants used non-probability sampling (18/22, 81.8%). The only exceptions were the RCT [41], the prospective cohort study which used a modified randomization due to a breach in its implementation [52], and one study which used stratified probability sampling [36]. One study did not provide enough information about the sampling method, only specifying that it was a complex sampling design [48]. The composition of the sample of participants is directly related to the focus of each study, i.e., some only include older adults as the final user and others also include e.g., caregivers or healthcare professionals. Four of the studies [35,38,42,51] address the development of technology for older adults, but they do not explicitly state the age of the participants.
The number of participants varied between one small study with less than 10 participants 0–9 (1/25, 4.0%), to medium-sized studies with 10–49 participants (11/25, 44.0%), and larger studies with 50–99 (2/25, 8.0%), and over 100 (8/25, 32.0%) participants. There was no clear correlation between study size and methodology. The averages of population age in the reviewed articles are the following: 60–69 years (4/25, 16%), 70–79 years (9/25, 36%), and 80–90 years (2/25, 8.0%). However, some did include participants who were not older adults, e.g., in one study the inclusion criteria was vascular surgery patients over 18, even though the average age of participants was over 70, and the youngest participant was 41.
4. Discussion
4.1. Literature Review Overview
The aim of this work was to study which interactive health technologies for older adults with multimorbidity have been proposed, how their outcomes are measured and how they are evaluated. With this aim, we conducted a systematic literature review of four computer science and medical databases, obtaining 681 papers, out of which 25 studies were analyzed in this review. We found evidence of the use of a variety of technologies; spanning from applications and websites, to wearable sensors and devices. These interventions have been used to support multimorbidity through facilitating communication, updating medical records, providing treatment guides and access to health information, and enabling medication management.
The reviewed studies aimed at supporting the physical, mental, emotional, social and environmental health of their users. This holistic focus that includes mental health is relevant due to the link between the mental health of older adults and mortality [56], and also because previous studies that have shown that people with multimorbidity are more likely to suffer from depression and anxiety, which can further exacerbate their physical conditions [57].
Taking into consideration the aging of society in general, and the accompanying cultural transformation, there should be an increasing trend of new technologies being designed, adapted, and oriented mainly for older adults [18]. During the last two years of reviewed papers—2018 and 2019—there seems to be a slightly increasing trend in research regarding technologies for multimorbidity (while in 2020 the COVID-19 pandemic began and research interests may have shifted). An upward trend in research on other technologies for older adults—e.g., home health monitoring systems—has been noted [58].
There are multiple challenges to multimorbidity that make self-management difficult for patients, e.g., the compound effects of conditions and medications, the burden of medications, and difficulties in communicating with healthcare providers, among others [59]. However, most healthcare processes still treat patients as though they had a single disease and ignore these complex interactions [3]. Our study found evidence of this, as 8/25 of the interventions were created for a single disease, even if they were evaluated in a context of multimorbidity.
Recent studies have proposed self-management guidelines for patients e.g., establishing disease and treatment burden and the support patients need to manage their conditions, establishing priorities of importance, setting up medication support and care plans, among others [60]. We wanted to find evidence of how interactive health technologies could specifically focus on the challenges of multimorbidity; and we found efforts tending to integrate information for older adults (see Table 3), which is a step in the right direction when dealing with the complex, fragmented information from several chronic conditions.
4.2. Limitations
Some limitations should be taken into account when evaluating the results of this work. We include only papers written in the English language that have been published between 2009 and 2019. Only ACM digital library, IEEExplore, Science direct, and Pubmed sources have been searched; other relevant material may exist in other databases, e.g., PsycINFO. Furthermore, our choice of keywords may have restricted our findings—e.g., the word “technology” was used to represent all types of interactive health technologies, while previous research may have used words such as “digital solutions”, “mhealth”, or directly named a technology.
