Abstract
Background: After a stroke, inpatients often receive less than the recommended dose of therapy. Telerehabilitation may assist by providing personalised rehabilitation programmes without face-to-face therapy time. This study aimed to evaluate the acceptability and feasibility of an individualised programme of upper-limb rehabilitation that is delivered via an online rehabilitation platform for inpatient stroke survivors. Methods: Stroke survivors were recruited from three stroke units in one NHS Board in Scotland and randomised to the intervention (personalised upper-limb exercise programme delivered via an online physiotherapy platform for four weeks, up to 30 min five times per week, in addition to usual care) or the control group (usual care). The main outcomes are related to recruitment, attrition, adherence and safety. The clinical measures were the Action Research Arm Test, Trunk Impairment Scale and Modified Ashworth Scale. The intervention participants, their carers and physiotherapists completed questionnaires on the acceptability of the intervention. Results: Twenty-six participants, 42% males, were recruited around three weeks post-stroke, on average. There were 13 participants in each group, with a mean age of 69 years (SD of 12) and 67 years (SD of 11) for the control and intervention groups, respectively. Overall, 47% of those screened for eligibility were randomised, and attrition was 23% in the intervention group mainly due to discharge before the end of the intervention. Participants who adhered to their programme (completed more than two-thirds), generally those with an engaged carer, demonstrated a trend toward improved clinical outcomes. Overall, the patients, carers and physiotherapists were positive regarding the intervention. There was a total of five reported adverse events, none of which were related to the study. Conclusion: An upper-limb unsupervised exercise intervention using an online physiotherapy platform for inpatient stroke survivors is feasible, safe and acceptable to patients, carers and physiotherapists. A fully powered RCT is warranted to investigate the clinical- and cost-effectiveness of such interventions for this patient group.
1. Introduction
Stroke incidence has been increasing, and in 2019, there were 12.2 million incident cases of stroke and over 101 million people living with stroke globally [1]. There are approximately 1.3 million stroke survivors in the United Kingdom (UK), with a stroke affecting 100,000 people per year in the UK [2]. Stroke care consumes around GBP 26 billion of the UK National Health Service (NHS)’s budget every year [3].
Stroke is one of the leading causes of disability worldwide [1]. Some people with stroke experience long-term motor deficiency, impaired functional activities and decreased participation in activities of daily living [4]. Upper-limb paresis affects 69%, and lower-limb paresis 61%, of stroke survivors in the acute stage [5], and about 50% of stroke survivors still have limited arm function six months post-stroke [6]. A stroke may lead to a loss of active movement and decreased sensation, dexterity and coordination in the affected arm, possibly preventing stroke survivors from undertaking normal everyday activities, such as eating, drinking, dressing and washing [7].
Rehabilitation features highly in the top priorities for stroke research, including improving upper-limb function [8]. Rehabilitation after stroke is based on the concept of neuroplasticity, where there is reorganisation (changes in function and structure) of the remaining cortical tissue in response to stimulation through activity [9]. Repetitive task-specific training optimises motor (re)learning and neuroplastic changes in the nervous system, improving patient outcomes [10,11]. High repetitions of task-specific movements that are functionally relevant and meaningful to stroke survivors are required in order to improve the functional recovery after stroke, as suggested by animal studies [12]. The first month after stroke is the peak time for nervous system neuroplasticity [13]; therefore, rehabilitation during this time is important for optimising functional recovery.
There is strong evidence that the dose of stroke rehabilitation is correlated with the degree of functional recovery [11,14,15,16,17]. Recently published national clinical guidelines for stroke in the UK recommend that post-stroke rehabilitation should involve a minimum of 3 h of multidisciplinary therapy, 5 days per week, with the intensity increasing based on the ability of the stroke survivor [18]. However, the dose of therapy received is often lower than these recommendations [19]. Barriers to achieving the recommendations include low staffing levels, increased time required for non-direct patient-related activity (e.g., daily handovers and documentation) and patient-related issues such as not being well enough to take part in therapy [20]. During the hospitalisation period, stroke survivors generally receive their therapy sessions throughout the working week; however, to increase the amount of rehabilitation, a few stroke units offer seven-day services [19]. There is also evidence that inpatient therapy sessions tend to focus on rehabilitation of the lower limbs, highlighting the need for stroke survivors to have extra upper-limb rehabilitation [21,22].
Augmenting the current rehabilitation provision and increasing the overall therapy time/dose for stroke survivors have been investigated in a number of studies; however, these studies often involve fully or partially supervised interventions [23,24,25,26,27,28], which do not address the issue of staffing levels and associated costs. Unsupervised, augmented upper-limb rehabilitation involving written sheets of exercises was found to be safe and feasible [29,30] and to improve functional recovery after stroke, with a high level of satisfaction [30,31]. The use of technology tools to augment the current rehabilitation provision is recommended by the recently updated UK National Clinical Guideline for Stroke [18,32].
There is increasing, although sometimes equivocal, evidence of the effectiveness of telerehabilitation in improving clinical outcomes, including upper-limb functions, after stroke [33,34,35,36]. Most studies focus on providing home-based telerehabilitation; however, telerehabilitation programmes could be a cost-effective approach if implemented in the inpatient setting to increase the therapy dose by encouraging patients to exercise without therapy times, particularly in the evenings and weekends, with the support of carers, if required.
The aim of this study was to evaluate the acceptability and feasibility of an individualised four-week programme of upper-limb rehabilitation, delivered via an online rehabilitation platform, for inpatient stroke survivors.
2. Materials and Methods
2.1. Ethical Considerations
Prior to the study, an existing online rehabilitation platform “www.giraffehealth.com accessed on 1 August 2020)” was adapted for use in a stroke population through co-production focus groups. The study was approved by the West of Scotland Research Ethics Committee (REC Ref 18/WS/0101), and Research and Development (R&D) approval was given by NHS Lanarkshire (R&D Ref L18047). The trial was registered on ClinicalTrials.gov (Ref. NCT03666702). Through the platform, the patient received a personalised video-based exercise programme, a stroke-specific advice page (including an aphasia version) and an exercise diary to complete if able. Participants were recruited from the three stroke units within NHS Lanarkshire, Scotland, UK. There were three groups of participants: stroke survivors, their carers and the physiotherapists. The study commenced on September 2018 and ended in August 2019. The study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guidelines [37].
The study aimed to recruit 30 stroke survivors—15 to the intervention group and 15 to the control group. This figure was felt to be feasible based on a 12-month recruitment period.
