Fair Healthcare Practices in Orthopedics Assessed with a New Framework
Abstract
1. Introduction
2. Materials and Methods
- Defining the domains of the new sustainable development framework in which fair healthcare practices are integrated;
- Studying scientific literature from relevant databases and extracting the most recent healthcare practices reported by healthcare facilities around the world;
- Elaborating on the content and evaluation grids of the indicators that describe fair healthcare practices;
- Integrating indicators related to fair healthcare practices in the matrix of the new framework for sustainable development;
- Practically validating indicators related to fair healthcare practices at an orthopedic field hospital.
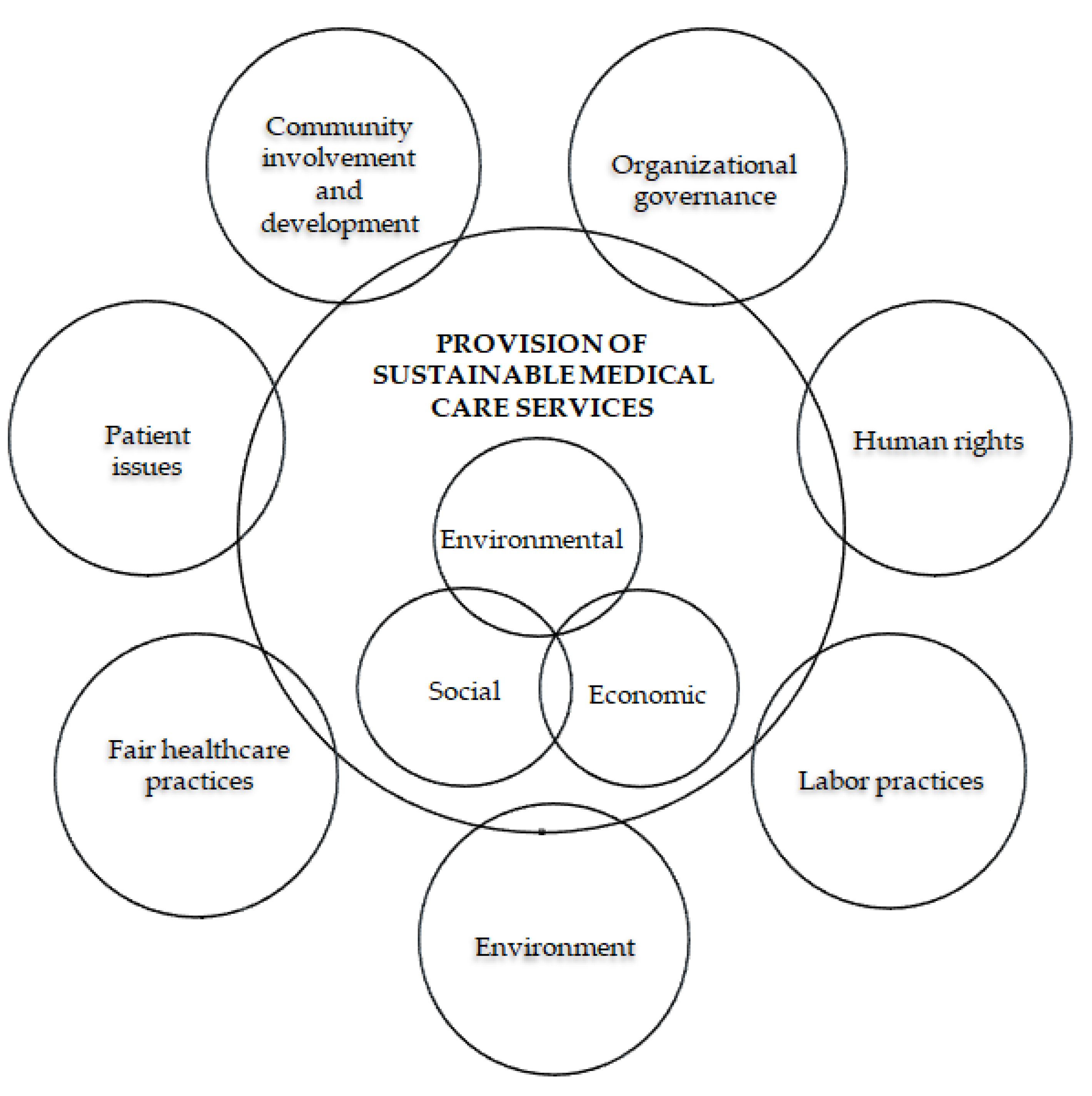
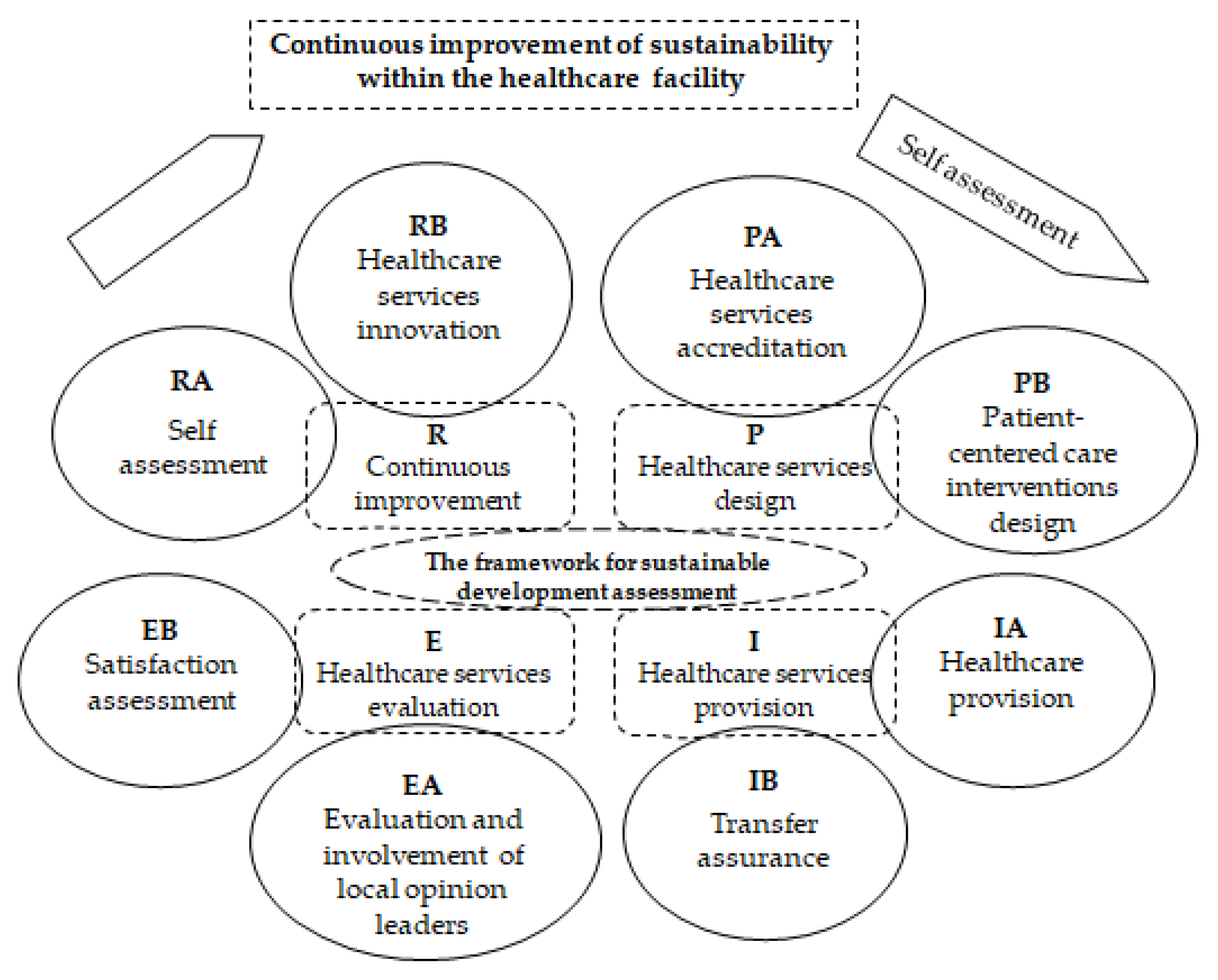
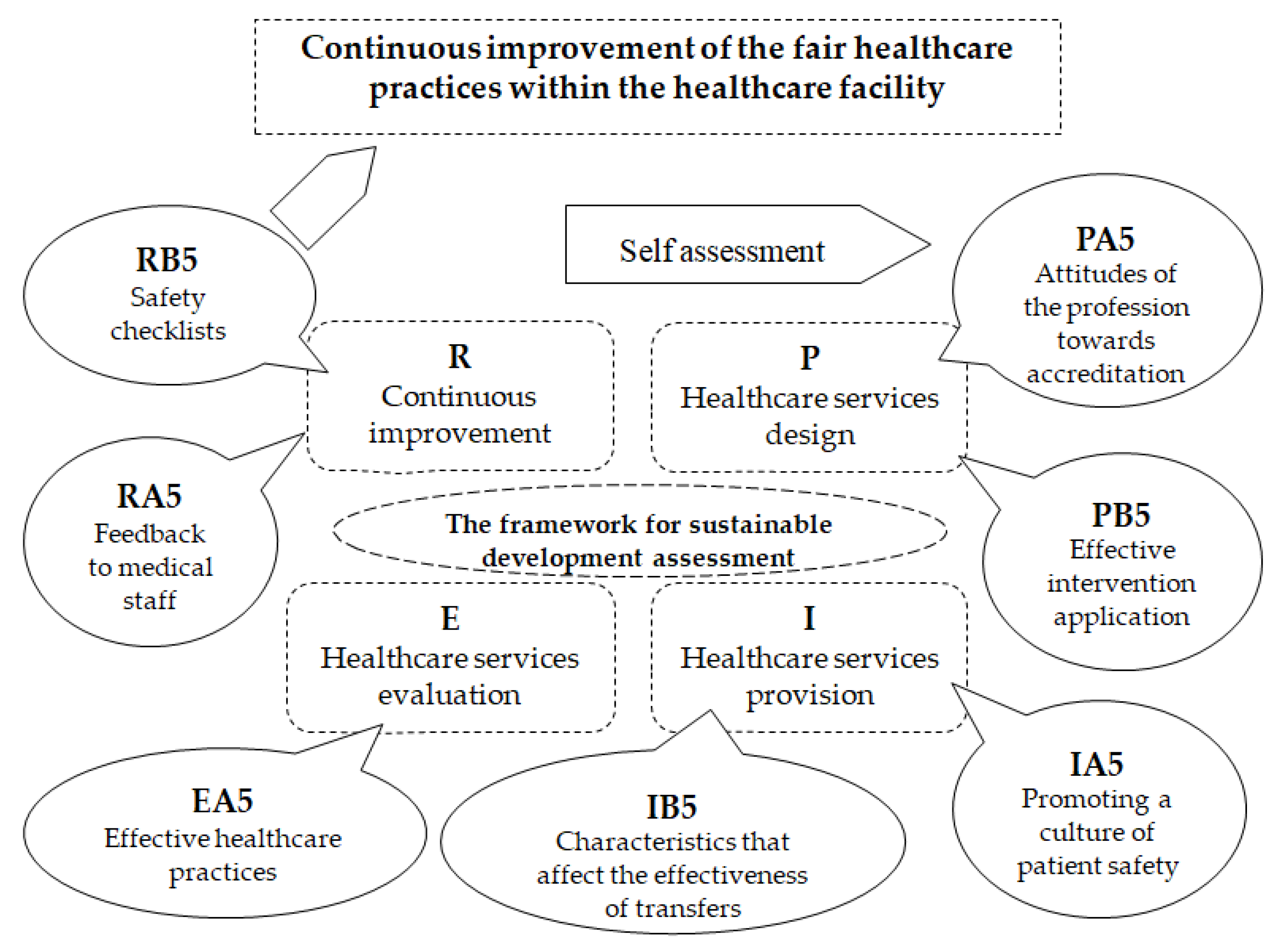
The Reference Framework Areas
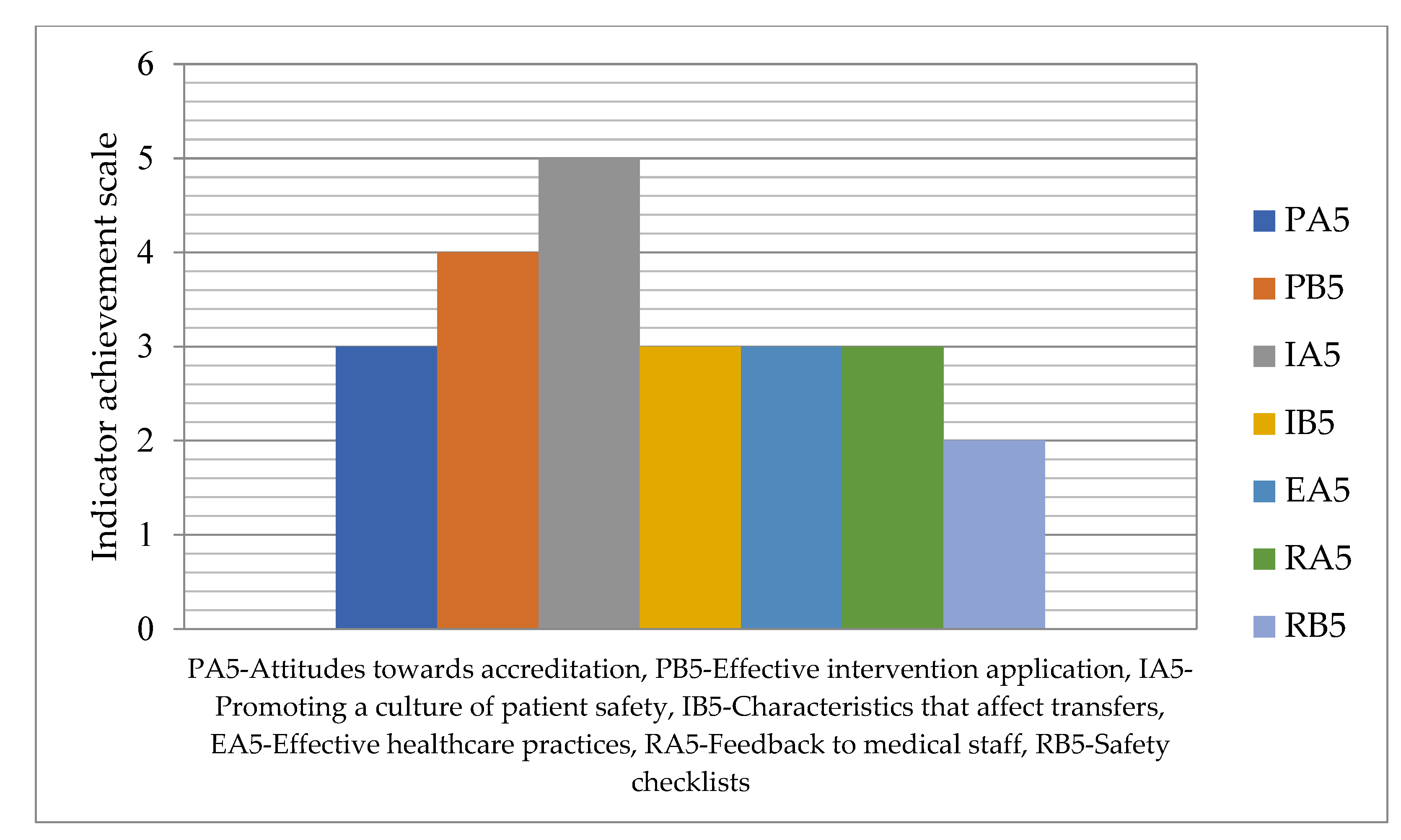
3. Results
3.1. Evidence of Fair Healthcare Practices in Healthcare Organizations
3.1.1. Indicators for Healthcare Services Design
3.1.2. Indicators for Healthcare Services Provision
3.1.3. Indicators for Healthcare Services Evaluation
3.1.4. Indicators for Continuous Improvement
3.2. Indicators Description and the Evaluation Model
3.3. Indicator Matrix
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Indicator | PA5—Attitudes of the Profession towards Accreditation |
|---|---|
| Description | The attitudes of the profession towards accreditation have an impact on its successful implementation. The attitudes of the profession towards accreditation are determined by:
|
| Evaluation question | Is a culture of quality created in the healthcare facility? Are staff consulted on the impact of accreditation on the quality of medical services provided? Is the impact of accreditation on the organization’s performance assessed? Are difficulties in data collection and system maintenance identified against accreditation standards? Are measures taken to reduce red tape, time consumption, and costs in accreditation activities? Are decisions made collegially? |
| Score [A] | Achievement | Content |
|---|---|---|
| 0 | Not relevant | — |
| 1 | Low | Staff consultations are periodically organized regarding the assessment of the impact of accreditation on the quality of the medical services offered. |
| 2 | Satisfactory | An organizational culture oriented towards quality is created in the healthcare facility. The values and mission of the healthcare facility are defined and based on a plan, they are accepted, assumed, and promoted at the behavioral level by all members of the organization. |
| 3 | Good | Difficulties in data collection and system maintenance against accreditation standards are identified and corrective actions are formulated. |
| 4 | Very good | Measures are taken to reduce bureaucracy, time consumption, and costs in accreditation activities, and decisions are made collegially. |
| 5 | Excellent | The impact of accreditation on the organization’s performance is assessed and an improvement plan is developed. |
| Indicator | PB5—Effective Intervention Application |
|---|---|
| Description | Applying consultation interventions that have clear positive effects on patients:
|
| Evaluation questions | Do medical interventions consider psychological distress? Does the patient’s medical consultation look at all health problems? Is disease-specific information provided to the patient? Is the communication behavior of medical personnel focused on the patient? Do medical staff empathize with patients? Do the collected data involve the skills of healthcare professionals? Are medical decisions made with patient involvement? |
| Score [A] | Achievement | Content |
|---|---|---|
| 0 | Not relevant | — |
| 1 | Low | At the patient’s medical consultation, the patient’s psychological suffering is also assessed, and this is taken into account during medical interventions. |
| 2 | Satisfactory | At the patient’s medical consultation, all his health problems are analyzed. |
| 3 | Good | After diagnosis, the patient is provided with information specific to the disease. |
