Trauma Quality Improvement Program: A Retrospective Analysis from A Middle Eastern National Trauma Center
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Study Design
2.2. Existing Model (TQIP)
2.3. Inclusion Criteria
2.4. Exclusion Criteria
2.5. Variable Selection/Primary Outcome
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- de Ramirez, S.S.; Hyder, A.A.; Herbert, H.K.; Stevens, K. Unintentional injuries: Magnitude, prevention, and control. Annu. Rev. Public Health 2012, 33, 175–191. [Google Scholar] [CrossRef] [PubMed]
- CDC. Center for Disease Control and Prevention (CDC). Injury Prevention and Control Homepage. Available online: https://www.cdc.gov/injury/index.html (accessed on 15 June 2022).
- World Health Organization. Global Health Estimates: Leading Causes of Death. Available online: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death (accessed on 14 July 2022).
- MacKenzie, E.J.; Rivara, F.P.; Jurkovich, G.J.; Nathens, A.B.; Frey, K.P.; Egleston, B.L.; Salkever, D.S.; Scharfstein, D.O. A national evaluation of the effect of trauma-center care on mortality. N. Engl. J. Med. 2006, 354, 366–378. [Google Scholar] [CrossRef]
- Pracht, E.E.; Langland-Orban, B.; Flint, L. Survival advantage for elderly trauma patients treated in a designated trauma center. J. Trauma 2011, 71, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Mullins, R.J.; Veum-Stone, J.; Helfand, M.; Zimmer-Gembeck, M.; Hedges, J.R.; Southard, P.A.; Trunkey, D.D. Outcome of hospitalized injured patients after institution of a trauma system in an urban area. JAMA 1994, 271, 1919–1924. [Google Scholar] [CrossRef] [PubMed]
- Tinkoff, G.H.; Reed, J.F., 3rd; Megargel, R.; Alexander, E.L., 3rd; Murphy, S.; Jones, M.S. Delaware’s inclusive trauma system: Impact on mortality. J. Trauma 2010, 69, 245–252. [Google Scholar] [CrossRef]
- Hemmila, M.R.; Cain-Nielsen, A.H.; Jakubus, J.L.; Mikhail, J.N.; Dimick, J.B. Association of Hospital Participation in a Regional Trauma Quality Improvement Collaborative With Patient Outcomes. JAMA Surg. 2018, 153, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Hemmila, M.R.; Jakubus, J.L. Trauma Quality Improvement. Crit. Care Clin. 2017, 33, 193–212. [Google Scholar] [CrossRef]
- Hemmila, M.R.; Nathens, A.B.; Shafi, S.; Calland, J.F.; Clark, D.E.; Cryer, H.G.; Goble, S.; Hoeft, C.J.; Meredith, J.W.; Neal, M.L.; et al. The Trauma Quality Improvement Program: Pilot study and initial demonstration of feasibility. J. Trauma 2010, 68, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Shafi, S.; Nathens, A.B.; Cryer, H.G.; Hemmila, M.R.; Pasquale, M.D.; Clark, D.E.; Neal, M.; Goble, S.; Meredith, J.W.; Fildes, J.J. The Trauma Quality Improvement Program of the American College of Surgeons Committee on Trauma. J. Am. Coll. Surg. 2009, 209, 521–530.e1. [Google Scholar] [CrossRef]
- Trooskin, S.Z.; Copes, W.S.; Bain, L.W.; Peitzman, A.B.; Cooney, R.N.; Jubelirer, R.A. Variability in trauma center outcomes for patients with moderate intracranial injury. J. Trauma 2004, 57, 998–1005. [Google Scholar] [CrossRef]
