Assessment of Knowledge, Perception, Experience and Phobia toward Corticosteroids Use among the General Public in the Era of COVID-19: A Multinational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Size
2.2. Ethical Statement
2.3. Study Tool
2.4. Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics
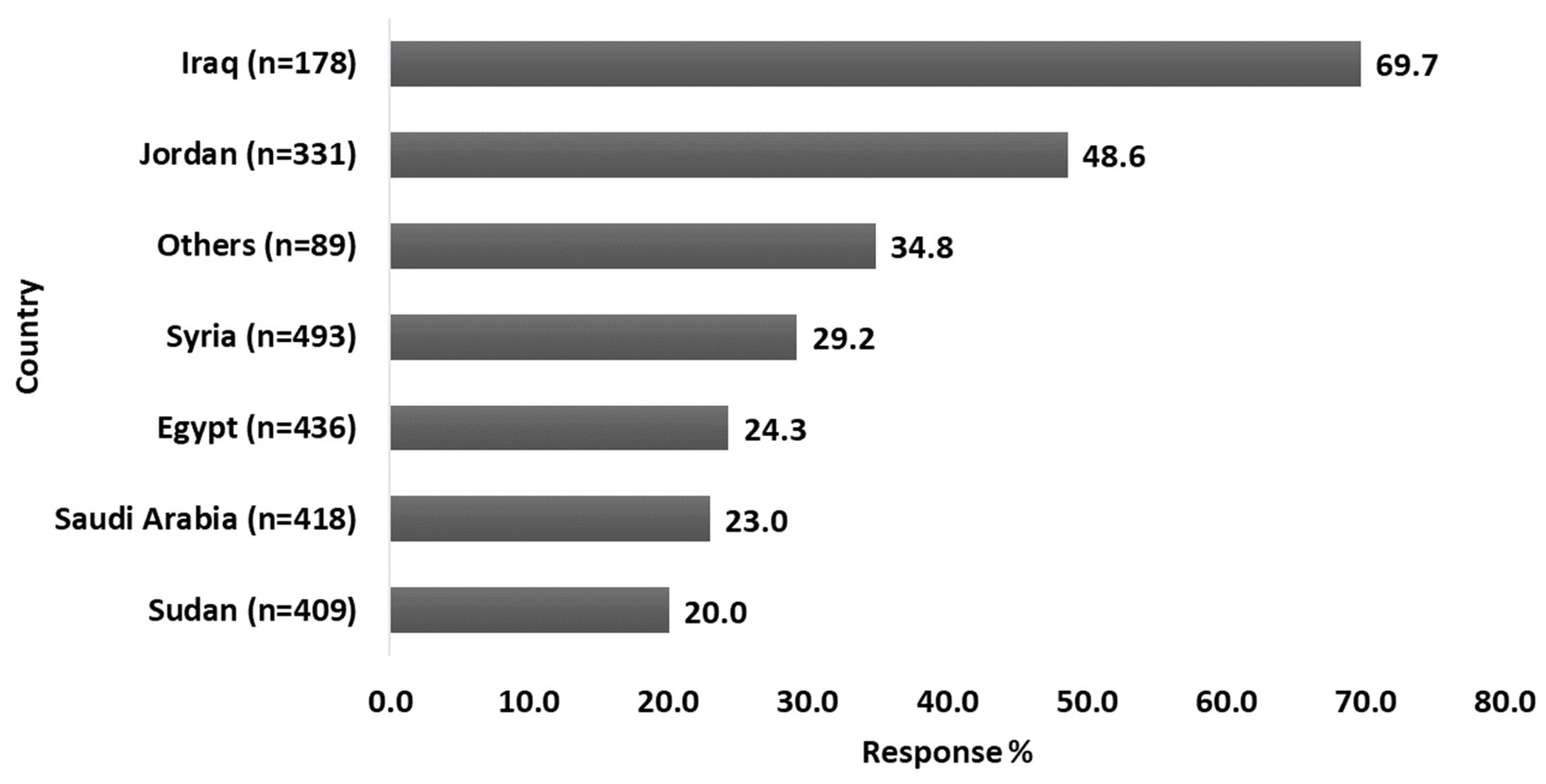
3.2. History of COVID-19 Infection
3.3. Experience with Corticosteroid Use
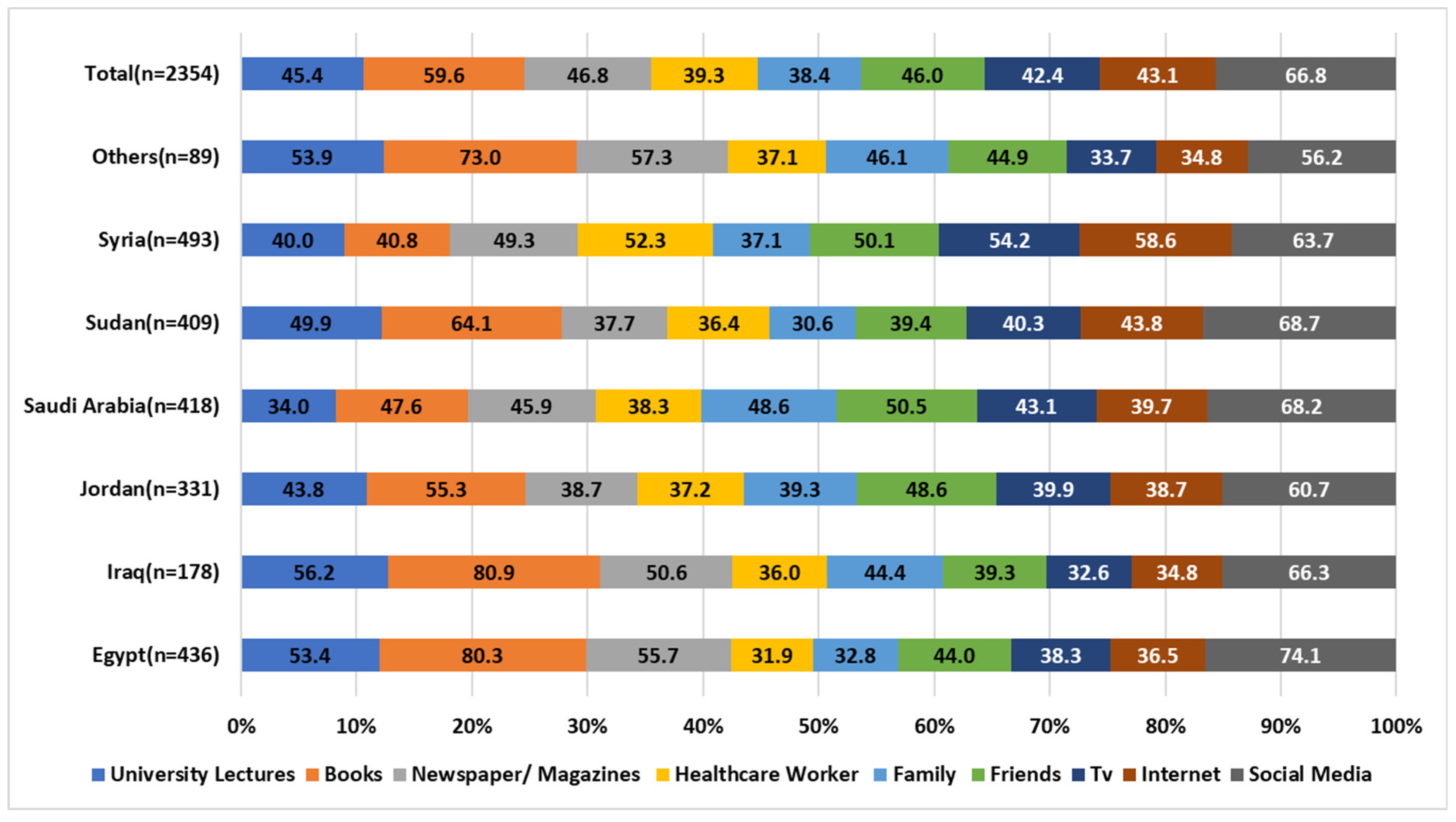
3.4. Knowledge about Corticosteroid
3.5. Corticophobia among the Participants
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alwahaibi, N.; Al Maskari, M.; Al Dhahli, B.; Al Issaei, H.; Al-Jaaidi Shadia Al Bahlani, S. One-year Review of COVID-19 in the Arab World. Qatar Med. J. 2021, 2021, 66. [Google Scholar] [CrossRef] [PubMed]
- Drożdżal, S.; Rosik, J.; Lechowicz, K.; Machaj, F.; Szostak, B.; Przybyciński, J.; Lorzadeh, S.; Kotfis, K.; Ghavami, S.; Łos, M.J. An update on drugs with therapeutic potential for SARS-CoV-2 (COVID-19) treatment. Drug Resist. Updat. 2021, 59, 100794. [Google Scholar] [CrossRef]
- Aouissi, H.A.; Kechebar, M.S.A.; Ababsa, M.; Roufayel, R.; Neji, B.; Petrisor, A.I.; Hamimes, A.; Epelboin, L.; Ohmagari, N. The Importance of Behavioral and Native Factors on COVID-19 Infection and Severity: Insights from a Preliminary Cross-Sectional Study. Healthcare 2022, 10, 1341. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Ahmet, A.; Ward, L.; Krishnamoorthy, P.; Mandelcorn, E.D.; Leigh, R.; Brown, J.P.; Cohen, A.; Kim, H. A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy. Allergy Asthma Clin. Immunol. 2013, 9, 30. [Google Scholar] [CrossRef]
