Factors Related to Oral-Health-Related Quality of Life in Adult Male Inmates: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Variables
2.3.1. Dependent Variables
2.3.2. Independent Variables
2.3.3. Covariables
2.4. Data Collection
2.5. Statistical Analyses
3. Results
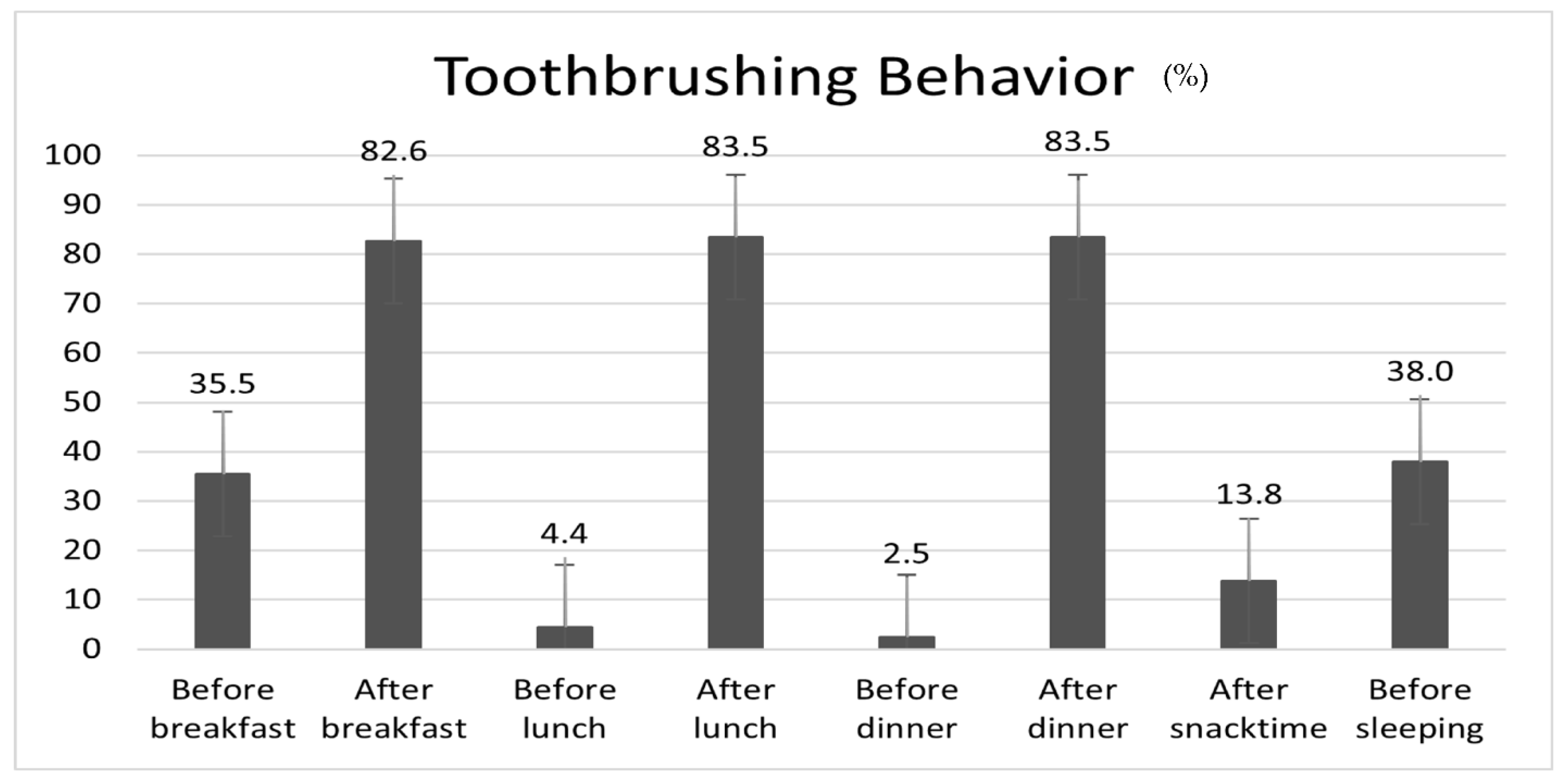
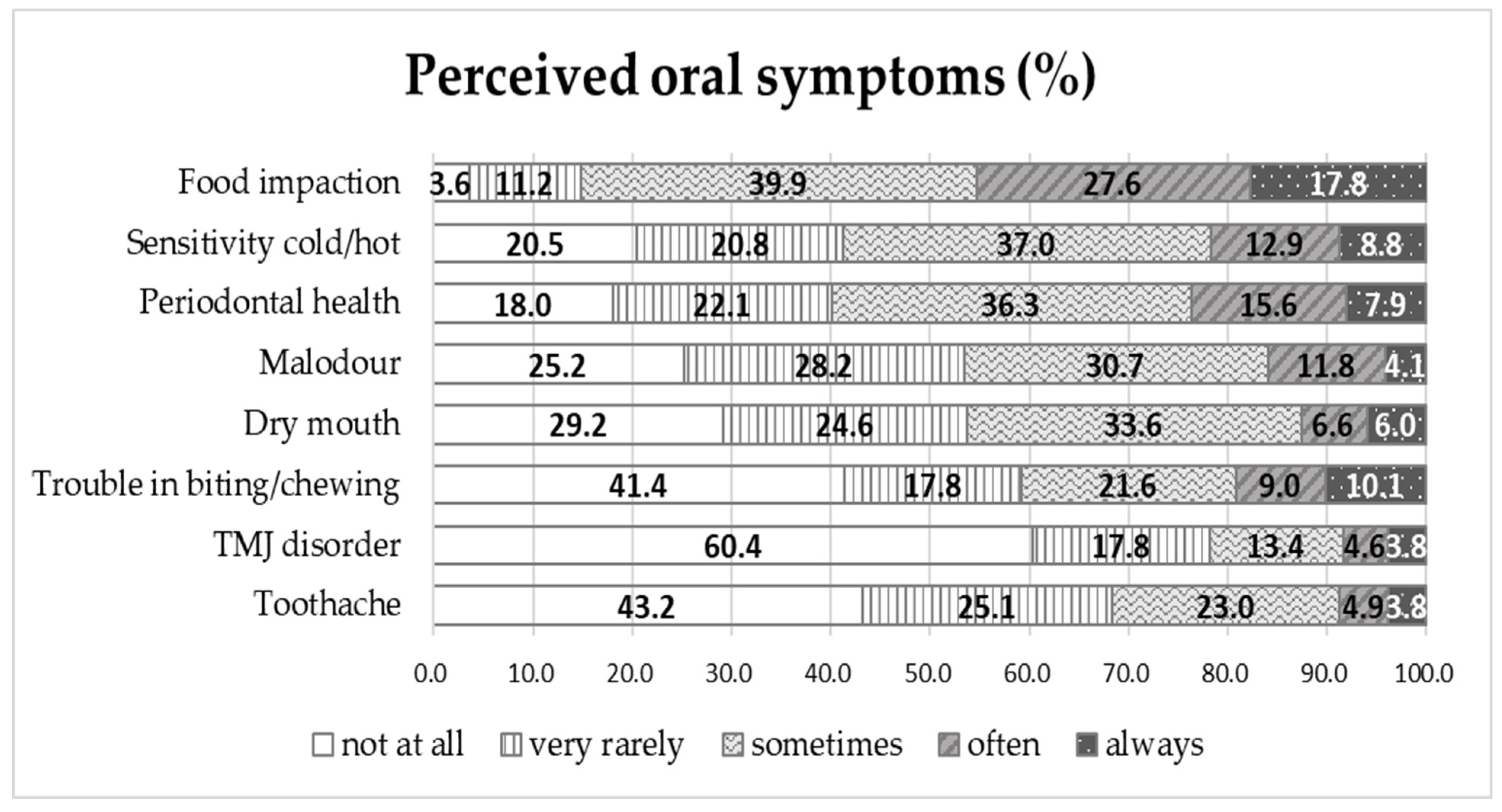
3.1. Toothbrushing Behaviour and Perceived Oral Symptoms in Male Inmates
3.2. OHIP-14 According to the General Characteristics of Male Inmates
3.3. Correlations between Perceived Oral Symptoms and Self-Esteem and the OHIP-14 in Male Inmates
3.4. Factors Related to the OHIP-14 in Male Inmates
4. Discussion
Clinical Strengths, Limitations, and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ryu, D.-Y.; Song, K.-S.; Han, S.-Y. Oral health condition, recognition, and practice in prisoners. J. Dent. Hyg. Sci. 2015, 15, 153–159. [Google Scholar] [CrossRef]
- Yeon, S.-J.; Roh, Y.-J.; Kim, A.-S.; Jung, Y.-J. Health and medical services for inmates in Korean correctional facilities. KICJ 2008, 12, 1–228. [Google Scholar]
- Ju, Y. Survey on the Right to Health in Detention Facilities; National Human Rights Commission of Korea: Seoul, Republic of Korea, 2017.