- Shafi, S.; Nathens, A.B.; Parks, J.; Cryer, H.M.; Fildes, J.J.; Gentilello, L.M. Trauma quality improvement using risk-adjusted outcomes. J. Trauma 2008, 64, 599–604, discussion 604-6. [Google Scholar] [CrossRef] [PubMed]
- Cudnik, M.T.; Sayre, M.R.; Hiestand, B.; Steinberg, S.M. Are all trauma centers created equally? A statewide analysis. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2010, 17, 701–708. [Google Scholar] [CrossRef]
- Al-Thani, H.; El-Menyar, A.; Asim, M.; Mollazehi, M.; Abdelrahman, H.; Parchani, A.; Consunji, R.; Castle, N.; Ellabib, M.; Al-Hassani, A.; et al. Evolution of The Qatar Trauma System: The Journey from Inception to Verification. J. Emergencies Trauma Shock. 2019, 12, 209–217. [Google Scholar]
- El-Menyar, A.; Mekkodathil, A.; Asim, M.; Consunji, R.; Strandvik, G.; Peralta, R.; Rizoli, S.; Abdelrahman, H.; Mollazehi, M.; Parchani, A.; et al. Maturation process and international accreditation of trauma system in a rapidly developing country. PLoS ONE 2020, 15, e0243658. [Google Scholar] [CrossRef] [PubMed]
- Blackmore, A.R.; Leonard, J.; Madayag, R.; Bourg, P.W. Using the Trauma Quality Improvement Program Metrics Data to Enhance Clinical Practice. J. Trauma Nurs. Off. J. Soc. Trauma Nurses 2019, 26, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Heaney, J.B.; Guidry, C.; Simms, E.; Turney, J.; Meade, P.; Hunt, J.P.; McSwain, N.E., Jr.; Duchesne, J.C. To TQIP or not to TQIP? That is the question. Am. Surg. 2014, 80, 386–390. [Google Scholar] [CrossRef]
- Heaney, J.B.; Schroll, R.; Turney, J.; Stuke, L.; Marr, A.B.; Greiffenstein, P.; Robledo, R.; Theriot, A.; Duchesne, J.; Hunt, J. Implications of the Trauma Quality Improvement Project inclusion of nonsurvivable injuries in performance benchmarking. J. Trauma Acute Care Surg. 2017, 83, 617–621. [Google Scholar] [CrossRef]
- Henry, R.; Ghafil, C.; Piccinini, A.; Liasidis, P.K.; Matsushima, K.; Golden, A.; Lewis, M.; Inaba, K.; Strumwasser, A. Extracorporeal support for trauma: A trauma quality improvement project (TQIP) analysis in patients with acute respiratory distress syndrome. Am. J. Emerg. Med. 2021, 48, 170–176. [Google Scholar] [CrossRef]
- Demetriades, D.; Martin, M.; Salim, A.; Rhee, P.; Brown, C.; Doucet, J.; Chan, L. Relationship between American College of Surgeons trauma center designation and mortality in patients with severe trauma (injury severity score >15). J. Am. Coll. Surg. 2006, 202, 212–215. [Google Scholar] [CrossRef]
- Newgard, C.D.; Fildes, J.J.; Wu, L.; Hemmila, M.R.; Burd, R.S.; Neal, M.; Mann, N.C.; Shafi, S.; Clark, D.E.; Goble, S.; et al. Methodology and analytic rationale for the American College of Surgeons Trauma Quality Improvement Program. J. Am. Coll. Surg. 2013, 216, 147-57. [Google Scholar] [CrossRef]
- Denson, K.; Morgan, D.; Cunningham, R.; Nigliazzo, A.; Brackett, D.; Lane, M.; Smith, B.; Albrecht, R. Incidence of venous thromboembolism in patients with traumatic brain injury. Am. J. Surg. 2007, 193, 380–383, discussion 383-4. [Google Scholar] [CrossRef] [PubMed]
- American College of Surgeons. ACS TQIP Best Practices in the Management of Traumatic Brain Injury In 2015 ed. Chicago, 2015. Available online: https://www.facs.org/media/mkej5u3b/tbi_guidelines.pdf (accessed on 27 June 2022).