- National Institutes of Health (NIH). COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines 2022. Available online: https://www.covid19treatmentguidelines.nih.gov/ (accessed on 25 July 2022).
- Buchman, A.L. Side effects of corticosteroid therapy. J. Clin. Gastroenterol. 2001, 33, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Bennadi, D. Self-medication: A current challenge. J. Basic Clin. Pharm. 2013, 5, 19. [Google Scholar] [CrossRef] [PubMed]
- van Herpen-Meeuwissen, L.J.; van den Bemt, B.J.; Derijks, H.J.; van den Bemt, P.M.; Maat, B.; van Onzenoort, H.A. The effect of Patient’s Own Medication use on patient’s self-reported medication knowledge during hospitalisation: A pre-post intervention study. J. BMC Health Serv. Res. 2022, 22, 423. [Google Scholar] [CrossRef]
- van Paassen, J.; Vos, J.S.; Hoekstra, E.M.; Neumann, K.M.I.; Boot, P.C.; Arbous, S.M. Corticosteroid use in COVID-19 patients: A systematic review and meta-analysis on clinical outcomes. Crit. Care 2020, 24, 696. [Google Scholar] [CrossRef]
- Li, A.W.; Yin, E.; Antaya, R. Topical Corticosteroid Phobia in Atopic Dermatitis: A Systematic Review. JAMA Derm. 2017, 153, 1036–1042. [Google Scholar] [CrossRef]
- Heymann, W.R. Countering Corticophobia. 2017. Available online: https://www.aad.org/dw/dw-insights-and-inquiries/pediatric-dermatology/countering-corticophobia (accessed on 15 September 2022).
