Abstract
Globally, we have seen a drop in adult and child quality of life (QOL) during the COVID-19 pandemic. However, little is known about adult or child QOL during the height of the pandemic in Australia and the impact of government-imposed restrictions, specifically attending school on-site versus home schooling. Our study aimed to establish if QOL in children and parents presenting to a Respiratory Infection Clinic in Victoria, Australia, for COVID-19 PCR testing differed from pre-pandemic population norms. We also explored whether on-site versus home schooling further impacted QOL. Following the child’s test and prior to receiving results, consenting parents of children aged 6 to 17 years old completed the Child Health Utility 9 Dimension (CHU9D) instrument on their child’s behalf. Parents of children aged birth to five years completed the EuroQOL 5-Dimension 5-Level (EQ-5D-5L) instrument on their own behalf (cross-sectional study). Data analyses utilised quantile regression, adjusting for the child’s age, COVID-19 symptoms, gender and chronic health conditions. From July 2020 to November 2021, 2025 parents completed the CHU9D; the mean age for children was 8.41 years (±3.63 SD), and 48.4 per cent were female (n = 980/2025). In the same time period, 5751 parents completed the EQ-5D-5L; the mean age for children was 2.78 years (±1.74 SD), and 52.2 per cent were female (n = 3002/5751). Results showed that QOL scores were lower than pre-pandemic norms for 68 per cent of the CHU9D group and 60 per cent of the EQ-5D-5L group. Comparing periods of on-site to home schooling, there was no difference between the median QOL scores for both CHU9D (0.017, 95% CI −0.05 to 0.01) and EQ-5D-5L (0.000, 95% CI −0.002 to 0.002). Our large-scale study found that while QOL was reduced for children and parents at the point of COVID-19 testing during the pandemic, differing levels of government-imposed restrictions did not further impact QOL. These unique insights will inform decision-making in relation to COVID-19 and future pandemics.
1. Introduction
Early responses to the COVID-19 pandemic in most countries included lockdown measures to reduce community transmission of the virus. In the Australian state of Victoria, people experienced some of the toughest lockdowns globally. These included stay-at-home measures, school closures and restrictions regarding travel [1]. Victoria experienced multiple ‘waves’ of infection throughout 2020 and 2021, and restrictions changed frequently over this period [1]. As the pandemic progressed, concerns increased regarding the impact of COVID-19 testing and extended school closures—with subsequent periods of home learning—on both parent and child health-related quality of life (QOL) [2].
Globally, we have seen a significant drop in adult and child QOL utility scores during the pandemic era [3,4,5,6,7,8]. A range of factors have been found to increase the negative impact the COVID-19 pandemic has on QOL. Social factors include job loss, lower income, location, nationality, medical co-morbidities such as anxiety disorders and chronic disease states, as well as COVID-19-specific factors such as perceived risk of COVID-19 infection, presence of symptoms, contact with infected persons and a lack of access to information regarding the pandemic [6,7,9,10,11,12]. Almost universally, individuals living under stay-at-home orders have suffered a loss of QOL since the beginning of the pandemic [13,14]. Although there is no data on the impact of undergoing polymerase chain reaction (PRC) testing on QOL, there is potential concern about possible infection and anticipation while awaiting the result.
While children and families in Victoria have been significantly affected by some of the most stringent COVID-19-related restrictions and long periods of remote school learning globally, little is known about child and parent QOL during the height of the pandemic in the Australian context, nor about the impact of home schooling during the stay-at-home orders [15]. It is important to investigate the impact on children’s quality of life because the health state of a child can impact the QOL of the parents [16]. It is also important to investigate the effect of home schooling on QOL as this was a core strategy for the Victorian stay-at-home orders and placed much stress on the family unit during the COVID-19 pandemic [15,17].
The aim of this study was to determine parent-reported child quality of life and parent quality of life during COVID-19 public health restrictions. Measurements were taken at the point of child and parent COVID-19 testing at an Australian paediatric hospital outpatient clinic. The study objectives were to (i) report parent-reported QOL in children aged 6 to 17 years; (ii) report QOL in parents of children aged birth to 5 years; (iii) investigate the effect of schooling location on QOL (on-site or home-based) as impacted by government-imposed COVID-19 pandemic restrictions; and (iv) compare QOL results to pre-pandemic population norms. It was hypothesised that home-based schooling, compared to on-site schooling, would have a negative impact on QOL and that QOL during the pandemic would be generally less than pre-pandemic population norms.
2. Methods
2.1. Study Setting
We completed this study at The Royal Children’s Hospital Respiratory Infection Clinic (RIC) in Melbourne, Victoria. The RIC was established in May 2020 and was a large testing site in Melbourne for children, particularly those under the age of five years who required testing according to state guidelines [18]. In Victoria, government-imposed restrictions relating to stay-at-home orders, including home schooling, were the most stringent in the country. The stay-at-home orders were ceased and reenacted multiple times throughout the COVID-19 pandemic [15]. Unique factors for this study are as follows:
- (1)
- This single-centre study was conducted at Victoria’s largest tertiary paediatric hospital, and this hospital was the only dedicated testing centre for children under five years of age in Victoria. As such, it captured the largest cohort of children under 5 years old in urban Melbourne and was also accessed by many regional families due to the anticipated distress of testing in young children;
- (2)
- We acknowledge that this study is not representative of children and families across Australia, and this was not the intention. Each state and territory in Australia experienced differing levels of COVID-19 waves of infection and subsequent public health restrictions. These results are specific to children and families in metropolitan Melbourne, Victoria, who visited the paediatric hospital outpatient clinic for COVID-19 testing and experienced the most stringent and long-lasting lockdowns in Australia. The experience of children and families would almost certainly have been different in the other Australian states, especially Western Australia, where no lockdowns were applied. These data are representative of populations undergoing harsh pandemic restrictions and the potential impact on QOL and wellbeing;
- (3)
- Our data have been time-stamped to allow comparison between periods of home and on-site schooling, which has generated intense debate in the media and between political parties in Australia and globally and, as such, will be of broad interest.
2.2. Study Design
This is a cross-sectional cohort study based on a single brief survey instrument to assess parent or child QOL and was administered soon after PCR COVID-19 testing. A sample of those who completed the QOL assessment were later invited to enrol in the COVID Wellbeing Study, a mixed-methods longitudinal cohort study investigating the immediate and longer-term health and wellbeing impacts of COVID-19 on children and families tested for COVID-19 at the RIC. The findings of the COVID Wellbeing Study will be published separately.
2.3. Participants and Consent
The sample included children and parents attending the RIC for respiratory SARS-CoV-2 PCR testing between July 2020 and November 2021. Parents completed the QOL instrument on behalf of themselves if the child was under five years old, or as a proxy for their child if the child was six years or older. Parents may or may not have been tested at the same time. All parents attending the RIC were asked, upon registration, for their consent to be contacted about COVID-19 research. Those who consented were sent a link via email to complete an online QOL assessment immediately following COVID-19 testing and prior to receiving test results. Consent to participate was implied by survey completion. The survey was only available in English.
If parents presented to the RIC Clinic for multiple episodes of their child’s COVID-19 testing during the data collection period, they were invited to complete the survey each time. The analysis has considered each response independent of the previous response, as it is not known how many repeat visits occurred due to the nature of the data or if it was the same parent who completed the survey on subsequent visits. If a parent did not complete the survey, they received three follow-up reminders.