As a limitation of our study, it should also be taken into account that most of the included studies come from the United States and Europe (consequently, the participants are from those countries). When designing systems, cultural aspects need to be taken into consideration, and in this regard research found in this study is overwhelmingly from the Global North; while the reality of access to and adoption of technology in the Global South may not be represented through these results. Therefore, generalization to other populations should be made with caution and more research is needed to account for and design health technology to support the needs of older adults with multimorbidity in the Global South.
Finally, we did not assess the quality of the selected studies and did not compare the effectiveness of the technologies, as not enough data was available for this purpose. This makes it difficult to provide solid recommendations regarding the best technologies for older adults with multimorbidity. It is important for future studies to provide clear data on the effectiveness of the proposed interventions. In this regard, we found only one RCT within our selected papers. To truly understand the effectiveness of proposed interventions, further experimental work is needed.
4.3. Requirements and Challenges for Interactive Health Technologies for Multimorbidity
From this work, we derive four requirements, or challenges, that are present in research on interactive technologies for older adults with multimorbidity: increasing integration, improving ubiquity, personalization, and older adult-centered design. We believe these are relevant as insights that should be taken into account by future researchers. Each is described below.
4.3.1. Increasing Integration
Some of the challenges of multimorbidity stem from managing several illnesses, each with their medication, healthcare team, and related information. The proposed systems in this review usually aim for one part of the integration—e.g., they integrate medication management for several illnesses, or they provide communication with the healthcare team, or they gather data to update medical records, but they do not cover all types of support simultaneously (see Table 2). An integrated system that centralizes all information, and ideally also integrates with healthcare providers’ systems, can provide patients with a rich overview of their health as well as better support their needs.
4.3.2. Improving Ubiquity
The technologies found in the reviewed papers range from mobile and web applications to tangible devices and wearable sensors. Although these solutions cover a range of technologies, special consideration should be given to making the management of multimorbidity an ubiquitous and pervasive technology, i.e., made to disappear into everyday routines effortlessly. This does not necessarily mean making technologies invisible, which could make users forget to use them or hinder adoption, but rather, incorporating them into existing practices so they are naturally part of users’ lives. Examples of such interventions are fall detection systems, or smart medication boxes; however, multimorbidity can add extra challenges (e.g., in detecting medicine interactions) and careful consideration should be given to this aspect when designing interactive technologies for these users.
4.3.3. Personalization
Often, patients are treated by healthcare providers as though they had a single disease, only focusing on that provider’s specific discipline. However, multimorbidity means that patients may have unique combinations of chronic illnesses and therefore unique—and often conflicting [61]—needs. Some existing approaches aim to provide personalized care (e.g., [31]), which is especially relevant in a multimorbidity setting.
4.3.4. Older Adult-Centered Design
Previous research has found that many older adults have positive attitudes towards technology and high levels of digital skills [62], but the barriers of adoption may present a challenge to some of them [45]. Older adults are a heterogeneous population with differing technological skills and interests; e.g., older internet users differ in their knowledge of the web, and skills vary both within and between age groups [63]. In order to design and implement health technologies for older adults, especially adults with multimorbidity, it is necessary to look beyond age range considerations and take into account individual differences in technological literacy, cognitive abilities, and physical limitations.
5. Conclusions
The number of older adults will continue to increase in the coming years, as will multiple chronic diseases. The design, implementation, and evaluation of technological tools aimed at older adults with multiple chronic diseases is required to enable this population to remain independent and maintain a good quality of life. Although slightly increasing in recent years, the development of technologies for older patients with multimorbidity remains low. We present a discussion of how technologies for multimorbidity should be designed in the future, to be personalized, ubiquitous, older-adult-centered, and integrated. This review highlights the importance of generating technologies that are directly focused on older adults’ needs.
