Development and Validation of Oral Health-Related Quality of Life Scale for Patients Undergoing Endodontic Treatment (OHQE) for Irreversible Pulpitis
Abstract
1. Introduction
2. Materials and Methods
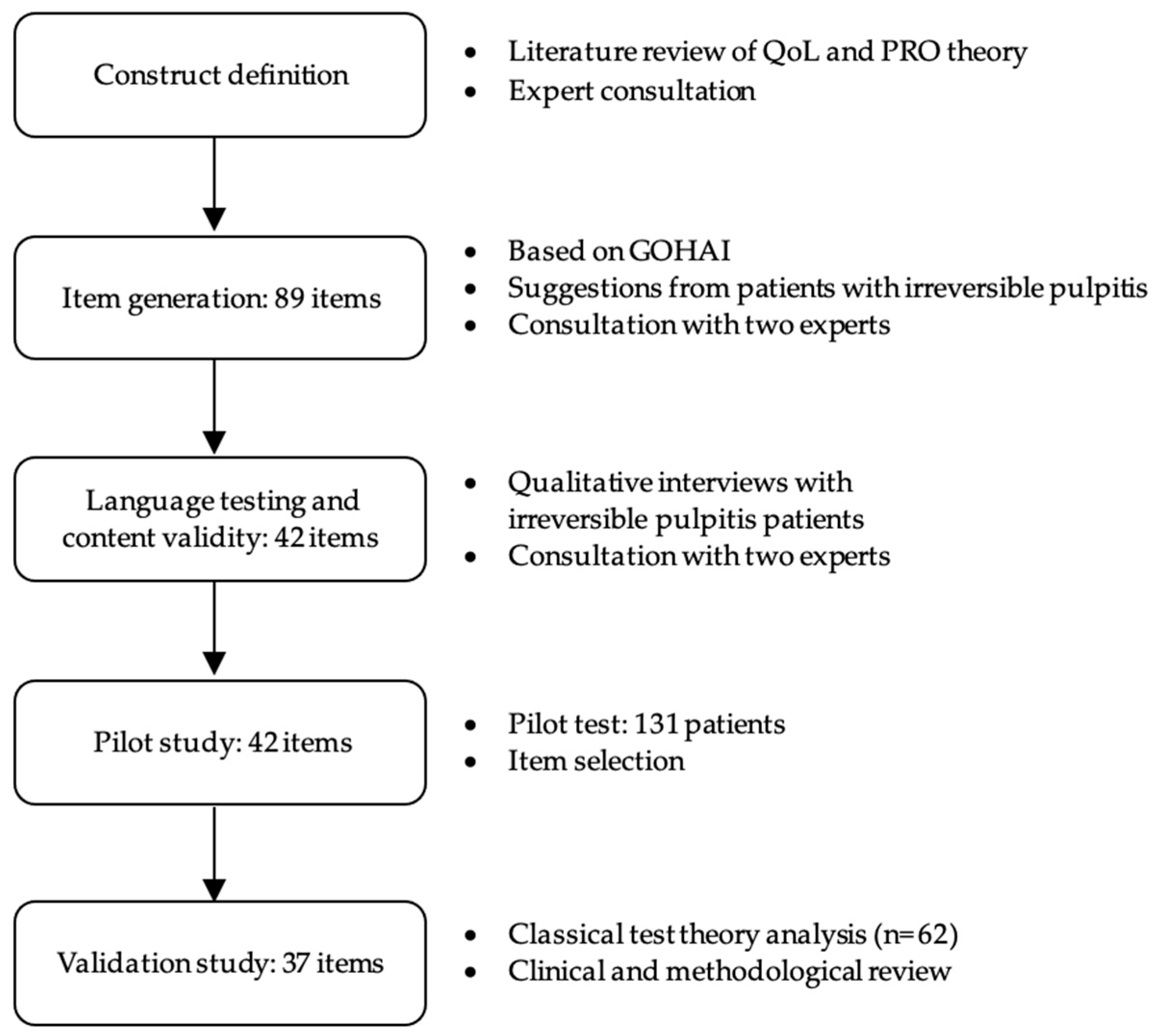
2.1. Preparation of the Question Pool
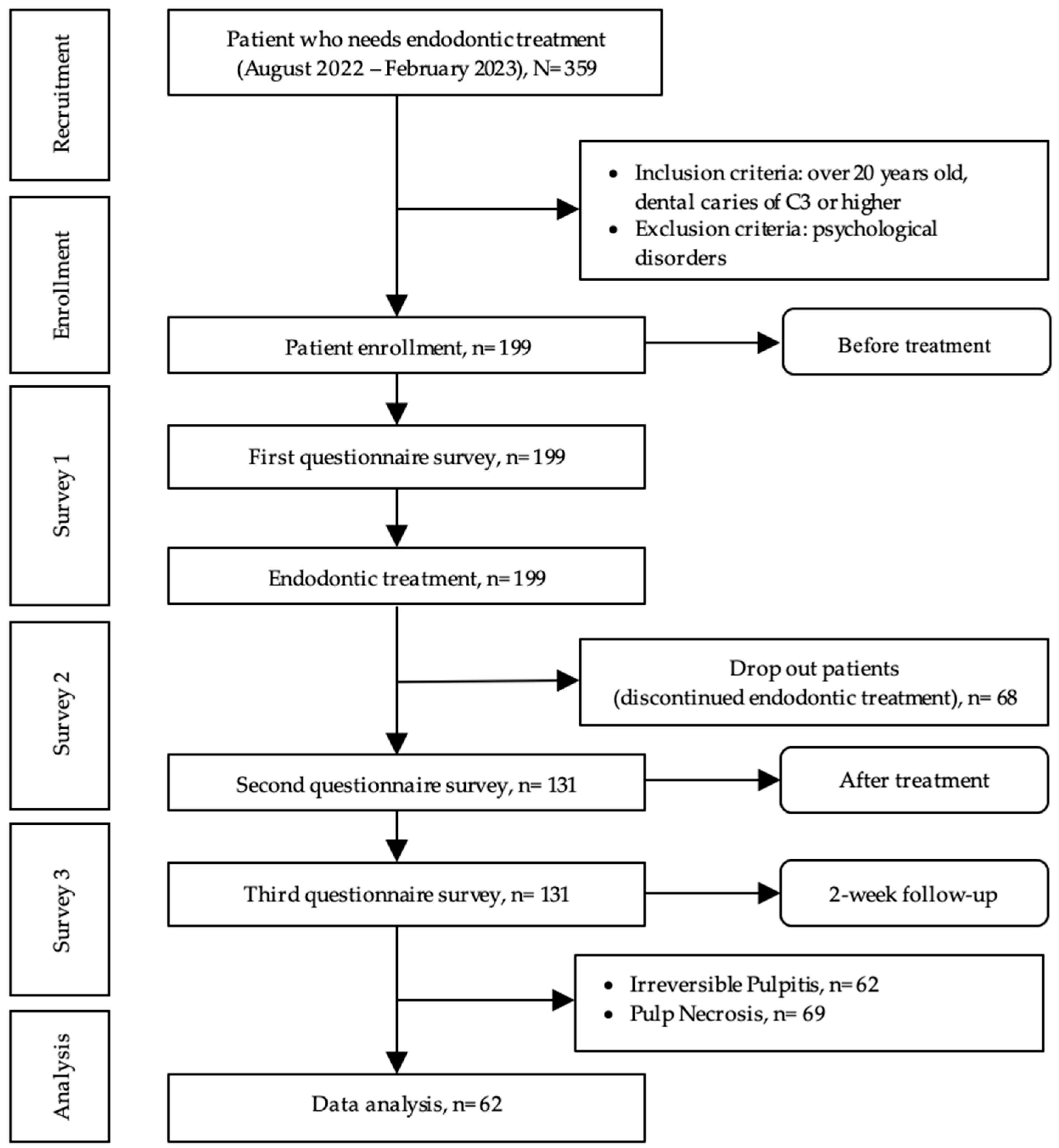
2.2. Participants
2.3. Data Collection
2.3.1. Background Data
2.3.2. Medical History
2.3.3. Dental History
2.3.4. Questionnaires
2.4. Study Design
2.5. Statistical Analysis
3. Results
3.1. Participant Characteristic
3.2. Construct Validity and Internal Consistency
3.3. Concurrent Validity
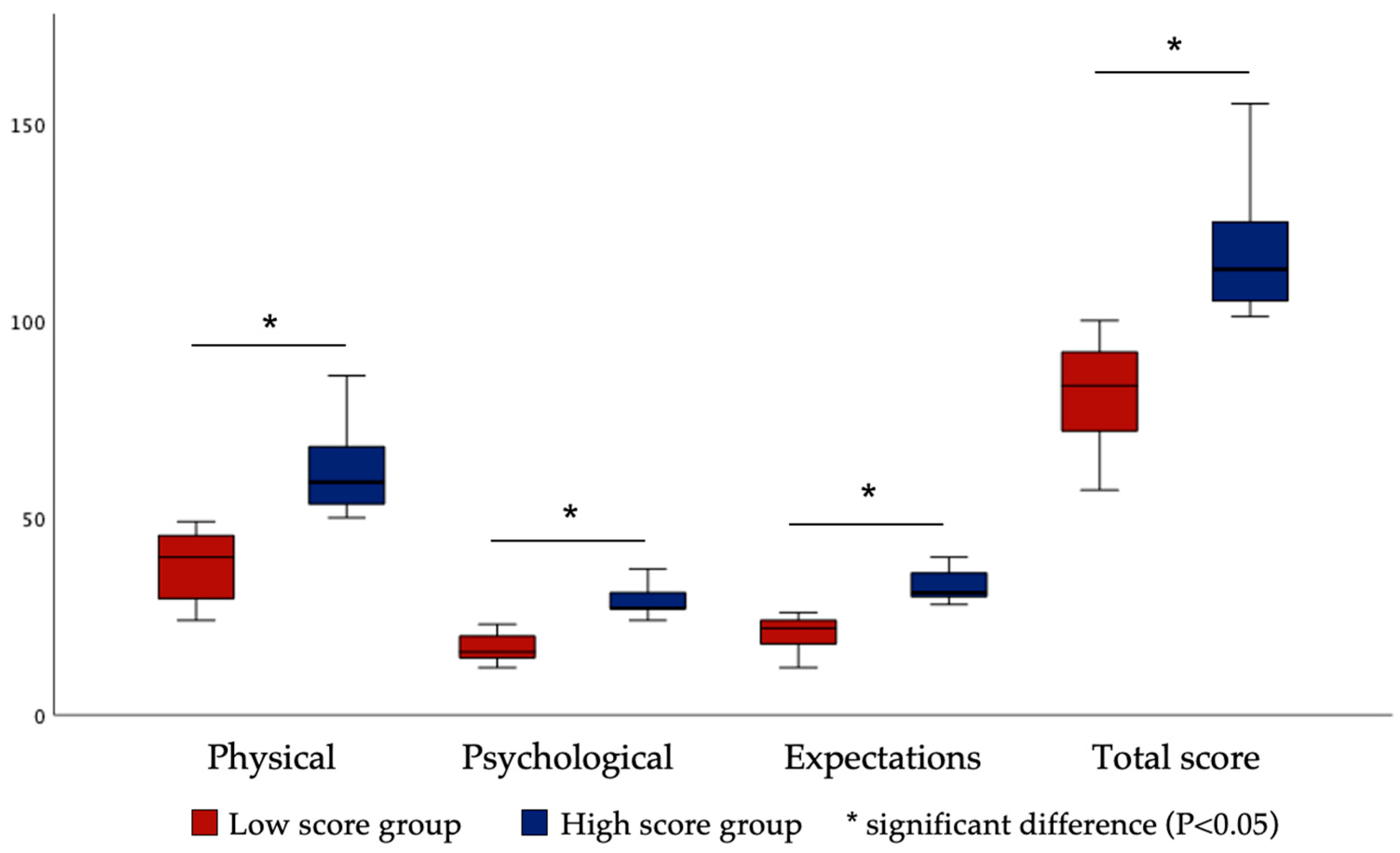
3.4. Good–Poor Analysis for Discriminant Validity
3.5. Reliability
3.6. Predictive Validity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Disease, G.B.D.; Injury, I.; Prevalence, C. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef]
- Hasil Utama Riskesdas 2018, Kementerian Kesehatan RI, Badan Penelitian dan Pengembangan Kesehatan. Available online: https://kesmas.kemkes.go.id/assets/upload/dir_519d41d8cd98f00/files/hasil-riskesdas-2018_1274.pdf (accessed on 27 June 2023).
- Aamodt, K.; Reyna-Blanco, O.; Sosa, R.; Hsieh, R.; De la Garza Ramos, M.; Garcia Martinez, M.; Orellana, M.F. Prevalence of caries and malocclusion in an indigenous population in Chiapas, Mexico. Int. Dent. J. 2015, 65, 249–255. [Google Scholar] [CrossRef]
- Shah, N.; Pandey, R.M.; Duggal, R.; Mathur, V.P.; Rajan, K.B. Oral Health in India: A Report of the Multi Centric Study; Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India and World Health Organisation Collaborative Program; Government of India: New Delhi, India, 2007. [Google Scholar]
- Abnet, C.C.; Qiao, Y.L.; Dawsey, S.M.; Dong, Z.W.; Taylor, P.R.; Mark, S.D. Tooth loss is associated with increased risk of total death and death from upper gastrointestinal cancer, heart disease, and stroke in a Chinese population-based cohort. Int. J. Epidemiol. 2005, 34, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Holmlund, A.; Holm, G.; Lind, L. Number of Teeth as a Predictor of Cardiovascular Mortality in a Cohort of 7,674 Subjects Followed for 12 Years. J. Periodontol. 2010, 81, 870–876. [Google Scholar] [CrossRef] [PubMed]
- Mack, F.; Schwahn, C.; Feine, J.S.; Mundt, T.; Bernhardt, O.; John, U.; Kocher, P.T.; Biffar, R. The impact of tooth loss on general health related to quality of life among elderly Pomeranians: Results from the study of health in Pomerania (SHIP-O). Int. J. Prosthodont. 2005, 18, 414–419. [Google Scholar]
- Wigsten, E.; Kvist, T.; Husberg, M.; EndoReCo; Davidson, T. Cost-effectiveness of root canal treatment compared with tooth extraction in a Swedish Public Dental Service: A prospective controlled cohort study. Clin. Exp. Dent. Res. 2023, 9, 661–669. [Google Scholar] [CrossRef]