Sample size: The sample size for this cross-sectional cohort study is all children and parents who attended the COVID-19 outpatient testing site at the state’s largest paediatric hospital between July 2020 and November 2021 and provided consent for study participation. It was not possible to establish an a priori sample size for this study, as this study commenced at the beginning of the pandemic in Australia when we were unable to predict how many children and parents would attend the testing site as the prevalence of the disease was unknown.
Sample selection: Reference population were people living in the City of Greater Melbourne in 2020/21 = 816,536 families with an average of 1.8 children aged 15 or less (https://www.abs.gov.au/census/find-census-data/quickstats/2021/2GMEL; accessed on 1 June 2022). Study population were people who attended the COVID-19 outpatient testing site between July 2020 and November 2021 (n = 70,000). Study participants were those from the study population who consented to participate in the survey (Figure 1).
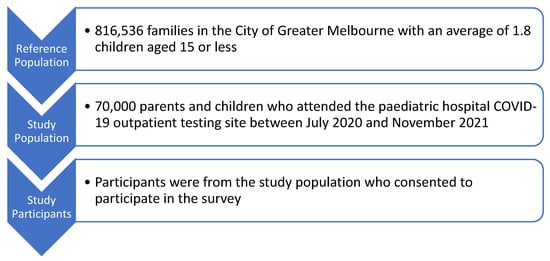
Figure 1.
Sample selection.
As all parents who attended the testing site with their child(ren) and provided consent to be sent a link via email to consider participating in the research were sent the study link, there was no sample-selection bias (as all parents were approached, and all parents who provided consent to send a link via email were invited). However, there is the possibility of self-selection bias with respect to the individuals who completed the survey. It is also noted that the identification of home vs. on-site schooling was done based on the data date stamp at the data analysis stage and was unlikely to be influenced by self-selection.
2.4. Data Collection
Data were collected over 18 months, between July 2020 and November 2021, representing the early to mid-stages of the COVID-19 pandemic. The surveys were administered using REDCap [19,20], a secure web-based platform to capture data for research, hosted at Murdoch Children’s Research Institute, Melbourne. Parents of children aged birth to five years old completed the EuroQOL 5-Dimension 5-Level (EQ-5D-5L) [21] questionnaire on their own behalf. Parents of children aged 6 to 17 years old completed the validated proxy-reported Child Health Utility 9 Dimension (CHU9D) [14] questionnaire on behalf of their child. Most questionnaires were completed at the RIC during the visit, as compared to being completed at home after the RIC visit.
2.5. Outcome Measures
The EQ-5D-5L instrument is the world’s most widely applied preference-based measure of health-related QOL and includes five key dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Participants are asked to rate their level of health across five levels within each of these domains (from ‘no problems’ to ‘extreme problems’), and the instrument takes, on average, about two minutes to complete [22].
Globally, psychometric testing for the EQ-5D-5L with adult populations has been extensive and includes the development of UK as well as many additional normative value sets in, for example, Spain, Hong Kong, France, Ethiopia, USA, Japan, Korea, Netherlands and China [21]. A recent systematic review examined the psychometric properties of the EQ-5D-5L and reported on 99 studies across 32 countries. The systematic review reported that reliability was strong for 9 of the 9 studies that examined this property and concluded that the EQ-5D-5L had excellent psychometric properties across multiple settings, populations and conditions [23]
Specific to Australia, an EQ-5D-5L value set has been recently developed for Australian adults, and this includes establishing utility weights for each health state [24,25]. The validity of the EQ-5D-5L in Australia has been evaluated across multiple studies, and examples of these studies include testing psychometric properties of the EQ-5D-5L with the First Nations peoples of Australia [26], validation for people living with multiple sclerosis [27], validation for people undergoing a hip replacement [28] and validation for people experiencing chronic fatigue syndrome [29]. Finally, the EQ-5D-5L has also been comparted to other QOL tools within the Australian context [30].
The CHU9D instrument was developed from the ground up to measure and value QOL in child populations. The CHU9D includes nine dimensions (worried, sad, pain, tired, annoyed, schoolwork, sleep, daily routine and ability to join in activities), with five response levels attached to each dimension [14]. The CHU9D has been validated for children aged 6 to 17 years old and takes about two minutes to complete.
Globally, psychometric testing for the CHU-9D with adolescent populations has been extensive and includes the development of UK and additional normative value sets in Peru [31], Spain [32], Sweden [33] and Netherlands [34], as well as measuring the impact of specific conditions on adolescent QOL, such as inflammatory bowel disease (Canada) [35] and oral/dental health conditions (Netherlands and New Zealand) [36,37]. Validity, reliability, feasibility and overall intelligibility/acceptability have been tested in the context of Swedish school-aged children [33], Danish children receiving mental health care (longitudinal, discriminant and convergent validity) [38,39] and in the UK education setting [40], and the tool has been evaluated for appropriateness of inclusion in economic evaluations [41].
Specific to Australia, a CHU9D value set has been developed for Australian adolescents [42], and the construct validity of the CHU9D has been evaluated across multiple studies. Examples of these studies include practicality and validity with general Australian adolescents [41], testing the validity of the CHU9D as a routine outcome measure for use in child and adolescent mental health services [43], reliability, acceptability, validity and responsiveness of the CHU9D for Australian children who are overweight and obese [44], data quality, feasibility, acceptability and construct validity [45], as well as via comparison with other adolescent quality of life tools [45,46].
For both QOL instruments, the raw QOL scores were converted into utilities on the 0–1 quality-adjusted life year (QALY) scale where 0 represents a state equal to being dead and 1 represents a state of full health [47]. CHU9D utilities were generated by applying the Australian adolescent preference weighted scoring algorithm (https://licensing.sheffield.ac.uk/product/CHU9D; accessed on 1 May 2022), and this was based on the ‘profile case best worst scaling’ methods to generate adolescent population health state values [47]. The EQ-5D-5L utilities were generated by applying the UK adult preference weights via the crosswalk calculator (https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/valuation-standard-value-sets/crosswalk-index-value-calculator/; accessed on 1 May 2022), and this was based on a protocol that combined the composite time trade-off valuation technique and a discrete-choice experiment [21].
2.6. Data Coding
Data were time-stamped and coded according to the level of government-imposed restrictions related to the location of school learning at the time of the child’s COVID-19 test. Restriction levels were categorised as Level 1: Children attend school on site (plus or minus other restrictions) or Level 2: Children do not attend school on-site and complete remote learning at home (plus or minus other restrictions).
2.7. Analysis
As QOL data do not typically have a normal distribution due to the positive skew towards a higher utility index score, QOLs were summarised using median and interquartile range. Median QOL between the two groups (Level 1 and Level 2) were compared using non-parametric quantile regressions to determine the effect of government-imposed restrictions, which impacted schooling location (on-site versus home), on QOL in children and parents adjusting for age, gender, symptoms of COVID-19 and chronic conditions. The QOLs were also categorised into a binary variable using the appropriate population norm as a cut-off and summarised using numbers and percentages. Binary logistic regressions were used to assess the effect of on-site schooling and home schooling on QOLs adjusting for age, gender, symptoms of COVID-19 and chronic conditions. Subsequently, the adjusted differences between two proportions were calculated using the fitted models. The child’s age, symptoms of COVID-19, gender and chronic health conditions were included in the models as these are known predictors of QOL [48,49,50].
To allow comparison with the published literature, where QOL data are most commonly presented as a mean value, the utility index and the individual domain scores have also been reported using means and standard deviations via a one-sample t-test for the QOL utility index scores (nominal data) as well as the individual domain scores (ordinal data). Data analysis was conducted in SPSS Version 25.