- Scudday, T.; Brasel, K.; Webb, T.; Codner, P.; Somberg, L.; Weigelt, J.; Herrmann, D.; Peppard, W. Safety and efficacy of prophylactic anticoagulation in patients with traumatic brain injury. J. Am. Coll. Surg. 2011, 213, 148–153, discussion 153-4. [Google Scholar] [CrossRef] [PubMed]
- Rappold, J.F.; Sheppard, F.R.; Carmichael Ii, S.P.; Cuschieri, J.; Ley, E.; Rangel, E.; Seshadri, A.J.; Michetti, C.P. Venous thromboembolism prophylaxis in the trauma intensive care unit: An American Association for the Surgery of Trauma Critical Care Committee Clinical Consensus Document. Trauma Surg. Acute Care Open 2021, 6, e000643. [Google Scholar] [CrossRef]
- Arabian, S.S.; Marcus, M.; Captain, K.; Pomphrey, M.; Breeze, J.; Wolfe, J.; Bugaev, N.; Rabinovici, R. Variability in interhospital trauma data coding and scoring: A challenge to the accuracy of aggregated trauma registries. J. Trauma Acute Care Surg. 2015, 79, 359–363. [Google Scholar] [CrossRef] [PubMed]

| TQIP Cohorts | Definitions |
|---|---|
| Blunt Multisystem Injuries |
|
| Penetrating Injuries |
|
| Hemorrhagic Shock |
|
| Severe Traumatic Brain Injury (TBI) |
|
| Elderly Patients |
|
| Elderly Blunt Multisystem Injury |
|
| Elderly Patients with Isolated Hip Fractures |
|
| Shock |
|
| TQIP Outcome Definitions | |
| Major Hospital Events | At least one of the following 13 hospital events defined in the NTDS data dictionary:
|
| Mortality | One of the following discharge dispositions:
|
| Major Hospital Events Including Death | Meet the outcome criteria for major hospital events/hospital arrival |
| Fall 2020 (April 2019–March 2020) | Fall 2021 (April 2020–March 2021) | |||
|---|---|---|---|---|
| Variables | All TQIP Centers | HTC TQIP Cohort | All TQIP Centers | HTC TQIP Cohort |
| Total No. of Patients; n (%) | 325,102 (88.0%) | 904 (98.8%) | 349,080 (87.9%) | 871 (98.5%) |
| Age (yrs.) | 55 ** | 37 ± 13 * | 53.7 ± 22.1 | 37.7 ± 14.1 * |
| Gender; n (%) | ||||
| Male | 208,065 (64.0%) | 830 (91.8) * | 228,997 (65.6%) | 818 (94.0%) * |
| Female | 117,037 (36.0%) | 74 (8.2) * | 120,083 (34.4%) | 53 (6.0%) * |
| Elderly (≥65 yrs) | 122,732 (37.7%) | 46 (5.0) * | 123,076 (35.2%) | 50 (5.74%) * |
| Race/Ethnicity; n (%) | ||||
| White | 244,152 (75.1%) | 289 (32.0) * | 254,479 (72.9%) | 274 (31.5%) * |
| Black | 464,891 (14.3%) | 63 (7) * | 57,934 (16.6%) | 71 (8.2%) * |