- Saqib, A.; Atif, M.; Ikram, R.; Riaz, F.; Abubakar, M.; Scahill, S. Factors affecting patients’ knowledge about dispensed medicines: A Qualitative study of healthcare professionals and patients in Pakistan. PLoS ONE 2018, 13, e0197482. [Google Scholar] [CrossRef]
- Kahssay, S.W.; Mulugeta, P. Determinants of exit-knowledge of ambulatory patients on their dispensed medications: The case in the outpatient pharmacy of Mizan-Tepi University Teaching Hospital, Southwest Ethiopia. PLoS ONE 2022, 17, e0268971. [Google Scholar]
- Basheti, I.A.; Nassar, R.; Barakat, M.; Alqudah, R.; Abufarha, R.; Mukattash, T.L.; Saini, B. Pharmacists’ readiness to deal with the coronavirus pandemic: Assessing awareness and perception of roles. Res. Soc. Adm. Pharm. 2021, 17, 514–522. [Google Scholar] [CrossRef]
- Mueller, S.M.; Itin, P.; Vogt, D.R.; Walter, M.; Lang, U.; Griffin, L.L.; Euler, S. Assessment of “corticophobia” as an indicator of non-adherence to topical corticosteroids: A pilot study. J. Dermatol. Treat. 2017, 28, 104–111. [Google Scholar] [CrossRef]
- Herxheimer, A. Public understanding of drug therapy. Br. J. Clin. Pharm. 2012, 73, 943–947. [Google Scholar] [CrossRef] [PubMed]
- Elnaem, M.H.; Mosaad, M.; Abdelaziz, D.H.; Mansour, N.O.; Usman, A.; Elrggal, M.E.; Cheema, E. Disparities in Prevalence and Barriers to Hypertension Control: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 14571. [Google Scholar] [CrossRef]
- McQuaid, E.L.; Landier, W. Cultural Issues in Medication Adherence: Disparities and Directions. J. Gen. Int. Med. 2018, 33, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Al-Ganmi, A.H.A.; Alotaibi, A.; Gholizadeh, L.; Perry, L. Medication adherence and predictive factors in patients with cardiovascular disease: A cross-sectional study. Nurs. Health Sci. 2020, 22, 454–463. [Google Scholar] [CrossRef] [PubMed]
- Al-Noumani, H.; Wu, J.R.; Barksdale, D.; Sherwood, G.; AlKhasawneh, E.; Knafl, G. Health beliefs and medication adherence in patients with hypertension: A systematic review of quantitative studies. Patient Educ. Couns. 2019, 102, 1045–1056. [Google Scholar] [CrossRef]
- Alsukait, S.F.; Alshamlan, N.M.; Alhalees, Z.Z.; Alsuwaidan, S.N.; Alajlan, A.M. Topical corticosteroids knowledge, attitudes, and practices of primary care physicians. Saudi Med. J. 2017, 38, 662–665. [Google Scholar] [CrossRef]
- Sekler, O.; Segev-Becker, A.; Interator, H.; Brener, A.; Schachter-Davidov, A.; Elkon-Tamir, E.; Lebenthal, Y. Paediatricians’ practices and knowledge of corticosteroids: A national survey. Acta Paediatr. 2021, 110, 711–717. [Google Scholar] [CrossRef]
- El Hachem, M.; Gesualdo, F.; Ricci, G.; Diociaiuti, A.; Giraldi, L.; Ametrano, O.; Occella, C.; Fortina, A.B.; Milioto, M.; Arcangeli, F.; et al. Topical corticosteroid phobia in parents of pediatric patients with atopic dermatitis: A multicentre survey. Ital. J. Pediatr. 2017, 43, 22. [Google Scholar] [CrossRef] [PubMed]
- Moawad, S.; Mahé, E.; Aubert-Wastiaux, H.; Phan, A.; Maruani, A.; Chiaverini, C.; Bodemer, C.; Mazereeuw-Hautier, J.; Lasek-Duriez, A.; Droitcourt, C.; et al. Topical Corticosteroid Concerns Among Parents of Children with Psoriasis versus Atopic Dermatitis: A French Multicenter Cross-Sectional Study. Am. J. Clin. Derm. 2018, 19, 261–265. [Google Scholar] [CrossRef]
- Özçeker, D.; Uçkun, U.; İslamova, D.; Tamay, Z.; Güler, N. Corticosteroid phobia among parents of asthmatic children. Turk. J. Pediatr. 2018, 60, 142–146. [Google Scholar] [CrossRef]
- Ashique, K.T.; Kaliyadan, F.; Mohan, S.; Vijayan, S.; Chandrasekhar, D. Knowledge, Attitudes and Behavior Regarding Topical Corticosteroids in a Sample of Pharmacy Students: A Cross Sectional Survey. Indian Derm. Online J. 2018, 9, 432–434. [Google Scholar] [CrossRef] [PubMed]
- Yakar, H.; Kanbay, A. Evaluation of corticophobia in asthmatic patients. Niger. J. Clin. Pr. 2020, 23, 1033–1038. [Google Scholar] [CrossRef] [PubMed]
- Aubert-Wastiaux, H.; Moret, L.; Le Rhun, A.; Fontenoy, A.M.; Nguyen, J.M.; Leux, C.; Misery, L.; Young, P.; Chastaing, M.; Danou, N.; et al. Topical corticosteroid phobia in atopic dermatitis: A study of its nature, origins and frequency. Br. J. Derm. 2011, 165, 808–814. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; LFidell, S.; Ullman, J. Using Multivariate Statistics; Pearson: Boston, MA, USA, 2007; Volume 5. [Google Scholar]
- Ahmad, D.; Wazaify, M.; Albsoul-Younes, A. The role of the clinical pharmacist in the identification and management of corticophobia–an Interventional Study. Trop. J. Pharm. Res. 2014, 13, 445–453. [Google Scholar] [CrossRef]