3. Results
There were approximately 70,000 presentations to the RIC during the study period. QOL data at the point of PCR COVID-19 testing were collected from 7931 families (n = 7931/70.000; 11.3%) over a time period of 71 weeks during the COVID-19 pandemic (July 2020 to November 2021). This included 2025 complete CHU9D responses for children and 5751 complete EQ-5D-5L responses for parents. Surveys missing complete CHU9D data (n = 74) and EQ-5D-5L data (n = 79) were excluded (Figure A1).
For both the CHU9D group and the EQ-5D-5L group, approximately half the children were female, and 74 per cent of children were under six years old (EQ-5D-5L group). Eighty-four per cent of children six years and over (CHU9D group) presented with COVID-19-related symptoms. The most common symptom in both groups was a runny/stuffy nose, occurring in 52 per cent under six years old and 65 per cent six years and over (Table 1).

Table 1.
Demographic and baseline symptoms of children included in study.
3.1. CHU9D
The median CHU9D value for the on-site schooling group was 0.741 (IQR 0.549 to 0.888), and for the home schooling group, it was 0.744 (IQR 0.550 to 0.905). There was insufficient evidence to suggest a difference in median CHU9D utilities between the two cohorts after adjusting for age, gender, symptoms of COVID-19 and chronic conditions (adjusted difference in median −0.02, 95% CI −0.05 to 0.01, p = 0.235). The median quality of life of the on-site schooling (0.741) and home schooling (0.744) was less than the median quality of life (0.86) of the corresponding pre-pandemic population norms. The median quality of life across all age groups for both cohorts is presented in Figure 2.
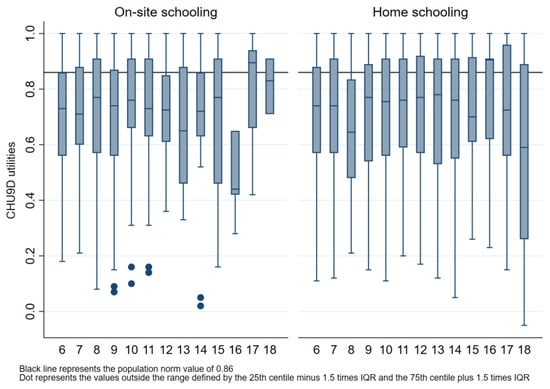
Figure 2.
Comparison of median (IQR) CHU9D utility scores for all age groups by on-site or home schooling and by the population norm. Box plot lines represent 25th, 50th and 75th percentiles.
During on-site schooling, 69.6 per cent (471/677) of the utilities, and during home schooling, 67.2 per cent (906/1348) of the utilities were below the 0.86 population norm score [51]. The difference in the proportion of children with a CHU9D utility below 0.86 [51] between on-site and home schooling groups was minimal after adjusting for age, gender, symptoms of COVID-19 and chronic conditions (adjusted difference in proportion 0.5%, 95% CI −3.8% to 4.9%, p = 0.813).
3.2. CHU9D Presented as Parametric Data to Enable Comparison with the Literature
At the time of COVID-19 testing, based on proxy reporting via the CHU9D by the parents of children aged 6 to 17 years old, the children’s mean utilities was 0.710 (SD 0.220). There was no mean difference in utilities between the two levels of government restrictions; however, three of the individual domains on the CHU9D had sufficient evidence of differences (Table A1). Pain was higher during on-site schooling compared to home schooling (difference in mean 0.085, 95% CI 0.018 to 0.151, p = 0.013), tiredness was higher in on-site schooling compared to home schooling (difference in mean 0.151, 95% CI 0.053 to 0.249, p = 0.003) and activity was higher in on-site schooling compared to home schooling (difference in mean 0.173, 95% CI 0.042 to 0.305, p = 0.010).
3.3. EQ-5D-5L
The median value for the on-site schooling group was 0.879 (Q1 0.837; Q3 1.000), and for the home schooling group, it was also 0.879 (Q1 0.837; Q3 1.000). There was no evidence of a difference in median EQ-5D-5L score between the two groups after adjusting for age, gender, symptoms of COVID and chronic conditions (adjusted difference in median 0, 95% CI −0.002 to 0.002, p = 1.000). For parents of children, the median quality of life for the current cohort (0.897) was less than the median quality of life of the corresponding pre-pandemic population norms (0.95). The median quality of life for parents of children across all child age groups is presented in Figure 3.
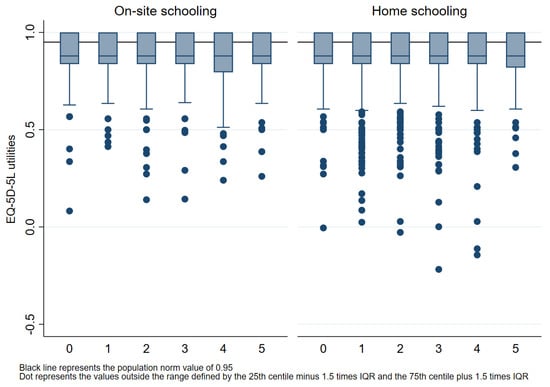
Figure 3.
Comparison of median (IQR) EQ-5D-5L utility scores for all age groups by on-site or home schooling and by the population norm. Box plot lines represent 25th, 50th and 75th percentiles.
During on-site schooling, 59.0 per cent (1006/1705) of the utilities, and during home schooling, 60.6 per cent (2453/4046) of the utilities were below the 0.95 population norm score [25]. The difference in the proportion of parents with EQ-5D-5L utilities below 0.95 between the on-site and home schooling group was minimal after adjusting for age, gender, symptoms of COVID-19 and chronic conditions (adjusted difference in proportion 1.8%, 95% CI −0.9% to 4.6%, p = 0.195).
3.4. EQ-5D-5L Presented as Parametric Data to Enable Comparison with the Literature
At the time of the child’s PCR COVID-19 test, based on the EQ-5D-5L, the combined mean utility index for parents of children aged five years and under was 0.882 (SD 0.131). For the EQ-5D-5L, there was no mean difference in utility index score between the two levels of government restrictions; however, one of the individual domains on the EQ-5D-5L had a significant difference; Table A2. Anxiety was lower during on-site schooling compared to home schooling (difference in mean −0.065, 95% CI −0.108 to −0.021, p = 0.003).
4. Discussion
Children and their parents accessing PCR COVID-19 testing experienced a lower QOL at the point of testing when compared to pre-pandemic population norms. However, there was no observed effect of schooling location, impacted by government-imposed COVID-19 pandemic restrictions, on QOL in children or parents. These findings indicate that during COVID-19 testing, parent and child QOL utilities were found to be between 0.15 and 0.07 below normative data, exceeding the reported 0.03 minimal clinically important difference for generic QOL utility scores [52,53,54].
The difference in utility scores could be due to multiple factors, including the threat of the COVID-19 pandemic itself or the response, such as the government-imposed restrictions, changes in employment or living arrangements, COVID-19 testing process or other individual reasons. There have been many disproportionate effects of the pandemic on the wellbeing of children, which may have impacted the utility scores [6,9,50,55]. Young people have experienced an increase in mental health difficulties and reported a reduction in physical activity, healthy eating and general wellbeing [9,49,55]. An Australian study found a decrease in life satisfaction and an increase in anxiety and depression among parents and children during lockdown [56].