- Gemmell, A.; Stone, S.; Edwards, D. Investigating acute management of irreversible pulpitis: A survey of general dental practitioners in North East England. Br. Dent. J. 2020, 228, 521–526. [Google Scholar] [CrossRef]
- Iaculli, F.; Rodriguez-Lozano, F.J.; Briseno-Marroquin, B.; Wolf, T.G.; Spagnuolo, G.; Rengo, S. Vital Pulp Therapy of Permanent Teeth with Reversible or Irreversible Pulpitis: An Overview of the Literature. J. Clin. Med. 2022, 11, 4016. [Google Scholar] [CrossRef]
- Modaresi, J.; Davoudi, A.; Badrian, H.; Sabzian, R. Irreversible pulpitis and achieving profound anesthesia: Complexities and managements. Anesth. Essays Res. 2016, 10, 3–6. [Google Scholar] [CrossRef] [PubMed]
- Zero, D.T.; Zandona, A.F.; Vail, M.M.; Spolnik, K.J. Dental Caries and Pulpal Disease. Dent. Clin. North Am. 2011, 55, 29–46. [Google Scholar] [CrossRef]
- Gomes, B.; Herrera, D.R. Etiologic role of root canal infection in apical periodontitis and its relationship with clinical symptomatology. Braz. Oral Res. 2018, 32, e69. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.; Cheung, G.S.P.; Lee, A.H.C.; McGrath, C.; Neelakantan, P. PROMs Following Root Canal Treatment and Surgical Endodontic Treatment. Int. Dent. J. 2023, 73, 28–41. [Google Scholar] [CrossRef] [PubMed]
- Tsesis, I.; Taschieri, S.; Slutzky-Goldberg, I. Contemporary endodontic treatment. Int. J. Dent. 2012, 2012, 231362. [Google Scholar] [CrossRef] [PubMed]
- Mathur, V.P.; Dhillon, J.K. Dental Caries: A Disease Which Needs Attention. Indian J. Pediatr. 2018, 85, 202–206. [Google Scholar] [CrossRef] [PubMed]
- Wigsten, E.; Kvist, T.; Jonasson, P.; Bjørndal, L.; Dawson, V.S.; Fransson, H.; Frisk, F.; Jonasson, P.; Kvist, T.; Markvart, M.; et al. Comparing Quality of Life of Patients Undergoing Root Canal Treatment or Tooth Extraction. J. Endod. 2020, 46, 19–28.e11. [Google Scholar] [CrossRef]
- Wasacz, K.; Chomyszyn-Gajewska, M.; Hukowska, D. Oral health-related quality of life (OHRQoL) in Polish adults with periodontal diseases, oral mucosal diseases and dental caries. Dent. Med. Probl. 2022, 59, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Denis, F.; Hamad, M.; Trojak, B.; Tubert-Jeannin, S.; Rat, C.; Pelletier, J.F.; Rude, N. Psychometric characteristics of the "General Oral Health Assessment Index (GOHAI) >> in a French representative sample of patients with schizophrenia. BMC Oral Health 2017, 17, 75. [Google Scholar] [CrossRef]
- Gerritsen, A.E.; Allen, P.F.; Witter, D.J.; Bronkhorst, E.M.; Creugers, N.H.J. Tooth loss and oral health-related quality of life: A systematic review and meta-analysis. Health Qual. Life Outcomes 2010, 8, 126. [Google Scholar] [CrossRef]