| Asian | 7477 (2.3%) | 551 (61.0) * | 6981 (2.0%) | 523 (60.0%) * |
| Others | 23,732 (7.3%) | 1 (0.1) * | 26,181 (7.5%) | 23 (0.3%) * |
| Unknown | 11,053 (3.4%) | (0.0) * | 12,567 (3.6%) | 1 (0.1%) * |
| Mechanism of Injury; n (%) | ||||
| Blunt | 46,997 (14.4%) | 170 (18.8) * | 52,136 (14.9%) | 173 (19.9%) * |
| Penetrating | 15,354 (4.7%) | 20 (3.3) * | 19,738 (5.7%) | 22 (2.5%) * |
| Mode of Injury; n (%) | ||||
| Fall | 151,172 (46.5%) | 298 (33) * | 155,340 (44.5%) | 282 (32.4%) * |
| MVT Occupant and Other | 71,847 (22.1%) | 295 (32.6%) * | 76,791 (22.0%) | 261 (30.0%) * |
| MVT Motorcyclist | 18,856 (5.8%) | 37 (4.1%) | 21,294 (6.1%) | 67 (7.7%) |
| Pedestrian | 23,732 (7.3%) | 125 (13.8%) * | 24,436 (7.0%) | 94 (10.8%) * |
| Struck by/Against | 15,605 (4.8%) | 66 (7.3%) * | 15,359 (4.4%) | 85 (9.8%) * |
| Firearm | 20,481 (6.3%) | 4 (0.4%) * | 28,973 (8.3%) | 1 (0.1%) * |
| Cut/Pierce | 8778 (2.7%) | 24 (2.7%) | 9774 (2.8%) | 28 (3.2%) |
| Others | 14,630 (4.5%) | 55 (6.1%) | 17,105 (4.9%) | 52 (6.0%) |
| Fall 2020 | Fall 2021 | |||
|---|---|---|---|---|
| Variables | All TQIP Centers | HTC TQIP Cohort | All TQIP Centers | HTC TQIP Cohort |
| Pre-Existing Comorbidities | N (%) | N (%) | N (%) | N (%) |
| Hypertension | 125,489 (38.6%) | 96 (10.6%) * | 129,159 (37.0%) | 98 (11.3%) * |
| Smoking | 74,123 (22.8%) | 63 (7.0%) * | 7086 (2.03%) | 36 (4.13%) * |
| Dementia/Mental Disorder | 53,317 (16.4%) | 8 (0.9%) * | 59,692 (17.1%) | 13 (1.4%) * |
| Diabetes Mellitus | 50,391 (15.5%) | 98 (10.8%) * | 52,013 (14.9%) | 94 (10.8%) * |
| COPD | 23,407 (7.2%) | 0 (0.0%) * | 23,737 (6.8%) | 1 (0.1%) * |
| Alcohol Use Disorder | 214,506 (6.6%) | 6 (0.6%) * | 82,034 (23.5%) | 58 (6.7%) * |
| Congestive Heart Failure | 14,304 (4.4%) | 0 (0.0%) * | 15,359 (4.4%) | 1 (0.1%) * |
| Cerebrovascular Accident | 9428 (2.9%) | 3 (0.3%) * | 9425 (2.7%) | 3 (0.3%) * |
| Chronic Renal Failure | 5852 (1.8%) | 4 (0.4%) * | 5934 (1.7%) | 5 (0.5%) * |
| Cirrhosis | 4551 (1.4%) | 1 (0.1%) * | 4887 (1.4%) | 4 (0.5%) * |
| Myocardial Infraction | 2276 (0.7%) | 0 (0.0%) * | 2095 (0.6%) | 1 (0.1%) * |
| Disseminated Cancer | 2094 (0.6%) | 3 (0.3%) | 2094 (0.6%) | 3 (0.3%) |
| Acute Respiratory Distress syndrome | 1626 (0.5%) | 4 (0.4%) | 1396 (0.4%) | 4 (0.5%) |
| Fall 2020 | Fall 2021 | |||
|---|---|---|---|---|
| Variables | All TQIP Centers | HTC TQIP Cohort | All TQIP Centers | HTC TQIP Cohort |