We do not understand to what extent COVID testing and the period of uncertainty following testing impact children’s QOL, but isolation after testing due to a positive or suspected COVID diagnosis likely results in a QOL utility decrease in parents and children [56,57]. There is minimal data regarding the impact of the COVID testing process itself or the impact of repeated testing, which many children experienced as they returned to childcare and school. It should be noted that the testing experience has changed over time, particularly since late 2021 when the government began to recommend at-home Rapid Antigen Testing instead of, or in addition to, PCR testing.
While this study did not show that home schooling compared to on-site schooling was a factor that impacted quality of life, other independent factors, such as vaccination, did impact quality of life during the COVID-19 pandemic. Globally, vaccines improved quality of life and mental health, reduced the spread of the disease, improved health outcomes for hospitalised patients and contributed to the end of lockdowns [58,59,60,61]. Specific to quality of life, when comparing partially vaccinated people and people waiting to be vaccinated to fully vaccinated people, the fully vaccinated people had a higher quality of life [58].
As the impact of the COVID-19 pandemic differed within counties and between countries, it is important that literature reports on the impact on the whole of the country, as well as on regions within a country. Survey-based studies examining the regional impacts have focussed on specific sub-populations, and recent examples of such studies include the following: the impact of COVID-19 on reduced physical activity experienced by young adult university students in Italy (n = 1430) [62]; the impact of COVID-19 on vaccine hesitancy from home health care service recipients in Saudi Arabia (n = 426) [63]; the impact of COVID-19 on developmental outcomes among kinship foster care children in the Republic of Korea (n = 217) [64]; the impact of COVID-19 on of perceived travel risks by travellers in Taiwan (n = 500) [65] and the impact of COVID-19 related lockdown on adult mental health in Italy (n = 1085) [66]. The current survey-based study reports on the regional impacts of a specific sub-population, specifically parent-reported child and parent quality of life during COVID-19 testing at a tertiary paediatric hospital outpatient clinic in metropolitan Melbourne, Australia (n = 7776). The current study is unique in that surveys were completed by parents of young children who visited the state’s largest paediatric hospital outpatient clinic for COVID-19 testing, which included the only dedicated facility for testing children under 5 years of age, in a region that experienced the most stringent pandemic lockdown conditions in Australia and globally.
Strengths and Limitations
This is the only study we are aware of in Australia that captured QOL data for children and families during the height of the COVID-19 restrictions in 2020–2021 in the state that experienced the most COVID-19 cases and strongest restrictions. This study has several strengths, including an extended data collection period of 71 weeks which captured the changing government-imposed COVID-19 restrictions, a large sample size for both the CHU9D and the EQ-5D-5L surveys, as well as support through Victoria’s largest public paediatric hospital.
Data from this study may enable future researchers to identify the pandemic shock over a long period of time. In addition, by using validated and frequently used QOL tools within this study [67], the opportunity for comparison between current and future studies has been maximised. This study has also highlighted the value of including QOL measures in longitudinal data sets to understand change over time and change in relation to significant public health events.
Despite the new and valuable data produced by this study, it has a number of limitations that should be considered. Our study population was not representative of the whole Victorian (or Australian) population and, as such, was skewed towards younger adults/parents (due to those under the age of five being referred to The Royal Children’s Hospital RIC for testing) who were relatively homogenous demographically. The survey was only available in English, limiting participation from culturally and linguistically diverse participants. We were unable to track multiple responses from one family, so some families could have been counted more than once. While we captured QOL around the time of COVID-19 testing, it is not possible to say whether the testing experience itself or other circumstances were the primary contributing factors to the QOL reported on the day. At the time of survey completion, participants did not know their test results.
Parents of children aged birth to five years old completed the EQ-5D-5L [21] questionnaire on their own behalf, as no QOL tool has been validated for children of this age group. Parents of children aged 6 to 17 years old completed the validated proxy-reported CHU9D questionnaire on behalf of their child [38]. The reason this was completed as a proxy by the parents, compared to being completed by the children themselves, was due to early reports of the negative impact of COVID-19 on child mental health and the desire to minimise the research burden on children. However, this proxy child QOL score may be prone to bias from the parent completing the survey. While other options for determining the child QOL may have been more accurate and less prone to bias, for example, the child completing the QOL questionnaire themselves, it was not feasible in the current study. While all parents were invited to complete the QOL survey (i.e., no sample-selection bias), it was not completed by all parents, so there may be bias with parents who did complete the survey representing those experiencing a different (higher or lower) QOL when compared to those who did not complete the QOL survey (i.e., potential for self-selection bias).
The analyses could only consider factors associated with the children, e.g., age, gender and co-morbidities, not with the parents. This is a potential limitation as these parental factors could also have impacted the results. A further limitation was that the difference between the QOL reported in the current study and the QOL reported in a previous pre-pandemic study was not tested for statistical significance, as the comparison involved two different populations, i.e., while our analysis did not test for statistical significance, it did explore how the current study median values and interquartile range compares to the previous pre-pandemic study median values (Figure 1 and Figure 2).
Finally, due to the COVID-19 pandemic, there were immense time pressures to commence the COVID Wellbeing program of research. As such, time did not permit the involvement of patient groups in the design or conduct of the study. Generalisability is limited to the metropolitan population in Victoria due to the single point of data collection.
In the future, we recommend that the preservation of community quality of life is given equal importance to other key pandemic considerations, such as reducing the spread of the disease and developing vaccinations to prevent infections and improve health outcomes for hospitalised patients.
5. Conclusions
Children and their parents accessing PCR COVID-19 testing experienced a lower QOL at the point of testing when compared to pre-pandemic population norms. However, there was no observed effect of schooling location, impacted by government-imposed COVID-19 pandemic restrictions, on QOL in children or parents. This large-scale study assessing the QOL of school-aged children and of parents of pre-school children during the COVID-19 pandemic provided unique insights into the impact of testing and government-imposed restrictions to inform future decision-making and planning globally in relation to COVID-19 and future pandemics. This study also highlighted the importance of collecting QOL in longitudinal data sets.
Author Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection and analysis were performed by all authors. The first draft of the manuscript was written by N.K.B., M.D. and J.K., and all authors commented on previous versions of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by The Royal Children’s Hospital Foundation, Victoria, Australia. Author Natasha Brusco has received research support from The Royal Children’s Hospital.
Institutional Review Board Statement
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by The Royal Children’s Hospital Ethics Committee (May 2020; HREC/63636/RCHM-2019).
Informed Consent Statement
Written informed consent was obtained from the parents.
Data Availability Statement
The data presented in this study are available on reasonable request from the corresponding author. The data are not publicly available due to privacy restrictions.
Acknowledgments
We would like to acknowledge the families who participated in, and the staff who supported, this research project. During a time of great pressure, you supported clinical research to try and better understand the impact of the COVID-19 pandemic on our community.
Conflicts of Interest
The authors have no relevant financial or non-financial interest to disclose.
Appendix A
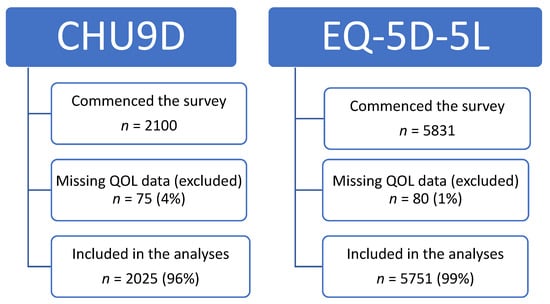
Figure A1.
Participant flow.