- Atchison, K.; Dolan, T. Development of the Geriatric Oral Health Assessment Index. J. Dent. Educ. 1990, 54, 680–687. [Google Scholar] [CrossRef]
- Locker, D.; Matear, D.; Stephens, M.; Lawrence, H.; Payne, B. Comparison of the GOHAI and OHIP-14 as measures of the oral health-related quality of life of the elderly. Community Dent. Oral Epidemiol. 2001, 29, 373–381. [Google Scholar] [CrossRef]
- Ling, Y.; Watanabe, M.; Yoshii, H.; Akazawa, K. Characteristics linked to the reduction of stigma towards schizophrenia: A pre-and-post study of parents of adolescents attending an educational program. BMC Public Health 2014, 14, 258. [Google Scholar] [CrossRef]
- Slade, G.D.; Spencer, A.J. Development and evaluation of the Oral Health Impact Profile. Community Dent. Health 1994, 11, 3–11. [Google Scholar]
- Locker, D. Measuring oral health: A conceptual framework. Community Dent. Health 1988, 5, 3–18. [Google Scholar]
- Slade, G.D. Derivation and validation of a short-form oral health impact profile. Community Dent. Oral Epidemiol. 1997, 25, 284–290. [Google Scholar] [CrossRef] [PubMed]
- El Osta, N.; Tubert-Jeannin, S.; Hennequin, M.; Bou Abboud Naaman, N.; El Osta, L.; Geahchan, N. Comparison of the OHIP-14 and GOHAI as measures of oral health among elderly in Lebanon. Health Qual. Life Outcomes 2012, 10, 131. [Google Scholar] [CrossRef] [PubMed]
- Ikebe, K.; Hazeyama, T.; Enoki, K.; Murai, S.; Okada, T.; Kagawa, R.; Matsuda, K.; Maeda, Y. Comparison of GOHAI and OHIP-14 measures in relation to objective values of oral function in elderly Japanese. Community Dent. Oral Epidemiol. 2012, 40, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Huh, J.; Nam, H.; Kim, J.; Park, J.; Shin, S.; Lee, R. Studies of Automatic Dental Cavity Detection System as an Auxiliary Tool for Diagnosis of Dental Caries in Digital X-ray Image. Prog. Med. Phys. 2015, 26, 52–58. [Google Scholar] [CrossRef][Green Version]
- Caton, J.G.; Armitage, G.; Berglundh, T.; Chapple, I.L.C.; Jepsen, S.; Kornman, K.S.; Mealey, B.L.; Papapanou, P.N.; Sanz, M.; Tonetti, M.S. A new classification scheme for periodontal and peri-implant diseases and conditions—Introduction and key changes from the 1999 classification. J. Clin. Periodontol. 2018, 45 (Suppl. S20), S1–S8. [Google Scholar] [CrossRef]
- Mat Nawi, F.A.; Abdul Malek, A.T.; Muhammad Faizal, S.; Wan Masnieza Wan, M. A Review on the Internal Consistency of a Scale: The Empirical Example of the Influence of Human Capital Investment on Malcom Baldridge Quality Principles in Tvet Institutions. Asian People J. APJ 2020, 3, 19–29. [Google Scholar] [CrossRef]