2.2. Inclusion/Exclusion Criteria
Stroke survivors were invited to take part if they were over 18 years old, had moderate-to-severe upper-limb functional limitation due to stroke (score 0–39 in the Action Research Arm Test (ARAT)) [38], were in the stroke unit with their first stroke, were able to sit in a chair or bed, could use a computer or tablet with or without help from carers, could understand English and we able to provide informed written consent. Stroke survivors were excluded if they had significant comorbidity, which would preclude them from taking part in an exercise programme; had moderate-to-severe cognitive impairment (<25 in the Mini Mental State Examination (MMSE) [39]; or they were participating in another interventional research study. Initially, anyone with a shoulder subluxation was excluded; however, it became apparent that almost all potential participants had some degree of shoulder subluxation, so a substantial amendment request was successfully made to the Ethics Committee (REC Ref AM01) to exclude only stroke survivors with shoulder subluxation greater than grade 3 (more than 1½ fingerbreadth gap) [40].
2.3. Data Collection
Stroke survivors were informed of the study by the physiotherapists in the stroke unit. They were given a participant information sheet (PIS) and were advised to contact the research team or physiotherapists if they would like to take part in the study. Aphasia-friendly versions of the consent form and PIS were available if required.
Participants who expressed an interest were assessed for eligibility before completing a consent form. Age, sex, time since stroke, ethnicity, level of education and stroke severity (National Institutes of Health Stroke Scale (NIHSS) [41]) were recorded. The NIHSS scale is scored from 0 to 42, with higher scores indicating higher stroke severity. In addition, social history and walking status before stroke, previous information technology (IT) use (computers/tablets/phones), medical history (stroke risk factors, comorbid conditions and previous transient ischemic attack (TIA)), stroke type and location (cortical, subcortical, midbrain or brainstem) were noted. Then, a baseline (initial) assessment was completed (see below).
Participants were then randomised. A set of sequential numbers (1–30) was generated by the researcher. Each number was placed in a separate envelope, and the envelopes were shuffled. Participants were randomised by choosing one of the envelopes: envelopes with odd numbers allocated participants to the intervention group, and even numbers allocated participants to the control group. The researcher (AA) was also the assessor and therefore was not blind to the group allocation.
Intervention: The intervention was developed and reported in accordance with the template for intervention description and replication (TIDieR) guidelines [42]. All stroke participants were given a leaflet from Chest Heart & Stroke Scotland about exercise and physical activity. The control group received usual physiotherapy care only. This was provided one-to one by physiotherapists and/or assistant physiotherapists for 4 or 5 sessions per week, with each lasting up to 45 min. The number, duration and content of all physiotherapy sessions were recorded by physiotherapists and occupational therapists for both groups, using forms developed for the study. Completed TIDieR checklist for the online physiotherapy programme has been uploaded it as Supporting Material.
Stroke survivors in the intervention group received a progressive, individualised four-week upper-limb physiotherapy intervention delivered via the Giraffe Healthcare online rehabilitation platform “www.giraffehealth.com (accessed on 1 August 2020)”, in addition to usual care. The individualised programme of upper-limb and trunk exercises was prescribed by the participant’s physiotherapist and was based on clinical assessment, their goals and their level of upper-limb function. The exercise dose (duration, frequency and intensity) was based on the participant’s level of functional ability, aiming to achieve 30 min of exercise, five sessions per week (including weekends), in addition to their usual physiotherapy care.
Participants in the intervention group received an explanation of their upper-limb programme and how to use the website. Physiotherapists reviewed their progress once a week and made any necessary changes to their programme. Participants were able to contact the research team during the study to ask any questions or to request a change in their programme. If participants had communication difficulties, where appropriate, an explanation of the participant’s upper-limb programme and how to access the website was provided to their carers, who then supported them to undertake their exercise programme. In addition, an aphasia-friendly version of the advice section on the website was available. Stroke survivors used their own tablets/laptop to access their programme; however, if they did not have an internet-enabled device, they were provided with a tablet and/or internet access for the duration of the study.
2.4. Outcome Measures
The main outcome measures related to the feasibility of the study are as follows:
- (1)
- Recruitment: number of stroke survivors who fulfilled the inclusion criteria and the number who agreed to take part.
- (2)
- Attrition: number of participants who dropped out.
- (3)
- Adherence: number of completed exercise diaries per week over the intervention period (maximum of 20 sessions, 5 sessions a week for 4 weeks) expressed as a percentage. Participants completing at least two-thirds of their prescribed sessions (13 sessions) were considered adherent [43].
- (4)
- Safety: number of related adverse and serious adverse events.
Clinical assessments were carried out by a researcher (AA) who was not blinded to the group allocation. The following assessments were undertaken in both groups of stroke survivors at baseline (week 0) and post-intervention (week 5). The Action Research Arm Test (ARAT) is a valid and reliable tool for stroke survivors and measures arm function in 19 items grouped into the following subscales: grasp (6 items), pinch (6 items), grip (4 items) and gross motor (3 items) [44,45]. Scores range from 0 to 57 (maximum) [38]. The Minimal Clinically Important Difference (MCID) for the ARAT in stroke survivors is an increase of 5.7 points [38]. The Trunk Impairment Scale (TIS) consists of 17 items for assessing the level of motor impairment of the trunk [46]. The scores range from 0 to 23, with lower scores indicating high levels of trunk impairment. The TIS is a valid and reliable scale for stroke [47]. The Modified Ashworth Scale (MAS) is also valid and reliable in the stroke population [48]. The scores range from 0 to 4, with higher scores indicating higher muscle tone. The spasticity of the shoulder adductor, elbow flexor, wrist flexor and finger flexor muscle groups was examined using the guidelines of [49]. The MAS is most reliable for assessing the elbow and wrist; therefore, it was appropriate for assessing upper-limb spasticity in this study [50,51]. In addition, the views of the stroke survivors in the intervention group and their carer (if relevant), as well as the physiotherapists, were sought using three versions of a developed questionnaire. All questionnaires were administered by the researcher (AA), face-to-face, to all participants. The questionnaires were piloted in two stages to make sure that important topics were covered fully, questions and instructions were clear and none of the questions had been objected to. The questionnaire for stroke survivors included sections on the exercise programme, any help need to complete the programme, the frequency with which it was completed and views on the Giraffe platform. Generally, closed questions were used, but free-text space was included, so participants could expand their responses. Stroke survivors’ questionnaire has been uploaded as Supporting Material.