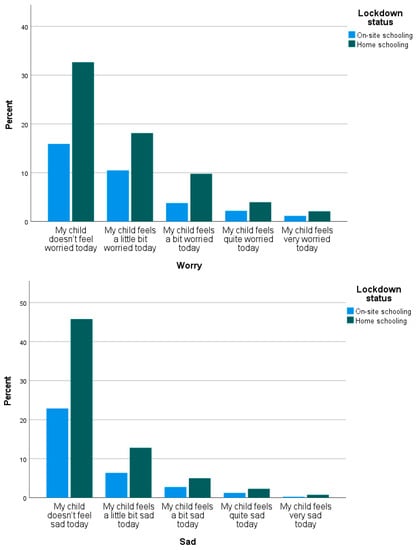
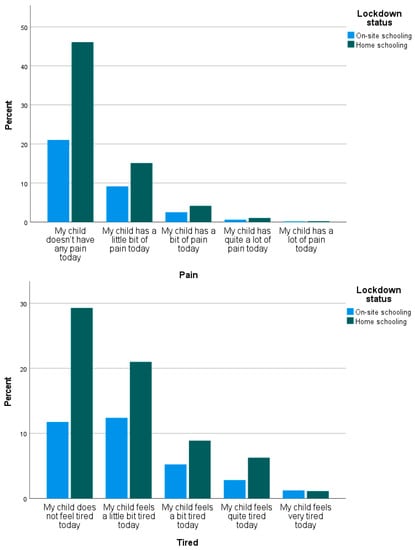
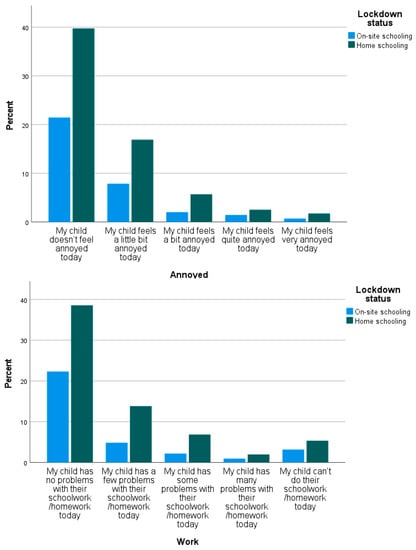
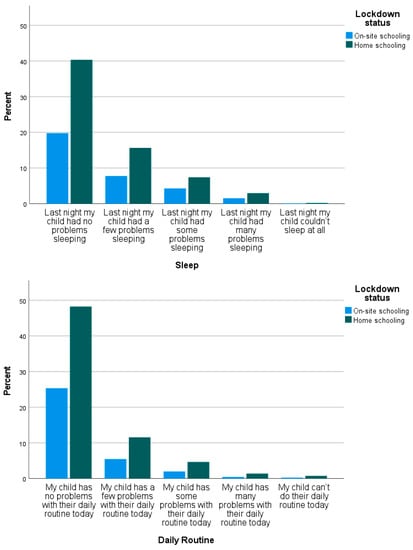
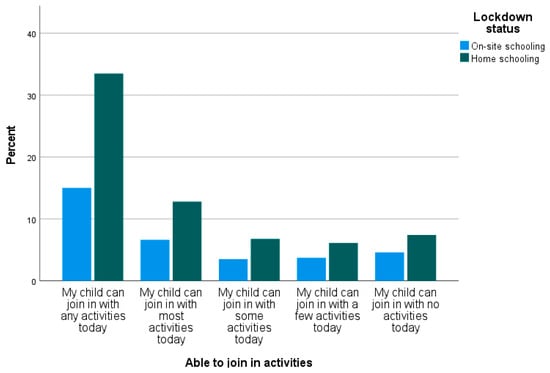
Figure A2.
Distribution of the categories for the nine individual CHU9D domains.

Table A1.
CHU9D utility index and domain scores.
Table A1.
CHU9D utility index and domain scores.
| On-Site Schooling (n = 677) | Home Schooling (n = 1348) | Mean Difference * On-Site Minus Home Schooling | |
|---|---|---|---|
| CHU9D Utility Index | 0.710 (SD 0.215) | 0.710 (SD 0.222) | −0.0003 (95% CI −0.021 to 0.020), p = 0.981 |
| CHU9D Worry Domain | 1.869 (SD 1.067) | 1.869 (SD 1.067) | 0.000 (95% CI −0.099 to 0.098), p = 0.998 |
| CHU9D Sad Domain | 1.493 (SD 0.851) | 1.489 (SD 0.859) | 0.004 (95% CI −0.075 to 0.084), p = 0.912 |
| CHU9D Pain Domain | 1.495 (SD 0.749) | 1.410 (SD 0.704) | 0.085 (95% CI 0.018 to 0.151), p = 0.013 |
| CHU9D Tired Domain | 2.084 (SD 1.083) | 1.933 (SD 1.049) | 0.151 (95% CI 0.053 to 0.249), p = 0.003 |
| CHU9D Annoyed Domain | 1.567 (SD 0.934) | 1.642 (SD 0.969) | −0.074 (95% CI −0.163 to 0.014), p = 0.099 |
| CHU9D Work Domain | 1.737 (SD 1.276) | 1.823 (SD 1.222) | −0.086 (95% CI −0.201 to 0.028), p = 0.139 |
| CHU9D Sleep Domain | 1.638 (SD 0.894) | 1.603 (SD 0.875) | 0.035 (95% CI −0.046 to 0.116), p = 0.399 |
| CHU9D Daily Domain | 1.350 (SD 0.718) | 1.420 (SD 0.801) | −0.070 (95% CI −0.141 to 0.002), p = 0.056 |
| CHU9D Activity Domain | 2.2902 (SD 1.467) | 2.116 (SD 1.401) | 0.173 (95% CI 0.042 to 0.305), p = 0.010 |
* Use of t-tests for parametric data. Bold = statistically significant.
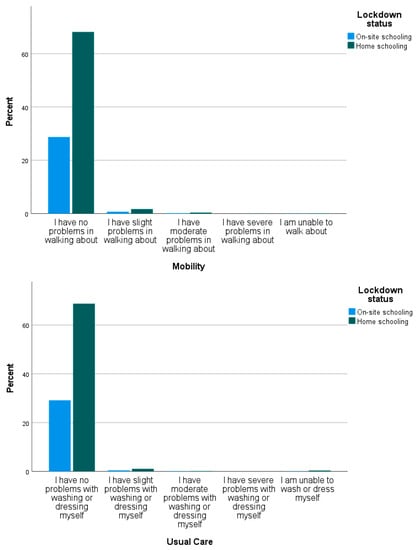
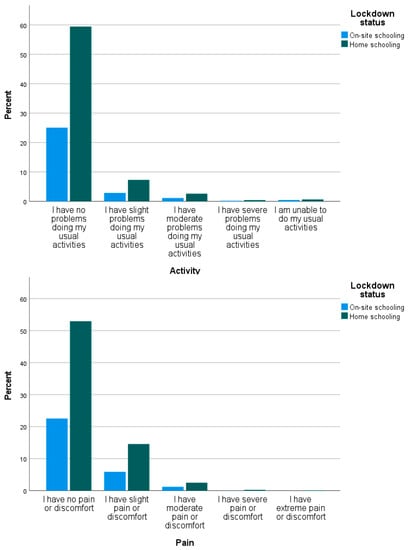
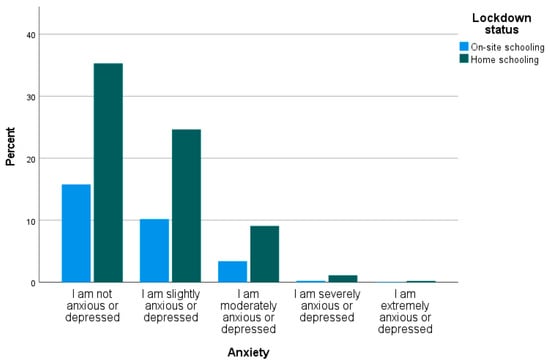
Figure A3.