Author Contributions
Conceptualization, R.F.C., N.V., F.J.F. and V.H.; methodology, G.C. and V.H.; investigation, G.C., V.P. and V.H.; resources, R.F.C., N.V., F.J.F. and V.H.; writing—original draft preparation, G.C., V.H. and V.P.; writing—review and editing, R.F.C., N.V., F.J.F. and V.H.; supervision, V.H.; funding acquisition, R.F.C., N.V., F.J.F. and V.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by ANID—Millennium Science Initiative Program ICS2019_024; National Center for Artificial Intelligence CENIA FB210017, Basal ANID; ANID—Fondecyt 1211210, ANID—PIA ACT210083, Vicerrectoría de Investigación de la Pontificia Universidad Católica de Chile, Concurso de Investigación Interdisciplinaria Convocatoria 2018—II180013.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| SLR | Systematic Literature Review |
| RQ | Research Question |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PICOC | Population, Intervention, Comparisons, Results, Context |
| CDS | Clinical Decision Support |
References
- Sanderson, W.C.; Scherbov, S.; Gerland, P. Probabilistic population aging. PLoS ONE 2017, 12, e0179171. [Google Scholar] [CrossRef] [PubMed]
- Fortin, M.; Soubhi, H.; Hudon, C.; Bayliss, E.A.; Van den Akker, M. Multimorbidity’s many challenges. BMJ 2007, 334, 1016–1017. [Google Scholar] [CrossRef] [PubMed]
- Fortin, M.; Bravo, G.; Hudon, C.; Vanasse, A.; Lapointe, L. Prevalence of multimorbidity among adults seen in family practice. Ann. Fam. Med. 2005, 3, 223–228. [Google Scholar] [CrossRef]
- Lochner, K.A.; Goodman, R.A.; Posner, S.; Parekh, A. Multiple chronic conditions among Medicare beneficiaries: State-level variations in prevalence, utilization, and cost, 2011. Medicare Medicaid Res. Rev. 2013, 3, mmrr.003.03.b02. [Google Scholar] [CrossRef]
- Williams, J.S.; Egede, L.E. The association between multimorbidity and quality of life, health status and functional disability. Am. J. Med. Sci. 2016, 352, 45–52. [Google Scholar] [CrossRef]
- Ryan, A.; Wallace, E.; O’Hara, P.; Smith, S.M. Multimorbidity and functional decline in community-dwelling adults: A systematic review. Health Qual. Life Outcomes 2015, 13, 168. [Google Scholar] [PubMed]
- Wei, M.Y.; Mukamal, K.J. Multimorbidity, mortality, and long-term physical functioning in 3 prospective cohorts of community-dwelling adults. Am. J. Epidemiol. 2018, 187, 103–112. [Google Scholar]
- Townsend, A.; Hunt, K.; Wyke, S. Managing multiple morbidity in mid-life: A qualitative study of attitudes to drug use. BMJ 2003, 327, 837. [Google Scholar] [CrossRef]
- Ploeg, J.; Matthew-Maich, N.; Fraser, K.; Dufour, S.; McAiney, C.; Kaasalainen, S.; Markle-Reid, M.; Upshur, R.; Cleghorn, L.; Emili, A. Managing multiple chronic conditions in the community: A Canadian qualitative study of the experiences of older adults, family caregivers and healthcare providers. BMC Geriatr. 2017, 17, 40. [Google Scholar]
- Consorti, F.; Borcea, M.C.; Laca, A.; Melcarne, R.; Scorziello, C.; Ventrone, L.; Giacomelli, L. Education of clinical reasoning in patients with multimorbidity: A scoping review and perspectives for technology-enhanced learning. Front. Educ. 2023, 8, 1202360. [Google Scholar] [CrossRef]
- Gallacher, K.; May, C.R.; Montori, V.M.; Mair, F.S. Understanding patients’ experiences of treatment burden in chronic heart failure using normalization process theory. Ann. Fam. Med. 2011, 9, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Morrison, R.S. Research priorities in geriatric palliative care: An introduction to a new series. J. Palliat. Med. 2013, 16, 726–729. [Google Scholar] [CrossRef] [PubMed]
