Effects of High-Intensity Exercise on Physiological Indicators of Recovery Period by Wearing Face Masks of Elite Athletes
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
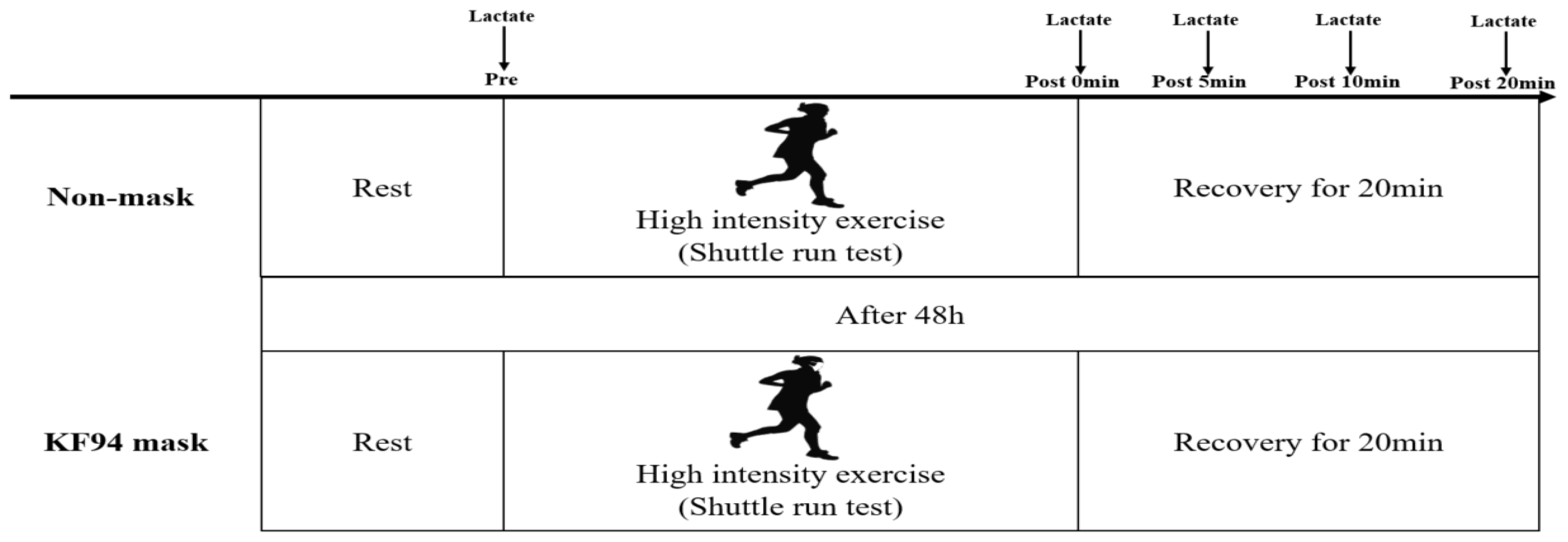
2.2. Procedures
2.2.1. Body Composition
2.2.2. Incremental Exertion Test (IET)
2.2.3. Blood Lactate and Heart Rate Level