Distribution of the categories for the five individual EQ-5L-5D domains.

Table A2.
EQ-5D-5L utility index and domain scores.
Table A2.
EQ-5D-5L utility index and domain scores.
| On-Site Schooling (n = 1705) | Home Schooling (n = 4046) | Mean Difference * On-Site Minus Home Schooling | |
|---|---|---|---|
| EQ-5D-5L Utility Index | 0.887 (SD 0.124) | 0.880 (SD 0.134) | 0.007 (95% CI −0.0004 to 0.014), p = 0.065 |
| EQ-5D-5L Mobility Domain | 1.042 (SD 0.271) | 1.043 (SD 0.274) | −0.001 (95% CI −0.016 to 0.015), p = 0.946 |
| EQ-5D-5L Usual Care Domain | 1.023 (SD 0.204) | 1.039 (SD 0.319) | −0.016 (95% CI −0.032 to 0.001), p = 0.058 |
| EQ-5D-5L Activity Domain | 1.248 (SD 0.688) | 1.230 (SD 0.626) | 0.017 (95% CI −0.019 to 0.054), p = 0.350 |
| EQ-5D-5L Pain Domain | 1.282 (SD 0.536) | 1.294 (SD 0.563) | −0.013 (95% CI −0.044 to 0.019), p = 0.432 |
| EQ-5D-5L Anxiety Domain | 1.603 (SD 0.732) | 1.668 (SD 0.781) | −0.065 (95% CI −0.108 to −0.021), p = 0.003 |
* Use of t-tests for parametric data. Bold = statistically significant.
References
- Macreadie, I. Reflections from Melbourne, the World’s Most Locked-Down City, through the COVID-19 Pandemic and Beyond; The Australian Society for Microbiology Inc.: Melbourne, Australia, 2022; p. 3. [Google Scholar]
- Viner, R.; Russell, S.; Saulle, R.; Croker, H.; Stansfeld, C.; Packer, J.; Hudson, L. Impacts of school closures on physical and mental health of children and young people: A systematic review. JAMA Pediatr. 2022, 176, 400–409. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Kaman, A.; Erhart, M.; Otto, C.; Devine, J.; Löffler, C.; Hurrelmann, K.; Bullinger, M.; Barkmann, C.; Siegel, N.A.; et al. Quality of life and mental health in children and adolescents during the first year of the COVID-19 pandemic: Results of a two-wave nationwide population-based study. Eur. Child Adolesc. Psychiatry 2021, 32, 575–588. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Kaman, A.; Erhart, M.; Devine, J.; Schlack, R.; Otto, C. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur. Child Adolesc. Psychiatry 2022, 31, 879–889. [Google Scholar] [CrossRef] [PubMed]
- Adıbelli, D.; Sümen, A. The effect of the coronavirus (COVID-19) pandemic on health-related quality of life in children. Child. Youth Serv. Rev. 2020, 119, 105595. [Google Scholar] [CrossRef] [PubMed]
- Geirdal, A.K.Ø.; Price, D.; Schoultz, M.; Thygesen, H.; Ruffolo, M.; Leung, J.; Bonsaksen, T. The significance of demographic variables on psychosocial health from the early stage and nine months after the COVID-19 pandemic outbreak. A Cross-National Study. Int. J. Environ. Res. Public Health 2021, 18, 4345. [Google Scholar] [CrossRef]
- Shamblaw, A.L.; Rumas, R.L.; Best, M.W. Coping during the COVID-19 pandemic: Relations with mental health and quality of life. Can. Psychol. Psychol. Can. 2021, 62, 92. [Google Scholar] [CrossRef]
- Suryavanshi, N.; Kadam, A.; Dhumal, G.; Nimkar, S.; Mave, V.; Gupta, A.; Gupte, N. Mental health and quality of life among healthcare professionals during the COVID-19 pandemic in India. Brain Behav. 2020, 10, e01837. [Google Scholar] [CrossRef]
- Imran, N.; Zeshan, M.; Pervaiz, Z. Mental health considerations for children & adolescents in COVID-19 Pandemic. Pak. J. Med. Sci. 2020, 36, S67. [Google Scholar]
- Lebrasseur, A.; Fortin-Bédard, N.; Lettre, J.; Raymond, E.; Bussières, E.L.; Lapierre, N.; Ouellet, M.C. Impact of the COVID-19 pandemic on older adults: Rapid review. JMIR Aging 2021, 4, e26474. [Google Scholar] [CrossRef]
- Persson, U.; Olofsson, S.; Gu, N.Y.; Gong, C.L.; Jiao, X.; Hay, J.W. Quality of Life in the Swedish General Population During COVID-19-Based on pre-and post-pandemic outbreak measurement. Nord. J. Health Econ. 2021, 9, 56–73. [Google Scholar] [CrossRef]
- Schuster, N.A.; de Breij, S.; Schaap, L.A.; van Schoor, N.M.; Peters, M.J.; de Jongh, R.T.; Hoogendijk, E.O. Older adults report cancellation or avoidance of medical care during the COVID-19 pandemic: Results from the Longitudinal Aging Study Amsterdam. Eur. Geriatr. Med. 2021, 12, 1075–1083. [Google Scholar] [CrossRef] [PubMed]
- Kasar, K.S.; Karaman, E. Life in lockdown: Social isolation, loneliness and quality of life in the elderly during the COVİD-19 pandemic: A scoping review. Geriatr. Nurs. 2021, 42, 1222–1229. [Google Scholar] [CrossRef] [PubMed]
- Petersen, K.D.; Chen, G.; Mpundu-Kaambwa, C.; Stevens, K.; Brazier, J.; Ratcliffe, J. Measuring Health-Related Quality of Life in Adolescent Populations: An Empirical Comparison of the CHU9D and the PedsQL TM 4.0 Short Form 15. Patient-Patient-Centered Outcomes Res. 2018, 11, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Stobart, A.; Duckett, S. Australia’s Response to COVID-19. Health Econ. Policy Law 2022, 17, 95–106. [Google Scholar] [CrossRef] [PubMed]
- Vonneilich, N.; Lüdecke, D.; Kofahl, C. The impact of care on family and health-related quality of life of parents with chronically ill and disabled children. Disabil. Rehabil. 2016, 38, 761–767. [Google Scholar] [CrossRef] [PubMed]
- Thorell, L.B.; Skoglund, C.; de la Peña, A.G.; Baeyens, D.; Fuermaier, A.B.; Groom, M.J.; Mammarella, I.C.; Van der Oord, S.; van den Hoofdakker, B.J.; Luman, M.; et al. Parental experiences of homeschooling during the COVID-19 pandemic: Differences between seven European countries and between children with and without mental health conditions. Eur. Child Adolesc. Psychiatry 2021, 31, 649–661. [Google Scholar] [CrossRef]
- Victorian State Government (Department of Health). Pandemic Order Register. 2022. Available online: https://www.health.vic.gov.au/covid-19/coronavirus-covid-19 (accessed on 21 January 2022).