- Zulman, D.M.; Jenchura, E.C.; Cohen, D.M.; Lewis, E.T.; Houston, T.K.; Asch, S.M. How can eHealth technology address challenges related to multimorbidity? Perspectives from patients with multiple chronic conditions. J. Gen. Intern. Med. 2015, 30, 1063–1070. [Google Scholar] [CrossRef] [PubMed]
- Moran, O.; Doyle, J.; Smith, S.; Giggins, O.; Dinsmore, J. Investigating the needs and concerns of older adults with multimorbidity and their healthcare professionals for conceivable digital psychotherapeutic interventions. Digit. Health 2022, 8, 20552076221089097. [Google Scholar] [CrossRef]
- Dabbs, A.D.V.; Myers, B.A.; Mc Curry, K.R.; Dunbar-Jacob, J.; Hawkins, R.P.; Begey, A.; Dew, M.A. User-centered design and interactive health technologies for patients. Comput. Inform. Nurs. CIN 2009, 27, 175. [Google Scholar] [CrossRef]
- Tam, L.T.; Valera, A.C.; Tan, H.P.; Koh, C. Online detection of behavioral change using unobtrusive eldercare monitoring system. In Proceedings of the 11th International Conference on Queueing Theory and Network Applications, Wellington, New Zealand, 13–15 December 2016; pp. 1–8. [Google Scholar]
- Steinhubl, S.R.; Muse, E.D.; Topol, E.J. Can Mobile Health Technologies Transform Health Care? JAMA 2013, 310, 2395–2396. [Google Scholar] [CrossRef]
- Stellefson, M.; Chaney, B.; Barry, A.E.; Chavarria, E.; Tennant, B.; Walsh-Childers, K.; Sriram, P.; Zagora, J. Web 2.0 chronic disease self-management for older adults: A systematic review. J. Med. Internet Res. 2013, 15, e35. [Google Scholar] [CrossRef]
- Whitlock, L.A.; McLaughlin, A.C.; Harris, M.; Bradshaw, J. The design of mobile technology to support diabetes self-management in older adults. In Human Aspects of IT for the Aged Population; Design for Everyday Life; Lecture Notes in Computer Science; Springer: Berlin/Heidelberg, Germany, 2015; Volume 9194, pp. 211–221. [Google Scholar]
- Searcy, R.P.; Summapund, J.; Estrin, D.; Pollak, J.P.; Schoenthaler, A.; Troxel, A.B.; Dodson, J.A. Mobile health technologies for older adults with cardiovascular disease: Current evidence and future directions. Curr. Geriatr. Rep. 2019, 8, 31–42. [Google Scholar] [CrossRef]
- Manning, S.E.; Wang, H.; Dwibedi, N.; Shen, C.; Wiener, R.C.; Findley, P.A.; Mitra, S.; Sambamoorthi, U. Association of multimorbidity with the use of health information technology. Digit. Health 2023, 9, 20552076231163797. [Google Scholar] [CrossRef]
- Matthew-Maich, N.; Harris, L.; Ploeg, J.; Markle-Reid, M.; Valaitis, R.; Ibrahim, S.; Gafni, A.; Isaacs, S. Designing, implementing, and evaluating mobile health technologies for managing chronic conditions in older adults: A scoping review. JMIR mHealth uHealth 2016, 4, e29. [Google Scholar] [CrossRef]
- Kim, B.Y.; Lee, J. Smart devices for older adults managing chronic disease: A scoping review. JMIR mHealth uHealth 2017, 5, e69. [Google Scholar] [CrossRef] [PubMed]
- Wildenbos, G.A.; Peute, L.; Jaspers, M. Aging barriers influencing mobile health usability for older adults: A literature based framework (MOLD-US). Int. J. Med. Inform. 2018, 114, 66–75. [Google Scholar] [CrossRef]
- Kitchenham, B.; Charters, S. Guidelines for Performing Systematic Literature Reviews in Software Engineering. Technical Report EBSE 2007-001, Keele University and Durham University Joint Report. 2007. Available online: https://www.elsevier.com/__data/promis_misc/525444systematicreviewsguide.pdf (accessed on 1 September 2023).