Carers: It was not mandatory that all stroke participants allocated to the intervention group had a carer who agreed to participate. Carers were defined as the person most likely to help the participant complete his/her exercise programme. The physiotherapists in the stroke unit informed the carers about the study. Once the stroke survivor was allocated to the intervention group, the carer was provided with a PIS. Carers were eligible to take part if they were over 18 years, able to communicate in English and able to support the stroke survivor with his/her online exercise programme. Following consent, demographic information was recorded: age, gender, relationship to stroke survivor, occupation, ethnicity, level of education, previous use of IT and general health status. The carer’s questionnaire covered similar areas to the stroke survivors but with questions related to the support they gave during the intervention period. Physiotherapist’s questionnaire has been uploaded as Supporting Material.
Physiotherapists: To be included, physiotherapists had to have delivered the intervention to at least two stroke survivors. Following consent, demographic information was recorded: age, gender, physiotherapist or assistant physiotherapist, level of education, previous use of IT and time working in stroke rehabilitation. The physiotherapist’s questionnaire gathered views on the exercise programme, the Giraffe platform and any challenges experienced. Physiotherapist’s questionnaire has been uploaded as Supporting Material.
2.5. Analysis
Quantitative data were analysed using the Statistical Package for the Social Sciences (SPSS) version 25. Data are presented as means with standard deviations (SDs), or medians with ranges (where appropriate) for continuous variables and numbers with percentages for ordinal and categorical variables.
For the clinical outcome measures (ARAT, TIS and MAS), medians with range baseline assessments and post-intervention assessments were calculated for each group.
For the feedback questionnaires, the frequencies and percentages were calculated to summarise the findings of ordinal and categorical variables and quotes from the free text sections used to expand upon the responses.
3. Results
3.1. Baseline Demographic and Stroke Characteristics
Twenty-six participants were recruited to the study—thirteen in each group (Table 1). The cohort comprised 11 males (42.3%) and 15 females (57.7%) and was allocated evenly to both groups. The mean age was 69 years (standard deviation (SD) of 12) and 67 years (SD of 11) for the control and intervention groups, respectively. Participants were recruited three weeks after stroke, on average. Twelve participants (46.1%) previously used computers daily, and one participant (3.8%) used computers only with the assistance of a relative.

Table 1.
Baseline participants’ characteristics.
Most participants (88.4%) were able to walk independently before their stroke, and only one participant from each group (7.7%) was able to walk independently after the stroke. The NIHSS scores were slightly higher for the control group than the intervention group (Table 1).
All had their strokes confirmed by imaging (most commonly CT scan), and five participants from each group received thrombolysis/reperfusion therapy. More information about stroke characteristics is provided in Table 2.

Table 2.
Stroke characteristics.
3.2. Outcome Measures
Feasibility Outcomes: Overall, 26 participants were recruited, 4 short of the target of 30 participants. Over the 12-month period of recruitment, 55 participants were assessed for eligibility, of which 29 did not fulfil the criteria, most commonly due to shoulder subluxation, and another 11 participants were generally too unwell to take part. Twenty-six participants were recruited equally into the intervention and control group. Both groups received the planned intervention (Figure 1). Around 5–6 participants were screened per month, and 47% of those were randomised. Ten people from the intervention group and eleven people from the control completed a post-intervention assessment. Thus, attrition was 23% in the intervention and 15% in the control group.
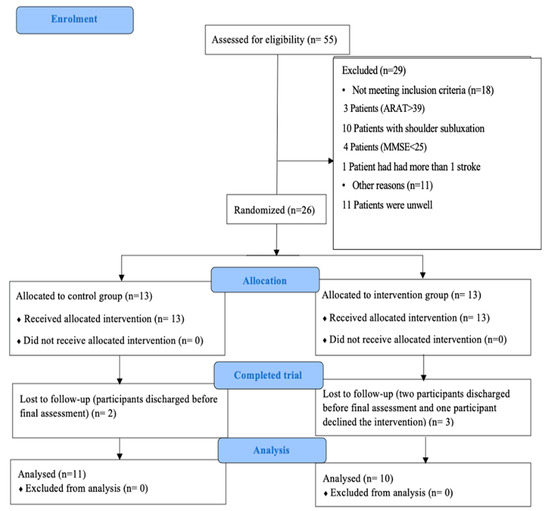
Figure 1.
CONSORT flow diagram for recruitment of the participants.
Of the ten participants who completed the intervention period, seven (70%) logged into the online rehabilitation platform and completed at least one complete exercise session. Of the remaining three participants, two did not log into the platform at all, and one participant logged into the platform and performed some exercises but did not complete a full exercise session.
Out of the seven participants who undertook some exercise, five participants were adherent, as they performed more than two-thirds of their prescribed intervention (Table 3). Overall, participants in the intervention group completed 3.7 exercise sessions per week, while those who were considered adherent completed 5.3 sessions per week, on average.

Table 3.
Usage of the online physiotherapy platform and adherence to the physiotherapy programme.
The number of prescribed exercises for the nonadherent participants was 3–5 exercises per session, and for the adherent participants, 3–10 exercises per session. Furthermore, there were no specific days of the week (weekdays or weekends) that the participants chose to undertake their prescribed exercises.
Participant safety: There were five recorded adverse events, namely shoulder pain (n = 2), fatigue (n = 1) and fall (n = 2), none of which were deemed to be related to the study intervention.
Clinical outcome measures: For the clinical measures, in the intervention group, the median ARAT was 0 (0–36) at baseline, with seven participants scoring 0. This increased to 11 (0–57) post-intervention, with 2 participants scoring 0. In the control group, the median ARAT at baseline was 0 (0–21), with eight scoring 0, and this increased to 11 (0–44) post-intervention, with four participants scoring 0. The ARAT scores for 6 out of those 15 participants who had a score of 0 did not change (two intervention group and four control group), while all of those with an ARAT of 1 or more improved over the intervention period, whether in the control or intervention group. In the intervention group, 8 out of 10 participants improved by more than the MCID (5.7 points) in the ARAT, while in the control group, 6 out of 11 participants showed clinically significant improvements.
There was an overall trend for both intervention and control groups toward an increase in TIS. In the intervention group, the median TIS was 16 (4–21) at baseline and increased to 17 (10–23) post-intervention. In the control group, the median TIS at baseline was 13 (0–19), increasing to 17 (7–21) post-intervention period. The median difference between the two groups in TIS score was similar.
An assessment of muscle spasticity (MAS) was performed for the shoulder adductor, elbow flexor, wrist flexor and finger flexor muscle groups. There were no notable trends for either the intervention or control group in any of the assessed muscle groups (Table 4).

Table 4.
Clinical outcomes at baseline and post-intervention.