- Choi, E.; Chandran, N.; Tan, C. Corticosteroid phobia: A questionnaire study using TOPICOP score. Singap. Med. J. 2020, 61, 149. [Google Scholar] [CrossRef]
- Boynton, P.M. Administering, analysing, and reporting your questionnaire. BMJ 2004, 328, 1372–1375. [Google Scholar] [CrossRef]
- Facebook. Assessment of General Perception toward the Use of Corticosteroid-Containing Drugs: A Cross-Sectional Study; Facebook: Menlo Park, CA, USA, 2022. [Google Scholar]
- Whatsapp. Assessment of General Perception toward the Use of Corticosteroid-Containing Drugs: A Cross-Sectional Study; Whatsapp: Menlo Park, CA, USA, 2022. [Google Scholar]
- Linkedin. Assessment of General Perception toward the Use of Corticosteroid-Containing Drugs: A Cross-Sectional Study; Linkedin: Sunnyvale, CA, USA, 2022. [Google Scholar]
- Ismail, Z.; Mohan, A.; Ngendahayo, C.; Aborode, A.T.; Abid, A.; dos Santos Costa, A.C.; Ahmad, S.; Essar, M.Y. Self-Medication in Africa during COVID-19 Pandemic. J. Innovaitions Pharm. 2021, 12, 1. [Google Scholar]
- Hamimes, A.; Aouissi, H.A.; Ababsa, M.; Lounis, M.; Jayarajah, U.; Napoli, C.; Kasemy, Z.A. The Effect of Preventive Measures and Vaccination against SARS-CoV-2 on the Infection Risk, Treatment, and Hospitalization: A Cross-Sectional Study of Algeria. Viruses 2022, 14, 2771. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.A.; Rasul, A.; Yousaf, R.; Haris, M.; Faheem, H.I.; Hamid, A.; Khan, H.; Khan, A.H.; Aschner, M.; Batiha, G.E.S. Combination of natural antivirals and potent immune invigorators: A natural remedy to combat COVID-19. Phytother. Res. 2021, 35, 6530–6551. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, K.; Wu, C.-P.; Bhardwaj, A.; Siuba, M. Steroids in COVID-19: An overview. Clevel. Clin. J. Med. 2020, 8, 1–4. [Google Scholar] [CrossRef]
- Fernández-Cruz, A.; Ruiz-Antorán, B.; Múñez-Rubio, E.; Sancho-López, A.; Callejas-Díaz, A.; Avendaño-Solá, C.; Ramos-Martínez, A. The Right Time for Steroids in COVID-19. Clin. Infect. Dis. 2020, 72, 1486–1487. [Google Scholar] [CrossRef]
- Shetty, Y.C.; Vinchurkar, P.; More, S.; Siddiqui, A.; Tilak, S.; Ginodia, S.; Jinturkar, S.; Pancholi, V.; Nair, N.; Goyal, R. Knowledge and Awareness Regarding Corticosteroids and Effectiveness of a Novel Steroid Educational Module among People Visiting General OPD of a Tertiary Care Hospital. Indian J. Pharm. Prac. 2022, 15, 40–45. [Google Scholar] [CrossRef]
- Sheth, N.K.; Nair, P.A. Topical steroids: Awareness and misuse among patients, pharmacists and general medical practitioner. Indian J. Derm. Vener Leprol. 2021, 87, 54–59. [Google Scholar] [CrossRef]
- Seo, H.; Song, S.Y.; Kim, D.; Park, J.H.; Shin, Y.; Lee, K.H.; Choi, S.A.; Lee, J.-Y.; Shin, W.G.; Kim, E. General Public Knowledge Regarding Topical Corticosteroids: A Nationwide Survey in South Korea. Korean J. Clin. Pharm. 2022, 32, 84–92. [Google Scholar] [CrossRef]
- Lau, W.M.; Donyai, P. Knowledge, Attitude and Advice-Giving Behaviour of Community Pharmacists Regarding Topical Corticosteroids. Pharmacy 2017, 5, 41. [Google Scholar] [CrossRef]
- Robert, S. Community-level socioeconomic status effects on adult health. J. Health Social Behav. 1998, 39, 18–37. [Google Scholar] [CrossRef]
- Case, A.; Lubotsky, D.; Paxson, C. Economic status and health in childhood: The origins of the gradient. Am. Econ. Rev. 2002, 92, 1308–1334. [Google Scholar] [CrossRef]
- Yuan, F.; Qian, D.; Huang, C.; Tian, M.; Xiang, Y.; He, Z.; Feng, Z. Analysis of awareness of health knowledge among rural residents in Western China. BMC Public Health 2015, 15, 55. [Google Scholar] [CrossRef]
- Schillinger, D.; Chittamuru, D.; Ramírez, A.S. From “infodemics” to health promotion: A novel framework for the role of social media in public health. Am. J. Public Health 2020, 110, 1393–1396. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.; Yang, L.; Chen, W.; Luo, H.; Zheng, K.; Zhang, Y.; Lian, T.; Yang, Y.; Ni, J. Current status of official WeChat accounts for public health education. J. Public Health 2021, 43, 618–624. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.; Alston, M.; Jambulingam, M.; Hunt, A. Social Media Usage for Changes in Health Practices and Health Promotion. Am. J. Public Health Res. 2022, 10, 53–62. [Google Scholar]
- Scanfeld, D.; Scanfeld, V.; Larson, E. Dissemination of health information through social networks: Twitter and antibiotics. Am. J. Infect. Control. 2010, 38, 182–188. [Google Scholar] [CrossRef]
- Antheunis, M.L.; Tates, K.; Nieboer, T. Patients’ and health professionals’ use of social media in health care: Motives, barriers and expectations. Patient Educ. Couns. 2013, 92, 426–431. [Google Scholar] [CrossRef] [PubMed]
