A Scoping Review on COVID-19 Vaccine Hesitancy among the Lesbian, Gay, Bisexual, Transgender, Queer, Intersex and Asexual (LGBTQIA+) Community and Factors Fostering Its Refusal
Abstract
1. Introduction
Objectives of the Study
2. Materials and Methods
2.1. Stage 1: Source of Information
2.2. Stage 2: Search Strategy
2.3. Stage 3: Process of Selection
2.4. Eligibility Criteria
2.4.1. Inclusion Criteria
- Scholarly articles published from the year 2020 onwards;
- Scientific literature discussing vaccine hesitancy among the LGBTQIA+ population only
- Studies investigating hesitancy to be vaccinated against coronavirus only were considered for this study;
- Quantitative, qualitative and mixed methods studies were encompassed for analysis;
- Studies conducted in high-, low- and middle-income countries were encompassed for this study;
- Research articles published in peer-reviewed, indexed journals and abstracts;
- Studies correlating the HIV status of the target population and vaccine hesitancy;
- Manuscripts with a core theme of COVID-19 vaccine hesitancy and barriers to acceptance;
- Studies published in only the English language.
2.4.2. Exclusion Criteria
- Articles published before 2021;
- Studies concerned with vaccine hesitancy other than COVID-19 vaccines;
- Scientific literature discussing vaccine hesitancy among the general population or populations other than the LGBTQIA+ community;
- Manuscripts published in languages other than English.
2.5. Data Charting
2.6. Data Items
3. Result
3.1. Selection of Source of Evidence
3.2. Characteristics and Results of Source of Evidence
3.3. Summary of Charted Data
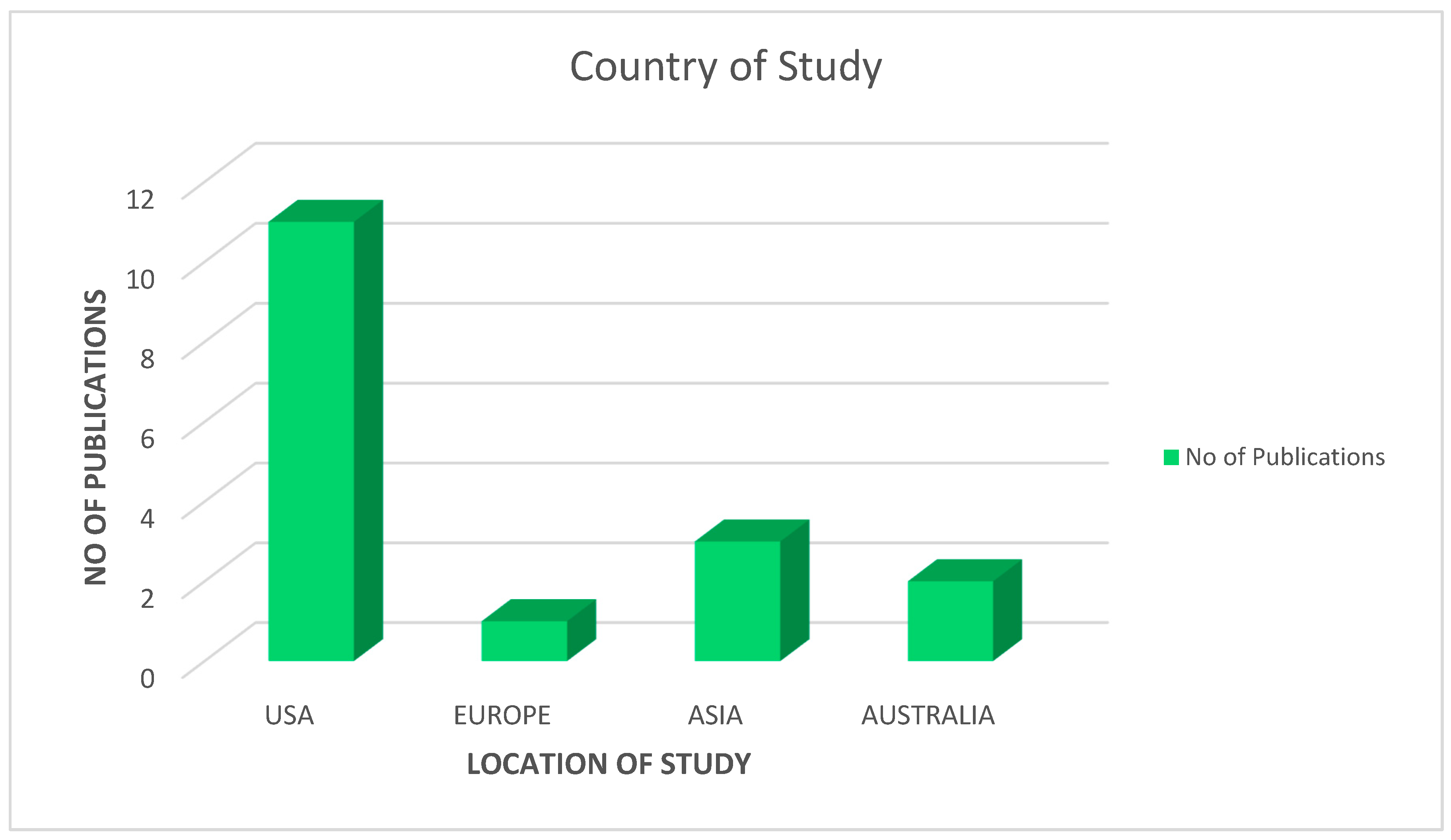
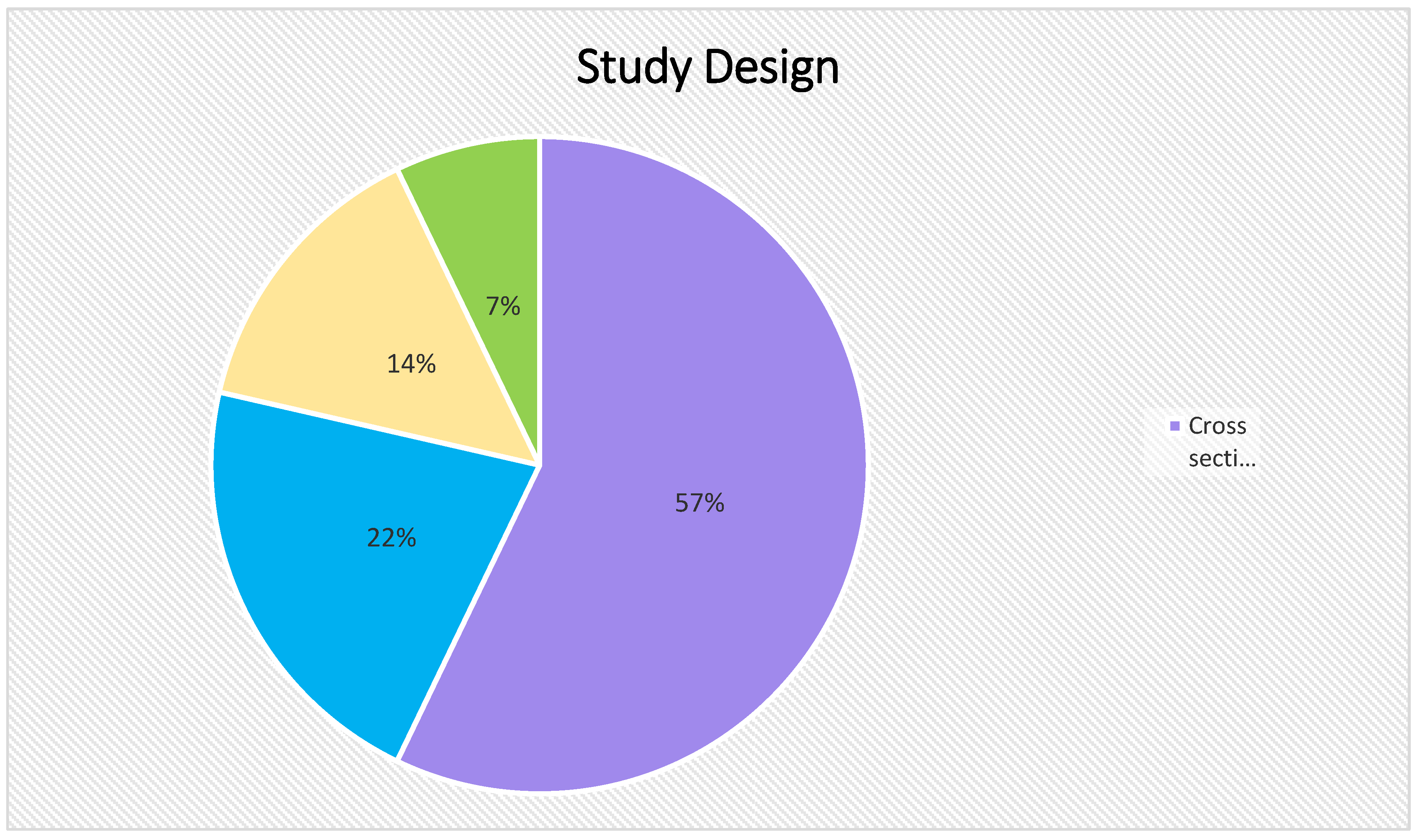
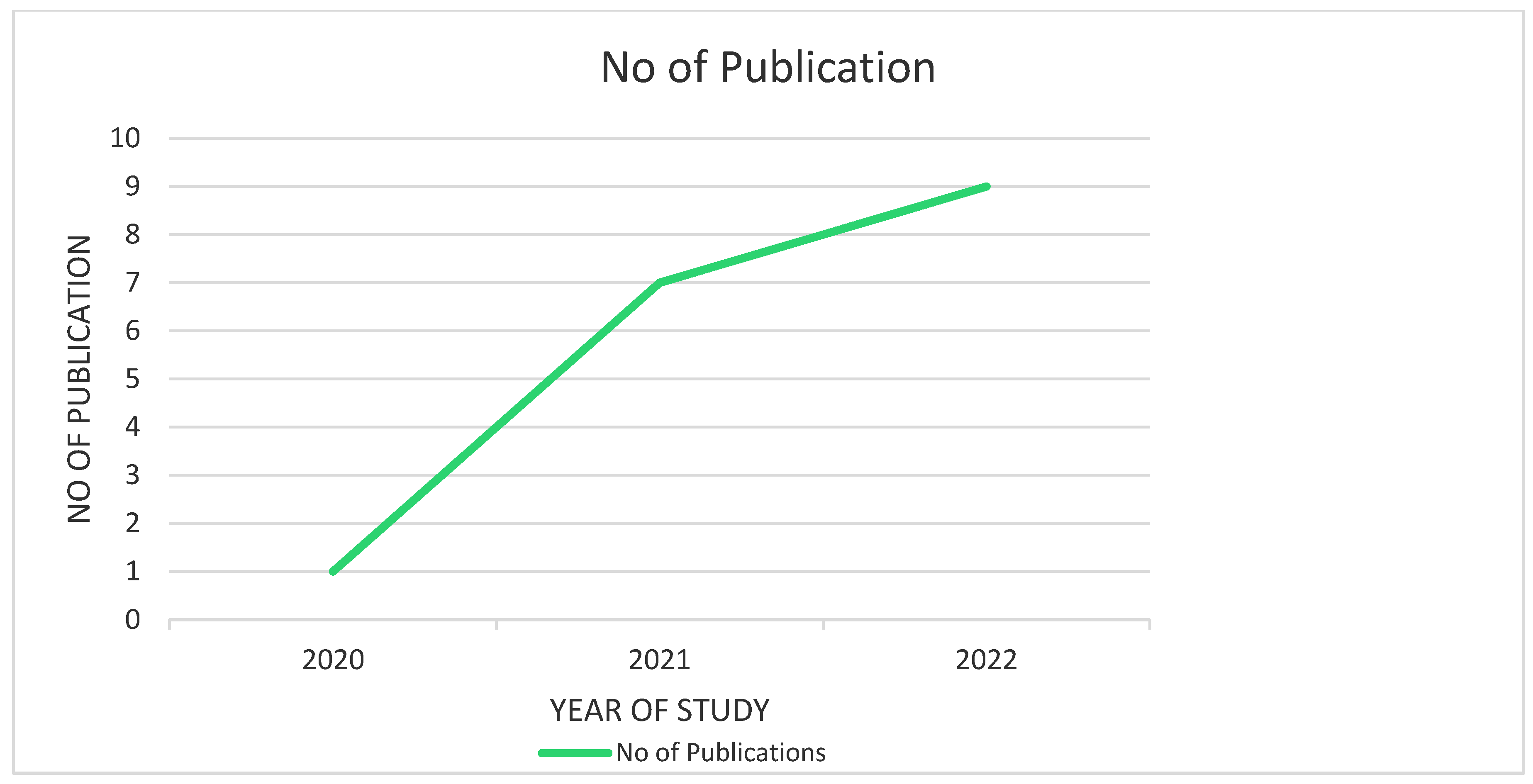
3.3.1. Characteristics of Charted Data
3.3.2. Results of Factors Influencing Vaccine Uptake among LGBTQIA+ Population
4. Discussion
4.1. The Current Scenario
4.2. Common Elements Influencing Vaccine Acceptance and Refusal
4.3. Determinants of Vaccine Hesitancy Specific to the LGBTQIA+ Community
4.3.1. Systemic Discrimination
4.3.2. Social Stigma
4.3.3. Medical Mistrust
4.3.4. HIV Status
4.4. The Need of the Hour
4.5. Mental Health and Vaccine Hesitancy
4.6. LGBTQIA+ Inclusivity in Vaccination and Public Health
5. Conclusions
5.1. Knowledge Gaps
5.2. Limitations
5.3. Directions of Future Research
6. Conceptual Framework
- I.
- Inclusive healthcare environment;
- II.
- Digital health interventions.
6.1. Rationale for Developing an Inclusive Healthcare Environment and Digital Health Interventions to Address Vaccine Hesitancy among LGBTQIA+ Individuals