Stroke survivor’s questionnaire: All the participants who completed the intervention responded to the questionnaire (n = 10). Three did not do any of their exercise programmes; therefore, they did not provide feedback on the study intervention. The main reason why participants did not undertake any exercise was “no [internet] signal at the ward” (Stroke Survivors 27 and 3). Four participants reported doing their exercises from memory, without accessing their exercise programmes; therefore, the exercise diary provided an underestimation of completed exercise sessions for those participants.
In general, the participants found the exercise programme easy to understand and beneficial and did not believe that it increased their level of fatigue, with most indicating that they would be happy to use the platform again in the future. Overall, the participants expressed positive views about using the platform to do their exercise, and the majority had no difficulties learning how to use it (Table 5).

Table 5.
Participants’ feedback on the intervention and the online platform.
Three participants reported using the online platform 3–5 times per week, one participant reported 7 times per week, and three participants reported 14 times per week. The majority of participants (71.4%, n = 5) reported spending less than 30 min per session, and 28.6% (n = 2) spent up to an hour per session. Six participants reported requesting help from carers to do their exercise programme. None of the participants asked staff for help. Four stroke survivors explained that they needed help from their partner/relative to provide motivation—“Encourage me to do my exercise” (Stroke Survivor 17)—and physically supporting the weaker part of the body: “Help me with my weak hand and the shoulder” (Stroke Survivor 5).
Five participants indicated that practising the exercises was easy for them because the website was clear and easy to use.
“It was self-explanatory, you just watch and listen, it was simple” (Stroke Survivor 10).
Carer’s questionnaire: Five carers were recruited, two males and three females, with a mean age of 36.8 (SD 11) years. Two of the stroke survivors had two carers helping them with the exercises and who responded to the questionnaires separately. Three had a college degree, one had a postgraduate degree and the other had other qualifications. All indicated that they use computers daily, and their professional careers varied from information technology officer to housewife.
All strongly agreed that it was easy to help their partner/relative to do the exercises, that the exercises were clear and understandable and that they would be happy to use the online platform to help their partner/relative in their future rehabilitation exercises. All strongly agreed that learning to use the platform was easy. Three participants (60%) indicated that they helped their partner/family member 7 times per week, and two participants (40%) indicated 3–5 times per week. They stated that they helped the stroke survivor to access and perform the exercise programmes. Similar to stroke-survivor participants, none of the carers asked the staff for help.
Physiotherapist’s questionnaire: Five physiotherapists, one male and four females, with a mean age of 35.4 (SD 7.7) years, were recruited. All identified as computer literate and had worked in stroke rehabilitation for a mean of 4.4 (SD 3.6) years. Four monitored stroke survivors’ exercise programmes once per week, and one monitored the programmes twice per week.
Overall, the responses were positive. The majority of physiotherapists found the exercises to be clear and well explained, and they expressed that they would be happy to use the website again. The participants showed some concerns about the effect of monitoring the online intervention on their workload (Table 6).

Table 6.
Physiotherapists’ responses to the questionnaire.
The physiotherapists provided details about the advantages/disadvantages of the online exercise programme, with advantages such as involving the patients in their rehabilitation.
“Helps patients to feel involved and control of their rehabilitation and influence in their mental health” (Physiotherapist 2).
They also felt that the platform provided opportunity for carers to support stroke survivors in their rehabilitation journeys and to encourage additional exercise out with usual care to help promote recovery:
“Good idea to have such a website for families to assist with the exercise” (Physiotherapist 9).
“Patients use their spare time to do more exercise beneficially for recovery” (Physiotherapist 2).
Finally, the simplicity of the website made things easier for stroke survivors and physiotherapists:
“Exercise very well described and useful to have videos of the specific exercise” (Physiotherapist 9).
In terms of disadvantages, the physiotherapists highlighted the limited choice of upper-limb exercises on the platform. However, some of the main challenges were technological, relating to poor internet connection in the hospitals and the fact that the website worked on the Chrome browser but the NHS default at the time was Internet Explorer. One physiotherapist highlighted that patients often did the exercise from memory without logging into the website.
“Not all patients managed to use tablet themselves” some patients remembered to exercise and then did not log in to do them each time” (Physiotherapist 7).
Finally, there was a recognition that online exercise might not be suitable for all stroke survivors, including older adults.
“Limited for patients with cognitive impairment” (Physiotherapist 2).
“Not suitable for all elderly people” (Physiotherapist 6).
“Many patients found it difficult to use and felt too tired to do as additional therapy work alongside daytime therapy” (Physiotherapist 9).
4. Discussion
Overall, this study demonstrated that an unsupervised upper-limb rehabilitation programme delivered via an online platform “www.giraffehealth.com (accessed on 1 August 2020)” was feasible and acceptable to stroke survivors, their carers and their physiotherapists at the inpatient stage of their rehabilitation, although a few issues need to be considered for a future fully powered randomised controlled trial.
Over the 12-month period of the study, 5–6 patients were screened per month in this single-centred study, 47% of which were randomised. Therefore, subsequent studies should aim to screen at least double the number of participants needed for the study to ensure recruitment figures are achieved, assuming similar recruitment figures in different clinical sites.
One of the main reasons for not being recruited was shoulder subluxation (n = 11), as per the initial inclusion/exclusion criteria (n = 10). Amending the inclusion criteria to only exclude participants with shoulder subluxation greater than grade 3 [40] significantly improved recruitment and did not lead to adverse events; therefore, the amended exclusion should be used in any future study.
Including participants with severely limited arm functions (ARAT = 0) resulted in the delivery of passive exercises rather than functional-task-specific/oriented exercises; however, half of participants with an ARAT score of 0 (7 out of 13) improved their score after the intervention, indicating the potential for recovery in patients even with severely limited arm function. The presence of voluntary movement in shoulder abduction and finger extension within three days of stroke can be a predictor for full recovery of upper-limb function for up to 60% of stroke survivors [52]. Future studies might consider stratifying participants based on their ARAT score at randomisation to better understand the potential effect of the study intervention on stroke survivors with different levels of upper-limb impairment.
The overall level of participant attrition was 19% (23% in the intervention group and 15% in the control group). The main reason for attrition was the patient being discharged from the stroke unit before the end of the study period. Participants were randomised on average three weeks from their stroke; thus, future studies may aim to reduce this period if the participant is medically stable, especially given the increase in early supported discharge (ESD) from stroke units. However, based on these figures, a sample size calculation for a future fully powered randomized controlled trial (RCT) should allow for at least 19% attrition.
There were five reported adverse events during the study period. Although adverse events are expected in an acute–subacute stroke population, none of the recorded adverse events were deemed directly related to the study; therefore, it can be concluded that the intervention showed no signal for harm in the current study.