| 4 | Very good | The communication behavior of medical personnel is focused on the patient, and they empathize with patients. |
| 5 | Excellent | Medical professionals use various data collection skills, and medical decisions are made through patient involvement. |
| Indicator | IA5—Promoting a Culture of Patient Safety |
|---|---|
| Description | Promoting a positive patient safety culture in all departments of the healthcare facility, which ensures appropriate values, attitudes, and behaviors regarding patient safety, is an important strategy that supports the improvement of healthcare system performance. Different activities can be used, such as:
|
| Evaluation questions | Are there cultivated values, attitudes, and behaviors regarding patient safety? Are educational sessions organized for the development of personal action plans regarding employee behavior at work, employee well-being, job satisfaction, organizational commitment? Are organizational culture change actions (e.g., administrative activities) planned regarding specific safety behavior (e.g., hand washing frequency and nosocomial infection rate)? Is team training provided that contains packages of structured methods for optimizing teamwork processes? For example: Communication, cooperation, collaboration, and leadership are assessed. Are representative function support visits conducted where managers or senior leaders visit frontline patient care areas to observe and discuss current or potential patient safety threats? During the visits, are frontline staff supported in addressing these threats? Is patient safety culture a component of organizational culture? |
| Score [A] | Achievement | Content |
|---|---|---|
| 0 | Not relevant | — |
| 1 | Low | A positive culture that ensures appropriate patient safety values, attitudes, and behaviors is promoted in all departments of the healthcare facility. |
| 2 | Satisfactory | Educational sessions are organized for the development of personal action plans regarding employee behavior at work, employee well-being, job satisfaction, and organizational commitment. |
| 3 | Good | To promote a culture of patient safety, actions aimed at changing the organizational culture regarding specific safety behavior are provided. Such actions can be administrative in nature, such as the frequency of hand washing, the rate of nosocomial infections, etc. |
| 4 | Very good | In order to promote a culture of patient safety, team trainings containing packages of structured methods for optimizing teamwork processes are provided. Patient safety culture is a component of organizational culture. |
| 5 | Excellent | To promote a culture of patient safety, representative function support visits are conducted where managers or senior leaders visit frontline patient care areas to observe and discuss current or potential patient safety threats. The patient safety culture is part of the healthcare facility’s strategy that supports improving the performance of the healthcare system. |
| Indicator | IA5—Characteristics that Affect the Effectiveness of Transfers |
|---|---|
| Description | Characteristics that may hinder or complicate the effectiveness of transfer interventions and need to be assessed are:
|
| Evaluation questions | Is multitasking of emergency department clinicians evaluated in the effectiveness of handover interventions? Is the influence of workload unpredictability on staff availability planning assessed? For example, recovery rooms are evaluated. Are the difficulties that arise in the exchange of information between departments assessed? Is the extent to which effective communication is hindered by lack of critical care knowledge assessed? Is the functional diversity of care teams ensured? Are longer-term in-hospital and outpatient transfer interventions evaluated to have measurable effects? For example, the effects are evaluated after 3 months. Are the effects of transfers quantified in specific patient subgroups in which data can be obtained? Are the effects of transfers evaluated for higher intensities that allow relevant data to be collected? |
| Score [A] | Achievement | Content |
|---|---|---|
| 0 | Not relevant | — |