6.2. Inclusive Healthcare Environment
6.3. Digital Health Interventions
6.4. Development of “mHealth” App for Facilitating Vaccination Programme for LGBTQIA+ Population
- Efficient mobile application development team;
- Effective designing of the mobile application;
- Testing of the prototype application;
- Components and features of the mobile application;
- Assuring privacy and data security.
6.5. Barriers to Promote Inclusivity and Implementation of Digital Health Technologies
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- She, J.; Jiang, J.; Ye, L.; Hu, L.; Bai, C.; Song, Y. 2019 novel coronavirus of pneumonia in Wuhan, China: Emerging attack and management strategies. Clin. Transl. Med. 2020, 9, 19. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19 (accessed on 11 March 2020).
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; Manzo, M.L.; Reingold, A.; et al. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Troiano, G.; Nardi, A. Vaccine hesitancy in the era of COVID-19. Public Health 2021, 194, 245–251. [Google Scholar] [CrossRef]
- Chatterjee, S.; Biswas, P.; Guria, R.T. LGBTQ care at the time of COVID-19. Diabetes Metab. Syndr. 2020, 14, 1757–1758. [Google Scholar] [CrossRef]
- Newman, P.A.; Reid, L.; Tepjan, S.; Fantus, S.; Allan, K.; Nyoni, T.; Guta, A.; Williams, C.C. COVID-19 vaccine hesitancy among marginalized populations in the U.S. and Canada: Protocol for a scoping review. PLoS ONE 2022, 17, e0266120. [Google Scholar] [CrossRef]
- Barchielli, B.; Cricenti, C.; Gallè, F.; Sabella, E.A.; Liguori, F.; Da Molin, G.; Liguori, G.; Orsi, G.B.; Giannini, A.M.; Ferracuti, S.; et al. Climate Changes, Natural Resources Depletion, COVID-19 Pandemic, and Russian-Ukrainian War: What Is the Impact on Habits Change and Mental Health? Int. J. Environ. Res. Public Health 2022, 19, 11929. [Google Scholar] [CrossRef]
- Ormiston, C.K.; Williams, F. LGBTQ youth mental health during COVID-19: Unmet needs in public health and policy. Lancet 2022, 399, 501–503. [Google Scholar] [CrossRef]
- Nowaskie, D.Z.; Roesler, A.C. The impact of COVID-19 on the LGBTQ+ community: Comparisons between cisgender, heterosexual people, cisgender sexual minority people, and gender minority people. Psychiatry Res. 2022, 309, 114391. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Azucar, D.; Slay, L.; Valerio, D.G.; Kipke, M.D. Barriers to COVID-19 Vaccine Uptake in the LGBTQIA Community. Am. J. Public Health 2022, 112, 405–407. [Google Scholar] [CrossRef] [PubMed]
