In Situ Simulation: A Strategy to Restore Patient Safety in Intensive Care Units after the COVID-19 Pandemic? Systematic Review
Abstract
1. Introduction
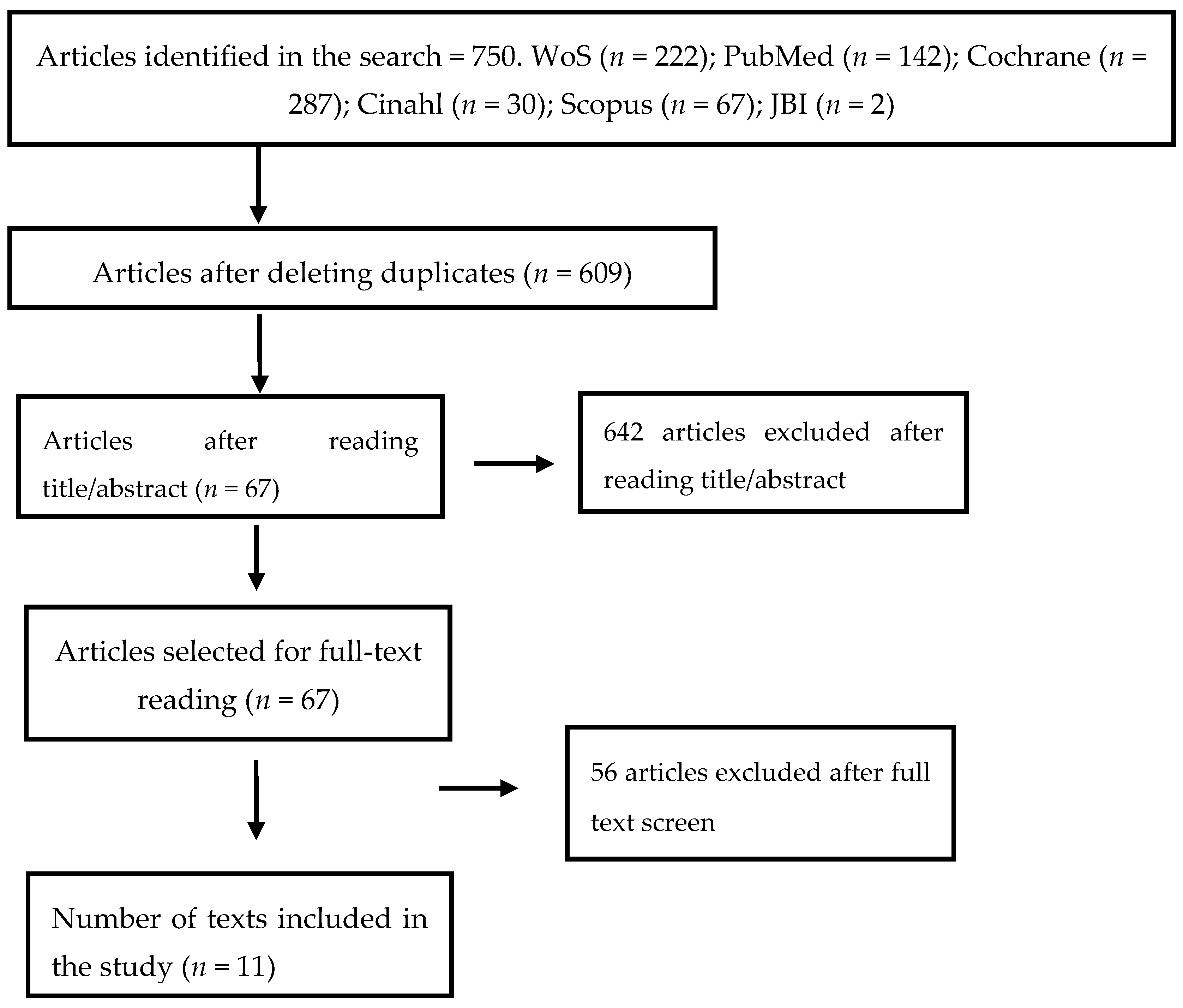
2. Materials and Methods
2.1. Search Strategy
2.2. Elegibility Criteria
2.3. Assessment of Methodological Quality
2.4. Data Collection and Synthesis
3. Results
3.1. Overview of Studies
3.2. Detection of Latent Security Threats (LST)
3.3. Staff Perception of Patient Safety Culture
3.4. Interprofessional Communication
3.5. System Organization
3.6. Assessment of Methodological Quality
4. Discussion
Implications for Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Institute of Medicine (US) Committee on Quality of Health Care in America. To Err is Human: Building a Safer Health System; Kohn, L.T., Corrigan, J.M., Donaldson, M.S., Eds.; National Academies Press: Washington, DC, USA, 2000. [Google Scholar]
- Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century; National Academies Press: Washington, DC, USA, 2001. [Google Scholar]
- Koukourikos, K.; Tsaloglidou, A.; Kourkouta, L.; Papathanasiou, I.V.; Iliadis, C.; Fratzana, A.; Panagiotou, A. Simulation in Clinical Nursing Education. Acta Inf. Med. 2021, 29, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Truchot, J.; Boucher, V.; Raymond-Dufresne, É.; Malo, C.; Brassard, É.; Marcotte, J.; Martel, G.; Côté, G.; Garneau, C.; Bouchard, G.; et al. Evaluation of the feasibility and impacts of in situ simulation in emergency medicine-a mixed-method study protocol. BMJ Open 2021, 4, e040360. [Google Scholar] [CrossRef] [PubMed]
- Dute, J. Council of Europe. Recommendation Rec(2006)7 of the Committee of Ministers to member states on management of patient safety and prevention of adverse advents in health care. Eur. J. Health Law 2008, 15, 79–98. [Google Scholar]
- European Commission. Recomendaciones del Consejo sobre la seguridad de los pacientes, en particular la prevención y lucha contra las infecciones relacionadas con la asistencia sanitaria. Diario del Consejo de la Unión Europea 9 de junio de 2009 (2009/C 151/01). European Commission: Brussels, Belgium, 2011. Available online: http://ec.europa.eu/health/patient_safety/docs/council_2009_es.pdf (accessed on 15 November 2022).
- Kowalski, S.L.; Anthony, M. CE: Nursing’s Evolving Role in Patient Safety. Am. J. Nurs. 2017, 117, 34–48. [Google Scholar] [CrossRef]
- Ministry of Health. Statement of the Advisory Board of the Critical Patient Safety Programme. Available online: https://hws.vhebron.net/envin-helics/Help/Declaracion_Consejo_Asesor_Seguridad_Paciente.pdf (accessed on 15 November 2022).
- Merino, P.; Álvarez, J.; Cruz, M.; Alonso, Á.; Gutiérrez, I. SYREC Study Investigators. Adverse events in Spanish intensive care units: The SYREC study. Int. J. Qual. Health Care 2012, 24, 105–113. [Google Scholar] [CrossRef] [PubMed]
- INACSL Standards Committee. INACSL standards of best practice: Simulation SM Simulation design. Clin. Simul. Nurs. 2016, 12, S5–S12. [Google Scholar] [CrossRef]
- INACSL Standards Committee. INACSL standards of best practice: Simulation SM Debriefing. Clin. Simul. Nurs. 2016, 12, S21–S25. [Google Scholar] [CrossRef]
- Jeffries, P.R.; Clochesy, J. Clinical simulation: An experiential, student-centered pedagogical approach. In Teaching in Nursing. A Guide for Faculty, 4th ed.; Billings, D.M., Halstead, J.A., Eds.; Elsevier: Barcelona, Spain, 2012; pp. 352–368. [Google Scholar]