| 1 | Low | Critical care knowledge gaps that prevent effective communication, as well as difficulties in sharing information between departments, are assessed, and steps are taken to ensure that these do not impede or complicate the effectiveness of handover interventions. |
| 2 | Satisfactory | Unpredictability of workload is assessed, and functional diversity of care teams is ensured through appropriate planning of staff availability. |
| 3 | Good | Multitasking of emergency department clinicians is assessed, and steps are taken to ensure that it does not impede or complicate the effectiveness of handover interventions. |
| 4 | Very good | The time period after which the effects of intrahospital transfer and discharge interventions can be measured is determined. |
| 5 | Excellent | Patient subgroups for which intrahospital transfer interventions can be quantified are determined. The effectiveness of in-hospital transfer and discharge interventions is evaluated and the intensity for which they are effective is determined. |
| Indicator | EA5—Effective Healthcare Practices |
|---|---|
| Description | The work of local opinion leaders is more effective when combined with other complementary interventions, for example:
|
| Evaluation questions | Is the activity of local opinion leaders combined with other complementary interventions? Are the following evaluated, for example: reminders; audits and feedback; awareness visits; marketing strategies; local consensus processes; patient-mediated interventions. |
| Score [A] | Achievement | Content |
|---|---|---|
| 0 | Not relevant | — |
| 1 | Low | The activity of local opinion leaders is combined with reminders. |
| 2 | Satisfactory | The activity of local opinion leaders is combined with outreach visits. |
| 3 | Good | The activity of local opinion leaders is combined with local consensus processes. |
| 4 | Very good | The activity of local opinion leaders is combined with audit and feedback activities that allow for the formulation of corrective actions. |
| 5 | Excellent | The activity of local opinion leaders is included in marketing strategies and has the effect of improving healthcare services. |
| Indicator | RA5—Feedback to Medical Staff |
|---|---|
| Description | Communicating the results of the evaluation to all employees guarantees responsibility, transparency, and honesty in the organization, which is a key factor for achieving correct institutional practices. |
| Evaluation questions | How are the results of self-assessments communicated to all staff? |
| Score [A] | Achievement | Content |
|---|---|---|
| 0 | Not relevant | — |
| 1 | Low | The results of the evaluations are communicated verbally to the heads of departments. |
| 2 | Satisfactory | The results of the evaluations are communicated in writing to the heads of departments. |
| 3 | Good | The results of the evaluations are communicated by the heads of departments to the subordinate staff. |
| 4 | Very good | All staff are informed of the evaluations results and are aware of the improvement tasks that fall upon them as a result of the evaluations carried out. |
| 5 | Excellent | Communicating assessment results to all employees ensures accountability, transparency, and honesty in the healthcare facility and ensures fair institutional practices. |
| Indicator | RB5—Safety Checklists |
|---|---|
| Description | Safety checklists, also known as medical checklists, are a tool for improving care processes and patient safety outcomes. Safety checklists can vary in structure, content, and method of implementation. The safety checklists suggest some improvements in patient safety resulting from their use by healthcare teams, particularly in terms of:
|
| Evaluation questions | Are safety checklists used in medical practice? Is the design and implementation of safety checklists based on an evidence-based approach? Are checklists pilot tested and validated prior to actual use to ensure that the checklists contain all relevant elements and are consistently interpreted by users? Is medical staff trained in the correct use and compliance of checklists? What is the frequency of training? |
| Score [A] | Achievement | Content |