- Low, A.; Wright, C.; Platt, J.; Chang, C.; Mantell, J.E.; Romero, E.; Hoos, D.; Mannheimer, S.; Greenleaf, A.; Castor, D.; et al. COVID-19 Vaccine Uptake and Factors Associated With Being Unvaccinated Among Lesbian, Gay, Bisexual, Transgender, Queer, and Other Sexual Identities (LGBTQ+) New Yorkers. Open Forum Infect. Dis. 2022, 9, ofac260. [Google Scholar] [CrossRef]
- Holt, M.; MacGibbon, J.; Bavinton, B.; Broady, T.; Clackett, S.; Ellard, J.; Kolstee, J.; Molyneux, A.; Murphy, D.; Power, C.; et al. COVID-19 Vaccination Uptake and Hesitancy in a National Sample of Australian Gay and Bisexual Men. AIDS Behav. 2022, 26, 2531–2538. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, R.; Sullivan, S.; Pitter, R.; Hunter, A.; Chavanduka, T. COVID-19 Pandemic Optimism and Vaccine Willingness among an Online Sample of US Gay, Bisexual, and Other Men Who Have Sex with Men. Vaccines 2021, 9, 745. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, E.R.; Balise, R.; Metheny, N.; Jose Baeza Robba, M.; Mayo, D.; Michel, C.; Chan, B.; Safren, S.A.; Harkness, A. Factors associated with latino sexual minority men’s likelihood and motivation for obtaining a COVID-19 vaccine: A mixed-methods study. J. Behav. Med. 2022, 27, 1–13. [Google Scholar] [CrossRef]
- Ousseine, Y.M.; Vaux, S.; Vandentorren, S.; Bonmarin, I.; Champenois, K.; Lydié, N.; Velter, A. Predictors of Uncertainty and Unwillingness to Receive the COVID-19 Vaccine in Men Who Have Sex with Men in France. Int. J. Environ. Res. Public Health 2022, 19, 5372. [Google Scholar] [CrossRef] [PubMed]
- Prestage, G.; Storer, D.; Jin, F.; Haire, B.; Maher, L.; Philpot, S.; Bavinton, B.; Saxton, P.; Murphy, D.; Holt, M.; et al. COVID-19 Vaccine Uptake and Its Impacts in a Cohort of Gay and Bisexual Men in Australia. AIDS Behav. 2022, 26, 2692–2702. [Google Scholar] [CrossRef] [PubMed]
- Abramovich, A.; Pang, N.; Kunasekaran, S.; Moss, A.; Kiran, T.; Pinto, A.D. Examining COVID-19 vaccine uptake and attitudes among 2SLGBTQ+ youth experiencing homelessness. BMC Public Health 2022, 22, 122. [Google Scholar] [CrossRef]
- Lin, Y.-J.; Chang, Y.-P.; Chou, W.-J.; Yen, C.-F. Explicit and Intrinsic Intention to Receive COVID-19 Vaccination among Heterosexuals and Sexual Minorities in Taiwan. Int. J. Environ. Res. Public Health 2021, 18, 7260. [Google Scholar] [CrossRef]
- da Silva, D.T.; Biello, K.; Lin, W.; Valente, P.; Mayer, K.; Hightow-Weidman, L.; Bauermeister, J. COVID-19 Vaccine Acceptance among an Online Sample of Sexual and Gender Minority Men and Transgender Women. Vaccines 2021, 9, 204. [Google Scholar] [CrossRef]