- Mukaka, M.M. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med. J. 2012, 24, 69–71. [Google Scholar]
- Chaparro-Rico, B.D.M.; Cafolla, D. Test-Retest, Inter-Rater and Intra-Rater Reliability for Spatiotemporal Gait Parameters Using SANE (an eaSy gAit aNalysis systEm) as Measuring Instrument. Appl. Sci. 2020, 10, 5781. [Google Scholar] [CrossRef]
- Vettore, M.V.; Rebelo, M.A.B.; Rebelo Vieira, J.M.; Cardoso, E.M.; Birman, D.; Leao, A.T.T. Psychometric Properties of the Brazilian Version of GOHAI among Community-Dwelling Elderly People. Int. J. Environ. Res. Public Health 2022, 19, 14725. [Google Scholar] [CrossRef] [PubMed]
- Basch, E.; Schrag, D.; Henson, S.; Jansen, J.; Ginos, B.; Stover, A.M.; Carr, P.; Spears, P.A.; Jonsson, M.; Deal, A.M.; et al. Effect of Electronic Symptom Monitoring on Patient-Reported Outcomes Among Patients with Metastatic Cancer: A Randomized Clinical Trial. JAMA 2022, 327, 2413–2422. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Alfonso, K.E.; Sánchez-Martínez, V. Electronic Patient-Reported Outcome Measures Evaluating Cancer Symptoms: A Systematic Review. Semin. Oncol. Nurs. 2021, 37, 151145. [Google Scholar] [CrossRef]
- Ogura, K.; Yakoub, M.A.; Christ, A.B.; Fujiwara, T.; Nikolic, Z.; Boland, P.J.; Healey, J.H. What Are the Minimum Clinically Important Differences in SF-36 Scores in Patients with Orthopaedic Oncologic Conditions? Clin. Orthop. Relat. Res. 2020, 478, 2148–2158. [Google Scholar] [CrossRef]
- Tuomi, L.; Johansson, M.; Andréll, P.; Finizia, C. Interpretation of the Swedish Self Evaluation of Communication Experiences after Laryngeal cancer: Cutoff levels and minimum clinically important differences. Head Neck 2016, 38, 689–695. [Google Scholar] [CrossRef]
- Khademi, A.; Roohafza, H.; Iranmanesh, P.; Yaraghi, N.; Sichani, A.V. Association between psychological factors and pain perception in patients with symptomatic irreversible pulpitis during endodontic treatment. G. Ital. Endod. 2020, 34, 13–19. [Google Scholar]
- Katijjahbe, M.A.; Denehy, L.; Granger, C.L.; Royse, A.; Royse, C.; Logie, S.; Sturgess, T.; Md Ali, N.A.; McManus, M.; Sandy, C.E.; et al. Psychometric evaluation of the shortened version of the Functional Difficulties Questionnaire to assess thoracic physical function. Clin. Rehabil. 2020, 34, 132–140. [Google Scholar] [CrossRef]
- Schmalz, G.; Fenske, F.; Reuschel, F.; Bartl, M.; Schmidt, L.; Goralski, S.; Roth, A.; Ziebolz, D. Association between oral health and oral health-related quality of life in patients before hip and knee endoprosthesis surgery: A cross-sectional study. BMC Oral Health 2022, 22, 604. [Google Scholar] [CrossRef]