|---|---|---|
| 0 | Not relevant | — |
| 1 | Low | Safety checklists are used in medical practice. |
| 2 | Satisfactory | An evidence-based approach is applied to the design and implementation of safety checklists. |
| 3 | Good | Before actual use, checklists are pilot tested and validated to ensure they contain all relevant elements and are consistently interpreted by users. |
| 4 | Very good | Medical staff members are frequently trained in the proper use and compliance of checklists. |
| 5 | Excellent | The use of safety checklists results in improvements in patient safety as a result of improved compliance in healthcare processes, reduced lengths of stay in intensive care or emergency rooms, reduced surgical complications, improved antibiotic administration. |
References
- Yang, A.; Farmer, P.; McGahan, A. ‘Sustainability’ in global health. Glob. Public Health 2010, 5, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Bauzon, S. Classical distributive justice and the European healthcare system: Rethinking the foundations of European health care in an age of crises. J. Med. Philos. 2015, 40, 190–200. [Google Scholar] [PubMed]
- Ferdynus, M.P. Is it true that all human beings have dignity? Nurs. Philos. 2023. [Google Scholar] [CrossRef]
- Gantsho, L.; Wareham, C.S. Medical Cosmopolitanism: The global extension of justice in healthcare practice. Dev. World Bioeth. 2021, 21, 131–138. [Google Scholar] [CrossRef]
- Rosenberger, M. Kann Rationierung fair sein? Ethische Uberlegungen zur Gerechtigkeit im Gesundheitssystem [Can rationing be fair? Ethical considerations regarding justice in the healthcare system]. Z. Arztl. Fortbild. Qualitatssich. 2007, 101, 356–361. [Google Scholar]
- Leung, T.I.; Dumontier, M. FAIR Principles for Clinical Practice Guidelines in a Learning Health System. Stud. Health Technol. Inform. 2019, 264, 1690–1691. [Google Scholar]
- Wilkinson, M.D.; Dumontier, M.; Aalbersberg, I.J.; Appleton, G.; Axton, M.; Baak, A.; Blomberg, N.; Boiten, J.W.; da Silva Santos, L.B.; Bourne, P.E.; et al. The FAIR Guiding Principles for scientific data management and stewardship. Sci. Data 2016, 3, 160018. [Google Scholar]
- Fritz, Z.; Cox, C.L. Integrating philosophy, policy and practice to create a just and fair health service. J. Med. Ethics 2020, 46, 797–802. [Google Scholar]
- Jansen, M.P.; Helderman, J.K.; Boer, B.; Baltussen, R. Fair Processes for Priority Setting: Putting Theory into Practice Comment on “Expanded HTA: Enhancing Fairness and Legitimacy”. Int. J. Health Policy Manag. 2017, 6, 43–47. [Google Scholar] [CrossRef][Green Version]
- Malone, S.; Prewitt, K.; Hackett, R.; Lin, J.C.; McKay, V.; Walsh-Bailey, C.; Luke, D.A. The Clinical Sustainability Assessment Tool: Measuring organizational capacity to promote sustainability in healthcare. Implement. Sci. Commun. 2021, 2, 77. [Google Scholar]
- Lennox, L.; Maher, L.; Reed, J. Navigating the sustainability landscape: A systematic review of sustainability approaches in healthcare. Implement. Sci. 2018, 13, 27. [Google Scholar] [CrossRef] [PubMed]
- Shigayeva, A.; Coker, R.J. Communicable disease control programmes and health systems: An analytical approach to sustainability. Health Policy Plan. 2015, 30, 368–385. [Google Scholar] [CrossRef] [PubMed]
- Scheirer, M.A.; Dearing, J.W. An agenda for research on the sustainability of public health programs. Am. J. Public Health 2011, 101, 2059–2067. [Google Scholar] [CrossRef]
- Isaksson, R. Total quality management for sustainable development: Process based system models. Bus. Process Manag. J. 2006, 12, 632–645. [Google Scholar] [CrossRef]
- Zdravkovic, D.; Radukic, S. Institutional framework for sustainable development in Serbia. Montenegrin J. Econ. 2012, 8, 27–36. [Google Scholar]
- Moldovan, F.; Blaga, P.; Moldovan, L.; Bataga, T. An Innovative Framework for Sustainable Development in Healthcare: The Human Rights Assessment. Int. J. Environ. Res. Public Health 2022, 19, 2222. [Google Scholar] [CrossRef]
- ISO 26000:2010; Guidance on Social Responsibility. ISO: Geneva, Switzerland, 2010. Available online: https://www.iso.org/standard/42546.html (accessed on 9 September 2023).