Adherence to telehealth interventions to improve physical function has been poorly reported in previous studies [33]. In terms of adherence, seven out of ten participants (70%) who completed the intervention period logged into their exercise programme and completed at least one exercise session; five were adherent, as they completed at least two-thirds of their prescribed sessions (mean of 5.3 sessions/week). This figure is comparable with a previous study of unsupervised upper-limb exercise programmes for hospitalised stroke patients using printed sheets of exercises, where participants were asked to complete the augmented intervention 1 h a day, 6 days a week, for 4 weeks and completed, on average, 3 h per week and 4.8 days per week [30]. The evaluation questionnaires in the present study, however, highlighted that four participants completed their exercise programme without logging; thus, the adherence figures in the present study may be an under-estimate. Participants using the platform in future studies should be reminded to record their exercises to provide more accurate data on adherence to the intervention.
Three participants in the present study did not complete any exercise sessions, which is similar to another study of online exercise in the management of type 2 diabetes, which found that 28% of participants never logged into the website [53]. The present study is the first study to use an online exercise platform during the inpatient stage of stroke rehabilitation; thus, the context is different from previous studies in stroke or other conditions but demonstrates that additional measures may be required to support some participants to engage with online interventions.
The main reason for participants not using the online exercise platform was poor Wi-Fi signal in the ward. Future studies should ensure that there is stable internet connection at the study site(s), but this also highlights the lack of infrastructure in some inpatient NHS facilities.
Many stroke-survivor participants sought help from their carers to access the website and/or perform their exercises, and most of the participants who were adherent to the augmented programme had a carer to assist them. Thus, patients who have carer support may be the ones who are most likely to benefit from this programme. The Early Versus Later Augmented Arm Physiotherapy (EVERLAP) trial, which involved up to 27 additional hours of upper-limb exercise (both supervised and unsupervised) over six weeks at time points up to nine weeks after stroke [54], also reported that the presence of carers to support stroke survivors facilitated their engagement with the unsupervised sessions [54].
There was also a trend toward better adherence in those with a greater number of exercises in their programmes, but the optimum number of exercises to improve adherence requires further investigation. Importantly, however, the intervention was not found to be a burden for participants in addition to their usual care/therapy, with the exception of one therapist who reported that as an issue.
In terms of the clinical outcomes assessments, both groups improved, thus demonstrating recovery with usual care post-stroke. The overall changes in the ARAT scores in this feasibility study were in favour of participants in the intervention group, as more participants in this group had improvement exceeding the MCID (5.7 points in scores). Although this provides some indication of the likely effect of the augmented intervention on upper-limb function, this study was not fully powered to detect differences between groups. The overall completeness of ARAT scores in this study was good, with missing scores only from those discharged before the final assessment. This would suggest that the ARAT is a viable primary outcome measure for any further study on the efficacy of upper-limb interventions for hospitalised stroke survivors.
In terms of spasticity, there was no indication of an increase in muscle tone in either group, as demonstrated by an increase in MAS. Previous studies of fully supervised augmented upper-limb exercises in inpatient stroke survivors similarly did not find any statistically significant changes across groups [45,55,56]. Given the time taken to complete the MAS and the low levels of spasticity in this stroke population, it may not be appropriate to include the MAS in a future study.
The TIS was assessed in this study because having a good trunk function is essential to be able to control upper-limb function [57]. A previous study also found telerehabilitation to be a feasible modality to deliver unsupervised augmented trunk exercises for stroke survivors in the chronic stage [58]. Given that trunk exercises can positively affect functional abilities and that this effect is at its peak in the acute stage after stroke [59], the TIS would seem an appropriate outcome to be included in any subsequent study.
There were only three clinical outcomes in this feasibility study; other domains may be relevant. Future studies should consider employing the recommended outcome measures for post-stroke arm-rehabilitation trials [60].
The ease of use of the technology, attractive user interface and personalisation of the programme are factors reported to improve adherence and user satisfaction with telerehabilitation for upper-limb disability, including stroke [61]. The results from the questionnaires demonstrated that stroke survivors, carers and physiotherapists thought that the exercise programme delivered through the online physiotherapy platform was clear, easy to use and helpful and that they would be keen to use it again in the future. The stroke survivors were happy with the exercise programme, and although one physiotherapist suggested that the programme increased patient fatigue, the stroke survivors did not report an increase in fatigue.
The physiotherapists who participated in the study stated that the process of setting up new patient exercise programmes on the website was easy and was not considered an imposition on their daily workload. However, the platform was not compatible with the browser used by the clinical site at the time, thus causing some issues, together with a perceived limited number of upper-limb exercises on the platform. The NHS now uses the Chrome browser more widely, and there has been a significant increase in the number of upper-limb exercises on the Giraffe platform so that these issues will not affect future studies.
Another study has investigated telerehabilitation in acute stroke. In the CARE4STROKE trial, carers supported stroke survivors with personalised exercises through an app, aiming for an additional 150 min of exercise per week for 12 weeks. There was no difference in length of hospital stay or mobility; however, there was a reduction in patient anxiety and caregiver depression [62]. It transpired that both groups undertook a similar number of minutes of exercise, and this may explain the similarity in clinical outcomes between groups. As with our trial, this study used technology to deliver augmented rehabilitation and recruited stroke survivors during their hospital period. However, while this study used CARE4STROKE application, our trial used the Giraffe platform to deliver augmented intervention. In addition, while the augmented intervention in this other study aimed to increase the intensity of practice and facilitate ESD, our trial aimed to improve upper-limb function.
The results of this study suggest that telerehabilitation, using an online exercise platform, has the potential to significantly increase the overall dose of therapy for inpatient stroke survivors, without adding significantly to the workload of the therapist. This may address the reported subtherapeutic dose of therapy often reported after a stroke [18,19,63] and, although further research is required may, in turn, improve clinical outcomes. This approach, however, may not be suitable for every stroke survivor, e.g., those with low health literacy or IT skills. We developed aphasia-friendly versions of the PIS, consent form and advice page to support the inclusion of people with aphasia; however, those resources were used by only one participant.
This study, however, had some limitations. The assessor and the participants were not blind to group allocation, which may introduce bias. Although blinding clinical physiotherapists and participants to group allocation is difficult, any future study should ensure that the assessor is blind to the group allocation. In terms of the dose of the augmented intervention, the sets and repetitions of exercises to complete can be extracted from the Giraffe platform, but not the time taken. In addition, participants often completed exercise sessions but did not log these on the platform. Future studies should more accurately calculate the exercise dose to evaluate the dose effect and ensure that all exercise sessions are logged. The content of usual care was not recorded for either group. Therapists were asked to complete a form of upper-limb exercises included in “usual care” sessions, as well as the duration of these exercises. However, the majority of these forms were not completed, and alternative methods to record the content of therapy sessions is required for any future RCT. Any changes in medications, such as anti-spasticity drugs, were not recorded, but this would be required in a future study.