- Huo, J.; Desai, R.; Hong, Y.-R.; Turner, K.; Mainous III, A.G.; Bian, J. Use of social media in health communication: Findings from the health information national trends survey 2013, 2014, and 2017. Cancer Control. 2019, 26, 1073274819841442. [Google Scholar] [CrossRef]
- Lambert, K.M.; Barry, P.; Stokes, G. Risk management and legal issues with the use of social media in the healthcare setting. J. Healthc. Risk Manag. 2012, 31, 41–47. [Google Scholar] [CrossRef]
- Ventola, C.L. Social media and health care professionals: Benefits, risks, and best practices. Pharm. Ther. 2014, 39, 491–520. [Google Scholar]
- Chandra, S.; Ward, P.; Mohammadnezhad, M. Factors associated with patient satisfaction in outpatient department of Suva Sub-divisional Health Center, Fiji, 2018: A mixed method study. Front. Public Health 2019, 7, 183. [Google Scholar] [CrossRef]
- Jirjees, F.; Barakat, M.; Shubbar, Q.; Othman, B.; Alzuabi, H.; Al-Obaidi, H.J. Perceptions of COVID-19 symptoms, prevention, and treatment strategies among people in seven Arab countries: A cross-sectional study. J. Infect. Public Health 2022, 15, 1108–1117. [Google Scholar] [CrossRef] [PubMed]
- Abazid, H.; Basheti, I.A.; Al-Jomaa, E.E.; Abazid, A.; Kloub, W.M. Public knowledge, beliefs, psychological responses, and behavioural changes during the outbreak of COVID-19 in the Middle East. Pharm. Pract. 2021, 19, 2306. [Google Scholar] [CrossRef]
- Fernandes, M.; Brábek, J. COVID-19, corticosteroids and public health: A reappraisal. Public Health 2021, 197, 48–55. [Google Scholar] [CrossRef]
- Ray, I.; Bardhan, M.; Hasan, M.M.; Sahito, A.M.; Khan, E.; Patel, S.; Jani, I.; Bhatt, P.K.; Sp, R.; Swed, S. Over the counter drugs and self-medication: A worldwide paranoia and a troublesome situation in India during the COVID-19 pandemic. Ann. Med. Surg. 2022, 78, 103797. [Google Scholar] [CrossRef] [PubMed]
- Choudhary, N.; Lahiri, K.; Singh, M. Increase and consequences of self-medication in dermatology during COVID-19 pandemic: An initial observation. Dermatol. Ther. 2021, 34, e14696. [Google Scholar] [CrossRef] [PubMed]
- Hon, K.L.; Tsang, Y.C.K.; Pong, N.H.; Luk, D.C.K.; Lee, V.W.; Woo, W.M.; Lam, C.Y.J.; Yeung, Y.T.E.; Chau, Y.S.S.; Chui, K.K.K.; et al. Correlations among steroid fear, acceptability, usage frequency, quality of life and disease severity in childhood eczema. J. Dermatol. Treat. 2015, 26, 418–425. [Google Scholar] [CrossRef]
- Charman, C.; Morris, A.; Williams, H. Topical corticosteroid phobia in patients with atopic eczema. Br. J. Dermatol. 2000, 142, 931–936. [Google Scholar] [CrossRef] [PubMed]
- Contento, M.; Cline, A.; Russo, M. Steroid Phobia: A review of prevalence, risk factors, and interventions. Am. J. Clin. Dermatol. 2021, 22, 837–851. [Google Scholar] [CrossRef] [PubMed]
- Müller, S.M.; Tomaschett, D.; Euler, S.; Vogt, D.R.; Herzog, L.; Itin, P. Topical corticosteroid concerns in dermatological outpatients: A cross-sectional and interventional study. Dermatology 2016, 232, 444–452. [Google Scholar] [CrossRef]
- Song, S.Y.; Jung, S.-Y.; Kim, E. Steroid phobia among general users of topical steroids: A cross-sectional nationwide survey. J. Dermatol. Treat. 2019, 30, 245–250. [Google Scholar] [CrossRef]
- Rice, J.B.; White, A.G.; Scarpati, L.M.; Wan, G.; Nelson, W.W. Long-term Systemic Corticosteroid Exposure: A Systematic Literature Review. Clin. Ther. 2017, 39, 2216–2229. [Google Scholar] [CrossRef] [PubMed]
- van Grunsven, P.M. The magnitude of fear of adverse effects as a reason for nonparticipation in drug treatment: A short review. J. Asthma 2001, 38, 113–119. [Google Scholar] [CrossRef]
- Feldman, S.R.; Huang, W.W. Steroid phobia isn’t reduced by improving patients’ knowledge of topical corticosteroids. J. Am. Acad. Dermatol. 2020, 83, e403–e404. [Google Scholar] [CrossRef] [PubMed]
- Basheti, I.A.; Nassar, R.; Barakat, M.; Alqudah, R.; Farha, R.A.; Muqatash, T.; Thiab, S.; Saini, B. Pharmacists’ perceived barriers towards delivering their emergency roles during the COVID-19 pandemic and perceived policymakers’ responsibilities. J. Pharm. Policy Pract. 2020, 13, 62. [Google Scholar] [CrossRef] [PubMed]
| Variable | Country | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Egypt (n = 436) | Iraq (n = 178) | Jordan (n = 331) | Saudi Arabia (n = 418) | Sudan (n = 409) | Syria (n = 493) | Others (n = 89) | Total (n = 2354) | p-Value * | |
| Age, years, median (IQR) | 25.0 (58.0) | 26.0 (49.0) | 31.0 (56.0) | 34.0 (57.0) | 24.0 (53) | 39.0 (57.0) | 32.0 (47.0) | 30.0 (58.0) | <0.001 $ |
| Gender | |||||||||
| Male, n (%) | 135 (31.0) | 53 (29.8) | 119 (36.0) | 127 (30.4) | 119 (29.1) | 315 (63.9) | 36 (40.4) | 904 (38.4) | <0.001 |