- Groene, O.; Kringos, D.; Sunol, R.; On Behalf of the DUQuE Project. Seven Ways to Improve Quality and Safety in Hospitals. An Evidence-Based Guide. DUQuE Collaboration. 2014. Available online: www.duque.eu (accessed on 9 September 2023).
- ANMCS. Standarde de Acreditare Unitatilor Sanitare cu Paturi si Liste de Verificare (Accreditation standards for Sanitary Units with Beds and Checklists). Available online: https://anmcs.gov.ro/web/acreditarea-spitalelor/standarde-de-acreditare/ (accessed on 9 September 2023).
- ANMCS. Standardele Autoritatii Nationale de Management al Calitatii in Sanatate Pentru Serviciile de Sanatate Acordate in Regim Ambulatoriu (Standards of the National Authority for Quality Management in Health for Outpatient Health Services). Available online: https://anmcs.gov.ro/web/standarde-ambulatoriu/ (accessed on 9 September 2023).
- ISO 9001:2015; Quality Management Systems—Requirements. ISO: Geneva, Switzerland, 2015. Available online: https://www.iso.org/standard/62085.html (accessed on 9 September 2023).
- Oliveira, J.L.; Gabriel, C.S.; Fertonani, H.P.; Matsuda, L.M. Management changes resulting from hospital accreditation. Rev. Lat. Am. Enfermagem. 2017, 25, e2851. [Google Scholar] [CrossRef]
- Ng, K.B.; Leung, G.K.K.; Johnston, J.M.; Cowling, B.J. Factors affecting implementation of accreditation programmes and the impact of the accreditation process on quality improvement in hospitals: A SWOT analysis. Hong Kong Med. J. 2013, 19, 434–446. [Google Scholar] [CrossRef]
- Avia, I.; Hariyati, R.T.S. Impact of hospital accreditation on quality of care: A literature review. Enferm. Clin. 2019, 29, 315–320. [Google Scholar] [CrossRef]
- Andres, E.B.; Song, W.; Schooling, C.M.; Johnston, J.M. The influence of hospital accreditation: A longitudinal assessment of organisational culture. BMC Health Serv. Res. 2019, 19, 467. [Google Scholar] [CrossRef]
- Greenfield, D.; Braithwaite, J. Health sector accreditation research: A systematic review. Int. J. Qual. Health 2008, 20, 172–183. [Google Scholar] [CrossRef] [PubMed]
- Flodgren, G.; Pomey, M.P.; Taber, S.A.; Eccles, M.P. Effectiveness of external inspection of compliance with standards in improving healthcare organisation behaviour, healthcare professional behaviour or patient outcomes. Cochrane Database Syst. Rev. 2011, 11, CD008992. [Google Scholar]
- Ehlers, L.H.; Jensen, M.B.; Simonsen, K.B.; Rasmussen, G.S.; Braithwaite, J. Attitudes towards accreditation among hospital employees in Denmark: A cross-sectional survey. Int. J. Qual. Health Care 2017, 29, 693–698. [Google Scholar] [CrossRef] [PubMed]
- Kakemam, E.; Rajabi, M.R.; Raeissi, P.; Ehlers, L.H. Attitudes Towards Accreditation and Quality Improvement Activities Among Hospital Employees in Iran: A Quantitative Study. J. Multidiscip. Healthc. 2020, 13, 799–807. [Google Scholar] [CrossRef]
- Vincent, H.K.; Horodyski, M.; Vincent, K.R.; Brisbane, S.T.; Sadasivan, K.K. Psychological Distress After Orthopedic Trauma: Prevalence in Patients and Implications for Rehabilitation. PM&R 2015, 7, 978–989. [Google Scholar]
- Kirven, J.C.; Everhart, J.S.; DiBartola, A.C.; Jones, J.; Flanigan, D.C.; Harrison, R. Interventional Efforts to Reduce Psychological Distress After Orthopedic Trauma: A Systematic Review. HSS J. 2020, 16, 250–260. [Google Scholar] [CrossRef]
- Coventry, P.A.; Meader, N.; Melton, H.; Temple, M.; Dale, H.; Wright, K.; Cloitre, M.; Karatzias, T.; Bisson, J.; Roberts, N.P.; et al. Psychological and pharmacological interventions for posttraumatic stress disorder and comorbid mental health problems following complex traumatic events: Systematic review and component network meta-analysis. PLoS Med. 2020, 17, e1003262. [Google Scholar] [CrossRef]
- Melton, H.; Meader, N.; Dale, H.; Wright, K.; Jones-Diette, J.; Temple, M.; Shah, I.; Lovell, K.; McMillan, D.; Churchill, R.; et al. Interventions for adults with a history of complex traumatic events: The INCiTE mixed-methods systematic review. Health Technol. Assess. 2020, 24, 1–312. [Google Scholar] [CrossRef]
- Wichman, D.; Rasio, J.P.; Looney, A.; Nho, S.J. Physical Examination of the Hip. Sports Health 2021, 13, 149–153. [Google Scholar] [CrossRef]
- Hoang, V.; Parekh, A.; Sagers, K.; Call, T.; Howard, S.; Hoffman, J.; Lee, D. Patient Utilization of Online Information and its Influence on Orthopedic Surgeon Selection: Cross-sectional Survey of Patient Beliefs and Behaviors. JMIR Form. Res. 2022, 6, e22586. [Google Scholar] [CrossRef]
- Wei, N.; Du, Y.; Chen, S. Application of Doctor-Nurse-Patient Co-Decision-Making Nursing Intervention Based on Evidence-Based Problems in the Rehabilitation of Acute Ankle Lateral Collateral Ligament Injury. Emerg. Med. Int. 2022, 2022, 2363230. [Google Scholar] [CrossRef] [PubMed]
- Kohlhof, H.; Marquardt, G.; Wirtz, D.C. Organisation und Klinikstruktur für die integrierte Betreuung orthogeriatrischer Patienten [Organizational and hospital structure for the integrated care of orthogeriatic patients]. Orthopade 2022, 51, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Sabharwal, S.; Lin, C.; Weistroffer, J.K.; LaPorte, D.M.; the Collaborative Orthopaedic Educational Research Group. Empathy Among Orthopaedic Surgery Trainees. JBJS Open Access 2021, 6, e21.00041. [Google Scholar] [CrossRef] [PubMed]