- Sharma, N.; Bhatia, S.; Sodhi, A.S.; Batra, N. Oral microbiome and health. AIMS Microbiol. 2018, 4, 42–66. [Google Scholar] [CrossRef] [PubMed]
- Kozak, M.; Pawlik, A. The role of the oral microbiome in the development of diseases. Int. J. Mol. Sci. 2023, 24, 5231. [Google Scholar] [CrossRef]
- Guzman, C.; Zaclli, A.; Molinari, J. Streptococcus cristatus bacteremia in a patient with poor oral hygiene: A case report. J. Med. Case Rep. 2023, 17, 218. [Google Scholar] [CrossRef] [PubMed]
- Amato, A. Periodontitis and Cancer: Beyond the boundaries of oral cavity. Cancers 2023, 15, 1736. [Google Scholar] [CrossRef] [PubMed]
- Ferruzzi, L.P.D.C.; Davi, L.R.; Lima, D.C.B.D.; Tavares, M.; Castro, A.M.D. Oral health-related quality of life of athletes with disabilities: A cross sectional study. Biosci. J. 2021, 37, e37008. [Google Scholar]
- Slade, G.D.; Spencer, A.J. Development and evaluation of the oral health impact profile. Community Dent. Health 1994, 11, 3–11. [Google Scholar]
- Slade, G.D. Derivation and validation of a short-form oral health impact profile. Community Dent. Oral Epidemiol. 1997, 25, 284–290. [Google Scholar] [CrossRef]
- Kwon, H.-J.; Yoon, M.-S. Relationship of depression, stress, and self-esteem with oral health-related quality of life of middle-aged women. J. Dent. Hyg. Sci. 2015, 15, 825–835. [Google Scholar] [CrossRef][Green Version]
- Balkrishna, A.; Singh, K.; Sharma, A.; Parkar, S.M.; Oberoi, G. Oral health among prisoners of district Jail, Haridwar, Uttarakhand, India—A cross-sectional study. Rev. Esp. Sanid. Penit. 2022, 24, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Moraes, L.R.; Duarte de Aquino, L.C.; da Cruz, D.T.; Leite, I.C.G. Self-perceived impact of oral health on the quality of life of women deprived of their liberty. Int. J. Dent. 2021, 2021, 5520652. [Google Scholar] [CrossRef]
- Soares, G.H.; Mendonça, I.; Michel-Crosato, E.; Moysés, S.J.; Moysés, S.T.; Werneck, R.I. Impact of oral conditions on the quality of life of incarcerated women in Brazil. Health Care Women Int. 2019, 40, 776–787. [Google Scholar] [CrossRef] [PubMed]
- Bukhari, R.; Al-Sulaim, A.; Fadaak, A.; Balhaddad, A.; AlKhalfan, A.; El Tantawi, M.; Al-Ansari, A. Oral health amongst male inmates in Saudi prisons compared with that of a sample of the general male population. S. Afr. Dent. J. 2017, 72, 402–407. [Google Scholar] [CrossRef]
- Casarin, M.; Nolasco, W.D.S.; Colussi, P.R.G.; Piardi, C.C.; Weidlich, P.; Rösing, C.K.; Muniz, F.W.M.G. Prevalence of tooth loss and associated factors in institutionalized adolescents: A cross-sectional study. Cien. Saúde Colet. 2021, 26, 2635–2642. [Google Scholar] [CrossRef] [PubMed]
- Alkhadra, T. Prevalence of dental caries and oral hygiene status among Juvenile Prisoners in the Kingdom of Saudi Arabia. J. Contemp. Dent. Pract. 2017, 18, 991–995. [Google Scholar] [CrossRef] [PubMed]