- Denyer, D.; Tranfield, D. Producing a systematic review. In The Sage Handbook of Organizational Research Methods; Sage Publications Ltd.: Thousand Oaks, CA, USA, 2009. [Google Scholar]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [PubMed]
- Huang, K.C.; Chiang, I.J.; Xiao, F.; Liao, C.C.; Liu, C.C.H.; Wong, J.M. PICO element detection in medical text without metadata: Are first sentences enough? J. Biomed. Inform. 2013, 46, 940–946. [Google Scholar] [CrossRef] [PubMed]
- Kot, S.; Kurkiewicz, J. The new measures of the population ageing. Stud. Demogr. 2004, 2, 17–29. [Google Scholar]
- World Health Organization. Definition of an Older or Elderly Person; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- Burnette, R.; Simmons, L.A.; Snyderman, R. Personalized health care as a pathway for the adoption of genomic medicine. J. Pers. Med. 2012, 2, 232–240. [Google Scholar] [CrossRef]
- Fortuna, K.L.; DiMilia, P.R.; Lohman, M.C.; Bruce, M.L.; Zubritsky, C.D.; Halaby, M.R.; Walker, R.M.; Brooks, J.M.; Bartels, S.J. Feasibility, acceptability, and preliminary effectiveness of a peer-delivered and technology supported self-management intervention for older adults with serious mental illness. Psychiatr. Q. 2018, 89, 293–305. [Google Scholar] [CrossRef]
- Vos, J.; Gerling, K.; Linehan, C.; Siriwardena, A.N.; Windle, K. Understanding care navigation by older adults with multimorbidity: Mixed-methods study using social network and framework analyses. JMIR Aging 2018, 1, e11054. [Google Scholar] [CrossRef]
- Schmidt, S.; Behrens, J.; Lautenschlaeger, C.; Gaertner, B.; Luderer, C. Experiences with combined personal-online case management and the self-reliance of older people with multimorbidity living alone in private households: Results of an interpretative-hermeneutical analysis. Scand. J. Caring Sci. 2019, 33, 931–939. [Google Scholar] [CrossRef]
- Martínez-García, A.; Moreno-Conde, A.; Jódar-Sánchez, F.; Leal, S.; Parra, C. Sharing clinical decisions for multimorbidity case management using social network and open-source tools. J. Biomed. Inform. 2013, 46, 977–984. [Google Scholar] [CrossRef]
- Portz, J.D.; Bayliss, E.A.; Bull, S.; Boxer, R.S.; Bekelman, D.B.; Gleason, K.; Czaja, S. Using the technology acceptance model to explore user experience, intent to use, and use behavior of a patient portal among older adults with multiple chronic conditions: Descriptive qualitative study. J. Med. Internet Res. 2019, 21, e11604. [Google Scholar] [CrossRef] [PubMed]
- Berner, J.; Anderberg, P.; Rennemark, M.; Berglund, J. Case management for frail older adults through tablet computers and Skype. Inform. Health Soc. Care 2016, 41, 405–416. [Google Scholar] [CrossRef] [PubMed]
- de Jong, C.C.; Ros, W.J.; van Leeuwen, M.; Schrijvers, G. How professionals share an E-care plan for the elderly in primary care: Evaluating the use of an E-communication tool by different combinations of professionals. J. Med. Internet Res. 2016, 18, e304. [Google Scholar] [CrossRef]
- Siek, K.A.; Ross, S.E.; Khan, D.U.; Haverhals, L.M.; Cali, S.R.; Meyers, J. Colorado Care Tablet: The design of an interoperable Personal Health Application to help older adults with multimorbidity manage their medications. J. Biomed. Inform. 2010, 43, S22–S26. [Google Scholar] [CrossRef]