5. Conclusions
Delivering an unsupervised augmented upper-limb exercise intervention using an online physiotherapy platform for inpatient stroke survivors is feasible, safe and acceptable to patients, carers and physiotherapists. There were a number of factors, such as Wi-Fi access, which adversely affected adherence to the intervention, but adherence was facilitated if a carer supported the participant with his/her exercise. A fully powered RCT is warranted to investigate if this approach could address the subtherapeutic dose of therapy often reported after stroke, as well as the clinical and cost-effectiveness of the intervention for inpatient stroke survivors. However, further consideration of both the dose of therapy and the outcome measures used is required.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare11182582/s1, Completed TIDieR checklist for the online physiotherapy programme, physiotherapist’s questionnaire, Stroke survivors’ questionnaire and Carers’ questionnaire.
Author Contributions
Conceptualization, A.I.A., E.S.C., E.C., M.B. and L.P.; methodology, A.I.A., E.S.C. and L.P.; formal analysis, A.I.A., E.C. and E.S.C.; investigation, A.I.A. and E.S.C.; resources, A.I.A., L.P. and M.B.; data curation, A.I.A.; writing—original draft preparation, A.I.A.; writing—review and editing, A.I.A., E.S.C., M.B. and L.P.; visualization, A.I.A., E.S.C. and L.P.; supervision, E.S.C. and L.P.; project administration, A.I.A., E.S.C. and L.P.; funding acquisition, A.I.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of the West of Scotland Research Ethics Committee (REC Ref. 18/WS/0101) and Research and Development approval was given by NHS Lanarkshire (R&D Ref. L18047).
Informed Consent Statement
Participants (stroke survivors, carers and physiotherapists) who expressed an interest gave written informed consent before taking part in the study.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Acknowledgments
Our sincere thanks to all the participants in the study for their time. We would also like to thank the staff of three stroke units within NHS Lanarkshire, University Hospital Hairmyres, University Hospital Wishaw and University Hospital Monklands for their various roles in facilitating the recruitment of participants for this study. The author would like to thank the Deanship of Scientific Research at Shaqra University for supporting this work.
Conflicts of Interest
The augmented intervention investigated in this study was delivered via the Giraffe Health website “www.giraffehealth.com (accessed on 1 August 2018)”, which was created by Lorna Paul and Elaine Coulter and is now a not-for-profit company. This may have potentially led to a bias in the study’s findings. However, Lorna Paul and Elaine Coulter were not directly involved in any data collection, and the other authors had no conflict of interests.
References
- Feigin, V.L.; Stark, B.A.; Johnson, C.O.; Roth, G.A.; Bisignano, C.; Abady, G.G.; Abbasifard, M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abedi, V.; et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef] [PubMed]
- Stroke Association. Available online: https://www.stroke.org.uk/what-is-stroke/stroke-statistics (accessed on 31 January 2023).
- Patel, A.; Berdunov, V.; Quayyum, Z.; King, D.; Knapp, M.; Wittenberg, R. Estimated societal costs of stroke in the UK based on a discrete event simulation. Age Ageing 2020, 49, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Langhorne, P.; Coupar, F.; Pollock, A. Motor recovery after stroke: A systematic review. Lancet Neurol. 2009, 8, 741–754. [Google Scholar] [CrossRef] [PubMed]
- Yew, K.S.; Cheng, E.M. Diagnosis of acute stroke. Am. Fam. Physician 2015, 91, 528–536. [Google Scholar]
- Kwah, L.K.; Harvey, L.A.; Diong, J.; Herbert, R.D. Models containing age and NIHSS predict recovery of ambulation and upper limb function six months after stroke: An observational study. J. Physiother. 2013, 59, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Geyh, S.; Cieza, A.; Schouten, J.; Dickson, H.; Frommelt, P.; Omar, Z.; Stucki, G. ICF core sets for stroke. J. Rehabil. Med. 2004, 36, 135–141. [Google Scholar] [CrossRef]
- Hill, G.; Regan, S.; Francis, R.; Stroke Priority Setting Partnership Steering Group. Research priorities to improve stroke outcomes. Lancet Neurol. 2022, 21, 312–313. [Google Scholar] [CrossRef]
- Nudo, R.J. Plasticity. NeuroRx 2006, 3, 420–427. [Google Scholar] [CrossRef]
- French, B.; Thomas, L.H.; Coupe, J.; McMahon, N.E.; Connell, L.; Harrison, J.; Watkins, C.L. Repetitive task training for improving functional ability after stroke. Cochrane Database Syst. Rev. 2016, 11, CD006073. [Google Scholar] [CrossRef]
- Veerbeek, J.M.; van Wegen, E.; van Peppen, R.; van der Wees, P.J.; Hendriks, E.; Rietberg, M.; Kwakkel, G. What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PLoS ONE 2014, 9, e87987. [Google Scholar] [CrossRef]
- Birkenmeier, R.L.; Prager, E.M.; Lang, C.E. Translating animal doses of task-specific training to people with chronic stroke in 1-hour therapy sessions: A proof-of-concept study. Neurorehabilit. Neural Repair 2010, 24, 620–635. [Google Scholar] [CrossRef] [PubMed]
- Krakauer, J.W.; Carmichael, S.T.; Corbett, D.; Wittenberg, G.F. Getting Neurorehabilitation Right: What Can Be Learned From Animal Models? Neurorehabilit. Neural Repair 2012, 26, 923–931. [Google Scholar] [CrossRef] [PubMed]
- Ballester, B.R.; Ward, N.S.; Brander, F.; Maier, M.; Kelly, K.; Verschure, P.F.M.J. Relationship between intensity and recovery in post-stroke rehabilitation: A retrospective analysis. J. Neurol. Neurosurg. Psychiatry 2022, 93, 226–228. [Google Scholar] [CrossRef]
- Pollock, A.; Farmer, S.E.; Brady, M.C.; Langhorne, P.; Mead, G.E.; Mehrholz, J.; van Wijck, F. Interventions for improving upper limb function after stroke. Cochrane Database Syst. Rev. 2014, CD010820. [Google Scholar] [CrossRef]
- Schneider, E.J.; Lannin, N.A.; Ada, L.; Schmidt, J. Increasing the amount of usual rehabilitation improves activity after stroke: A systematic review. J. Physiother. 2016, 62, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Ward, N.S.; Brander, F.; Kelly, K. Intensive upper limb neurorehabilitation in chronic stroke: Outcomes from the Queen Square programme. J. Neurol. Neurosurg. Psychiatry 2019, 90, 498–506. [Google Scholar] [CrossRef]
- Intercollegiate Stroke Working Party. National Clinical Guideline for Stroke for the UK and Ireland. London: Intercollegiate Stroke Working Party. 2023. Available online: www.strokeguideline.org (accessed on 20 May 2023).