| Female, n (%) | 301 (69.0) | 125 (70.2) | 212 (64.0) | 291 (69.6) | 290 (70.9) | 178 (36.1) | 53 (59.6) | 1450 (61.6) | |
| Educational level | <0.001 | ||||||||
| School level, n (%) | 38 (8.7) | 15 (8.4) | 19 (5.7) | 57 (13.6) | 24 (5.9) | 116 (23.5) | 5 (5.6) | 274 (11.6) | |
| Diploma, n (%) | 20 (4.6) | 10 (5.6) | 31 (9.4) | 45 (10.8) | 20 (4.9) | 124 (25.2) | 5 (5.6) | 255 (10.8) | |
| Bachelor, n (%) | 318 (72.9) | 112 (62.9) | 223 (67.4) | 260 (62.2) | 340 (83.1) | 181 (36.7) | 60 (67.4) | 1494 (63.5) | |
| Postgraduates, n (%) | 60 (13.8) | 41 (23.0) | 58 (17.5) | 56 (13.4) | 25 (6.1) | 72 (14.6) | 19 (21.3) | 331 (14.1) | |
| Residential area | |||||||||
| Urban, n (%) | 302 (69.3) | 135 (75.8) | 306 (92.4) | 376 (90.0) | 368 (90.0) | 403 (81.7) | 77 (86.5) | 1967 (83.6) | <0.001 |
| Rural, n (%) | 134 (30.7) | 43 (24.2) | 25 (7.6) | 42 (10.0) | 41 (10.0) | 90 (18.3) | 12 (13.5) | 387 (16.4) | |
| Major | |||||||||
| Student, n (%) | 187 (42.9) | 56 (31.5) | 68 (20.5) | 81 (19.4) | 231 (56.5) | 52 (10.5) | 14 (15.7) | 689 (29.3) | <0.001 |
| Health sector, n (%) | 126 (28.9) | 76 (42.7) | 102 (30.8) | 124 (29.7) | 81 (19.8) | 141 (28.6) | 34 (38.2) | 684 (29.1) | |
| Non-Health sector, n (%) | 49 (11.2) | 32 (18.0) | 86 (26.0) | 107 (25.6) | 56 (13.7) | 188 (38.1) | 22 (24.7) | 540 (22.9) | |
| Unemployed/retired, n (%) | 74 (17.0) | 14 (7.9) | 75 (22.7) | 106 (25.4) | 41 (10.0) | 112 (22.7) | 19 (21.3) | 441 (18.7) | |
| Do you have any chronic diseases? | |||||||||
| No, n (%) | 382 (87.6) | 153 (86.0) | 272 (82.2) | 306 (73.2) | 339 (82.9) | 401 (81.3) | 71 (79.8) | 1924 (81.7) | |
| Yes, n (%) | 54 (12.4) | 25 (14.0) | 59 (17.8) | 112 (26.8) | 70 (17.1) | 92 (18.7) | 18 (20.2) | 430 (18.3) | <0.001 |
| If yes, which of the following could apply? n (%) | |||||||||
| Hypertension (High blood pressure) | 9 (2.1) | 6 (3.4) | 18 (5.4) | 27 (6.5) | 11 (2.7) | 61 (12.4) | 6 (6.7) | 138 (5.9) | <0.001 |
| Diabetes mellitus | 34 (7.8) | 25 (14.0) | 13 (3.9) | 27 (6.5) | 9 (2.2) | 29 (5.9) | 18 (20.2) | 155 (6.6) | <0.001 |
| Obesity/overweight | 34 (7.8) | 17 (9.6) | 32 (9.7) | 40 (9.6) | 23 (5.6) | 47 (9.5) | 5 (5.6) | 198 (8.4) | <0.001 |
| Cardiovascular diseases (e.g., Stroke) | 54 (12.4) | 20 (11.2) | 11 (3.3) | 66 (15.8) | 41 (10.0) | 17 (3.4) | 18 (20.2) | 227 (9.6) | <0.001 |
| Kidney disease | 5 (1.1) | 5 (2.8) | 6 (1.8) | 11 (2.6) | 11 (2.7) | 18 (3.7) | 5 (5.6) | 61 (2.6) | <0.001 |
| Osteoporosis | 10 (2.3) | 12 (6.7) | 6 (1.8) | 12 (2.9) | 8 (2.0) | 62 (12.6) | 11 (12.4) | 121 (5.1) | <0.001 |
| Depression | 35 (8.0) | 10 (5.6) | 17 (5.1) | 23 (5.5) | 20 (4.9) | 50 (10.1) | 5 (5.6) | 160 (6.8) | <0.001 |
| Rheumatoid Arthritis | 9 (2.1) | 6 (3.4) | 10 (3.0) | 21 (5.0) | 9 (2.2) | 60 (12.2) | 5 (5.6) | 120 (5.1) | <0.001 |
| Immune disorder | 13 (3.0) | 6 (3.4) | 14 (4.2) | 14 (3.3) | 9 (2.2) | 20 (4.1) | 6 (6.7) | 82 (3.5) | <0.001 |
| Respiratory disease (e.g., Asthma) | 19 (4.4) | 8 (4.5) | 14 (4.2) | 30 (7.2) | 35 (8.6) | 30 (6.1) | 13 (14.6) | 149 (6.3) | <0.001 |
| Dermatological disorder (e.g., acne, psoriasis) | 36 (8.3) | 15 (8.4) | 15 (4.5) | 37 (8.9) | 34 (8.3) | 32 (6.5) | 18 (20.2) | 187 (7.9) | <0.001 |
| Others | 31 (7.1) | 12 (6.7) | 25 (7.6) | 42 (10.0) | 26 (6.4) | 27 (5.5) | 5 (5.6) | 168 (7.1) | <0.001 |
| Residential Country | ||||||||
|---|---|---|---|---|---|---|---|---|
| Question | n (%) | |||||||
| Egypt (n = 436) | Iraq (n = 178) | Jordan (n = 331) | Saudi Arabia (n = 418) | Sudan (n = 409) | Syria (n = 493) | Others (n = 89) | Total (n = 2354) | |
| Have you been infected with COVID-19? | ||||||||
| 289 (66.3) | 65 (36.5) | 129 (39.0) | 267 (63.9) | 332 (81.2) | 329 (66.7) | 46 (51.7) | 1457 (61.9) |
| 147 (33.7) | 113 (63.5) | 202 (61.0) | 151 (36.1) | 77 (18.8) | 164 (33.3) | 43 (48.3) | 897 (38.1) |
| How did you rate the severity | ||||||||
| 0 (0.0) | 1 (0.6) | 0 (0.0) | 4 (1.0) | 0 (0.0) | 1 (0.2) | 0 (0.0) | 6 (0.3) |
| 84 (19.3) | 58 (32.6) | 111 (33.5) | 86 (20.6) | 53 (13.0) | 92 (18.7) | 22 (24.7) | 506 (21.5) |
| 60 (13.8) | 52 (29.2) | 82 (24.8) | 47 (11.2) | 23 (5.6) | 62 (12.6) | 18 (20.2) | 344 (14.6) |
| 3 (0.7) | 2 (1.1) | 9 (2.7) | 14 (3.3) | 1 (0.2) | 9 (1.8) | 3 (3.4) | 41 (1.7) |
| How many times have you been infected with COVID-19? | ||||||||
| 88 (20.2) | 62 (34.8) | 138 (41.7) | 121 (28.9) | 52 (12.7) | 118 (23.9) | 34 (38.2) | 613 (26.0) |
| 45 (10.3) | 35 (19.7) | 57 (17.2) | 28 (6.7) | 20 (4.9) | 33 (6.7) | 8 (9.0) | 226 (9.6) |
| 14 (3.2) | 16 (9.0) | 7 (2.1) | 2 (0.5) | 5 (1.2) | 13 (2.6) | 1 (1.1) | 58 (2.5) |
| Did you get your COVID-19 vaccine? | ||||||||