- Jiménez-Gómez, M.A.; Cárdenas-Becerril, L.; Velásquez-Oyola, M.B.; Carrillo-Pineda, M.; Barón-Díaz, L.Y. Reflective and critical thinking in nursing curriculum. Rev. Lat. Am. Enfermagem. 2019, 5, e3173. [Google Scholar] [CrossRef]
- Costa, R.; Medeiros, S.M.; Martins, J.; Coutinho, V.; Araújo, M. Effectiveness of simulation in teaching immunization in nursing: A randomized clinical trial. Rev. Lat. Am. Enfermagem. 2020, 28, e3305. [Google Scholar] [CrossRef]
- Calleja, J.L.; Soublette Sánchez, A.; Radedek, P. Is clinical simulation an effective learning tool in teaching clinical ethics? (¿Es la simulación clínica una herramienta de aprendizaje efectiva en la enseñanza de la ética clínica?). Medwave 2020, 20, e7824. [Google Scholar] [CrossRef]
- Souza-Junior, V.; Mendes, I.; Tori, R.; Marques, L.; Mashuda, F.; Hirano, L.; Godoy, S. VIDA-Nursing v1.0: Immersive virtual reality in vacuum blood collection among adults. Rev. Lat. Am. Enfermagem. 2020, 28, e3263. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, J.; Nascimento, K.; Oliveira, J.; Alves, M.G.; Silva, A.; Dalri, M. Clinical simulation for nursing competence development in cardiopulmonary resuscitation: Systematic review. Rev. Lat. Am. Enfermagem. 2020, 28, e3391. [Google Scholar] [CrossRef]
- Rojo, E.; Maestre, J.M.; Piedra, L.; Esteban, J.; Sánchez, B.; Hoz, V.; Del Moral, I. Interprofessional team training with in situ simulation to improve the quality of cardiopulmonary resuscitation. J. Healthc. Qual. Res. 2021, 37, 92–99. [Google Scholar] [CrossRef]
- Zonta, J.B.; Eduardo, A.; Ferreira, M.; Chaves, G.H.; Okido, A. Self-confidence in the management of health complications at school: Contributions of the in situ simulation. Rev. Lat. Am. Enfermagem. 2019, 27, e3174. [Google Scholar] [CrossRef]
- Cánovas, Y.; Casabella, B.; Martín, C.; González, F.; Moreno, S.; Del Val, J.L. Evaluation of a training model for health professionals in the care of critical patients: AIPCAP Study. Aten. Primaria 2019, 52, 151–158. [Google Scholar] [CrossRef]
- Schertzer, K.; Patti, L. In Situ Debriefing in Medical Simulation. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Gable, B.; Hommema, L. In-Situ Simulation in Interdisciplinary Family Practice Improves Response to In-Office Emergencies. Cureus 2021, 13, e14315. [Google Scholar] [CrossRef] [PubMed]
- Linares-Espinós, E.; Hernández, V.; Domínguez-Escrig, J.L.; Fernández-Pello, S.; Hevia, V.; Mayor, J.; Padilla-Fernández, B.; Ribal, M.J. Methodology of a systematic review. Actas Urol. Esp. 2018, 42, 499–506. [Google Scholar] [CrossRef]
- Pasay-An, E.; Alshammari, F.; Mostoles, R., Jr.; Gattud, V.; Cajigal, J.; Buta, J. A qualitative study on nurses’ experiences with social stigma in the context of COVID-19. Enferm. Clinica 2021, 32, 75–82. [Google Scholar] [CrossRef]
- Astier-Peña, M.P.; Torijano-Casalengua, M.L.; Olivera-Cañadas, G. Patient Safety Group of the Spanish Society of Family and Community Medicine (SEMFYC). Setting priorities for patient safety in Primary Care. Aten. Prim. 2016, 48, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Gil, T. Plantilla para ayudarte a entender un estudio cualitativo. In CASPe. Guías CASPe de Lectura Crítica de la Literatura Médica; CASPe: Alicante, Spain, 2010; Volume III, pp. 3–8. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Rev. Esp. Cardiol. 2021, 74, 790–799. [Google Scholar] [CrossRef]
- Bapteste, L.; Bertucat, S.; Balanca, B. Unexpected Detection of Latent Safety Threats by In Situ Simulation: About Two Cases in an Adult Intensive Care Unit. Clin. Simul. Nurs. 2020, 47, 6–8. [Google Scholar] [CrossRef]