- Haverhals, L.M.; Lee, C.A.; Siek, K.A.; Darr, C.A.; Linnebur, S.A.; Ruscin, J.M.; Ross, S.E. Older adults with multi-morbidity: Medication management processes and design implications for personal health applications. J. Med. Internet Res. 2011, 13, e44. [Google Scholar] [CrossRef] [PubMed]
- Reeder, B.; Demiris, G.; Marek, K.D. Older adults’ satisfaction with a medication dispensing device in home care. Inform. Health Soc. Care 2013, 38, 211–222. [Google Scholar] [CrossRef] [PubMed]
- Mertens, M.; Raepsaet, J.; Mondelaers, M.; Vanrumste, B.; Davis, J. Use of wearable technology to quantify fall risk in psychogeriatric environments: A feasability study. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 3187–3190. [Google Scholar]
- Tchalla, A.E.; Lachal, F.; Cardinaud, N.; Saulnier, I.; Bhalla, D.; Roquejoffre, A.; Rialle, V.; Preux, P.M.; Dantoine, T. Efficacy of simple home-based technologies combined with a monitoring assistive center in decreasing falls in a frail elderly population (results of the Esoppe study). Arch. Gerontol. Geriatr. 2012, 55, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Pires, G.; Correia, P.; Jorge, D.; Mendes, D.; Gomes, N.; Dias, P.; Ferreira, P.; Lopes, A.; Manso, A.; Almeida, L.; et al. VITASENIOR-MT: A telehealth solution for the elderly focused on the interaction with TV. In Proceedings of the 2018 IEEE 20th International Conference on e-Health Networking, Applications and Services (Healthcom), Ostrava, Czech Republic, 17–20 September 2018; pp. 1–6. [Google Scholar]
- Murphy, E.; Doyle, J.; Hannigan, C.; Smith, S.; Kuiper, J.; Jacobs, A.; Hoogerwerf, E.J.; Desideri, L.; Fiordelmondo, V.; Maluccelli, L.; et al. Perceptions and Use of Technology to Support Older Adults with Multimorbidity. In Proceedings of the AAATE Conference, Sheffield, UK, 11–15 September 2017; pp. 160–167. [Google Scholar]
- Mangin, D.; Parascandalo, J.; Khudoyarova, O.; Agarwal, G.; Bismah, V.; Orr, S. Multimorbidity, eHealth and implications for equity: A cross-sectional survey of patient perspectives on eHealth. BMJ Open 2019, 9, e023731. [Google Scholar] [CrossRef] [PubMed]
- Bousquet, J.; Agache, I.; Aliberti, M.; Angles, R.; Annesi-Maesano, I.; Anto, J.; Arnavielhe, S.; Asayag, E.; Bacci, E.; Bedbrook, A.; et al. Transfer of innovation on allergic rhinitis and asthma multimorbidity in the elderly (MACVIA-ARIA)-EIP on AHA Twinning Reference Site (GARD research demonstration project). Allergy 2018, 73, 77–92. [Google Scholar] [CrossRef]
- Levine, D.M.; Lipsitz, S.R.; Linder, J.A. Changes in everyday and digital health technology use among seniors in declining health. J. Gerontol. Ser. A 2018, 73, 552–559. [Google Scholar] [CrossRef]
- Doyle, J.; Murphy, E.; Hannigan, C.; Smith, S.; Bettencourt-Silva, J.; Dinsmore, J. Designing Digital Goal Support Systems for Multimorbidity Self-Management: Insights from Older Adults and their Care Network. In Proceedings of the 12th EAI International Conference on Pervasive Computing Technologies for Healthcare, New York, NY, USA, 21–24 May 2018; pp. 168–177. [Google Scholar]
- Barron, J.S.; Finkelstein, J. Feasibility of providing personalized health information to older adults and their caregivers. In Proceedings of the 2013 IEEE Point-of-Care Healthcare Technologies (PHT), Bangalore, India, 16–18 January 2013; pp. 232–235. [Google Scholar]