- Evensen, K.B.; Bull, V.H. Oral Health in Prison: An Integrative Review. Int. J. Prison. Health 2023, 19, 251–269. [Google Scholar] [CrossRef]
- Evensen, K.B.; Bull, V.H.; Ness, L. A health promotion intervention to improve oral health of prisoners: Results from a pilot study. Int. J. Prison. Health 2021, 17, 546–559. [Google Scholar] [CrossRef]
- Hwang, I.; Park, K.; Park, H.K. Prevalence ofdDental caries and associated factors of detention center inmates in South Korea compared with Korea National Health and Nutrition Examination Survey (KNHANES) respondents: A retrospective study. BMC Oral Health 2022, 22, 383. [Google Scholar] [CrossRef]
- Lee, C.-U.; Yoo, J.-H.; Choi, B.-H.; Sul, S.-H.; Kim, H.-R.; Mo, D.-Y.; Kim, J.-B. Conservative infection control on acute pericoronitis in mandibular third molar patients referred from the prison. J. Korean Assoc. Oral Maxillofac. Surg. 2010, 36, 57–61. [Google Scholar] [CrossRef]
- Hong, S.-H. A research on recognition of oral health based on oral health education for adolescents in some reformatories. J. Dent. Hyg. Sci. 2007, 7, 187–191. [Google Scholar]
- Jung, Y.-J.; Jeong, S.-Y.; Kang, B.-J.; Baek, K.-W. Oral health status and self-perceived oral health status of students in Juvenile protection education institutions. J. Korean Acad. Pediatr. Dent. 2009, 36, 539–549. [Google Scholar]
- Clinical Research Information System (CRIS). Available online: https://cris.nih.go.kr/cris/index.jsp (accessed on 13 July 2023).
- Bana, K.F.M.A.; Shadab, S.; Hakeem, S.; Ilyas, F. Comparing oral health-related quality of life (OHIP-14) and masticatory efficiency with complete denture treatment. J. Coll. Physicians Surg. Pak. 2021, 30, 694–698. [Google Scholar] [CrossRef]
- Lee, D.-I.; Han, S.-J. Factors Which affect the oral health-related quality of life of workers. J. Dent. Hyg. Sci. 2013, 13, 480–486. [Google Scholar]
- Rosenberg, M. Society and the Adolescent Self-Image; Princeton: Singapore, 1965; pp. 16–36. [Google Scholar]
- Nasiriziba, F.; Saati, M.; Haghani, H. Correlation between self-efficacy and self-esteem in patients with an intestinal stoma. Br. J. Nurs. 2020, 29, S22–S29. [Google Scholar] [CrossRef] [PubMed]
- Choi, C.-H.; Choi, Y.-H.; Jeong, S.-H.; Cho, H.-J.; Son, C.-K.; Jeong, S.-H. Korea National Children’s Oral Health Survey; National Center for Medical Information and Knowledge (NCMIK): Cheongju-si, Republic of Korea, 2018.
- Public Health England. Survey of Prison Dental Services England, Wales and Northern Ireland 2017 to 2018; Public Health England: Bristol, UK, 2022.
- The Scottish Government. Oral Health Improvement and Dental Services in Scottish Prisons; The Scottish Government: Edinburgh, UK, 2015.