- Levandowski, B.A.; Miller, S.B.; Ran, D.; Pressman, E.A.; Van der Dye, T. Piling it on: Perceived stress and lack of access to resources among US-based LGBTQ+ community members during the COVID-19 pandemic. PLoS ONE 2022, 17, e0271162. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Chan, P.S.-F.; Chen, S.; Fang, Y.; Cao, H.; Chen, H.; Hu, T.; Chen, Y.; Zhou, X.; Wang, Z. Factors Predicting COVID-19 Vaccination Uptake Among Men Who Have Sex With Men in China: An Observational Prospective Cohort Study. Front. Med. 2022, 9, 838973. [Google Scholar] [CrossRef] [PubMed]
- Zheng, W.; Sun, Y.; Li, H.; Zhao, H.; Zhan, Y.; Gao, Y.; Hu, Y.; Li, P.; Lin, Y.-F.; Chen, H.; et al. COVID-19 vaccine uptake and hesitancy among HIV-infected men who have sex with men in mainland China: A cross-sectional survey. Hum. Vaccines Immunother. 2021, 17, 4971–4981. [Google Scholar] [CrossRef] [PubMed]
- Ii, G.P.; Xu, J.; Ruprecht, M.M.; Costa, D.; Felt, D.; Wang, X.; Glenn, E.E.; Beach, L.B. Associations with COVID-19 Symptoms, Prevention Interest, and Testing Among Sexual and Gender Minority Adults in a Diverse National Sample. LGBT Health 2021, 8, 322–329. [Google Scholar] [CrossRef]
- Garg, I.; Hanif, H.; Javed, N.; Abbas, R.; Mirza, S.; Javaid, M.A.; Pal, S.; Shekhar, R.; Sheikh, A.B. COVID-19 Vaccine Hesitancy in the LGBTQ+ Population: A Systematic Review. Infect. Dis. Rep. 2021, 13, 872–887. [Google Scholar] [CrossRef]
- Swendeman, D.; Norwood, P.; Saleska, J.; Lewis, K.; Ramos, W.; SantaBarbara, N.; Sumstine, S.; Comulada, W.S.; Jimenez, S.; Ocasio, M.A.; et al. Vaccine Attitudes and COVID-19 Vaccine Intentions and Prevention Behaviors among Young People At-Risk for and Living with HIV in Los Angeles and New Orleans. Vaccines 2022, 10, 413. [Google Scholar] [CrossRef]
- D’Avanzo, P.A.; LoSchiavo, C.E.; Krause, K.D.; Karr, A.G.; Halkitis, P.N. Biological, Behavioral, and Demographic Drivers of Recent Syphilis Infection Among Emerging Adult Sexual Minority Men in New York City: The P18 Cohort Study. AIDS Patient Care STDs 2022, 36, 416–424. [Google Scholar] [CrossRef]
- Layland, E.K.; Carter, J.A.; Perry, N.S.; Cienfuegos-Szalay, J.; Nelson, K.M.; Bonner, C.P.; Rendina, H.J. A systematic review of stigma in sexual and gender minority health interventions. Transl. Behav. Med. 2020, 10, 1200–1210. [Google Scholar] [CrossRef]
- Steven Ross Johnson. Study: COVID Vaccination Rates Higher Among Gay, Lesbian Adults. Available online: https://www.usnews.com/news/health-news/articles/2022-02-03/gay-lesbian-adults-have-higher-covid-vaccination-rates (accessed on 15 December 2022).