- Magaway, C.L.; Malanga, G. Patient registries in orthopedics and orthobiologic procedures: A narrative review. BMC Musculoskelet. Disord. 2022, 23, 543. [Google Scholar] [CrossRef]
- Panesar, S.S.; Mirza, S.B.; Madhok, R. Patient Saf. Orthop: Are We Doing Enough? Orthopedics 2011, 34, 82–83. [Google Scholar] [CrossRef]
- Scott, T.; Mannion, R.; Marshall, M.; Davies, H. Does organisational culture influence health care performance? A review of the evidence. J. Health Serv. Res. Policy 2003, 8, 105–117. [Google Scholar] [CrossRef]
- Rocha, E.S.; Trevizan, M.A. Quality management at a hospital’s nursing service. Rev. Lat.-Am. Enferm. 2009, 17, 240–245. [Google Scholar] [CrossRef]
- Weaver, S.J.; Lubomski, L.H.; Wilson, R.F.; Pfoh, E.R.; Martinez, K.A.; Dy, S.M. Promoting a culture of safety as a patient safety strategy: A systematic review. Ann. Intern. Med. 2013, 158 Pt 2, 369–374. [Google Scholar] [CrossRef]
- Bradley, E.H.; Brewster, A.L.; McNatt, Z.; Linnander, E.L.; Cherlin, E.; Fosburgh, H.; Ting, H.H.; Curry, L.A. How guiding coalitions promote positive culture change in hospitals: A longitudinal mixed methods interventional study. BMJ Qual. Saf. 2018, 27, 218–225. [Google Scholar] [CrossRef]
- Morello, R.T.; Lowthian, J.A.; Barker, A.L.; McGinnes, R.; Dunt, D.; Brand, C. Strategies for improving patient safety culture in hospitals: A systematic review. BMJ Qual. Saf. 2013, 22, 11–18. [Google Scholar] [CrossRef]
- Parmelli, E.; Flodgren, G.; Beyer, F.; Baillie, N.; Schaafsma, M.E.; Eccles, M.O. The effectiveness of strategies to change organisational culture to improve healthcare performance: A systematic review. Implement. Sci. 2011, 6, 33. [Google Scholar] [CrossRef]
- Curry, L.A.; Brault, M.A.; Linnander, E.L.; McNatt, Z.; Brewster, A.L.; Cherlin, E.; Flieger, S.P.; Ting, H.H.; Bradley, E.H. Influencing organisational culture to improve hospital performance in care of patients with acute myocardial infarction: A mixed-methods intervention study. BMJ Qual. Saf. 2018, 27, 207–217. [Google Scholar] [CrossRef]
- Azar, F.M. Quality, Value, and Patient Safety in Orthopedic Surgery. Orthop. Clin. N. Am. 2018, 49, xvii. [Google Scholar] [CrossRef]
- Braet, A.; Weltens, C.; Sermeus, W. Effectiveness of discharge interventions from hospital to home on hospital readmissions: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2016, 14, 106–173. [Google Scholar] [CrossRef] [PubMed]
- Bracey, J.; Morell, S.; Tait, M.; Frazier, G.T.; Wyrick, T.O. Assessment of Telemedicine and Phone Consultation Effects on Rate of Hand Transfers to Trauma Centers and Specialty Services Referrals. Hand 2023, 18, 668–672. [Google Scholar] [CrossRef]
- O’Connell, R.S.; Haug, E.C.; Malasitt, P.; Mallu, S.; Satpathy, J.; Isaacs, J.; Mounasamy, V. Appropriateness of patients transferred with orthopedic injuries: Experience of a level I trauma center. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 551–554. [Google Scholar] [CrossRef] [PubMed]
- D’Amore, T.; Blaber, O.; Magnuson, J.A.; Sutton, R.M.; Haag, T.; Krueger, C.A. Orthopedic Specialty Hospital Reasons for Transfer and Subsequent Outcomes. J. Arthroplast. 2022, 37, 819–823. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Lau, E.C.; Ong, K.L.; Adler, E.M.; Kolisek, F.R.; Manley, M.T. Which Clinical and Patient Factors Influence the National Economic Burden of Hospital Readmissions After Total Joint Arthroplasty? Clin. Orthop. Relat. Res. 2017, 475, 2926–2937. [Google Scholar] [CrossRef]
- Thakur, N.A.; Plante, M.J.; Kayiaros, S.; Reinert, S.E.; Ehrlich, M.G. Inappropriate transfer of patients with orthopaedic injuries to a Level I trauma center: A prospective study. J. Orthop. Trauma. 2010, 24, 336–339. [Google Scholar] [CrossRef]
- Hahn, P.; Qaderi, A.; Jung, J.; Schwarzkopf, R. The Institutional Costs and Resource Profile of Transfer Patients Into an Arthroplasty Service. Surg. Technol. Int. 2015, 27, 257–262. [Google Scholar]
- Bernstein, D.N.; Bozic, K.J. Coaching for the Orthopedic Surgery Leader. Clin. Sports Med. 2023, 42, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Roy, J.; Adhikary, K.; Kar, S.; Pamučar, D. A rough strength relational DEMATEL model for analysing the key success factors of hospital service quality. Decis. Mak. Appl. Manag. Eng. 2018, 1, 121–142. [Google Scholar] [CrossRef]
- Carpenter, C.R.; Sherbino, J. How does an “opinion leader” influence my practice? Can. J. Emerg. Med. 2010, 12, 431–434. [Google Scholar] [CrossRef]
- Holliday, J.; Audrey, S.; Campbell, R.; Moore, L. Identifying Well-Connected Opinion Leaders for Informal Health Promotion: The Example of the ASSIST Smoking Prevention Program. Health Commun. 2016, 31, 946–953. [Google Scholar] [CrossRef] [PubMed]
- Parand, A.; Dopson, S.; Renz, A.; Vincent, C.A. The role of hospital managers in quality and patient safety: A systematic review. BMJ Open 2014, 4, e005055. [Google Scholar] [CrossRef]