| Complications | N (%) | N (%) | N (%) | N (%) |
| Acute Kidney Injury | 2563 (0.8%) | 4 (0.4%) | 3141 (0.9%) | 6 (0.7%) |
| Pressure Ulcer | 2242 (0.7%) | 5 (0.5%) | 2793 (0.8%) | 3 (0.3%) |
| Deep vein Thrombosis | 3524 (1.1%) | 4 (0.4%) | 3839 (1.1%) | 2 (0.2%) * |
| Pulmonary Embolism | 1602 (0.5%) | 10 (1.1%) * | 2094 (0.6%) | 10 (1.1%) * |
| Catheter-Associated Urinary Tract Infection | 961 (0.3%) | 7 (0.8%) * | 1047 (0.3%) | 7 (0.8%) * |
| Ventilator-Associated Pneumonia | 2563 (0.8%) | 15 (1.7%) * | 2793 (0.8%) | 29 (3.3%) * |
| Severe Sepsis | 1281 (0.4%) | 2 (0.2%) | 1745 (0.5%) | 2 (0.2%) |
| Superficial Incisional Surgical Site Infection | 641 (0.2%) | 13 (1.4%) * | 698 (0.2%) | 10 (1.1%) * |
| Deep Surgical Site infection | 641 (0.2%) | 1 (0.1%) | 698 (0.2%) | 4 (0.5%) |
| Central Line Bloodstream Infection (CLABSI) | 320 (0.1%) | 5 (0.5%) * | 349 (0.1%) | 9 (1.0%) * |
| Fall 2020 | Fall 2021 | |||
|---|---|---|---|---|
| Variables | All TQIP Centers | HTC TQIP Cohort | All TQIP Centers | HTC TQIP Cohort |
| Hemorrhagic Shock | N (%) | N (%) | N (%) | N (%) |
| Number of Patients (%) | 7766 (2.4%) | 28 (3.1%) | 9003 (2.6%) | 35 (4.01%) * |
| PRBC Transfusion within 24 h | 7700 (99.1%) | 28 (100%) | 8479 (94.1%) | 35 (4.01%) * |
| Plasma Transfusion within 24 h | 5571 (71.7%) | 7 (25%) * | 6184 (68.6%) | 14 (40%) |
| Platelets Transfusion within 24 h | 3322 (42.7%) | 8 (28.6%) | 3397 (37.7%) | 12 (34.2%) |
| Surgery for Hemorrhagic Control | 4066 (52.3%) | 11 (39.2%) | 4745 (52.8%) | 19 (54.3%) * |
| Angiography for Hemorrhagic Shock | 1327 (17.1%) | 5 (17.8%) | 1457 (16.2%) | 10 (28.6%) * |
| Pharmacologic VTE Prophylaxis | 217,794 (66.9%) | 739 (81.7%) * | 241,147 (71.8%) | 734 (86.4%) * |
| Time to VTE Prophylaxis, Median (IQR) | 2 (2–3) | 2 (2–3) | 2 (2–3) | 2 (2–3) |
| Unfractionated Heparin | 48,870 (20.1%) | 3 (0.3%) * | 47,005 (19.5%) | 4 (0.4%) * |
| Low-Molecular-Weight Heparin | 164,697 (75.6%) | 732 (99.1%) * | 184,626 (76.6%) | 727 (99.0%) * |
| Fall 2020 | Fall 2021 | |||
|---|---|---|---|---|
| Variables | All TQIP Centers | HTC TQIP Cohort | All TQIP Centers | HTC TQIP Cohort |
| Injury Severity | N (%) | N (%) | N (%) | N (%) |
| Total GCS ≤ 8 | 37,062 (11.4%) | 108 (12%) | 40,144 (11.5%) | 122 (14%) * |
| Injury Severity Score (ISS), Median (IQR) | 14 (10–19) | 14 (10–20) | 14 (10–19) | 14 (10–21) |