- Greenhalgh, T.; Procter, R.; Wherton, J.; Sugarhood, P.; Hinder, S.; Rouncefield, M. What is quality in assisted living technology? The ARCHIE framework for effective telehealth and telecare services. BMC Med. 2015, 13, 91. [Google Scholar] [CrossRef] [PubMed]
- Valdivieso, B.; García-Sempere, A.; Sanfélix-Gimeno, G.; Faubel, R.; Librero, J.; Soriano, E.; Peiró, S.; GeChronic Group. The effect of telehealth, telephone support or usual care on quality of life, mortality and healthcare utilization in elderly high-risk patients with multiple chronic conditions. A prospective study. Med. Clin. 2018, 151, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Ancker, J.S.; Witteman, H.O.; Hafeez, B.; Provencher, T.; Van de Graaf, M.; Wei, E. “You get reminded you’re a sick person”: Personal data tracking and patients with multiple chronic conditions. J. Med. Internet Res. 2015, 17, e202. [Google Scholar] [CrossRef] [PubMed]
- Tseng, M.H.; Wu, H.C. A cloud medication safety support system using QR code and Web services for elderly outpatients. Technol. Health Care 2014, 22, 99–113. [Google Scholar] [CrossRef] [PubMed]
- Wiseman, J.T.; Fernandes-Taylor, S.; Barnes, M.L.; Tomsejova, A.; Saunders, R.S.; Kent, K.C. Conceptualizing smartphone use in outpatient wound assessment: Patients’ and caregivers’ willingness to use technology. J. Surg. Res. 2015, 198, 245–251. [Google Scholar] [CrossRef]
- Schulz, R.; Beach, S.R.; Ives, D.G.; Martire, L.M.; Ariyo, A.A.; Kop, W.J. Association between depression and mortality in older adults: The Cardiovascular Health Study. Arch. Intern. Med. 2000, 160, 1761–1768. [Google Scholar] [CrossRef]
- Bayliss, E.A.; Bonds, D.E.; Boyd, C.M.; Davis, M.M.; Finke, B.; Fox, M.H.; Glasgow, R.E.; Goodman, R.A.; Heurtin-Roberts, S.; Lachenmayr, S.; et al. Understanding the context of health for persons with multiple chronic conditions: Moving from what is the matter to what matters. Ann. Fam. Med. 2014, 12, 260–269. [Google Scholar] [CrossRef]
- Liu, L.; Stroulia, E.; Nikolaidis, I.; Miguel-Cruz, A.; Rios Rincon, A. Smart homes and home health monitoring technologies for older adults: A systematic review. Int. J. Med. Inform. 2016, 91, 44–59. [Google Scholar] [CrossRef]
- Bayliss, E.A.; Steiner, J.F.; Fernald, D.H.; Crane, L.A.; Main, D.S. Descriptions of barriers to self-care by persons with comorbid chronic diseases. Ann. Fam. Med. 2003, 1, 15–21. [Google Scholar] [CrossRef]
- Muth, C.; Blom, J.; Smith, S.; Johnell, K.; Gonzalez-Gonzalez, A.I.; Nguyen, T.S.; Brueckle, M.S.; Cesari, M.; Tinetti, M.; Valderas, J. Evidence supporting the best clinical management of patients with multimorbidity and polypharmacy: A systematic guideline review and expert consensus. J. Intern. Med. 2019, 285, 272–288. [Google Scholar] [CrossRef]
- Caldeira, C.; Gui, X.; Reynolds, T.L.; Bietz, M.; Chen, Y. Managing healthcare conflicts when living with multiple chronic conditions. Int. J. Hum.-Comput. Stud. 2021, 145, 102494. [Google Scholar] [CrossRef]
- Mitzner, T.L.; Boron, J.B.; Fausset, C.B.; Adams, A.E.; Charness, N.; Czaja, S.J.; Dijkstra, K.; Fisk, A.D.; Rogers, W.A.; Sharit, J. Older adults talk technology: Technology usage and attitudes. Comput. Hum. Behav. 2010, 26, 1710–1721. [Google Scholar] [CrossRef] [PubMed]
- Hargittai, E.; Piper, A.M.; Morris, M.R. From internet access to internet skills: Digital inequality among older adults. Univers. Access Inf. Soc. 2019, 18, 881–890. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).