- Petrosoniak, A.; Hicks, C.; Barratt, L.; Gascon, D.; Kokoski, C.; Campbell, D.; White, K.; Bandiera, G.; Lum-Kwong, M.M.; Nemoy, L.; et al. Design Thinking-Informed Simulation: An Innovative Framework to Test, Evaluate, and Modify New Clinical Infrastructure. Simul. Healthc. 2020, 15, 205–213. [Google Scholar] [CrossRef]
- Couto, T.; Barreto, J.; Marcon, F.C.; Mafra, A.; Accorsi, T. Detecting latent safety threats in an interprofessional training that combines in situ simulation with task training in an emergency department. Adv. Simul. 2018, 3, 23. [Google Scholar] [CrossRef] [PubMed]
- Schram, A.; Paltved, C.; Christensen, K.B.; Kjaergaard-Andersen, G.; Jensen, H.I.; Kristensen, S. Patient safety culture improves during an in situ simulation intervention: A repeated cross-sectional intervention study at two hospital sites. BMJ Open Qual. 2021, 10, e001183. [Google Scholar] [CrossRef] [PubMed]
- Paltved, C.; Bjerregaard, A.T.; Krogh, K.; Pedersen, J.; Musaeus, P. Designing in situ simulation in the emergency department: Evaluating safety attitudes amongst physicians and nurses. Adv. Simul. 2017, 2, 4. [Google Scholar] [CrossRef]
- Chetcuti, S.; Bhowmick, K. Simulation on the job: An intensive care unit’s report of how in situ simulation has impacted on human factors and ergonomics in the workplace. BMJ Simul. Technol. Enhanc. Learn. 2020, 6, 39–40. [Google Scholar] [CrossRef]
- Jonsson, K.; Brulin, C.; Härgestam, M.; Lindkvist, M.; Hultin, M. Do team and task performance improve after training situation awareness? A randomized controlled study of interprofessional intensive care teams. Scand. J. Trauma. Resucitation Emerg. Med. 2021, 29, 73. [Google Scholar] [CrossRef]
- So, E.H.K.; Chia, N.H.; George, W.Y.; Chan, O.P.K.; Yuen, S.L.; Lung, D.C.; Li, W.C.; So, S.S.; Cheung, V.K.L. Multidisciplinary simulation training for endotracheal intubation during COVID-19 in one Hong Kong regional hospital: Strengthening of existing procedures and preparedness. BMJ Simul. Technol. Enhanc. Learn. 2021, 7, 501–509. [Google Scholar] [CrossRef]
- Santos, T.M.; dos Santos Pedrosa, R.B.; dos Santos Carvalho, D.R.; Franco, M.H.; Silva, J.L.G.; Franci, D.; de Jorge, B.; Munhoz, D.; Calderan, T.; de Araujo Guerra Grangeia, T.; et al. Implementing healthcare professionals’ training during COVID-19: A pre and post-test design for simulation training. Sao Paulo Med. J. 2021, 139, 514–519. [Google Scholar] [CrossRef]
- Fregene, T.E.; Nadarajah, P.; Buckley, J.F.; Bigham, S.; Nangalia, V. Use of in situ simulation to evaluate the operational readiness of a high-consequence infectious disease intensive care unit. Anaesthesia 2020, 75, 733–738. [Google Scholar] [CrossRef]
- Kozlowski, S.; Chao, G.; Grand, J.; Braun, M.; Kuljanin, G. Advancing Multilevel Research Design: Capturing the Dynamics of Emergence. Organ. Res. Methods 2013, 16, 581–615. [Google Scholar] [CrossRef]
- Wheeler, D.; Geis, G.; Mack, E.; LeMaster, T.; Patterson, M. High-reliability emergency response teams in the hospital: Improving quality and safety using in situ simulation training. BMJ Qual. Saf. 2013, 22, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Patterson, M.; Geis, G.; Falcone, R.; LeMaster, T.; Wears, R. In situ simulation: Detection of safety threats and teamwork training in a high risk emergency department. BMJ Qual. Saf. 2013, 22, 468–477. [Google Scholar] [CrossRef]