| Midline Shift TBI | 17,454 (5%) | 41 (4.7%) | 17,454 (5%) | 41 (4.7%) |
| Shock (SBP < 90 mm Hg) | 13,869 (4.3%) | 60 (6.6%) * | 15,564 (3.9%) | 56 (6.3%) * |
| Severe TBI (AIS ≥ 3 and GCS 3–8) | 23,772 (7.3%) | 87 (9.6%) * | 26,480 (6.7%) | 92 (10.4%) * |
| Pre-Hospital Cardiac Arrest | 4226 (1.3%) | 19 (2.1%) * | 4887 (1.4%) | 21 (2.4%) * |
| Outcome Variables | ||||
| Hospital Length of Stay, Median (IQR) | 5 (3–9) | 8 (5–14) * | 5 (3–9) | 8 (4–16) * |
| Patients with ICU Care (disposition) | 159,295 (49.0%) | 475 (52.5%) * | 163,020 (46.7%) | 486 (55.9%) * |
| ICU Length of Stay, Median (IQR) | 3 (2–6) | 5 (3–8) * | 3 (2–6) | 5 (3–9) * |
| Patients with Mechanical Ventilation | 62,094 (19.1%) | 190 (21%) | 67,372 (19.3%) | 202 (23.2%) * |
| Ventilatory Days, Median (IQR) | 3 (2–8) | 4 (2–9) | 3 (2–8) | 5 (2–11) * |
| Death within 72 h. | 10,382 (43.3%) | 0 (0%) * | 166,511 (47.7%) | 158 (18.2%) * |
| Death After 30 Days | 623 (2.6%) | 3 (8.3%) * | 8378 (2.4%) | 2 (0.2%) * |
| Time to Death, Median (IQR) Days | 4 (2–9) | 7 (4.5–10.5) * | 4 (2–9) | 7 (5–8) * |
| Overall Mortality | 23,977 (7.4%) | 36 (3.9%) * | 27,577 (7.9%) | 31 (3.6%) * |
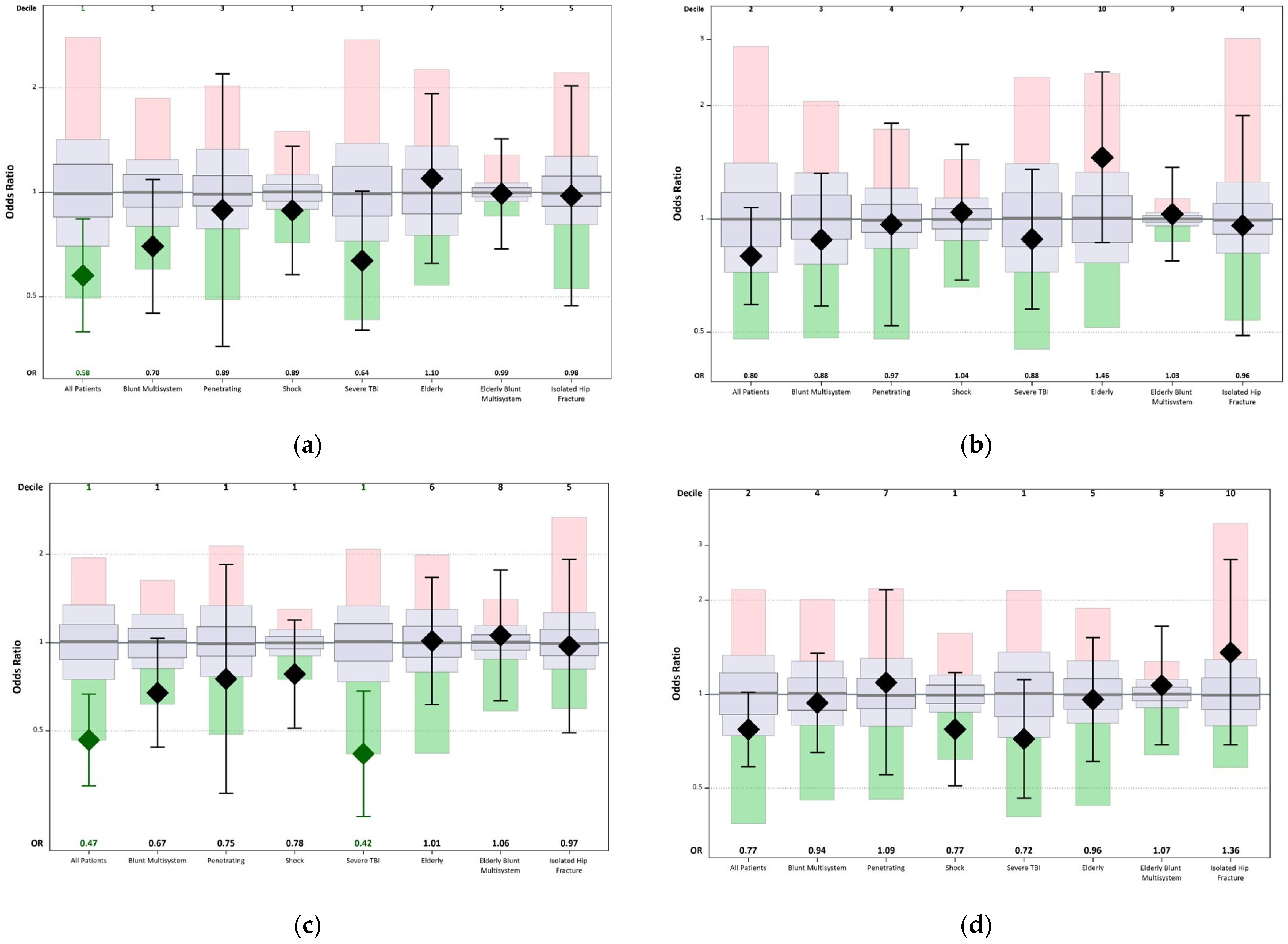
| TQIP Risk-Adjusted Mortality | ||||||||
|---|---|---|---|---|---|---|---|---|
| Fall 2020 | Fall 2021 | |||||||
| Cohort | Patients (n) | Observed Events; n (%) | TQIP Average | Odds Ratio (95% CI) | Patients (n) | Observed Events; n (%) | TQIP Average | Odds Ratio (95% CI) |
| All Patients | 904 | 36 (4.0%) | 7.4% | 0.58 (0.40–0.84) * | 871 | 31 (3.6%) | 7.9% | 0.47 (0.32–0.67) * |
| Blunt Multisystem | 170 | 19 (11.2%) | 15.1% | 0.70 (0.45–1.09) | 173 | 20 (11.6%) | 14.9% | 0.67 (0.44–1.03) |
| Penetrating | 20 | 1 (5.0%) | 7.8% | 0.89 (0.36–2.19) | 22 | 00 (0.0%) | 10.8% | 0.75 (0.31–1.85) |
| Shock | 60 | 15 (25.0%) | 26.8% | 0.89 (0.58–1.36) | 56 | 12 (21.4%) | 27.4% | 0.78 (0.51–1.20) |
| Severe TBI | 87 | 28 (32.2%) | 45.5% | 0.64 (0.40–1.01) | 92 | 18 (19.6%) | 46.0% | 0.42 (0.26–0.68) * |
| Elderly | 46 | 6 (13.0%) | 10.1% | 1.10 (0.63–1.92) | 50 | 6 (12.0%) | 10.9% | 1.01 (0.61–1.67) |
| Elderly Blunt Multisystem | 5 | 1 (20.0%) | 21.9% | 0.99 (0.69–1.43) | 6 | 2 (33.3%) | 21.9% | 1.06 (0.63–1.77) |
| Isolated Hip Fracture | 11 | 0 (0.0%) | 3.2% | 0.98 (0.47–2.03) | 13 | 0 (0.0%) | 3.8% | 0.97 (0.49–1.92) |