| 9 (2.1) | 15 (8.4) | 8 (2.4) | 4 (1.0) | 42 (10.3) | 27 (5.5) | 9 (10.1) | 114 (4.8) |
| 138 (31.7) | 98 (55.1) | 194 (58.6) | 147 (35.2) | 35 (8.6) | 137 (27.8) | 34 (38.2) | 783 (33.3) |
| Residential Country n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Question | Egypt | Iraq | Jordan | Saudi Arabia | Sudan | Syria | Others | Total |
| If your answer was yes, how long did you (or he/she) use it? | ||||||||
| 27 (25.5) | 74 (59.7) | 61 (37.9) | 20 (20.8) | 25 (30.5) | 55 (38.2) | 11 (35.5) | 273 (36.7) |
| 10 (9.4) | 36 (29.0) | 42 (26.1) | 35 (36.5) | 23 (28.0) | 37 (25.7) | 7 (22.6) | 190 (25.5) |
| 14 (13.2) | 9 (7.3) | 20 (12.4) | 12 (12.5) | 14 (17.1) | 18 (12.5) | 3 (9.7) | 90 (12.1) |
| 55 (51.9) | 5 (4.0) | 38 (23.6) | 29 (30.2) | 20 (24.4) | 34 (23.6) | 10 (32.3) | 191 (25.7) |
| What was the used dosage form? More than one option is/are allowed | ||||||||
| 50 (47.2) | 63 (50.8) | 90 (55.9) | 51 (53.1) | 41 (50.0) | 61 (42.4) | 19 (61.3) | 375 (50.4) |
| 40 (37.7) | 37 (29.8) | 65 (40.4) | 29 (30.2) | 26 (31.7) | 47 (32.6) | 10 (32.3) | 254 (34.1) |
| 71 (67.0) | 75 (60.5) | 105 (65.2) | 48 (50.0) | 52 (63.4) | 86 (59.7) | 25 (80.6) | 462 (62.1) |
| 42 (39.6) | 64 (51.6) | 67 (41.6) | 21 (21.9) | 16 (19.5) | 50 (34.7) | 13 (41.9) | 273 (36.7) |
| 24 (22.6) | 29 (23.4) | 36 (22.4) | 7 (7.3) | 18 (22.0) | 22 (15.3) | 9 (29.0) | 145 (19.5) |
| What was the main indication for corticosteroids use? More than one option is/are allowed | ||||||||
| 45 (42.5) | 41 (33.1) | 75 (46.6) | 30 (31.3) | 37 (45.1) | 61 (42.4) | 16 (51.6) | 305 (41.0) |
| 45 (42.5) | 47 (37.9) | 51 (31.7) | 11 (11.5) | 13 (15.9) | 18 (12.5) | 9 (29.0) | 194 (26.1) |
| 41 (38.7) | 52 (41.9) | 90 (55.9) | 54 (56.3) | 40 (48.8) | 88 (61.1) | 18 (58.1) | 383 (51.5) |
| 21 (19.8) | 31 (25.0) | 33 (20.5) | 16 (16.7) | 21 (25.6) | 64 (44.4) | 7 (22.6) | 193 (25.9) |
| 9 (8.5) | 11 (8.9) | 24 (14.9) | 10 (10.4) | 13 (15.9) | 17 (11.8) | 3 (9.7) | 87 (11.7) |
| 9 (8.5) | 10 (8.1) | 22 (13.7) | 7 (7.3) | 12 (14.6) | 24 (16.7) | 4 (12.9) | 88 (11.8) |
| 25 (23.6) | 39 (31.5) | 39 (24.2) | 18 (18.8) | 25 (30.5) | 50 (34.7) | 12 (38.7) | 208 (28.0) |
| Did you suffer from any of the following side effects following Corticosteroid usage? More than one option is/are allowed | ||||||||
| 32 (30.2) | 51 (41.1) | 74 (46.0) | 34 (35.4) | 29 (35.4) | 97 (67.4) | 18 (58.1) | 335 (45.0) |
| 18 (17.0) | 31 (25.0) | 29 (18.0) | 15 (15.6) | 22 (26.8) | 84 (58.3) | 8 (25.8) | 207 (27.8) |
| 21 (19.8) | 24 (19.4) | 33 (20.5) | 28 (29.2) | 19 (23.2) | 60 (41.7) | 9 (29.0) | 194 (26.1) |
| 20 (18.9) | 37 (29.8) | 24 (14.9) | 14 (14.6) | 17 (20.7) | 38 (26.4) | 7 (22.6) | 157 (21.1) |
| 37 (34.9) | 47 (37.9) | 66 (41.0) | 28 (29.2) | 31 (37.8) | 32 (22.2) | 13 (41.9) | 254 (34.1) |
| 6 (5.7) | 10 (8.1) | 12 (7.5) | 8 (8.3) | 6 (7.3) | 15 (10.4) | 2 (6.5) | 59 (7.9) |
| 12 (11.3) | 24 (19.4) | 18 (11.2) | 11 (11.5) | 14 (17.1) | 17 (11.8) | 6 (19.4) | 102 (13.7) |
| 11 (10.4) | 23 (18.5) | 19 (11.8) | 10 (10.4) | 10 (12.2) | 66 (45.8) | 6 (19.4) | 145 (19.5) |
| 9 (8.5) | 28 (22.6) | 28 (17.4) | 10 (10.4) | 17 (20.7) | 31 (21.5) | 6 (19.4) | 129 (17.3) |
| Residential Country n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Statements | Egypt (n = 436) | Iraq (n = 178) | Jordan (n = 331) | Saudi Arabia (n = 418) | Sudan (n = 409) | Syria (n = 493) | Others (n = 89) | Total (n = 2354) |
| 377 (86.5) | 150 (84.3) | 210 (63.4) | 258 (61.7) | 265 (64.8) | 315 (63.9) | 71 (79.8) | 1646 (69.9) |
| 359 (82.3) | 138 (77.5) | 196 (59.2) | 201 (48.1) | 233 (57.0) | 301 (61.1) | 48 (53.9) | 1476 (62.7) |
| 341 (78.2) | 140 (78.7) | 221 (66.8) | 239 (57.2) | 276 (67.5) | 302 (61.3) | 62 (69.7) | 1581 (67.2) |
| 330 (75.7) | 134 (75.3) | 224 (67.7) | 262 (62.7) | 253 (61.9) | 260 (52.7) | 60 (67.4) | 1523 (64.7) |
| 371 (85.1) | 146 (82.0) | 255 (77.0) | 300 (71.8) | 279 (68.2) | 331 (67.1) | 65 (73.0) | 1747 (74.2) |
| 357 (81.9) | 144 (80.9) | 233 (70.4) | 296 (70.8) | 286 (69.9) | 321 (65.1) | 67 (75.3) | 1704 (72.4) |
| Potential side effects of long-term treatment of Corticosteroids are: | ||||||||
| 365 (83.7) | 145 (81.5) | 252 (76.1) | 281 (67.2) | 260 (63.6) | 342 (69.4) | 64 (71.9) | 1709 (72.6) |
| 278 (63.8) | 119 (66.9) | 180 (54.4) | 172 (41.1) | 197 (48.2) | 296 (60.0) | 46 (51.7) | 1288 (54.7) |
| 297 (68.1) | 122 (68.5) | 182 (55.0) | 202 (48.3) | 237 (57.9) | 290 (58.8) | 53 (59.6) | 1383 (58.8) |
| 326 (74.8) | 136 (76.4) | 178 (53.8) | 192 (45.9) | 232 (56.7) | 248 (50.3) | 57 (64.0) | 1369 (58.2) |
| 284 (65.1) | 113 (63.5) | 183 (55.3) | 219 (52.4) | 218 (53.3) | 207 (42.0) | 54 (60.7) | 1278 (54.3) |