- Hosseini, B.; Nedjat, S.; Zendehdel, K.; Majdzadeh, R.; Nourmohammadi, A.; Montazeri, A. Response shift in quality of life assessment among cancer patients: A study from Iran. Med. J. Islam Repub. Iran 2017, 31, 120. [Google Scholar] [CrossRef]
- Carlier, I.V.E.; van Eeden, W.A.; de Jong, K.; Giltay, E.J.; van Noorden, M.S.; van der Feltz-Cornelis, C.; Zitman, F.G.; Kelderman, H.; van Hemert, A.M. Testing for response shift in treatment evaluation of change in self-reported psychopathology amongst secondary psychiatric care outpatients. Int. J. Methods Psychiatr. Res. 2019, 28, e1785. [Google Scholar] [CrossRef]
- Liu, P.; McGrath, C.; Cheung, G. Quality of life and psychological well-being among endodontic patients: A case-control study. Aust. Dent. J. 2012, 57, 493–497. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; McGrath, C.; Cheung, G.S. Improvement in oral health-related quality of life after endodontic treatment: A prospective longitudinal study. J. Endod. 2014, 40, 805–810. [Google Scholar] [CrossRef] [PubMed]
- Neelakantan, P.; Liu, P.; Dummer, P.M.H.; McGrath, C. Oral health-related quality of life (OHRQoL) before and after endodontic treatment: A systematic review. Clin. Oral Investig. 2020, 24, 25–36. [Google Scholar] [CrossRef]
- Dugas, N.N.; Lawrence, H.P.; Teplitsky, P.; Friedman, S. Quality of life and satisfaction outcomes of endodontic treatment. J. Endod. 2002, 28, 819–827. [Google Scholar] [CrossRef] [PubMed]
- Hamadallah, A.O.A.; Abdullah Alshuaybi, A.A.; Alhamid, A.w.h.; Hassan, R.E.S. Quality of Life and Patient Satisfaction after Endodontic Treatment Performed in Three Hospitals in Jeddah, kingdom of Saudi Arabia. J. Pharm. Res. Int. 2021, 33, 84–96. [Google Scholar] [CrossRef]
- Allen, P.F. Assessment of oral health related quality of life. Health Qual. Life Outcomes 2003, 1, 40. [Google Scholar] [CrossRef] [PubMed]
- Kravitz, R.L.; Cope, D.W.; Bhrany, V.; Leake, B. Internal medicine patients’ expectations for care during office visits. J. Gen. Intern. Med. 1994, 9, 75–81. [Google Scholar] [CrossRef]
- Dogramaci, E.J.; Rossi-Fedele, G. Patient-related outcomes and Oral Health-Related Quality of Life in endodontics. Int. Endod. J. 2023, 56 (Suppl. S2), 169–187. [Google Scholar] [CrossRef]
- Gravesande, J.; Richardson, J.; Griffith, L.; Scott, F. Test-retest reliability, internal consistency, construct validity and factor structure of a falls risk perception questionnaire in older adults with type 2 diabetes mellitus: A prospective cohort study. Arch. Physiother. 2019, 9, 14. [Google Scholar] [CrossRef]
- Tubert-Jeannin, S.; Riordan, P.J.; Morel-Papernot, A.; Porcheray, S.; Saby-Collet, S. Validation of an oral health quality of life index (GOHAI) in France. Community Dent. Oral Epidemiol. 2003, 31, 275–284. [Google Scholar] [CrossRef] [PubMed]