- Movement Advancement Project. November 2020. The Disproportionate Impacts of COVID-19 on LGBTQ Households in the U.S. Available online: www.lgbtmap.org/2020-covid-lgbtq-households (accessed on 28 October 2022).
- Gil, R.M.; Freeman, T.L.; Mathew, T.; Kullar, R.; Fekete, T.; Ovalle, A.; Nguyen, D.; Kottkamp, A.; Poon, J.; Marcelin, J.R.; et al. Lesbian, Gay, Bisexual, Transgender, and Queer (LGBTQ+) Communities and the Coronavirus Disease 2019 Pandemic: A Call to Break the Cycle of Structural Barriers. J. Infect. Dis. 2021, 224, 1810–1820. [Google Scholar] [CrossRef]
- United Nations. The 2030 Agenda and the Sustainable Development Goals: An Opportunity for Latin America and the Caribbean; LC/G.2681-P/Rev.3; United Nations Publication: Santiago, Chile, 2018. [Google Scholar]
- Manandhar, M.; Hawkes, S.; Buse, K.; Nosrati, E.; Magar, V. Gender, health and the 2030 agenda for sustainable development. Bull. World Health Organ 2018, 96, 644–653. [Google Scholar] [CrossRef]
- McNaghten, A.; Brewer, N.T.; Hung, M.; Lu, P.J.; Daskalakis, D.; Abad, N.; Kriss, J.; Black, C.; Wilhelm, E.; Lee, J.T.; et al. COVID-19 Vaccination Coverage and Vaccine Confidence by Sexual Orientation and Gender Identity—United States, August 29–October 30, 2021. Morb. Mortal. Wkly. Rep. 2022, 71, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Singer, R.B.; Crooks, N.; Singer, R.; Green, N.; Stamps, J.; Patil, C.; Matthews, A. Ballroom Icons and the Power to Promote COVID-19 Vaccination Among Black and Brown LGBTQ+ Individuals. Am. J. Public Health 2022, 112, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Andrasik, M.P.; Maunakea, A.K.; Oseso, L.; Rodriguez-Diaz, C.E.; Wallace, S.; Walters, K.; Yukawa, M. Awakening. Infect. Dis. Clin. N. Am. 2022, 36, 295–308. [Google Scholar] [CrossRef] [PubMed]
- Parker, C.M.; Hirsch, J.S.; Philbin, M.M.; Parker, R.G. The Urgent Need for Research and Interventions to Address Family-Based Stigma and Discrimination Against Lesbian, Gay, Bisexual, Transgender, and Queer Youth. J. Adolesc. Health 2018, 63, 383–393. [Google Scholar] [CrossRef]
- Rainbow Health Australia. Available online: https://rainbowhealthaustralia.org.au/media/pages/research-resources/research-matters-covid-19-and-lgbtiq-communities/3033295656-1650953507/research-matters-covid-lgbtiq.pdf (accessed on 28 October 2022).
- Henriquez, N.R.; Ahmad, N. “The Message Is You Don’t Exist”: Exploring Lived Experiences of Rural Lesbian, Gay, Bisexual, Transgender, Queer/Questioning (LGBTQ) People Utilizing Health care Services. SAGE Open Nurs. 2021, 7, 23779608211051174. [Google Scholar] [CrossRef]
- Khubchandani, J.; Macias, Y. COVID-19 Vaccination Hesitancy in Hispanics and African-Americans: A Review and Recommendations for Practice. Brain Behav. Immun. Health 2021, 15, 100277. [Google Scholar] [CrossRef]
- Tomar, A.; Spadine, M.N.; Graves-Boswell, T.; Wigfall, L.T.; Center, U.A.C. COVID-19 among LGBTQ+ individuals living with HIV/AIDS: Psycho-social challenges and care options. AIMS Public Health 2021, 8, 303–308. [Google Scholar] [CrossRef]
- Bragazzi, N.L. The COVID-19 Pandemic Seen from a Syndemic Perspective: The LGBTQIA2SP+ Community. Infect. Dis. Rep. 2021, 13, 865–871. [Google Scholar] [CrossRef]
- Ruprecht, M.M.; Wang, X.; Johnson, A.K.; Xu, J.; Felt, D.; Ihenacho, S.; Stonehouse, P.; Curry, C.W.; DeBroux, C.; Costa, D.; et al. Evidence of Social and Structural COVID-19 Disparities by Sexual Orientation, Gender Identity, and Race/Ethnicity in an Urban Environment. J. Urban Health 2021, 98, 27–40. [Google Scholar] [CrossRef]
- Discrimination Prevents LGBTQ People from Accessing Health Care. Available online: https://www.americanprogress.org/article/discrimination-prevents-lgbtq-people-accessing-health-care/ (accessed on 28 October 2022).