2.3. Statistical Analysis
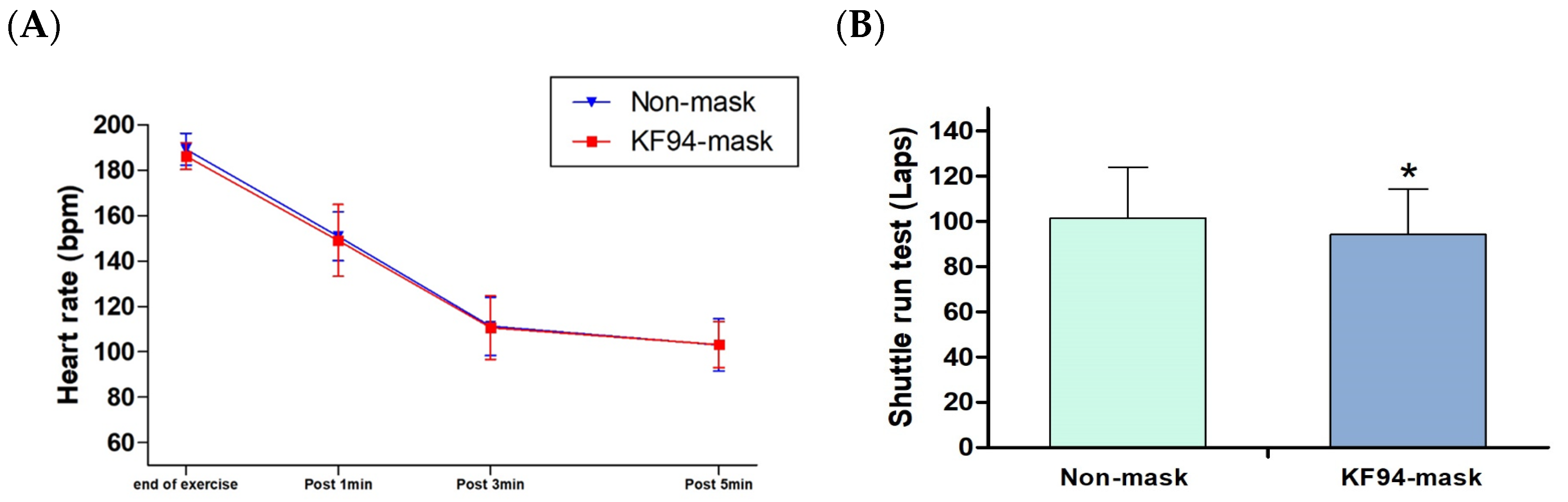
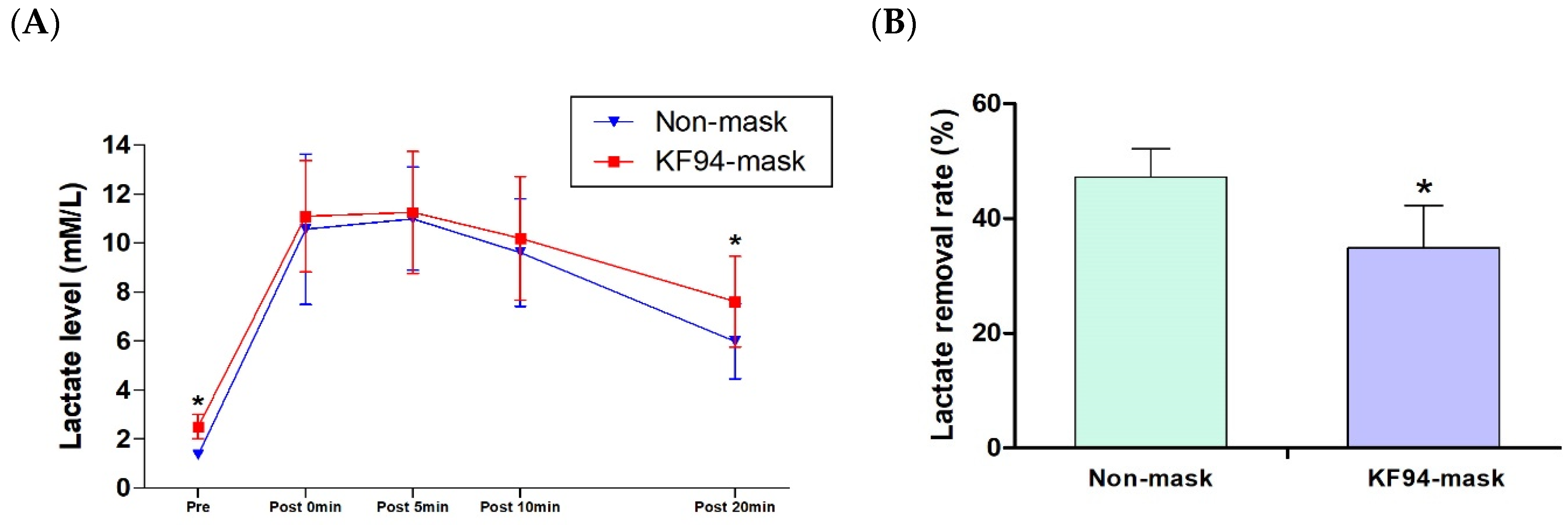
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cucinotta, D.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [PubMed]
- World Health Organization. Available online: https://covid19.who.int/ (accessed on 5 September 2022).