- Billa, A.L.; Sukhabogi, J.R.; Doshi, D.; Jummala, S.; Turaga, S.S. Correlation of self-esteem with oral hygiene behaviour and oral health status among adult dental patients. Ann. Ig. 2023, 35, 534–545. [Google Scholar] [CrossRef] [PubMed]
- Ibigbami, O.I.; Folayan, M.O.; Oginni, O.; Lusher, J.; Sam-Agudu, N.A. Moderating effects of resilience and self-esteem on associations between self-reported oral health problems, quality of oral health, and mental health among adolescents and adults in Nigeria. PLoS ONE 2023, 18, e0285521. [Google Scholar] [CrossRef]
- Melbye, E.L. Dimensional structure of the OHIP-14 and associations with self-report oral health-related variables in home-dwelling Norwegians aged 70. Acta Odontol. Scand. 2023, 81, 66–72. [Google Scholar] [CrossRef]
- Korea Centers for Disease Control & Prevention. Community Health Survey. Internet. 2022. Available online: https://chs.kdca.go.kr/chs/ststs/statsMain.do (accessed on 15 July 2023).
- Korea Centers for Disease Control & Prevention. Korean National Health and Nutrition Examination Surveys 2013~2015. Available online: https://knhanes.cdc.go.kr/knhanes/sub01/sub01_02.do#s2_01 (accessed on 15 July 2023).
- The Korean Law Information Center. Act on the Execution of Penalties and Treatment of Inmates. The Korean Law Information Center. Act on Execution of Sentences and Treatment of Prisoners. 2022. Available online: https://law.go.kr (accessed on 15 July 2023).
- Park, C.-S.; Kim, I.-J. Oral health behavior according to perceived oral symptoms in the elderly. J. Korean Soc. Dent. Hyg. 2016, 16, 955–968. [Google Scholar] [CrossRef]
- Hong, M.-H.; Lee, J.-M.; Jang, K.-W. Effect of oral health status and work loss on oral health-related quality of life of non-medical hospital workers. J. Converg. Inf. Technol. 2022, 12, 163–173. [Google Scholar]
- Kim, A.-J.; Kang, E.-J. A study on the oralsSymptoms and oral health-related quality of life (OHIP-14) of industrial workers. J. Dent. Hyg. Sci. 2014, 14, 51–58. [Google Scholar]
- Moon, B.; Jeong, S.-R.; Jang, J.-Y.; Kim, K.-Y. Health-related quality of life by oral health behavior and oral health status for the middle-aged people. J. Korean Soc. Dent. Hyg. 2015, 15, 197–204. [Google Scholar] [CrossRef]
- Park, E.-S.; Choi, J.-S. The effect of health status on general quality of life and oral health related quality of life in the middle-aged adults. J. Dent. Hyg. Sci. 2012, 12, 624–633. [Google Scholar]
- Yoon, S.-U.; Nam, I.-S. Oral health impact profile(OHIP) according to the oral health behavior of foreign workers. J. Korean Soc. Dent. Hyg. 2015, 15, 451–459. [Google Scholar] [CrossRef][Green Version]
- Yoon, H.-S. Relationship of Oral health status and oral health care to the quality of life in patients of dental hospitals and clinics. J. Dent. Hyg. Sci. 2015, 15, 594–602. [Google Scholar] [CrossRef][Green Version]
- Kim, J.-L.; Kim, J.-H.; Jang, J.-H. Relationship between dental checkups and unmet dental care needs in Korean adults. J. Korean Soc. Dent. Hyg. 2020, 20, 581–591. [Google Scholar]