- How Discrimination Impacts LGBTQ Healthcare. Available online: https://www.stkate.edu/academics/healthcare-degrees/lgbtq-health-discrimination (accessed on 28 October 2022).
- Whitehead, J.; Shaver, J.; Stephenson, R. Outness, Stigma, and Primary Health Care Utilization among Rural LGBT Populations. PLoS ONE 2016, 11, e0146139. [Google Scholar] [CrossRef]
- Poteat, T.; German, D.; Kerrigan, D. Managing uncertainty: A grounded theory of stigma in transgender health care encounters. Soc. Sci. Med. 2013, 84, 22–29. [Google Scholar] [CrossRef]
- Brenick, A.; Romano, K.; Kegler, C.; Eaton, L.A. Understanding the Influence of Stigma and Medical Mistrust on Engagement in Routine Healthcare Among Black Women Who Have Sex with Women. LGBT Health 2017, 4, 4–10. [Google Scholar] [CrossRef]
- Christensen, J. We Need Vaccines, and We Need Them Yesterday’: Frustration Builds in LGBTQ Community over Government Response to Monkeypox, CNN. Available online: https://www.cnnphilippines.com/world/2022/7/30/monkeypox-lgbtq-slow-response.html (accessed on 14 December 2022).
- Phillips, G.; Felt, D.; Ruprecht, M.M.; Wang, X.; Xu, J.; Pérez-Bill, E.; Bagnarol, R.M.; Roth, J.; Curry, C.W.; Beach, L.B. Addressing the Disproportionate Impacts of the COVID-19 Pandemic on Sexual and Gender Minority Populations in the United States: Actions Toward Equity. LGBT Health 2020, 7, 279–282. [Google Scholar] [CrossRef]
- Wu, Z.; Wang, X.; Zhang, S.; Ding, N.; Zhang, G.; Zhao, C.; Xu, H.; Lai, X.; Tu, X.; Yang, X. Do Attitudes, Mental Health Status, and Interpersonal Factors Predict COVID-19 Vaccine Hesitancy at the Early Phase of the Pandemic? A Longitudinal Study in Chinese College Students. Front. Psychol. 2022, 13, 876116. [Google Scholar] [CrossRef]
- COVID-19: Can Mental Health Experts Help Improve Vaccine Hesitancy? Available online: https://www.medicalnewstoday.com/articles/covid-19-can-mental-health-experts-help-improve-vaccine-hesitancy (accessed on 7 January 2023).
- LGBTQ+ Health Initiatives. Available online: https://www.phdmc.org/programs-a-to-z/lgbtq-health-initiatives (accessed on 7 January 2023).
- LGBTQ Community and Public Health. Available online: https://academicpartnerships.uta.edu/articles/public-health/lgbtq-community-public-health.aspx (accessed on 7 January 2023).
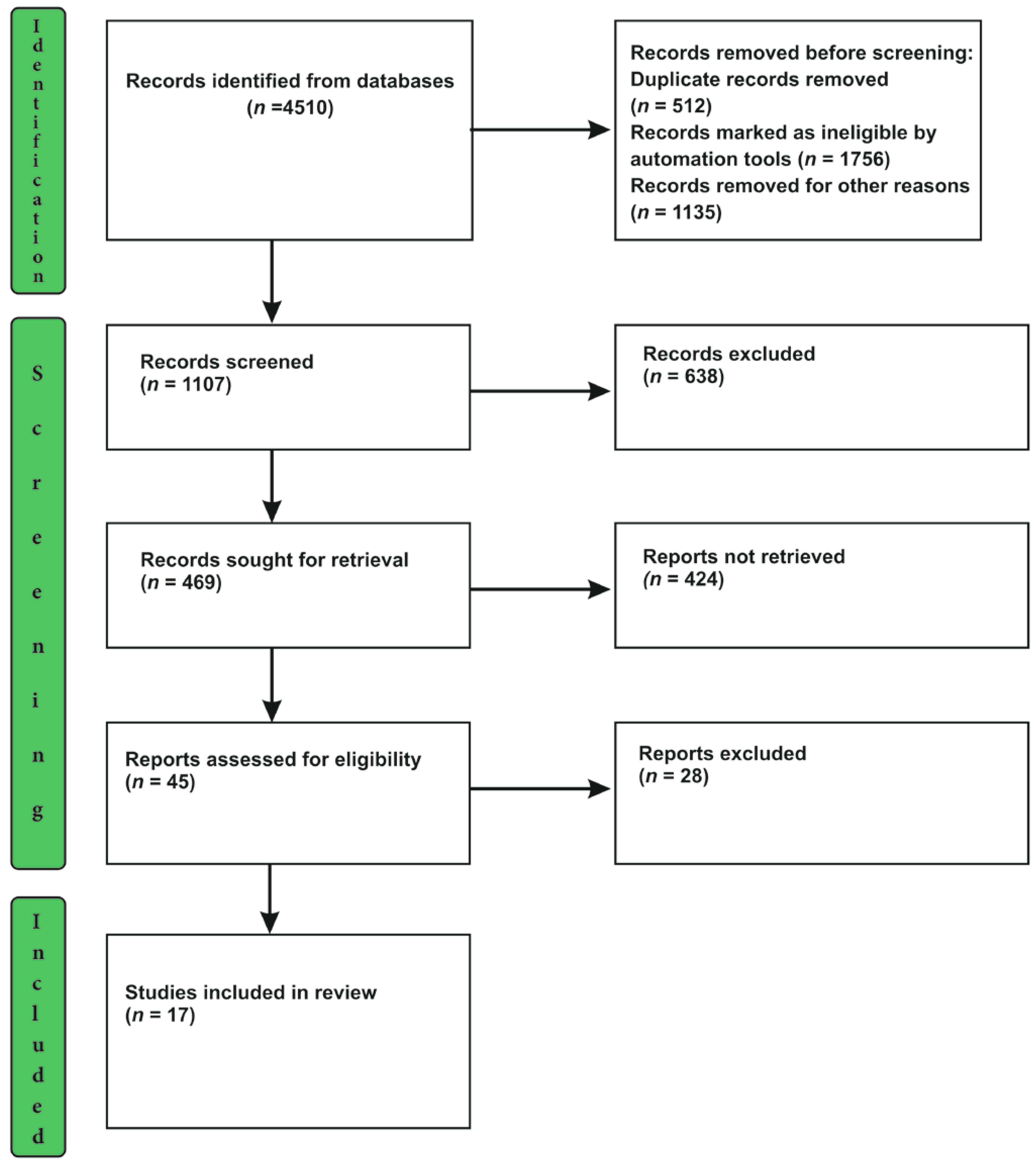


| Stage of Screening | Total No of Articles Reviewed | Articles Included | Excluded Articles | Rationale for Exclusion |
|---|---|---|---|---|
| Title Screening Stage | 1107 | 469 | 638 | Irrelevant to the objective of this study |
| Abstract Screening Stage | 469 | 45 | 424 | Did not qualify the eligibility criteria set up for this study (given in Section 2.4.1) |
| Full-Text Screening | 45 | 17 | 28 | Articles did not provide the required information for vaccine hesitancy among LGBTQIA+ and book\book chapters, comments, editorials, letters |
| Sl. No | Reference | Author | Country | Year | Aim | Study Design | Population (Sample Size) | HIV Status of Individuals Involved in the Study | Major Findings |
|---|---|---|---|---|---|---|---|---|---|
| 1 | [12] | Danny Azucar | USA | 2022 | To delineate the factors affecting vaccine uptake in the LGBTQIA+ population. | Qualitative study | 32 individuals from LGBTQIA+ communities | Not specified | Medical trauma, stigma, discrimination and violence are the major factors contributing to vaccine hesitancy |
| 2 | [13] | Andrea Low | USA | 2022 | To collate COVID-19 vaccine uptake among LGBTQIA+ communities to the general population | Cross-sectional study | Self-identified LGBTQIA+ individuals older than 18 years of age | Not specified | Education, socioeconomic status, medical mistrust, less integration, stigma and discrimination are the strongest determinants of vaccine hesitancy |