- Flodgren, G.; Parmelli, E.; Doumit, G.; Gattellari, M.; O’Brien, M.A.; Grimshaw, J.; Eccles, M.P. Local opinion leaders: Effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2011, 8, CD000125. [Google Scholar] [CrossRef]
- Flodgren, G.; O’Brien, M.A.; Parmelli, E.; Grimshaw, J.M. Local opinion leaders: Effects on professional practice and healthcare outcomes. Cochrane Database Syst. Rev. 2019, 6, CD000125. [Google Scholar] [CrossRef]
- Ivers, N.; Jamtvedt, G.; Flottorp, S.; Young, J.M.; Odgaard-Jensen, J.; French, S.D.; O’Brien, M.A.; Johansen, M.; Grimshaw, J.; Oxman, A.D. Audit and feedback: Effects on professional practice and healthcare outcomes. Cochrane Database Syst. Rev. 2012, 6, CD000259. [Google Scholar] [CrossRef]
- Rozell, J.C.; Owusu-Sarpong, S.; Robin, J.X.; Karamitopoulos, M. Giving and Receiving Meaningful Feedback in Orthopaedic Surgery Training. J. Am. Acad. Orthop. Surg. Epub ahead of print. 2023. [Google Scholar] [CrossRef]
- Anazor, F. Ipsative Assessment and Peer Feedback in an Orthopaedic Junior Doctor Teaching Programme: A Project Plan and Narrative Review of the Literature. Cureus 2022, 14, e31961. [Google Scholar] [CrossRef]
- Hysong, S.J. Meta-analysis: Audit and feedback features impact effectiveness on care quality. Med. Care. 2009, 47, 356–363. [Google Scholar] [CrossRef] [PubMed]
- Hurst, D. Audit and feedback had small but potentially important improvements in professional practice. Evid. Based Dent. 2013, 14, 8–9. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Brown, B.; Gude, W.T.; Blakeman, T.; van der Veer, S.N.; Ivers, N.; Francis, J.J.; Lorencatto, F.; Presseau, J.; Peek, N.; Daker-White, G. Clinical Performance Feedback Intervention Theory (CP-FIT): A new theory for designing, implementing, and evaluating feedback in health care based on a systematic review and meta-synthesis of qualitative research. Implement. Sci. 2019, 14, 40. [Google Scholar] [CrossRef] [PubMed]
- Ko, H.C.; Turner, T.J.; Finnigan, M.A. Systematic review of safety checklists for use by medical care teams in acute hospital settings-limited evidence of effectiveness. BMC Health Serv. Res. 2011, 11, 211. [Google Scholar] [CrossRef] [PubMed]
- Boyd, J.; Wu, G.; Stelfox, H. The Impact of Checklists on Inpatient Safety Outcomes: A Systematic Review of Randomized Controlled Trials. J. Hosp. Med. 2017, 12, 675–682. [Google Scholar] [CrossRef]
- Chen, C.; Kan, T.; Li, S.; Qiu, C.; Gui, L. Use and implementation of standard operating procedures and checklists in prehospital emergency medicine: A literature review. Am. J. Emerg. Med. 2016, 34, 2432–2439. [Google Scholar] [CrossRef]
- Treadwell, J.R.; Lucas, S.; Tsou, A.Y. Surgical checklists: A systematic review of impacts and implementation. BMJ Qual. Saf. 2014, 23, 299–318. [Google Scholar] [CrossRef]
- Tang, R.; Ranmuthugala, G.; Cunningham, F. Surgical safety checklists: A review. ANZ J. Surg. 2014, 84, 148–154. [Google Scholar] [CrossRef]
- Williams, A.K.; Cotter, R.A.; Bompadre, V.; Goldberg, M.J.; Steinman, S.S. Patient Safety Checklists: Do They Improve Patient Safety for Supracondylar Humerus Fractures? J. Pediatr. Orthop. 2019, 39, 232–236. [Google Scholar] [CrossRef]
- County Emergency Clinical Hospital of Targu Mures. Available online: https://www.spitalmures.ro/en/ (accessed on 9 September 2023).
- Moldovan, F.; Moldovan, L.; Bataga, T. Assessment of Labor Practices in Healthcare Using an Innovatory Framework for Sustainability. Medicine 2023, 59, 796. [Google Scholar] [CrossRef]
- Moldovan, F.; Moldovan, L.; Bataga, T. The Environmental Sustainability Assessment of an Orthopedics Emergency Hospital Supported by a New Innovative Framework. Sustainability 2023, 15, 13402. [Google Scholar] [CrossRef]
- Activity Report. County Emergency Clinical Hospital of Targu Mures. Available online: https://www.spitalmures.ro/en/management/raport-de-activitate/ (accessed on 9 September 2023).
- Moldovan, F.; Bataga, T. Torque Control during Bone Insertion of Cortical Screws. Procedia Manuf. 2020, 46, 484–490. [Google Scholar] [CrossRef]
- Moldovan, L.; Gligor, A.; Grif, H.S.; Moldovan, F. Dynamic Numerical Simulation of the 6-PGK Parallel Robot Manipulator. Proc. Rom. Acad. Ser. A 2019, 20, 67–75. [Google Scholar]
- Mikolajczyk, T.; Moldovan, L.; Chalupczak, A.; Moldovan, F. Computer Aided Learning Process. Procedia Eng. 2017, 181, 1028–1035. [Google Scholar] [CrossRef]
- Mikolajczyk, T.; Moldovan, F.; Ciobanu, I.; Chalupczak, A.; Marin, A.G. Brain Research Using Computer Test. Procedia Technol. 2016, 22, 1113–1120. [Google Scholar] [CrossRef]
- Ciobanu, I.; Stanculescu Badea, D.I.; Iliescu, A.; Popescu, A.M.; Seiciu, P.S.; Mikolajczyk, T.; Moldovan, F.; Berteanu, M. The Usability Pilot Study of a Mechatronic System for Gait Rehabilitation. Procedia Manuf. 2018, 22, 864–871. [Google Scholar] [CrossRef]
- World Health Organization. WHO Surgical Safety Checklist. Available online: https://www.who.int/teams/integrated-health-services/patient-safety/research/safe-surgery/tool-and-resources (accessed on 9 September 2023).