- Jang, J.H.; Kim, J.L.; Kim, J.H. Associations between dental checkups and unmet dental care needs: An examination of cross-sectional data from the seventh Korea National Health and Nutrition Examination Survey (2016–2018). Int. J. Environ. Res. Public Health 2021, 18, 3750. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.-J.; Kim, M.-G. The effect of oral function on the quality of life of Korean adults by age group. Korean J. Health Serv. Manag. 2016, 10, 99–110. [Google Scholar] [CrossRef]
- Lee, M.-R.; Choi, J.-S. Relationship of self-perceived symptoms of periodontal disease to quality of life in adults. J. Dent. Hyg. Sci. 2012, 12, 115–121. [Google Scholar]
- Lee, J.-Y.; Kim, G.-P.; Yu, B.-C. Relationship between periodontal diseases and quality of life. J. Korean Soc. Dent. Hyg. 2013, 13, 835–843. [Google Scholar] [CrossRef]
- Park, M.-S.; Jang, J.-H. Relationship between health risk behaviors, oral health-related quality of life (OHIP-14) and happiness in soldiers. J. Korean Soc. Dent. Hyg. 2017, 17, 1159–1169. [Google Scholar]
- Grecu, A.G.; Balazsi, R.; Dudea, D.; Mesaro, A.; Strmbu, M.; Dumitracu, D.L. Oral health related quality of life and self-esteem in a general population. Med. Pharm. Rep. 2019, 92, S65–S72. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.-N.; Lee, M.-R. Main Cause of influencing oral health impact profile (OHIP) and self-esteem of orthodontic patients. J. Korean Soc. Dent. Hyg. 2010, 10, 513–522. [Google Scholar]
- Belusic Gobic, M.; Kralj, M.; Harmicar, D.; Cerovic, R.; Mady Maricic, B.; Spalj, S. Dentofacial deformity and orthognatic surgery: Influence on self-esteem and aspects of Qqality of life. J. Craniomaxillofac. Surg. 2021, 49, 277–281. [Google Scholar] [CrossRef]
- United Nations (UN). Available online: https://treaties.un.org/Pages/ViewDetails.aspx?src=TREATY&mtdsg_no=IV-4&chapter=4&clang=_en (accessed on 21 September 2022).
- Chun, J.H. A Study on correctional medical treatment for disabled prisoners and sick prisoners. Correct. Welf. Soc. Korea 2021, 73, 175–202. [Google Scholar] [CrossRef]
- Hwang, I.; Park, H.-K. Dental public health Doctors’ awareness of dental services in Korean correctional institutions. J. Korean Dent. Assoc. 2022, 60, 72–84. [Google Scholar]
- Lee, S.-G.; Sun, J.-G.; Park, I.-K.; Kang, H.-H.; Kim, S.-Y.; Sohn, M.-S. Correctional health care delivery system and prisoners’ human rights. Korean J. Med. Law 2009, 17, 121–150. [Google Scholar]
- Park, Y.-K. Medical treatment for prisoners. Correct. Rev. 2010, 48, 73–104. [Google Scholar]
- Briggs, M.S.; Kolbus, E.S.; Patterson, K.M.; Harmon-Matthews, L.E.; McGrath, S.; Quatman-Yates, C.C.; Meirelles, C.; Salsberry, M.J. Role of oral intake, mobility, and activity measures in informing discharge recommendations for hospitalized inmate and noninmate patients with COVID-19: Retrospective analysis. JMIR Rehabil. Assist. Technol. 2023, 10, e43250. [Google Scholar] [CrossRef]