| 3 | [14] | Martin Holt | Australia | 2022 | To analyze the level of willingness to be vaccinated | Cross-sectional study | 1280 bisexual and gay individuals | HIV-positive or negative | Education, employment and socioeconomic status are established factors affecting vaccine acceptance. HIV-positive individuals show a higher rate of vaccine acceptance |
| 4 | [15] | Rob Stephenson | USA | 2021 | To determine the factors associated with beliefs about the COVID-19 vaccine | Cross-sectional study | Bisexual, gay and men who have sex with men above 18 years of age | HIV-positive or HIV negative | HIV-positive individuals have greater levels of vaccine optimism |
| 5 | [16] | Elliott R. Weinstein | USA | 2022 | To discover the factors related to vaccine likelihood and uptake | Mixed method study | Latino sexual minority men | Not specified | Altruistic motivations were influential in likelihood and vaccine uptake |
| 6 | [17] | Youssoufa M. Ousseine | France | 2022 | To explore the elements causing vaccine uncertainty and unwillingness | Cross-sectional study | Homosexuals, bisexuals, or men who have sex with men aged 18 years or older | HIV-positive or negative | Socioeconomically at-risk individuals are highly reluctant to be vaccinated |
| 7 | [18] | G. Prestage | Australia | 2022 | To recognize factors contributing towards COVID-19 vaccination and contrast sexual behavior pre- and post-vaccination | Prospective, cohort study | Men aged 16 years or above, identified as gay or bisexual or had sex with men | Not specified | Skepticism was a hurdle to vaccine uptake |
| 8 | [19] | Alex Abramovich | USA | 2022 | To enumerate the facilitators and barriers of vaccine uptake among the LGBTQIA+ population | Mixed method study | 922 LGBTQIA+ individuals experiencing homelessness | HIV-positive and negative | Mistrust in healthcare, paucity of targeted vaccine-related information, vaccine adverse effects and inequitable access are some of the attributes of vaccine refusal |
| 9 | [20] | Yen Ju Lin | Taiwan | 2021 | To differentiate the levels of explicit and intrinsic intentions to become vaccinated | Prospective cohort study | 1047 participants aged 20 years or older | Not specified | Sexual minority populations have greater levels of explicit and intrinsic intentions to accept COVID-19 vaccine uptake |
| 10 | [21] | Daniel Teixeira | USA | 2021 | To assess the vaccine acceptancy among sexual and gender minorities | Cross-sectional study | 1350 SGM participants | Not specified | Factors such as medical mistrust, altruism, race, and social concern affected the vaccine acceptancy among this population |
| 11 | [22] | Brooke A. Levandowski | USA | 2022 | To study the nonmedical impact of COVID-19 on LGBTQIA+ | Cross-sectional survey | 1362 LGBTQ+ participants | Not specified | Public health interventions should be made to countercoup the increased stress among LGBTQIA+ communities to avail them of all resources |
| 12 | [23] | Kechun Zhang | China | 2022 | To analyze the factors that are involved in the vaccine uptake among MSM in China | Prospective cohort study | 420 participants | Not specified | The COVID-19 vaccine uptake among this population was identified not to be poor when compared to the general population. Tapping the factors that increase vaccine acceptance will enhance the coverage |
| 13 | [24] | Weiran Zheng | China | 2021 | To assess the barriers to COVID-19 vaccine uptake among HIV-infected MSM in China | Cross-sectional survey | 1295 participants | HIV-positive | The vaccine acceptancy among the LGBTQIA+ population is still sub-standard. Addressing the barriers will improve hesitancy. |