| Social Responsibility | 1—Organizational Governance | 2—Human Rights | 3—Labor Practices | 4—Environment | 5—Fair Healthcare Practices | 6—Patient Issues | 7—Community Involvement and Development | |
|---|---|---|---|---|---|---|---|---|
| Quality Cycle | ||||||||
| (P) Healthcare services design | PA—Healthcare services accreditation | PA1—Decision structures and processes | PA21—Health care services accessibility PA22—Medical care services for disadvantaged groups | PA3—Promotion of change and professional development | PA4—Environ-mental impact plan | PA5—Attitudes of the profession towards accreditation | PA6—Performance information | PA7—Community involvement activities |
| PB—Patient-centered care interventions design | PB1—Quality assurance processes design | PB2—Interventions with positive effects on patient satisfaction | PB3—Quality assurance of patient- centered medical interventions | PB4—Environ-mental criteria for selection of materials used in interventions | PB5—Effective interventions implementation | PB6—Patient self-care design and self-management | PB7—Content of the interventions adapted to the community | |
| (I) Healthcare services provision | IA—Health care provision | IA1—Computerized support systems for clinical decisions | IA2—Specific medical approaches | IA31—Continuous healthcare education IA32—Practice guidelines employment and dissemination | IA41—Usage of recycled materials IA42—Waste recycling | IA5—Promotion of the patient safety culture | IA6—Critical features for improving the surveillance of patients with chronic conditions | IA71—Networking and partnership IA72—Involvement of volunteers and training networks |
| IB—Transfer assurance | IB1—Transfer evaluation mechanisms | IB2—Fair transfer interventions | IB3—Interventions for transfers improvement | IB4—Environmen-tally friendly transfer interventions | IB5—Features that affect transfer effectiveness | IB6—Interventions to reduce problems in outpatients | IB7—Involvement and participation of professional associations | |
| (E) Healthcare services evaluation | EA—Evaluation and involvement of local opinion leaders | EA1—Existence and recognition of local opinion leaders | EA2—Evaluation of current medical practices | EA3—Professional practices improvement | EA4—Improve-ment of environmental consumption | EA5—Effective work practices | EA6—Patient-specific issues management | EA7—Local opinion leaders involved in the community |
| EB—Satisfaction assessment | EB1—Monitoring mechanisms assignment | EB2—Patient satisfaction degree | EB3—Medical staff satisfaction | Not relevant | Not relevant | EB6—Patient satisfaction degree regarding therapeutic benefits | EB7—Satisfaction regarding partnerships | |
| (R) Continuous improvement | RA-Self assessment | RA1—Self-assessment tools | RA2—Freedom of expression assurance | RA3—Audit and feedback | RA4—Mechanisms for monitoring energy consumption and waste generation | RA5—Feedback to medical staff | RA6—Complaints management | RA7—Communitarian initiatives |
| RB—Healthcare services innovation | RB1—Changes to healthcare services | Not relevant | RB3—Medical organization supported by Six sigma and Lean | RB4—Environmental measures | RB5—Safety checklists | RB6—Incident report | RB7—Educational visits |
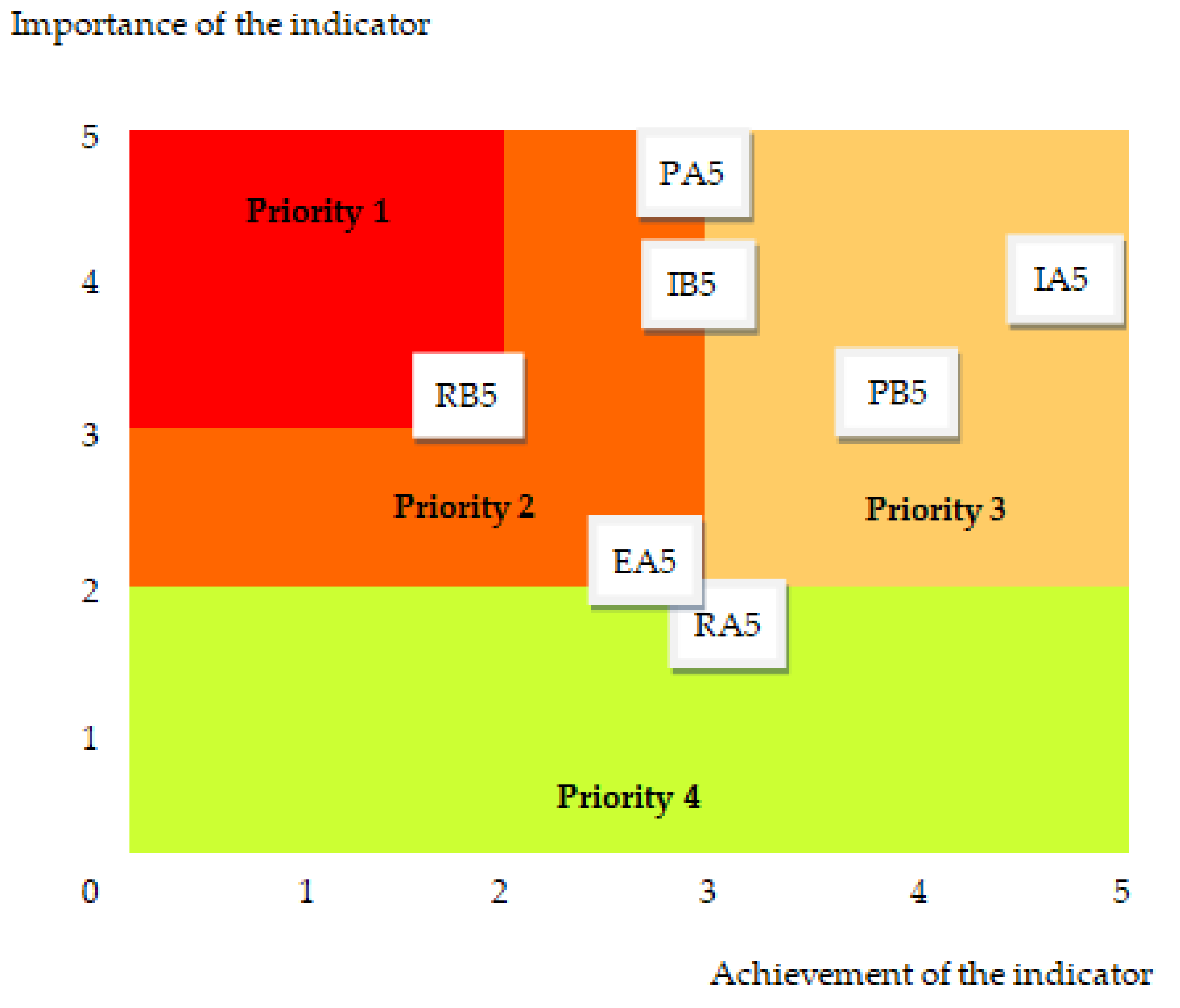
| No. | Indicator Description | Importance (Ii) | Achievement (Ai) | Sustainability Indicator (Si = Ii·Ai) |
|---|---|---|---|---|
| 1 | PA5—Attitudes of the profession towards accreditation | 5 | 3 | 15 |
| 2 | PB5—Effective intervention application | 3 | 4 | 12 |
| 3 | IA5—Promoting a culture of patient safety | 4 | 5 | 20 |
| 4 | IB5—Characteristics that affect the effectiveness of transfers | 4 | 3 | 12 |
| 5 | EA5—Effective healthcare practices | 2 | 3 | 6 |
| 6 | RA5—Feedback to medical staff | 2 | 3 | 6 |
| 7 | RB5—Safety checklists | 3 | 2 | 6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moldovan, F.; Moldovan, L. Fair Healthcare Practices in Orthopedics Assessed with a New Framework. Healthcare 2023, 11, 2753. https://doi.org/10.3390/healthcare11202753
Moldovan F, Moldovan L. Fair Healthcare Practices in Orthopedics Assessed with a New Framework. Healthcare. 2023; 11(20):2753. https://doi.org/10.3390/healthcare11202753
Chicago/Turabian StyleMoldovan, Flaviu, and Liviu Moldovan. 2023. "Fair Healthcare Practices in Orthopedics Assessed with a New Framework" Healthcare 11, no. 20: 2753. https://doi.org/10.3390/healthcare11202753
APA StyleMoldovan, F., & Moldovan, L. (2023). Fair Healthcare Practices in Orthopedics Assessed with a New Framework. Healthcare, 11(20), 2753. https://doi.org/10.3390/healthcare11202753