- Weaver, S.; Lubomksi, L.; Wilson, R.; Pfoh, E.; Martinez, K. Supplement Promoting a Culture of Safety as a Patient Safety Strategy. Ann. Intern. Med. 2013, 158, 369–374. [Google Scholar] [CrossRef]
- Bleakley, A.; Allard, J.; Hobbs, A. Towards culture change in the operating theatre: Embedding a complex educational intervention to improve teamwork climate. Med. Teach. 2012, 34, e635–e640. [Google Scholar] [CrossRef]
- Cooper, J.; Blum, R.; Carroll, J.; Dershwitz, M.; Feinstein, D.; Gaba, D.; Morey, J.; Singla, A. Differences in safety climate among hospital anesthesia departments and the effect of a realistic simulation-based training program. Anesth Analg. 2008, 106, 574–584. [Google Scholar] [CrossRef]
- Guise, J.; Mladenovic, J. In situ simulation: Identification of systems issues. Semin Perinatol. 2013, 37, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Gardner, A.; Johnston, M.; Korndorffer, J.; Haque, I.; Paige, J. Using Simulation to Improve Systems-Based Practices. J. Comm. J. Qual. Patient Safe. 2017, 43, 484–491. [Google Scholar] [CrossRef]
- Laco, R.; Stuart, W. Simulation-Based Training Program to Improve Cardiopulmonary Resuscitation and Teamwork Skills for the Urgent Care Clinic Staff. Mil. Med. 2018, 187, 5–6. [Google Scholar] [CrossRef] [PubMed]
| Search Strategies | Pubmed | Cochrane | WoS | Cinahl | Scopus | JBI |
|---|---|---|---|---|---|---|
| (((((((((patient) OR (patient *)) OR (client *)) OR (adult)) OR (aged)) AND (UCI)) OR (Intensive care units)) OR (ICU)) OR (emergencies)) AND (((simulation “in situ”) OR (high fidelity simulation training)) AND (patient safety)) Filters: in the last 10 years, Humans | 142 | 30 | 2 | |||
| patient in Title Abstract Keyword OR client in Title Abstract Keyword AND in situ simulation in Title Abstract Keyword AND intensive care units in Title Abstract Keyword OR emergencies in Title Abstract Keyword—with publication date in the Cochrane Library Between Jan 2011 and Jun 2021 | 287 | |||||
| ALL = ((((((((((patient) OR (patient *)) OR (client *)) OR (adult)) OR (aged)) AND (UCI)) OR (Intensive care units)) OR (ICU)) OR (emergencies)) AND (((simulation “in situ”) OR (high fidelity simulation training)) AND (patient safety))) | 222 | |||||
| TITLE-ABS KEY (intensive AND care AND unit AND in AND situ AND simulation) AND (LIMIT-TO (PUBYEAR, 2021) OR LIMIT-TO (PUBYEAR, 2020) OR LIMIT-TO (PUBYEAR, 2019) OR LIMIT-TO (PUBYEAR, 2018) OR LIMIT-TO (PUBYEAR, 2017) OR LIMIT-TO (PUBYEAR, 2016) OR LIMIT-TO (PUBYEAR, 2015) OR LIMIT-TO (PUBYEAR, 2014) OR LIMIT-TO (PUBYEAR, 2013)) AND (LIMIT-TO (SUBJAREA, “MEDI”) OR LIMIT-TO (SUBJAREA, “NURS”)) AND (LIMIT-TO (LANGUAGE, “English”)) AND (LIMIT-TO (SRCTYPE, “j”)) | 67 |
| Author/Study Design | Participants | Interventions | Outcome Measurements | Results | CASPe Score |
|---|---|---|---|---|---|
| Truchot et al. [4] Mixed method: qualitative method for the assessment of feasibility and acceptability and a quantitative method for the assessment of patient safety and participant risks. | Phase 1: Non-random, voluntary participation. (Announced or unannounced). Phase 2: random | 40 min simulation sessions (20 min scenario and 20 min debriefing). | Semi-structured interviews were used to assess the acceptability of the intervention. | On-site simulation in an emergency department is feasible, safe and associated with benefits for both staff and patients. | 9/11 |