- Obayashi, H.; Ikuta, Y.; Nakashima, N.; Yamamoto, R.; Fujishita, H.; Fukuhara, K.; Sakamitsu, T.; Ushio, K.; Kimura, H.; Adachi, N. Impact of COVID-19-Related Sports Activity Disruptions on the Physical Fitness of Japanese Adolescent Athletes. Adolescents 2022, 2, 140–149. [Google Scholar] [CrossRef]
- Tsoukos, A.; Bogdanis, G.C. The effects of a five-month lockdown due to COVID-19 on physical fitness parameters in adolescent students: A comparison between cohorts. Int. J. Environ. Res. Public Health 2021, 19, 326. [Google Scholar] [CrossRef]
- Sunda, M.; Gilic, B.; Peric, I.; Jurcev Savicevic, A.; Sekulic, D. Evidencing the influence of the COVID-19 pandemic and imposed lockdown measures on fitness status in adolescents: A preliminary report. Healthcare 2021, 9, 681. [Google Scholar] [CrossRef] [PubMed]
- Esposito, S.; Principi, N.; Leung, C.C.; Migliori, G.B. Universal use of face masks for success against COVID-19: Evidence and implications for prevention policies. Eur. Respir J. 2020, 55, 2001260. [Google Scholar] [CrossRef]
- Luo, C.; Yao, L.; Zhang, L.; Yao, M.; Chen, X.; Wang, Q.; Shen, H. Possible transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in a public bath center in Huai’an, Jiangsu Province, China. JAMA Netw. Open 2020, 3, e204583. [Google Scholar] [CrossRef] [PubMed]
- Adams, J. Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community-Based Transmission; CDC: Atlanta, GA, USA, 2020.
- Cheng, K.K.; Lam, T.H.; Leung, C.C. Wearing face masks in the community during the COVID-19 pandemic: Altruism and solidarity. Lancet 2022, 399, e39–e40. [Google Scholar] [CrossRef] [PubMed]
- Leung, N.H.; Chu, D.K.; Shiu, E.Y.; Chan, K.H.; McDevitt, J.J.; Hau, B.J.; Yen, H.L.; Li, Y.; Lp, D.K.; Peiris, J.S.; et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020, 26, 676–680. [Google Scholar] [CrossRef]
- CDC. Determination of Particulate Filter Efficiency Level of N95 Series Flters against Solid Particulates for Non-Powered, Air-Purifying Respirators Standard; CDC: Atlanta, GA, USA, 2019.
- Dai, H.; Zhao, B. Association between the infection probability of COVID-19 and ventilation rates: An update for SARS-CoV-2 variants. Build Simul. 2023, 16, 3–12. [Google Scholar] [CrossRef]
- Blocken, B.; Malizia, F.; Van Druenen, T.; Marchal, T. Towards Aerodynamically Equivalent COVID19 1.5 m Social Distancing for walking and Running. 2020. preprint. Available online: www.urbanphysics.net/Social%20Distancing%20v20_White_Paper.pdf (accessed on 13 December 2022).