- Novais, A.; Fac, C.; Allouche, M.; Atallah, É.; Godkine, N.; Guyader, T.; Hariga, A.; Hoarau, W.; Oulmi, A.; Trumbic, F.; et al. Télédent, an oral tele-expertise experience in a penitentiary environment. Med. Sci. 2019, 35, 866–870. [Google Scholar] [CrossRef]
- Inquimbert, C.; Balacianu, I.; Huyghe, N.; Pasdeloup, J.; Tramini, P.; Meroueh, F.; Montal, S.; Bencharit, S.; Giraudeau, N. Applications of teledentistry in a French inmate population: A one-year observational study. PLoS ONE 2021, 16, e0247778. [Google Scholar] [CrossRef] [PubMed]
| Variables | Division | N (%) | OHIP-14 | |
|---|---|---|---|---|
| M ± SD | p-Value * | |||
| Age (years) | 20–29 a | 37 (10.2) | 46.86 ± 10.57 | < 0.001 |
| 30–39 ab | 80 (22.0) | 43.60 ± 10.84 | ||
| 40–49 bc | 85 (23.4) | 39.84 ± 13.39 | ||
| 50–59 c | 99 (27.3) | 36.15 ± 12.07 | ||
| ≥ 60 c | 62 (17.1) | 36.39 ± 11.28 | ||
| EDT (for last year) | Yes | 110 (30.3) | 38.26 ± 13.39 | 0.265 |
| No | 246 (67.8) | 40.59 ± 12.06 | ||
| Do not know | 7 (1.9) | 39.71 ± 4.79 | ||
| EDE (for last year) | Yes | 145 (39.8) | 41.19 ± 12.04 | 0.247 |
| No | 214 (59.0) | 38.96 ± 12.70 | ||
| Do not know | 5 (1.4) | 40.60 ± 5.59 | ||
| Toothbrushing time (min) | <1 a | 51 (14.01) | 37.12 ± 12.37 | 0.020 |
| 1 to less than 2 ab | 126 (34.62) | 38.10 ± 13.06 | ||
| 2 to less than 3 b | 121 (33.24) | 41.87 ± 10.84 | ||
| ≥3 b | 66 (18.13) | 41.73 ± 13.12 | ||
| Use of fluoride toothpaste | Use | 173 (47.92) | 39.90 ± 11.89 | 0.432 |
| Do not use | 73 (20.22) | 38.60 ± 11.67 | ||
| Do not know | 115 (31.86) | 40.97 ± 13.15 | ||
| Chewing discomfort | Tofu and Rice a | 21 (5.8) | 25.81 ± 13.04 | <0.001 |
| Apple a | 9 (2.5) | 26.22 ± 15.47 | ||
| Kimchi ab | 36 (10.0) | 29.06 ± 12.80 | ||
| Meat bc | 61 (16.9) | 37.30 ± 90.4 | ||
| Dried squid bc | 29 (8.1) | 36.45 ± 11.53 | ||
| Hard candy c | 204 (56.7) | 45.46 ± 8.80 | ||
| Subjective health | Strongly disagree a | 56 (15.38) | 26.41 ± 13.86 | <0.001 |
| Disagree b | 93 (25.55) | 36.47 ± 10.17 | ||
| Neutral bc | 123 (33.79) | 43.22 ± 8.95 | ||
| Agree c | 82 (22.53) | 46.89 ± 9.38 | ||
| Strongly agree c | 10 (2.75) | 48.10 ± 12.77 | ||
| Subjective oral health | Strongly disagree a | 78 (21.49) | 27.77 ± 13.58 | <0.001 |
| Disagree b | 130 (35.81) | 38.68 ± 9.78 | ||
| Neutral bc | 117 (32.23) | 46.01 ± 8.00 | ||
| Agree bc | 34 (9.37) | 49.26 ± 7.57 | ||
| Strongly agree c | 4 (1.10) | 54.75 ± 1.89 | ||
| Self-esteem | High | 49 (13.39) | 41.10 ± 15.64 | 0.547 |
| Usual | 252 (68.85) | 40.12 ± 11.97 | ||
| Low | 65 (17.76) | 38.65 ± 10.55 | ||
| Total | 376 (100.0) | 39.90 ± 12.38 | ||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Food impaction | 1 | |||||||||
| 2. Sensitivity to cold/hot | 0.492 ** | 1 | ||||||||
| 3. Periodontal health | 0.434 ** | 0.566 ** | 1 | |||||||
| 4. Malodour | 0.373 ** | 0.507 ** | 0.633 ** | 1 | ||||||
| 5. Dry mouth | 0.316 ** | 0.446 ** | 0.499 ** | 0.622 ** | 1 | |||||
| 6. Trouble biting/chewing | 0.366 ** | 0.570 ** | 0.555 ** | 0.520 ** | 0.514 ** | 1 | ||||
| 7. TMJ disorder | 0.176 ** | 0.340 ** | 0.386 ** | 0.431 ** | 0.426 ** | 0.447 ** | 1 | |||