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; Kirby, J. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- EuroQOL. EQ-5D. 2020. Available online: https://euroqol.org/ (accessed on 30 June 2021).
- Stark, P.A.; Myles, P.S.; Burke, J.A. Development and Psychometric Evaluation of a Postoperative Quality of Recovery Score The QoR-15. J. Am. Soc. Anesthesiol. 2013, 118, 1332–1340. [Google Scholar] [CrossRef]
- Feng, Y.-S.; Kohlmann, T.; Janssen, M.F.; Buchholz, I. Psychometric properties of the EQ-5D-5L: A systematic review of the literature. Qual. Life Res. 2021, 30, 647–673. [Google Scholar] [CrossRef]
- Norman, R.; Mulhern, B.; Lancsar, E.; Lorgelly, P.; Ratcliffe, J.; Street, D.; Viney, R. The Use of a Discrete Choice Experiment Including Both Duration and Dead for the Development of an EQ-5D-5L Value Set for Australia. PharmacoEconomics 2023, 41, 427–438. [Google Scholar] [CrossRef]
- McCaffrey, N.; Kaambwa, B.; Currow, D.C.; Ratcliffe, J. Health-related quality of life measured using the EQ-5D–5L: South Australian population norms. Health Qual. Life Outcomes 2016, 14, 133. [Google Scholar] [CrossRef]
- Ribeiro Santiago, P.H.; Haag, D.; Macedo, D.M.; Garvey, G.; Smith, M.; Canfell, K.; Hedges, J.; Jamieson, L. Psychometric properties of the EQ-5D-5L for aboriginal Australians: A multi-method study. Health Qual. Life Outcomes 2021, 19, 81. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.A.; Ahmad, H.; Chen, G.; van der Mei, I.; Taylor, B.V.; Claflin, S.; Henson, G.J.; Simpson-Yap, S.; Laslett, L.L.; Hawkes, K.; et al. Validation of the EQ-5D-5L and psychosocial bolt-ons in a large cohort of people living with multiple sclerosis in Australia. Qual. Life Res. 2023, 32, 553–568. [Google Scholar] [CrossRef] [PubMed]
- Lin, D.-Y.; Cheok, T.S.; Samson, A.J.; Kaambwa, B.; Brown, B.; Wilson, C.; Kroon, H.M.; Jaarsma, R.L. A longitudinal validation of the EQ-5D-5L and EQ-VAS stand-alone component utilising the Oxford Hip Score in the Australian hip arthroplasty population. J. Patient-Rep. Outcomes 2022, 6, 71. [Google Scholar] [CrossRef] [PubMed]
- Orji, N.C.; Cox, I.A.; Jason, L.A.; Chen, G.; Zhao, T.; Rogerson, M.J.; Kelly, R.M.; Wills, K.; Hensher, M.; Palmer, A.J.; et al. Assessing health state utilities for people with myalgic encephalomyelitis/chronic fatigue syndrome in Australia using the EQ-5D-5L, AQoL-8D and EQ-5D-5L-psychosocial instruments. Qual. Life Res. 2023. [CrossRef]
- Cheng, Q.; Kularatna, S.; Lee, X.J.; Graves, N.; Pacella, R.E. Comparison of EQ-5D-5L and SPVU-5D for measuring quality of life in patients with venous leg ulcers in an Australian setting. Qual. Life Res. 2019, 28, 1903–1911. [Google Scholar] [CrossRef]
- Palacios-Cartagena, R.P.; Pastor-Cisneros, R.; Adsuar, J.C.; Pérez-Gómez, J.; García-Gordillo, M.Á.; Mendoza-Muñoz, M. CHU9D Normative Data in Peruvian Adolescents. J. Pers. Med. 2021, 11, 1272. [Google Scholar] [CrossRef]
- Calzada-Rodríguez, J.I.; Denche-Zamorano, M.; Pérez-Gómez, J.; Mendoza-Muñoz, M.; Carlos-Vivas, J.; Barrios-Fernandez, S.; Adsuar, J.C. Health-Related Quality of Life and Frequency of Physical Activity in Spanish Students Aged 8–14. Int. J. Environ. Res. Public Health 2021, 18, 9418. [Google Scholar] [CrossRef]
- Lindvall, K.; Vaezghasemi, M.; Feldman, I.; Ivarsson, A.; Stevens, K.J.; Petersen, S. Feasibility, reliability and validity of the health-related quality of life instrument Child Health Utility 9D (CHU9D) among school-aged children and adolescents in Sweden. Health Qual. Life Outcomes 2021, 19, 193. [Google Scholar] [CrossRef]
- Rowen, D.; Mulhern, B.; Stevens, K.; Vermaire, J.H. Estimating a Dutch value set for the pediatric preference-based CHU9D using a discrete choice experiment with duration. Value Health 2018, 21, 1234–1242. [Google Scholar] [CrossRef] [PubMed]
- Bashir, N.S.; Walters, T.D.; Griffiths, A.M.; Ungar, W.J. An Assessment of the Validity and Reliability of the Pediatric Child Health Utility 9D in Children with Inflammatory Bowel Disease. Children 2021, 8, 343. [Google Scholar] [CrossRef] [PubMed]
- Foster Page, L.A.; Thomson, W.M.; Marshman, Z.; Stevens, K.J. The potential of the Child Health Utility 9D Index as an outcome measure for child dental health. BMC Oral Health 2014, 14, 90. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rogers, H.J.; Vermaire, J.H.; Gilchrist, F.; Schuller, A.A. The Relationship between Caries-Specific Quality of Life and Generic Wellbeing in a Dutch Pediatric Population. Dent. J. 2019, 7, 67. [Google Scholar] [CrossRef]
- Petersen, K.D.; Ratcliffe, J.; Chen, G.; Serles, D.; Frøsig, C.S.; Olesen, A.V. The construct validity of the Child Health Utility 9D-DK instrument. Health Qual. Life Outcomes 2019, 17, 187. [Google Scholar] [CrossRef]
- Wolf, R.T.; Ratcliffe, J.; Chen, G.; Jeppesen, P. The longitudinal validity of proxy-reported CHU9D. Qual. Life Res. 2021, 30, 1747–1756. [Google Scholar] [CrossRef]
- Boyer, N.R.; Miller, S.; Connolly, P.; McIntosh, E. Paving the way for the use of the SDQ in economic evaluations of school-based population health interventions: An empirical analysis of the external validity of SDQ mapping algorithms to the CHU9D in an educational setting. Qual. Life Res. 2016, 25, 913–923. [Google Scholar] [CrossRef]
- Stevens, K. Valuation of the child health utility 9D index. Pharmacoeconomics 2012, 30, 729–747. [Google Scholar] [CrossRef]
- Ratcliffe, J.; Flynn, T.; Terlich, F.; Stevens, K.; Brazier, J.; Sawyer, M. Developing adolescent-specific health state values for economic evaluation: An application of profile case best-worst scaling to the Child Health Utility 9D. Pharmacoeconomics 2012, 30, 713–727. [Google Scholar] [CrossRef]
- Furber, G.; Segal, L. The validity of the Child Health Utility instrument (CHU9D) as a routine outcome measure for use in child and adolescent mental health services. Health Qual. Life Outcomes 2015, 13, 22. [Google Scholar] [CrossRef]
- Hayes, A.; Raghunandan, R.; Killedar, A.; Smith, S.; Cvejic, E.; Howell, M.; Petrou, S.; Lancsar, E.; Wong, G.; Craig, J.; et al. Reliability, acceptability, validity and responsiveness of the CHU9D and PedsQL in the measurement of quality of life in children and adolescents with overweight and obesity. Int. J. Obes. 2023, 47, 622–629. [Google Scholar] [CrossRef]