| 14 | [25] | Gregory Philips | USA | 2021 | To analyze the impediments in achieving total COVID-19 vaccine coverage among sexual and gender minority groups | Cross-sectional survey | 932 participants | HIV-positive and HIV-negative | The factors that stand as challenges need to be addressed via public health measures to improve the standard of living of the SGM population |
| 15 | [26] | Ishan Garg | USA | 2021 | To determine the factors contributing to vaccine hesitancy among the LGBTQIA+ population | Systematic review | Not applicable | Not specified | The LGBTQIA+ community has undergone discrimination, oppression and health inequities which elevated the vaccine hesitancy among this population |
| 16 | [27] | Dallas Swendeman | USA | 2020 | To investigate the attitude of SGM youth towards COVID-19 vaccines | Cross-sectional study | 440 individuals | HIV positive | Treatment abuse, incarceration and homelessness contribute to vaccine hesitancy. SGM youth-targeted vaccine campaigns provide promising results in alleviating vaccine hesitancy |
| 17 | [28] | Jessica Jaiswal | USA | 2021 | To Determine the factors contributing to vaccine hesitancy among the SGM population living with HIV | Cross-sectional study | 496 HIV-positive individuals | HIV positive | Education, HIV status and higher perceived risk for COVID-19 vulnerability foster vaccine acceptance among the LGBTQIA+ population |
| Individual Factors | Interpersonal Factors | Social and Community Factors | Healthcare System-Related Factors | Vaccine Specific Factors |
|---|---|---|---|---|
|
|
|
|
|
| Level of Action | Elements | Purpose and Methods | Intended Outcomes |
|---|---|---|---|
| Healthcare Worker Level | Actively engaging Leader |
|
|
| Communication and Care |
|
| |
| Organizational Level | Non-discriminative policies forms |
|
|
| Welcoming Environment | Promoting LGBTQIA+ inclusivity in healthcare facilities, public places and virtual health centers by
|
| |
| Recruitment and retainment |
|
| |
| Community level | Partnership with LGBTQIA+ organizations |
|
|
| Process of Developing mHealth App | Explanation |
|---|---|
| Efficient mobile application development team |
|
| Effective designing of the mobile application |
|
| Testing of the prototype application |
|
| Components and features of the mobile application |
|
| Ethical Considerations |
|
| Intervention | Social and Cultural Barriers | Structural Barriers |
|---|---|---|
| Promoting Inclusivity |
|
|
| Digital health interventions |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balaji, J.N.; Prakash, S.; Joshi, A.; Surapaneni, K.M. A Scoping Review on COVID-19 Vaccine Hesitancy among the Lesbian, Gay, Bisexual, Transgender, Queer, Intersex and Asexual (LGBTQIA+) Community and Factors Fostering Its Refusal. Healthcare 2023, 11, 245. https://doi.org/10.3390/healthcare11020245
Balaji JN, Prakash S, Joshi A, Surapaneni KM. A Scoping Review on COVID-19 Vaccine Hesitancy among the Lesbian, Gay, Bisexual, Transgender, Queer, Intersex and Asexual (LGBTQIA+) Community and Factors Fostering Its Refusal. Healthcare. 2023; 11(2):245. https://doi.org/10.3390/healthcare11020245
Chicago/Turabian StyleBalaji, Jyotsna Needamangalam, Sreenidhi Prakash, Ashish Joshi, and Krishna Mohan Surapaneni. 2023. "A Scoping Review on COVID-19 Vaccine Hesitancy among the Lesbian, Gay, Bisexual, Transgender, Queer, Intersex and Asexual (LGBTQIA+) Community and Factors Fostering Its Refusal" Healthcare 11, no. 2: 245. https://doi.org/10.3390/healthcare11020245
APA StyleBalaji, J. N., Prakash, S., Joshi, A., & Surapaneni, K. M. (2023). A Scoping Review on COVID-19 Vaccine Hesitancy among the Lesbian, Gay, Bisexual, Transgender, Queer, Intersex and Asexual (LGBTQIA+) Community and Factors Fostering Its Refusal. Healthcare, 11(2), 245. https://doi.org/10.3390/healthcare11020245