- Furnham, A. Relationship among Four Big Five Measures of Different Length. Psychol. Rep. 2008, 102, 312–316. [Google Scholar] [CrossRef]
- Balgiu, B.A.; Sfeatcu, R.; Mihai, C.; Lupusoru, M.; Bucur, M.V.; Tribus, L. Romanian Version of the Oral Health Values Scale: Adaptation and Validation. Medicina 2022, 58, 544. [Google Scholar] [CrossRef] [PubMed]
- Schober, P.; Boer, C.; Schwarte, L.A. Correlation Coefficients: Appropriate Use and Interpretation. Anesth. Analg. 2018, 126, 1763–1768. [Google Scholar] [CrossRef] [PubMed]
- Gkavela, G.; Kossioni, A.; Lyrakos, G.; Karkazis, H.; Volikas, K. Oral health related quality of life in older people: Preliminary validation of the Greek version of the Geriatric Oral Health Assessment Index (GOHAI). Eur. Geriatr. Med. 2015, 6, 245–250. [Google Scholar] [CrossRef]
- Carlson, N. Accounting for Participant Dropout in Clinical Studies. Sci. Transl. Med. 2010, 2, 16ec14. [Google Scholar] [CrossRef]
| Variables | Categories | n (%) or Mean [SD] |
|---|---|---|
| Age (years) | 36.5 [12.4] | |
| Sex | Male | 23 (37.1) |
| Female | 39 (62.9) | |
| Body mass index (kg/m2) | 23.5 [3.6] | |
| Job | Employed | 34 (54.8) |
| Unemployed | 28 (45.2) | |
| University graduate | Yes | 32 (51.6) |
| No | 30 (48.4) | |
| Monthly income | <3,300,000 IDR | 43 (69.4) |
| ≥3,300,000 IDR | 19 (30.6) | |
| Number of housemates | 4.2 [1.6] | |
| Systemic disease | Yes | 15 (24.2) |
| No | 47 (75.8) | |
| Medication taken | Yes | 8 (12.9) |
| No | 54 (87.1) | |
| Allergies | Yes | 5 (8.1) |
| No | 57 (91.9) | |
| Number of teeth | 26.7 [4.3] | |
| Denture use | Yes | 4 (6.5) |
| No | 58 (93.5) | |
| Grade of caries | C3 | 55 (88.7) |
| C4 | 7 (11.3) | |
| Grade of periodontal disease | S1 | 37 (59.7) |
| S2 | 21 (33.9) | |
| S3 | 4 (6.5) | |
| S4 | 0 (0.0) | |
| Brushing (times) | 2.2 [0.5] | |
| VAS | 4.5 [2.7] |
| Items | Factor Loading | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| Factor 1. Physical | |||
| Q10. Have you had toothache? | 0.81 | −0.32 | 0.17 |
| Q14. Have you ever felt pain that radiates from a dental pain? | 0.79 | 0.34 | 0.07 |
| Q24. Has your sleep been interrupted because of dental pain? | 0.79 | 0.31 | −0.03 |
| Q9. Have you had headaches because of dental pain? | 0.76 | 0.24 | −0.08 |
| Q8. Have you had a sore jaw because of dental pain? | 0.75 | 0.19 | 0.29 |
| Q7. Have you had painful aching in your mouth because of dental pain? | 0.71 | 0.17 | 0.06 |
| Q11. Have you had painful gums? | 0.70 | 0.05 | 0.15 |
| Q26. Have you found it difficult to relax because of dental pain? | 0.68 | 0.53 | 0.14 |