- Sentinel Stroke National Audit Programme (SSNAP). Sentinel Stroke National Audit Programme: Clinical Audit April 2013–March 2018. Royal College of Physicians, London. 2019. Available online: https://strokeaudit.org/ (accessed on 20 June 2020).
- Clarke, D.J.; Burton, L.J.; Tyson, S.F.; Rodgers, H.; Drummond, A.; Palmer, R.; Forster, A. Why do stroke survivors not receive recommended amounts of active therapy? Findings from the ReAcT study, a mixed-methods case-study evaluation in eight stroke units. Clin. Rehabil. 2018, 32, 1119–1132. [Google Scholar] [CrossRef]
- Serrada, I.; McDonnell, M.N.; Hillier, S.L. What is current practice for upper limb rehabilitation in the acute hospital setting following stroke? A systematic review. Neurorehabilitation 2016, 39, 431–438. [Google Scholar] [CrossRef]
- Stockley, R.; Peel, R.; Jarvis, K.; Connell, L. Current therapy for the upper limb after stroke: A cross-sectional survey of UK therapists. BMJ Open 2019, 9, e030262. [Google Scholar] [CrossRef]
- English, C.; Bernhardt, J.; Crotty, M.; Esterman, A.; Segal, L.; Hillier, S. Circuit class therapy or seven-day week therapy for increasing rehabilitation intensity of therapy after stroke (CIRCIT): A randomized controlled trial. Int. J. Stroke 2015, 10, 594–602. [Google Scholar] [CrossRef]
- Horsley, S.; Lannin, N.A.; Hayward, K.S.; Herbert, R.D. Additional early active repetitive motor training did not prevent contracture in adults receiving task-specific upper limb training after stroke: A randomised trial. J. Physiother. 2019, 65, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Kong, K.H.; Loh, Y.J.; Thia, E.; Chai, A.; Ng, C.Y.; Soh, Y.M.; Tjan, S.Y. Efficacy of a Virtual Reality Commercial Gaming Device in Upper Limb Recovery after Stroke: A Randomized, Controlled Study. Top. Stroke Rehabil. 2016, 23, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Kwakkel, G.; Winters, C.; van Wegen, E.E.; Nijland, R.H.; van Kuijk, A.A.; Visser-Meily, A.; Consortium, E. XPLICIT-Stroke. Effects of Unilateral Upper Limb Training in Two Distinct Prognostic Groups Early After Stroke: The EXPLICIT-Stroke Randomized Clinical Trial. Neurorehabilt. Neural Repair 2016, 30, 804–816. [Google Scholar] [CrossRef] [PubMed]
- Rogers, J.M.; Duckworth, J.; Middleton, S.; Steenbergen, B.; Wilson, P.H. Elements virtual rehabilitation improves motor, cognitive, and functional outcomes in adult stroke: Evidence from a randomized controlled pilot study. J. Neuroeng. Rehabil. 2019, 16, 56. [Google Scholar] [CrossRef]
- Yin, C.W.; Sien, N.Y.; Ying, L.A.; Chung, S.F.C.M.; Leng, D.T.M. Virtual reality for upper extremity rehabilitation in early stroke: A pilot randomized controlled trial. Clin. Rehabil. 2014, 28, 1107–1114. [Google Scholar] [CrossRef]
- Brkic, L.; Shaw, L.; van Wijck, F.; Francis, R.; Price, C.; Forster, A.; Rodgers, H. Repetitive arm functional tasks after stroke (RAFTAS): A pilot randomised controlled trial. Pilot Feasibility Stud. 2016, 2, 50. [Google Scholar] [CrossRef]
- Harris, J.E.; Eng, J.J.; Miller, W.C.; Dawson, A.S.A. Self-Administered Graded Repetitive Arm Supplementary Program (GRASP) Improves Arm Function During Inpatient Stroke Rehabilitation A Multi-Site Randomized Controlled Trial. Stroke 2009, 40, 2123–2128. [Google Scholar] [CrossRef]
- Laver, K.E.; Adey-Wakeling, Z.; Crotty, M.; Lannin, N.A.; George, S.; Sherrington, C. Telerehabilitation services for stroke. Cochrane Database Syst. Rev. 2020, 1, CD010255. [Google Scholar] [CrossRef]
- Kringle, E.; Trammell, M.; Brown, E.D.; American Congress of Rehabilitation Medicine (ACRM) Stroke International Special Interest Group. Telerehabilitation Strategies and Resources for Rehabilitation Professionals. Arch. Phys. Med. Rehabil. 2023; online ahead of print. [Google Scholar] [CrossRef]
- Rintala, A.; Kossi, O.; Bonnechère, B.; Evers, L.; Printemps, E.; Feys, P. Mobile health applications for improving physical function, physical activity, and quality of life in stroke survivors: A systematic review. Disabil. Rehabil. 2022, 1–15. [Google Scholar] [CrossRef]
- Tchero, H.; Teguo, M.T.; Lannuzel, A.; Rusch, E. Telerehabilitation for Stroke Survivors: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2018, 20, e10867. [Google Scholar] [CrossRef]
- Tarihoran, D.E.T.A.U.; Daryanti Saragih, I.; Saragih, I.S.; Tzeng, H.M. Effects of videoconferencing intervention on stroke survivors: A systematic review and meta-analysis of randomised controlled studies. J. Clin. Nurs. 2023, 32, 5938–5947. [Google Scholar] [CrossRef]
- Sharififar, S.; Ghasemi, H.; Geis, C.; Azari, H.; Adkins, L.; Speight, B.; Vincent, H.K. Telerehabilitation service impact on physical function and adherence compared to face-to-face rehabilitation in patients with stroke: A systematic review and meta-analysis. PM R J. Inj. Funct. Rehabil. 2023; online ahead of print. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. J. Pharmacol. Pharmacother. 2010, 1, 100–107. [Google Scholar] [CrossRef]
- van der Lee, J.H.; Wagenaar, R.C.; Lankhorst, G.J.; Vogelaar, T.W.; Devillé, W.L.; Bouter, L.M. Forced use of the upper extremity in chronic stroke patients: Results from a single-blind randomized clinical trial. Stroke 1999, 30, 2369–2375. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Hall, J.; Dudgeon, B.; Guthrie, M. Validity of clinical measures of shoulder subluxation in adults with poststroke hemiplegia. Am. J. Occup. Ther. Off. Publ. Am. Occup. Ther. Assoc. 1995, 49, 526–533. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hinkle, J.L. Reliability and validity of the National Institutes of Health Stroke Scale for neuroscience nurses. Stroke 2014, 45, e32–e34. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef] [PubMed]