| Bapteste et al. [28] Case studies | New nurses and professionals | On site-simulation session in a room available in ICU. High fidelity Dummy (SimMan, Laerdal). | Participatory observational | Session 1: medication error. Session 2: delay in treatment. | 6/11 |
| Petrosoniak et al. [29] Systematic review and experimental review with case example | n = 117 manually reviewed papers | Cases with on-site simulation intervention. Group experience: 200 on-site simulation sessions in the emergency department in various countries | Bibliographic search in Pubmed, Medline, Scopus, Web of Science and ERIC. | Simulation training in the ED leads to tangible improvements in teamwork, safety and systems. | 7/10 |
| Couto et al. [30] Prospective Study | n = 114 participants in the scenarios. n = 101 in training tasks. n = 49 scenarios | Three scheduled 10-min on-site simulation scenarios alternated for each theme on a daily basis. | On-site simulation sessions followed by debriefing by two facilitators. Latent safety threats were identified using a checklist. | 56 latent safety threats were detected, with an average of 1.1 per scenario. | 10/11 |
| Schram et al. [31] Cross-sectional pre-post intervention study | n = 967 healthcare professionals (39 trained as simulation instructors) | Interventions were conducted in the hospital setting (in situ), 54 sessions in Hospital 1 and 62 in Hospital 2. No systematic simulation was carried out prior to the intervention. | To measure outcomes, the Safety Attitudes Questionnaire (SAQ) was used, which investigates patient safety culture before the intervention and 4–8 weeks after the intervention. | The response rate varied between 63.6% and 72.0% between surveys and hospitals. Mean scores on the scale improved significantly in five of the six safety dimensions in hospital 1, while only one dimension improved significantly in hospital 2. | 10/11 |
| Paltved. et al. [32] Denmark Mixed qualitative (ethnography) and quantitative pre-post intervention study | n = 16 health teams composed by 9 doctors and 30 nurses. | Three-pronged strategy: 1. thematic analysis of patient safety data. 2. Needs analysis based on a short-term ethnography. 3. Pre-post assessment using the validated Safety Attitudes questionnaire. | A convergent parallel mixed method was used to collect both qualitative and quantitative data in parallel and the analysis was merged in the final phase. | The findings of this study suggested that an on-site simulation program can act as an important catalyst for the improvement of safety and teamwork attitudes. | 9/11 |
| Chetcuti and Bhowmick [33] Pre-post intervention study | n = 12-bed ICU hospital admitting 450 patients per year (Random selection). | On-site simulation sessions using the Laerdal SimMan EssentialTM dummy. | After the evaluation and treatment of each clinical case, a didactic report was carried out using the FAST-PAGE model. The recording of the sessions was used to facilitate the information. | The evaluation of the outcome through pre- and post-simulation questionnaires was positive, participants improved their human factor skills as well as confidence in handling critical situations. | 8/11 |
| Jonsson et al. [34] Switzerland Randomized controlled intervention study | n = 167 ICU nurses, distributed among 26 teams | 1 control group and 1 intervention group are faced with an acute care situation to solve. | Evaluation through questionnaires and viewing of videos of the sessions. | Team leadership and task management improved in the intervention group | 8/11 |