| Q13. Have you ever taken medication to relieve dental pain? | 0.67 | 0.11 | 0.19 |
| Q15. Have you ever felt pain radiating to the ear because of dental pain? | 0.67 | 0.23 | 0.26 |
| Q1. Have you had difficulty chewing any foods because of dental pain? | 0.65 | 0.26 | −0.002 |
| Q6. Have you ever had difficulty opening your mouth because of dental pain? | 0.63 | 0.53 | −0.06 |
| Q23. Have you ever been unable to lie down because of dental pain? | 0.62 | 0.37 | 0.09 |
| Q21. Have you had to avoid eating some foods because of dental pain? | 0.62 | 0.43 | 0.11 |
| Q27. Have you avoided going out because of dental pain? | 0.59 | 0.53 | −0.17 |
| Q17. Have you felt tense because of dental pain? | 0.57 | 0.54 | 0.13 |
| Q18. Have you ever felt that your toothache is a serious disease? | 0.54 | 0.44 | 0.31 |
| Q28. Have you been a bit irritable with other people because of dental pain? | 0.45 | 0.39 | −0.15 |
| Q33. Have you ever thought that the root canal treatment can be reinfected in the future? | 0.36 | 0.11 | −0.37 |
| Factor 2. Psychological | |||
| Q16. Have you felt uncomfortable about the appearance of your teeth because of dental pain? | 0.12 | 0.84 | 0.22 |
| Q4. Have you felt that your sense of taste has worsened because of dental pain? | 0.11 | 0.82 | 0.01 |
| Q5. Have you felt that your digestion has worsened because of dental pain? | 0.11 | 0.78 | 0.14 |
| Q3. Have you felt that your appearance has been affected because of dental pain? | 0.15 | 0.73 | −0.008 |
| Q19. Do you ever overthink about your health condition because of dental pain? | 0.41 | 0.59 | 0.27 |
| Q2. Have you had trouble pronouncing any words because of dental pain? | 0.39 | 0.55 | −0.11 |
| Q29. Have you felt that your general health has worsened because of dental pain? | 0.29 | 0.54 | 0.16 |
| Q25. Have you been upset because of dental pain? | 0.47 | 0.54 | 0.21 |
| Q20. Has your speech been unclear because of dental pain? | 0.38 | 0.41 | −0.29 |
| Q31. Have you ever thought that it is better to have a tooth extracted than to treat it? | 0.17 | 0.29 | −0.03 |
| Factor 3. Expectations | |||
| Q37. Have you ever thought that root canal treatment could have a good impact on your health? | −0.07 | 0.00 | 0.82 |
| Q22. Have you ever thought that root canal treatment can improve your chewing function? | 0.15 | −0.08 | 0.79 |
| Q35. Have you ever thought that root canal treatment can improve quality of life? | 0.03 | 0.12 | 0.79 |
| Q36. Have you ever thought that root canal treatment can improve dental aesthetics? | −0.05 | 0.30 | 0.77 |
| Q12. Have you ever felt that root canal treatment can eliminate your dental pain? | 0.18 | 0.01 | 0.76 |