- Roberge, R.J.; Coca, A.; Williams, W.J.; Powell, J.B.; Palmiero, A.J. Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Respir. Care 2010, 55, 569–577. [Google Scholar]
- Greenhalgh, T.; Dijkstra, P.; Jones, N.; Bowley, J. Exercising and face masks: An important hypothesis buried in a selective review. Med. Hypotheses 2020, 144, 110255. [Google Scholar] [CrossRef]
- Jagim, T.R.; Dominy, T.A.; Camic, C.L.; Wright, G.; Doberstein, S.; Jones, M.T.; Oliver, J.M. Acute effects of the elevation training mask on strength performance in recreational weight lifters. J. Strength Cond. Res. 2018, 32, 482–489. [Google Scholar] [CrossRef]
- Egger, F.; Blumenauer, D.; Fishcer, P.; Venhorst, A.; Kulenthiran, S.; Bewarder, Y.; Zimmer, A.; Böhm, M.; Meyer, T.; Mahfoud, F. Effects of face masks on performance and cardiorespiratory response in well-trained athletes. Clin. Res. Cardiol. 2022, 111, 264–271. [Google Scholar] [CrossRef]
- Pyne, D.B.; Lee, H.; Swanwick, K.M. Monitoring the lactate threshold in world-ranked swimmers. Med. Sci. Sports Exerc. 2001, 33, 291–297. [Google Scholar] [CrossRef]
- Ribeiro, J.; Figueiredo, P.; Morais, S.; Alves, F.; Toussaint, H.; Vilas-Boas, J.P.; Fernandes, R.J. Biomechanics, energetics and coordination during extreme swimming intensity: Effect of performance level. J. Sports Sci. 2017, 35, 1614–1621. [Google Scholar] [CrossRef] [PubMed]
- Mota, M.R.; Dantas, R.A.E.; Oliveira-Silva, I.; Sales, M.M.; Sotero, R.D.C.; Venâncio, P.E.M.; Teixeira Júnior, J.; Chaves, S.N.; de Lima, F.D. Effect of self-paced active recovery and passive recovery on blood lactate removal following a 200 m freestyle swimming trial. Open Access J. Sports Med. 2017, 8, 155–160. [Google Scholar] [CrossRef]
- Catcheside, P.G.; Scroop, G.C. Lactate kinetics in resting and exercising forearms during moderate-intensity supine leg exercise. J. Appl. Physiol. 1993, 74, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Liao, L.; Xiao, W.; Yu, X.; Wang, H.; Zhao, D.M.; Wang, D.Q.; Cui, Y. Can N95 facial masks be used after disinfection? and for how many times. ACS Nano 2020, 14, 6348–6356. [Google Scholar] [CrossRef] [PubMed]
- Fikenzer, S.; Uhe, T.; Lavall, D.; Rudolph, U.; Falz, R.; Busse, M.; Hepp, P.; Laufs, U. Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clin. Res. Cardiol. 2020, 109, 1522–1530. [Google Scholar] [CrossRef]
- Gontjes, K.J.; Gibson, K.E.; Lansing, B.; Cassone, M.; Mody, L. Contamination of common area and rehabilitation gym environment with multidrug-resistant organisms. J. Am. Geriatr. Soc. 2020, 68, 478–485. [Google Scholar] [CrossRef]
- Lässing, J.; Falz, R.; Pökel, C.; Fikenzer, S.; Laufs, U.; Schulze, A.; Hölldobler, N.; Rüdrich, P.; Busse, M. Effects of surgical face masks on cardiopulmonary parameters during steady state exercise. Sci. Rep. 2020, 10, 22363. [Google Scholar] [CrossRef] [PubMed]
- Pifarré, F.; Zabala, D.D.; Grazioli, G.; Maura, I.D.Y. COVID-19 and mask in sports. Apunt. Sports Med. 2020, 55, 143–145. [Google Scholar] [CrossRef]
- Tornero-Aguilera, J.F.; Rubio-Zarapuz, A.; Bustamante-Sánchez, A.; Clemente-Suárez, V.J. The effect of surgical mask use in anaerobic running performance. Appl. Sci. 2021, 11, 6555. [Google Scholar] [CrossRef]
- Andre, T.L.; Gann, J.J.; Hwang, P.S.; Ziperman, E.; Magnussen, M.J.; Willoughby, D.S. Restrictive breathing mask reduces repetitions to failure during a session of lower-body resistance exercise. J. Strength Cond. Res. 2018, 32, 2103–2108. [Google Scholar] [CrossRef]