- Hawley-Hague, H.; Horne, M.; Skelton, D.A.; Todd, C. Review of how we should define (and measure) adherence in studies examining older adults’ participation in exercise classes. BMJ Open 2016, 6, e011560. [Google Scholar] [CrossRef]
- Hsieh, C.L.; Hsueh, I.P.; Chiang, F.M.; Lin, P.H. Inter-rater reliability and validity of the Action Research arm test in stroke patients. Age Ageing 1998, 27, 107–114. [Google Scholar] [CrossRef]
- Platz, T.; Eickhof, C.; van Kaick, S.; Engel, U.; Pinkowski, C.; Kalok, S.; Pause, M. Impairment-oriented training or Bobath therapy for severe arm paresis after stroke: A single-blind, multicentre randomized controlled trial. Clin. Rehabil. 2005, 19, 714–724. [Google Scholar] [CrossRef]
- Verheyden, G.; Nieuwboer, A.; Mertin, J.; Preger, R.; Kiekens, C.; De Weerdt, W. The Trunk Impairment Scale: A new tool to measure motor impairment of the trunk after stroke. Clin. Rehabil. 2004, 18, 326–334. [Google Scholar] [CrossRef]
- Collin, C.; Wade, D. Assessing Motor Impairment after Stroke—A Pilot Reliability Study. J. Neurol. Neurosurg. Psychiatry 1990, 53, 576–579. [Google Scholar] [CrossRef]
- Ghotbi, N.; Nakhostin Ansari, N.; Naghdi, S.; Hasson, S. Measurement of lower-limb muscle spasticity: Intrarater reliability of Modified Modified Ashworth Scale. J. Rehabil. Res. Dev. 2011, 48, 83–88. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Smith, M.B. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys. Ther. 1987, 67, 206–207. [Google Scholar] [CrossRef]
- Gregson, J.M.; Leathley, M.J.; Moore, A.P.; Smith, T.L.; Sharma, A.K.; Watkins, C.L. Reliability of measurements of muscle tone and muscle power in stroke patients. Age Ageing 2000, 29, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Pandyan, A.D.; Johnson, G.R.; Price, C.I.; Curless, R.H.; Barnes, M.P.; Rodgers, H. A review of the properties and limitations of the Ashworth and modified Ashworth Scales as measures of spasticity. Clin. Rehabil. 1999, 13, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Nijland, R.H.; van Wegen, E.E.; Harmeling-van der Wel, B.C.; Kwakkel, G.; EPOS Investigators. Presence of finger extension and shoulder abduction within 72 hours after stroke predicts functional recovery: Early prediction of functional outcome after stroke: The EPOS cohort study. Stroke 2010, 41, 745–750. [Google Scholar] [CrossRef] [PubMed]
- Akinci, B.; Yeldan, I.; Satman, I.; Dirican, A.; Ozdincler, A.R. The effects of Internet-based exercise compared with supervised group exercise in people with type 2 diabetes: A randomized controlled study. Clin. Rehabil. 2018, 32, 799–810. [Google Scholar] [CrossRef]
- Schnabel, S.; Kidd, L.; van Wijck, F. ’It was never too much’: Stroke survivors’ and their carers’ experiences with augmented arm physiotherapy in the EVERLAP study. Physiotherapy 2020, 107, e19–e20. [Google Scholar] [CrossRef]
- Lincoln, N.B.; Parry, R.H.; Vass, C.D. Randomized, controlled trial to evaluate increased intensity of physiotherapy treatment of arm function after stroke. Stroke 1999, 30, 573–579. [Google Scholar] [CrossRef]
- Parry, R.H.; Lincoln, N.B.; Vass, C.D. Effect of severity of arm impairment on response to additional physiotherapy early after stroke. Clin. Rehabil. 1999, 13, 187–198. [Google Scholar] [CrossRef] [PubMed]
- Wee, S.K.; Hughes, A.M.; Warner, M.B.; Brown, S.; Cranny, A.; Mazomenos, E.B.; Burridge, J.H. Effect of Trunk Support on Upper Extremity Function in People With Chronic Stroke and People Who Are Healthy. Phys. Ther. 2015, 95, 1163–1171. [Google Scholar] [CrossRef] [PubMed]
- Salgueiro, C.; Urrútia, G.; Cabanas-Valdés, R. Influence of Core-Stability Exercises Guided by a Telerehabilitation App on Trunk Performance, Balance and Gait Performance in Chronic Stroke Survivors: A Preliminary Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 5689. [Google Scholar] [CrossRef] [PubMed]
- Alhwoaimel, N.; Turk, R.; Warner, M.; Verheyden, G.; Thijs, L.; Wee, S.K.; Hughes, A.M. Do trunk exercises improve trunk and upper extremity performance, post stroke? A systematic review and meta-analysis. NeuroRehabilitation 2018, 43, 395–412. [Google Scholar] [CrossRef] [PubMed]
- Duncan Millar, J.; VAN Wijck, F.; Pollock, A.; Ali, M. International consensus recommendations for outcome measurement in post-stroke arm rehabilitation trials. Eur. J. Phys. Rehabil. Med. 2021, 57, 61–68. [Google Scholar] [CrossRef]
- Moulaei, K.; Sheikhtaheri, A.; Nezhad, M.S.; Haghdoost, A.; Gheysari, M.; Bahaadinbeigy, K. Telerehabilitation for upper limb disabilities: A scoping review on functions, outcomes, and evaluation methods. Arch. Public Health 2022, 80, 196. [Google Scholar] [CrossRef]
- Vloothuis, J.D.M.; Mulder, M.; Nijland, R.H.M.; Goedhart, Q.S.; Konijnenbelt, M.; Mulder, H.; Hertogh, C.M.P.M.; van Tulder, M.; van Wegen, E.E.H.; Kwakkel, G. Caregiver-mediated exercises with e-health support for early supported discharge after stroke (CARE4STROKE): A randomized controlled trial. PLoS ONE 2019, 14, e0214241. [Google Scholar] [CrossRef]
- NSS Information and Intelligence. Scottish Stroke Improvement Programme. Edinburgh: NSS Information and Intelligence. 2019. Available online: https://www.scot.nhs.uk/ (accessed on 15 May 2020).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).