| Q32. Have you ever thought that root canal treatment is worth doing? | 0.09 | −0.04 | 0.65 |
| Q30. Have you ever thought that root canal treatment is expensive? | 0.12 | 0.17 | 0.55 |
| Q34. Have you ever thought that root canal treatment should be performed by a specialist rather than a general dentist? | 0.26 | 0.05 | 0.51 |
| Sum of squares on factor loading | 9.29 | 6.43 | 4.98 |
| Variance explained (%) | 25.13 | 17.38 | 13.45 |
| Cumulative variance explained (%) | 25.13 | 42.50 | 55.95 |
| Cronbach’s alpha coefficient | 0.95 | 0.87 | 0.87 |
| GOHAI | OHQE | |||
|---|---|---|---|---|
| Physical | Psychological | Expectations | Total Score | |
| Physical function | ||||
| r | 0.28 | 0.21 | 0.36 | 0.38 |
| p-value | 0.03 * | 0.09 | 0.004 * | 0.003 * |
| Psychosocial function | ||||
| r | 0.48 | 0.57 | 0.37 | 0.61 |
| p-value | <0.01 * | <0.01 * | 0.003 * | <0.01 * |
| Pain or discomfort in the mouth | ||||
| r | 0.27 | 0.18 | 0.29 | 0.31 |
| p-value | 0.03 * | 0.15 | 0.02 * | 0.02 * |
| Total score | ||||
| r | 0.44 | 0.45 | 0.41 | 0.57 |
| p-value | <0.01 * | <0.01 * | 0.001 * | <0.01 * |
| Factor | ICC (95% CI) |
|---|---|
| Physical | 0.95 (0.93–0.96) |
| Psychological | 0.92 (0.89–0.95) |
| Expectations | 0.89 (0.84–0.93) |
| Total score | 0.58 (0.18–0.77) |
| Variables | β | B | 95% CI | p-Value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Physical | 0.04 | 0.05 | −0.29 | 0.39 | 0.77 |
| Psychological | 0.26 | 0.74 | 0.02 | 1.45 | 0.04 * |
| Expectations | 0.21 | 0.60 | −0.13 | 1.33 | 0.11 |
| Total score | 0.16 | 0.14 | −0.08 | 0.35 | 0.21 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arifin, F.A.; Matsuda, Y.; Kanno, T. Development and Validation of Oral Health-Related Quality of Life Scale for Patients Undergoing Endodontic Treatment (OHQE) for Irreversible Pulpitis. Healthcare 2023, 11, 2859. https://doi.org/10.3390/healthcare11212859
Arifin FA, Matsuda Y, Kanno T. Development and Validation of Oral Health-Related Quality of Life Scale for Patients Undergoing Endodontic Treatment (OHQE) for Irreversible Pulpitis. Healthcare. 2023; 11(21):2859. https://doi.org/10.3390/healthcare11212859
Chicago/Turabian StyleArifin, Fadil Abdillah, Yuhei Matsuda, and Takahiro Kanno. 2023. "Development and Validation of Oral Health-Related Quality of Life Scale for Patients Undergoing Endodontic Treatment (OHQE) for Irreversible Pulpitis" Healthcare 11, no. 21: 2859. https://doi.org/10.3390/healthcare11212859
APA StyleArifin, F. A., Matsuda, Y., & Kanno, T. (2023). Development and Validation of Oral Health-Related Quality of Life Scale for Patients Undergoing Endodontic Treatment (OHQE) for Irreversible Pulpitis. Healthcare, 11(21), 2859. https://doi.org/10.3390/healthcare11212859