- Jones, R.; Mulhern, B.; Devlin, N.; O’loughlin, R.; Xiong, X.; Bahrampour, M.; McGregor, K.; Yip, S.; Hiscock, H.; Dalziel, K. PCR62 The Australian Paediatric Multi-Instrument Comparison (P-MIC) Study: Data Quality, Feasibility, Acceptability, and Construct Validity of the EQ-5D-Y-3L, EQ-5D-Y5L, CHU9D, PedsQL, HUI, PROMIS-25 and AQoL-6D. Value Health 2022, 25, S401–S402. [Google Scholar] [CrossRef]
- Chen, G.; Flynn, T.; Stevens, K.; Brazier, J.; Huynh, E.; Sawyer, M.; Ratcliffe, J. Assessing the health-related quality of life of Australian adolescents: An empirical comparison of the child health utility 9D and EQ-5D-Y instruments. Value Health 2015, 18, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Ratcliffe, J.; Huynh, E.; Chen, G.; Stevens, K.; Swait, J.; Brazier, J.; Flynn, T. Valuing the child health utility 9D: Using profile case best worst scaling methods to develop a new adolescent specific scoring algorithm. Soc. Sci. Med. 2016, 157, 48–59. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.Y.; Li, T.; Gong, F.H.; Zhang, J.S.; Li, X.K. Predictors of health-related quality of life and influencing factors for COVID-19 patients, a follow-up at one month. Front. Psychiatry 2020, 11, 668. [Google Scholar] [CrossRef] [PubMed]
- Fuerboeter, M.; Boettcher, J.; Barkmann, C.; Zapf, H.; Nazarian, R.; Wiegand-Grefe, S.; Boettcher, M. Quality of life and mental health of children with rare congenital surgical diseases and their parents during the COVID-19 pandemic. Orphanet J. Rare Dis. 2021, 16, 498. [Google Scholar] [CrossRef] [PubMed]
- Riiser, K.; Helseth, S.; Haraldstad, K.; Torbjørnsen, A.; Richardsen, K.R. Adolescents’ health literacy, health protective measures, and health-related quality of life during the COVID-19 pandemic. PLoS ONE 2020, 15, e0238161. [Google Scholar] [CrossRef]
- Canaway, A.G.; Frew, E.J. Measuring preference-based quality of life in children aged 6–7 years: A comparison of the performance of the CHU-9D and EQ-5D-Y—The WAVES Pilot Study. Qual. Life Res. 2013, 22, 173–183. [Google Scholar] [CrossRef]
- Chen, P.; Lin, K.C.; Liing, R.J.; Wu, C.Y.; Chen, C.L.; Chang, K.C. Validity, responsiveness, and minimal clinically important difference of EQ-5D-5L in stroke patients undergoing rehabilitation. Qual. Life Res. 2016, 25, 1585–1596. [Google Scholar] [CrossRef]
- Kaplan, R.M. The minimally clinically important difference in generic utility-based measures. COPD J. Chronic Obstr. Pulm. Dis. 2005, 2, 91–97. [Google Scholar] [CrossRef]
- McClure, N.S.; Al Sayah, F.; Xie, F.; Luo, N.; Johnson, J.A. Instrument-defined estimates of the minimally important difference for EQ-5D-5L index scores. Value Health 2017, 20, 644–650. [Google Scholar] [CrossRef] [PubMed]
- De Araújo, L.A.; Veloso, C.F.; de Campos Souza, M.; de Azevedo, J.M.C.; Tarro, G. The potential impact of the COVID-19 pandemic on child growth and development: A systematic review. J. Pediatr. 2020, 97, 369–377. [Google Scholar] [CrossRef] [PubMed]
- Westrupp, E.M.; Greenwood, C.J.; Fuller-Tyszkiewicz, M.; Olsson, C.A.; Sciberras, E.; Mikocka-Walus, A.; Wood, A.G. Parent and child mental health trajectories April 2020 to May 2021: Strict lockdown versus no lockdown in Australia. Aust. N. Z. J. Psychiatry 2021, 56, 1491–1502. [Google Scholar] [CrossRef] [PubMed]
- Guessoum, S.B.; Lachal, J.; Radjack, R.; Carretier, E.; Minassian, S.; Benoit, L.; Moro, M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2021, 291, 113264. [Google Scholar] [CrossRef]
- Babicki, M.; Malchrzak, W.; Hans-Wytrychowska, A.; Mastalerz-Migas, A. Impact of vaccination on the sense of security, the anxiety of COVID-19 and quality of life among polish. A nationwide online survey in Poland. Vaccines 2021, 9, 1444. [Google Scholar]
- Freund, O.; Tau, L.; Weiss, T.E.; Zornitzki, L.; Frydman, S.; Jacob, G.; Bornstein, G. Associations of vaccine status with characteristics and outcomes of hospitalized severe COVID-19 patients in the booster era. PLoS ONE 2022, 17, e0268050. [Google Scholar] [CrossRef]
- Bilge, Y.; Keles, E.; Baydili, K.N. The impact of COVID-19 vaccination on mental health. J. Loss Trauma 2022, 27, 285–288. [Google Scholar] [CrossRef]
- Webster, P. COVID-19 timeline of events. Nat. Med. 2021, 27, 2054–2055. [Google Scholar] [CrossRef]
- Gallè, F.; Sabella, E.A.; Ferracuti, S.; De Giglio, O.; Caggiano, G.; Protano, C.; Valeriani, F.; Parisi, E.A.; Valerio, G.; Liguori, G.; et al. Sedentary behaviors and physical activity of Italian undergraduate students during lockdown at the time of COVID−19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 6171. [Google Scholar] [CrossRef]
- Alkeridy, W.A.; Alquaydheb, H.; Almuhaidib, S.; Sindi, N.A.; Aljasser, A.; Kow, J.K.; Alqahtani, A.S. Determinants of Vaccine Hesitancy among Home Health Care Service Recipients in Saudi Arabia. Vaccines 2023, 11, 1436. [Google Scholar] [CrossRef]
- Kang, H.; Chung, I.-J.; Oh, S. Impact of the COVID-19 Pandemic on the Developmental Outcomes among Korean Kinship Foster Care Children: Gender Differences. Societie 2023, 13, 202. [Google Scholar] [CrossRef]
- Teng, C.-C.; Cheng, Y.-J.; Yen, W.-S.; Shih, P.-Y. COVID-19 Perceived Risk, Travel Risk Perceptions and Hotel Staying Intention: Hotel Hygiene and Safety Practices as a Moderator. Sustainability 2023, 15, 13048. [Google Scholar] [CrossRef]
- Ruotolo, F.; Ruggiero, G.; Cattaneo, Z.; Arioli, M.; Candini, M.; Frassinetti, F.; Pazzaglia, F.; Fornara, F.; Bosco, A.; Iachini, T. Psychological Reactions during and after a Lockdown: Self-Efficacy as a Protective Factor of Mental Health. Int. J. Environ. Res. Public Health 2023, 20, 6679. [Google Scholar] [CrossRef]
- Pietersma, S.; van den Akker-van, M.E.; de Vries, M. Generic quality of life utility measures in health-care research: Conceptual issues highlighted for the most commonly used utility measures. Int. J. Wellbeing 2013, 3, 2. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).