| Eric et al. [35] Hong Kong Interdisciplinary group training programme | n = 1170 over 101 sessions | Groups made up of doctors, nurses and other health care professionals | 35-item questionnaires and a 13-item questionnaire related to the quality of training. | Simulation-based training contributed significantly to preparing hospital staff, reinforcing protocols and workflow for endotracheal intubation. | 10/11 |
| Martins et al. [36] Brazil Pre-post test design for simulation training | n= 48 doctors, nurses and nursing technicians | Pre- and post-simulation study | Knowledge test | Simulation equips professionals with skills to deal with COVID-19, generating benefits for health systems, professionals and patients. | 7/11 |
| Fregene et al. [37] London Pre-post test design for simulation training | n= 32 from the departments of anesthesia | A total of 8 scenarios were carried out | Corrective measures are established for errors detected during the simulation. | It showed that on-site simulations identified multiple operational deficiencies in the ICU isolation room and allowed corrective action to be taken prior to admission of the first patient with COVID-19. | 8/11 |
| Question | Truchot [4] | Bapteste [28] | Petrosoniak [29] * | Couto [30] | Schram [31] | Paltved [32] | Chetcuti [33] | Jonsson [34] | Eric [35] | Martins [36] | Fregene [37] |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q2 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 |
| Q3 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 |
| Q4 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 |
| Q5 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| Q6 | Concluding | Concluding | Concluding | Concluding | Concluding | Concluding | Concluding | Concluding | Concluding | Concluding | Concluding |
| Q7 | P.A. ** | P.A. ** | P.A. ** | G.A. *** | G.A. *** | P.A. ** | P.A. ** | P.A. ** | G.A. *** | P.A. ** | P.A. ** |
| Q8 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 |
| Q9 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q10 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q11 | 1 | 1 | X | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 |
| CASPe score | 9/11 | 6/11 | 7/10 | 10/11 | 10/11 | 9/11 | 8/11 | 8/11 | 10/11 | 7/11 | 8/11 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-Pérez, V.; Escrivá Peiró, D.; Sancho-Cantus, D.; Casaña Mohedo, J. In Situ Simulation: A Strategy to Restore Patient Safety in Intensive Care Units after the COVID-19 Pandemic? Systematic Review. Healthcare 2023, 11, 263. https://doi.org/10.3390/healthcare11020263
Gómez-Pérez V, Escrivá Peiró D, Sancho-Cantus D, Casaña Mohedo J. In Situ Simulation: A Strategy to Restore Patient Safety in Intensive Care Units after the COVID-19 Pandemic? Systematic Review. Healthcare. 2023; 11(2):263. https://doi.org/10.3390/healthcare11020263
Chicago/Turabian StyleGómez-Pérez, Vanesa, Dolores Escrivá Peiró, David Sancho-Cantus, and Jorge Casaña Mohedo. 2023. "In Situ Simulation: A Strategy to Restore Patient Safety in Intensive Care Units after the COVID-19 Pandemic? Systematic Review" Healthcare 11, no. 2: 263. https://doi.org/10.3390/healthcare11020263
APA StyleGómez-Pérez, V., Escrivá Peiró, D., Sancho-Cantus, D., & Casaña Mohedo, J. (2023). In Situ Simulation: A Strategy to Restore Patient Safety in Intensive Care Units after the COVID-19 Pandemic? Systematic Review. Healthcare, 11(2), 263. https://doi.org/10.3390/healthcare11020263