| 8. Toothache | 0.318 ** | 0.509 ** | 0.548 ** | 0.536 ** | 0.520 ** | 0.628 ** | 0.583 ** | 1 | ||
| 9. Self-esteem | 0.018 | 0.008 | −0.050 | −0.114 * | −0.063 | −0.040 | −0037 | −0.023 | 1 | |
| 10. OHIP-14 | −0.338 ** | −0.546 ** | −0.570 ** | −0.552 ** | −0.523 ** | −0.749 ** | −0.488 ** | −0.649 ** | 0.057 | 1 |
| Model 1 | Model 2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | ß | t | p-Value * | B | SE | ß | t | p-Value * | |
| (Constant) | 20.705 | 2.998 | 6.905 | <0.001 | 53.394 | 3.381 | 15.790 | <0.001 | ||
| Age | −0.093 | 0.038 | −0.099 | −2.436 | 0.015 | −0.138 | 0.031 | −0.146 | −4.412 | <0.001 |
| Subjective health | 2.259 | 0.597 | 0.200 | 3.785 | <0.001 | 1.482 | 0.471 | 0.131 | 3.146 | 0.002 |
| Subjective oral health | 3.493 | 0.676 | 0.278 | 5.168 | <0.001 | 0.755 | 0.570 | 0.060 | 1.326 | 0.186 |
| Chewing discomfort (ref. = tofu and rice) | ||||||||||
| Apple | −2.735 | 3.569 | −0.034 | −0.766 | 0.444 | −4.808 | 2.809 | −0.060 | −1.712 | 0.088 |
| Kimchi | 3.100 | 2.400 | 0.077 | 1.292 | 0.197 | 0.273 | 1.908 | 0.007 | 0.143 | 0.886 |
| Meat | 8.629 | 2.207 | 0.270 | 3.910 | <0.001 | 3.196 | 1.778 | 0.100 | 1.798 | 0.073 |
| Squid | 5.675 | 2.548 | 0.126 | 2.228 | 0.027 | 1.279 | 2.041 | 0.028 | 0.627 | 0.531 |
| Candy | 12.665 | 2.080 | 0.522 | 6.089 | <0.001 | 4.255 | 1.768 | 0.175 | 2.407 | 0.017 |
| Perceived oral symptoms | ||||||||||
| Food impaction | 0.212 | 0.423 | 0.018 | 0.502 | 0.616 | |||||
| Sensitivity to cold/hot | 0.400 | 0.429 | 0.039 | 0.931 | 0.353 | |||||
| Periodontal health | −0.936 | 0.463 | −0.089 | −2.021 | 0.044 | |||||
| Malodour | −1.423 | 0.481 | −0.131 | −2.957 | 0.003 | |||||
| Dry mouth | −0.008 | 0.425 | −0.001 | −0.018 | 0.985 | |||||
| Trouble biting/chewing | −2.735 | 0.429 | −0.307 | −6.376 | <0.001 | |||||
| TMJ disorder | −1.086 | 0.409 | −0.099 | −2.656 | 0.008 | |||||
| Toothache | −1.687 | 0.491 | −0.154 | −3.439 | 0.001 | |||||
| F (p-Value) | 44.754 (<0.001) | 51.631 (<0.001) | ||||||||
| R2 | 0.511 | 0.711 | ||||||||
| Adj. R2 | 0.499 | 0.698 | ||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoon, H.-S.; Kim, K.-S.; Jang, J.-H. Factors Related to Oral-Health-Related Quality of Life in Adult Male Inmates: A Cross-Sectional Study. Healthcare 2023, 11, 2848. https://doi.org/10.3390/healthcare11212848
Yoon H-S, Kim K-S, Jang J-H. Factors Related to Oral-Health-Related Quality of Life in Adult Male Inmates: A Cross-Sectional Study. Healthcare. 2023; 11(21):2848. https://doi.org/10.3390/healthcare11212848
Chicago/Turabian StyleYoon, Hae-Soo, Kyoung-Seon Kim, and Jong-Hwa Jang. 2023. "Factors Related to Oral-Health-Related Quality of Life in Adult Male Inmates: A Cross-Sectional Study" Healthcare 11, no. 21: 2848. https://doi.org/10.3390/healthcare11212848
APA StyleYoon, H.-S., Kim, K.-S., & Jang, J.-H. (2023). Factors Related to Oral-Health-Related Quality of Life in Adult Male Inmates: A Cross-Sectional Study. Healthcare, 11(21), 2848. https://doi.org/10.3390/healthcare11212848