| 299 (68.6) | 131 (73.6) | 173 (52.3) | 156 (37.3) | 178 (43.5) | 202 (41.0) | 52 (58.4) | 1191 (50.6) |
| 302 (69.3) | 125 (70.2) | 162 (48.9) | 162 (38.8) | 198 (48.4) | 203 (41.2) | 52 (58.4) | 1204 (51.1) |
| 278 (63.8) | 124 (69.7) | 193 (58.3) | 194 (46.4) | 197 (48.2) | 311 (63.1) | 56 (62.9) | 1353 (57.5) |
| Knowledge score, Mean (STD) * | 10.5 (3.7) | 10.5 (3.9) | 8.6 (4.2) | 7.5 (4.1) | 8.1 (4.1) | 8.0 (5.3) | 9.1 (4.3) | 8.7 (4.5) |
| Statement | Residential Country, Mean (STD) | |||||||
|---|---|---|---|---|---|---|---|---|
| Egypt | Iraq | Jordan | Saudi Arabia | Sudan | Syria | Others | Total | |
| 4.3 (0.9) | 3.6 (1.1) | 3.8 (1.1) | 3.9 (1.1) | 4.2 (1.0) | 3.9 (1.1) | 3.9 (1.1) | 4.0 (1.1) |
| 4.1 (0.9) | 4.5 (0.9) | 4.0 (0.9) | 3.9 (1.0) | 4.1 (0.9) | 4.1 (0.9) | 3.9 (1.0) | 4.1 (0.9) |
| 4.1 (0.9) | 4.3 (0.9) | 3.9 (0.9) | 3.8 (1.0) | 4.1 (0.9) | 4.0 (0.9) | 3.7 (1.0) | 4.0 (1.0) |
| 4.0 (1.0) | 4.2 (1.0) | 3.9 (1.0) | 3.9 (1.0) | 4.1 (0.9) | 4.0 (1.0) | 3.7 (1.0) | 4.0 (1.0) |
| 4.0 (1.1) | 4.2 (1.0) | 3.8 (1.1) | 3.8 (1.1) | 4.1 (1.0) | 4.1 (1.0) | 3.7 (1.1) | 4.0 (1.1) |
| 4.0 (1.1) | 4.1 (1.1) | 3.8 (1.0) | 3.9 (1.1) | 3.9 (1.0) | 4.0 (1.0) | 3.7 (1.2) | 3.9 (1.1) |
| 3.1 (1.3) | 3.7 (1.3) | 3.2 (1.2) | 3.2 (1.3) | 3.5 (1.1) | 3.7 (1.2) | 3.0 (1.2) | 3.4 (1.3) |
| 3.8 (1.0) | 3.6 (1.3) | 3.6 (1.1) | 3.7 (1.1) | 4.0 (1.0) | 3.8 (1.0) | 3.6 (1.1) | 3.8 (1.1) |
| 4.1 (1.0) | 4.1 (1.0) | 3.8 (1.1) | 3.9 (1.0) | 4.1 (1.0) | 3.9 (1.0) | 3.7 (1.1) | 4.0 (1.0) |
| 3.9 (1.0) | 4.1 (1.0) | 3.7 (1.0) | 3.7 (1.1) | 3.8 (1.1) | 3.9 (1.0) | 3.6 (1.1) | 3.8 (1.1) |
| 3.6 (1.1) | 3.8 (1.1) | 3.7 (1.1) | 3.5 (1.2) | 3.8 (1.1) | 3.8 (1.1) | 3.2 (1.2) | 3.7 (1.1) |
| 3.7 (1.1) | 3.6 (1.2) | 3.7 (1.1) | 3.7 (1.1) | 3.7 (1.0) | 3.8 (1.1) | 3.4 (1.1) | 3.7 (1.1) |
| Overall scores per country, mean (STD) | 3.9 (0.3) | 4.0 (0.3) | 3.8 (0.2) | 3.7 (0.2) | 4.0 (0.2) | 3.9 (0.1) | 3.6 (0.3) | 3.9 (0.2) |
| Category of the corticophobia score * | High | High | High | High | High | High | High | High |
| Predictor | p-Value | Odds Ratio | 95% Confidence Interval | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| Age (Years) | 0.02 | 1.034 | 1.005 | 1.063 |
| Gender (Ref = Male) | ||||
| Female | 0.018 | 0.794 | 0.629 | 1.571 |
| Major (Ref = Unemployed) | ||||
| Health sector | 0.514 | 0.787 | 0.384 | 1.615 |
| Working in Non-health sector | 0.789 | 1.137 | 0.444 | 2.912 |
| Student | 0.125 | 0.257 | 0.045 | 1.462 |
| Educational level (Ref = School level) | ||||
| Bachelor | 0.036 | 0.439 | 0.686 | 3.02 |
| Diploma | 0.04 | 0.894 | 1.053 | 9.093 |
| Postgraduates | 0.034 | 0.491 | 0.449 | 4.954 |
| COVID-19 Infection (Ref = Yes) | ||||
| No | 0.319 | 1.352 | 0.747 | 2.447 |
| Experience with corticosteroids side effects (Ref = Yes) | 0.003 | 2.126 | 1.29 | 3.504 |
| No | ||||
| Knowledge score | 0.009 | 0.841 | 0.61 | 1.158 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barakat, M.; Elnaem, M.H.; Al-Rawashdeh, A.; Othman, B.; Ibrahim, S.; Abdelaziz, D.H.; Alshweiki, A.O.; Kharaba, Z.; Malaeb, D.; Syed, N.K.; et al. Assessment of Knowledge, Perception, Experience and Phobia toward Corticosteroids Use among the General Public in the Era of COVID-19: A Multinational Study. Healthcare 2023, 11, 255. https://doi.org/10.3390/healthcare11020255
Barakat M, Elnaem MH, Al-Rawashdeh A, Othman B, Ibrahim S, Abdelaziz DH, Alshweiki AO, Kharaba Z, Malaeb D, Syed NK, et al. Assessment of Knowledge, Perception, Experience and Phobia toward Corticosteroids Use among the General Public in the Era of COVID-19: A Multinational Study. Healthcare. 2023; 11(2):255. https://doi.org/10.3390/healthcare11020255
Chicago/Turabian StyleBarakat, Muna, Mohamed Hassan Elnaem, Amani Al-Rawashdeh, Bayan Othman, Sarah Ibrahim, Doaa H. Abdelaziz, Anas O. Alshweiki, Zelal Kharaba, Diana Malaeb, Nabeel Kashan Syed, and et al. 2023. "Assessment of Knowledge, Perception, Experience and Phobia toward Corticosteroids Use among the General Public in the Era of COVID-19: A Multinational Study" Healthcare 11, no. 2: 255. https://doi.org/10.3390/healthcare11020255
APA StyleBarakat, M., Elnaem, M. H., Al-Rawashdeh, A., Othman, B., Ibrahim, S., Abdelaziz, D. H., Alshweiki, A. O., Kharaba, Z., Malaeb, D., Syed, N. K., Nashwan, A. J., Adam, M. F., Alzayer, R., Albarbandi, M. S., Abu-Farha, R. K., Sallam, M., Barakat, Y., & Mansour, N. O. (2023). Assessment of Knowledge, Perception, Experience and Phobia toward Corticosteroids Use among the General Public in the Era of COVID-19: A Multinational Study. Healthcare, 11(2), 255. https://doi.org/10.3390/healthcare11020255