- Garnacho-Castaño, M.V.; Albesa-Albiol, L.; Serra-Payá, N.; Gomis Bataller, M.; Felíu-Ruano, R.; Guirao Cano, L.; Plequezuelos Cobo, E.; Maté-Muñoz, J.L. The slow component of oxygen uptake and efficiency in resistance exercises: A comparison with endurance exercises. Front. Physiol. 2019, 10, 357. [Google Scholar] [CrossRef] [PubMed]
- Suchomel, T.J.; Nimphius, S.; Bellon, C.R.; Stone, M.H. The importance of muscular strength: Training considerations. Sports Med. 2018, 48, 765–785. [Google Scholar] [CrossRef] [PubMed]
- Epstein, D.; Korytny, A.; Isenberg, Y.; Marcusohn, E.; Zukermann, R.; Bishop, B.; Minha, S.; Raz, A.; Miller, A. Return to training in the COVID-19 era: The physiological effects of face masks during exercise. Scand. J. Med. Sci. Sports 2021, 31, 70–75. [Google Scholar] [CrossRef]
- Chandrasekaran, B.; Fernandes, S. “Exercise with facemask; Are we handling a devil’s sword?”–A physiological hypothesis. Med. Hypotheses 2020, 144, 110002. [Google Scholar] [CrossRef]
- Iepsen, U.W.; Plovsing, R.R.; Tjelle, K.; Foss, N.B.; Meyhoff, C.S.; Ryrsø, C.K.; Berg, R.M.G.; Secher, N.H. The role of lactate in sepsis and COVID-19: Perspective from contracting skeletal muscle metabolism. Exp. Physiol. 2022, 107, 665–673. [Google Scholar] [CrossRef]
- Ramos-Campo, D.J.; Rubio-Arias, J.A.; Dufour, S.; Chung, L.; Ávila-Gandía, V.; Alcaraz, P.E. Biochemical responses and physical performance during high-intensity resistance circuit training in hypoxia and normoxia. Eur. J. Appl. Physiol. 2017, 117, 809–818. [Google Scholar] [CrossRef]
- Melnikov, V.N.; Divert, V.E.; Komlyagina, T.G.; Consedine, N.S.; Krivoschekov, S.G. Baseline values of cardiovascular and respiratory parameters predict response to acute hypoxia in young healthy men. Physiol. Res. 2017, 66, 467–479. [Google Scholar] [CrossRef] [PubMed]
- Barbieri, J.F.; Gáspari, A.F.; Teodoro, C.L.; Motta, L.; Castaño, L.A.A.; Bertuzzi, R.; Bernades, C.F.; Chacon-Mikahil, M.P.T.; de Moraes, A.C. The effect of an airflow restriction mask (ARM) on metabolic, ventilator, and electromyographic responses to continuous cycling exercise. PLoS ONE 2020, 15, e0237010. [Google Scholar] [CrossRef] [PubMed]
- Tornero-Aguilera, J.F.; Rubio-Zarapuz, A.; Clemente-Suárez, V.J. Implications of surgical mask use in physical education lessons. Physiol Behav. 2021, 239, 113513. [Google Scholar] [CrossRef] [PubMed]
- Clemente-Suárez, V.J.; Navarro-Jiménez, E.; Moreno-Luna, L.; Saavedra-Serrano, M.C.; Jimenez, M.; Simón, J.A.; Tornero-Aguilera, J.F. The impact of the COVID-19 pandemic on social, health, and economy. Sustainability 2021, 13, 6314. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, H.-T.; Kim, D. Effects of High-Intensity Exercise on Physiological Indicators of Recovery Period by Wearing Face Masks of Elite Athletes. Healthcare 2023, 11, 268. https://doi.org/10.3390/healthcare11020268
Kwon H-T, Kim D. Effects of High-Intensity Exercise on Physiological Indicators of Recovery Period by Wearing Face Masks of Elite Athletes. Healthcare. 2023; 11(2):268. https://doi.org/10.3390/healthcare11020268
Chicago/Turabian StyleKwon, Hyeong-Tae, and Daeho Kim. 2023. "Effects of High-Intensity Exercise on Physiological Indicators of Recovery Period by Wearing Face Masks of Elite Athletes" Healthcare 11, no. 2: 268. https://doi.org/10.3390/healthcare11020268
APA StyleKwon, H.-T., & Kim, D. (2023). Effects of High-Intensity Exercise on Physiological Indicators of Recovery Period by Wearing Face Masks of Elite Athletes. Healthcare, 11(2), 268. https://doi.org/10.3390/healthcare11020268