| TQIP Risk-Adjusted Major Hospital Events | ||||||||
| Cohort | Fall 2020 | Fall 2021 | ||||||
| All Patients | 876 | 66 (7.5%) | 11.1% | 0.80 (0.59–1.07) | 871 | 79 (9.1%) | 11.8% | 0.77 (0.59–1.02) |
| Blunt Multisystem | 160 | 33 (20.6%) | 24.5% | 0.88 (0.59–1.32) | 173 | 43 (24.9%) | 24.4% | 0.94 (0.65–1.36) |
| Penetrating | 18 | 2 (11.1%) | 19.4% | 0.97 (0.52–1.80) | 22 | 3 (13.6%) | 20.0% | 1.09 (0.55–2.16) |
| Shock | 56 | 24 (42.9%) | 37.9% | 1.04 (0.69–1.58) | 56 | 18 (32.1%) | 38.8% | 0.77 (0.51–1.17) |
| Severe TBI | 82 | 41 (50.0%) | 55.1% | 0.88 (0.58–1.36) | 92 | 38 (41.3%) | 56.0% | 0.72 (0.46–1.11) |
| Elderly | 44 | 10 (22.7%) | 12.7% | 1.46 (0.87–2.46) | 50 | 7 (14.0%) | 13.6% | 0.96 (0.61–1.52) |
| Elderly Blunt Multisystem | 4 | 2 (50.0%) | 28.4% | 1.03 (0.77–1.37) | 6 | 3 (50.0%) | 28% | 1.07 (0.69–1.66) |
| Isolated Hip Fracture | 11 | 0 (0%) | 5% | 0.96 (0.49–1.89) | 13 | 3 (23.1%) | 5.3% | 1.36 (0.69–2.70) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Thani, H.; El-Menyar, A.; Khan, N.A.; Consunji, R.; Mendez, G.; Abulkhair, T.S.; Mollazehi, M.; Peralta, R.; Abdelrahman, H.; Chughtai, T.; et al. Trauma Quality Improvement Program: A Retrospective Analysis from A Middle Eastern National Trauma Center. Healthcare 2023, 11, 2865. https://doi.org/10.3390/healthcare11212865
Al-Thani H, El-Menyar A, Khan NA, Consunji R, Mendez G, Abulkhair TS, Mollazehi M, Peralta R, Abdelrahman H, Chughtai T, et al. Trauma Quality Improvement Program: A Retrospective Analysis from A Middle Eastern National Trauma Center. Healthcare. 2023; 11(21):2865. https://doi.org/10.3390/healthcare11212865
Chicago/Turabian StyleAl-Thani, Hassan, Ayman El-Menyar, Naushad Ahmad Khan, Rafael Consunji, Gladys Mendez, Tarik S. Abulkhair, Monira Mollazehi, Ruben Peralta, Husham Abdelrahman, Talat Chughtai, and et al. 2023. "Trauma Quality Improvement Program: A Retrospective Analysis from A Middle Eastern National Trauma Center" Healthcare 11, no. 21: 2865. https://doi.org/10.3390/healthcare11212865
APA StyleAl-Thani, H., El-Menyar, A., Khan, N. A., Consunji, R., Mendez, G., Abulkhair, T. S., Mollazehi, M., Peralta, R., Abdelrahman, H., Chughtai, T., & Rizoli, S. (2023). Trauma Quality Improvement Program: A Retrospective Analysis from A Middle Eastern National Trauma Center. Healthcare, 11(21), 2865. https://doi.org/10.3390/healthcare11212865







