Sleep Quality as a Mediator of Burnout, Stress and Multisite Musculoskeletal Pain in Healthcare Workers: A Longitudinal Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Data Collection Instruments
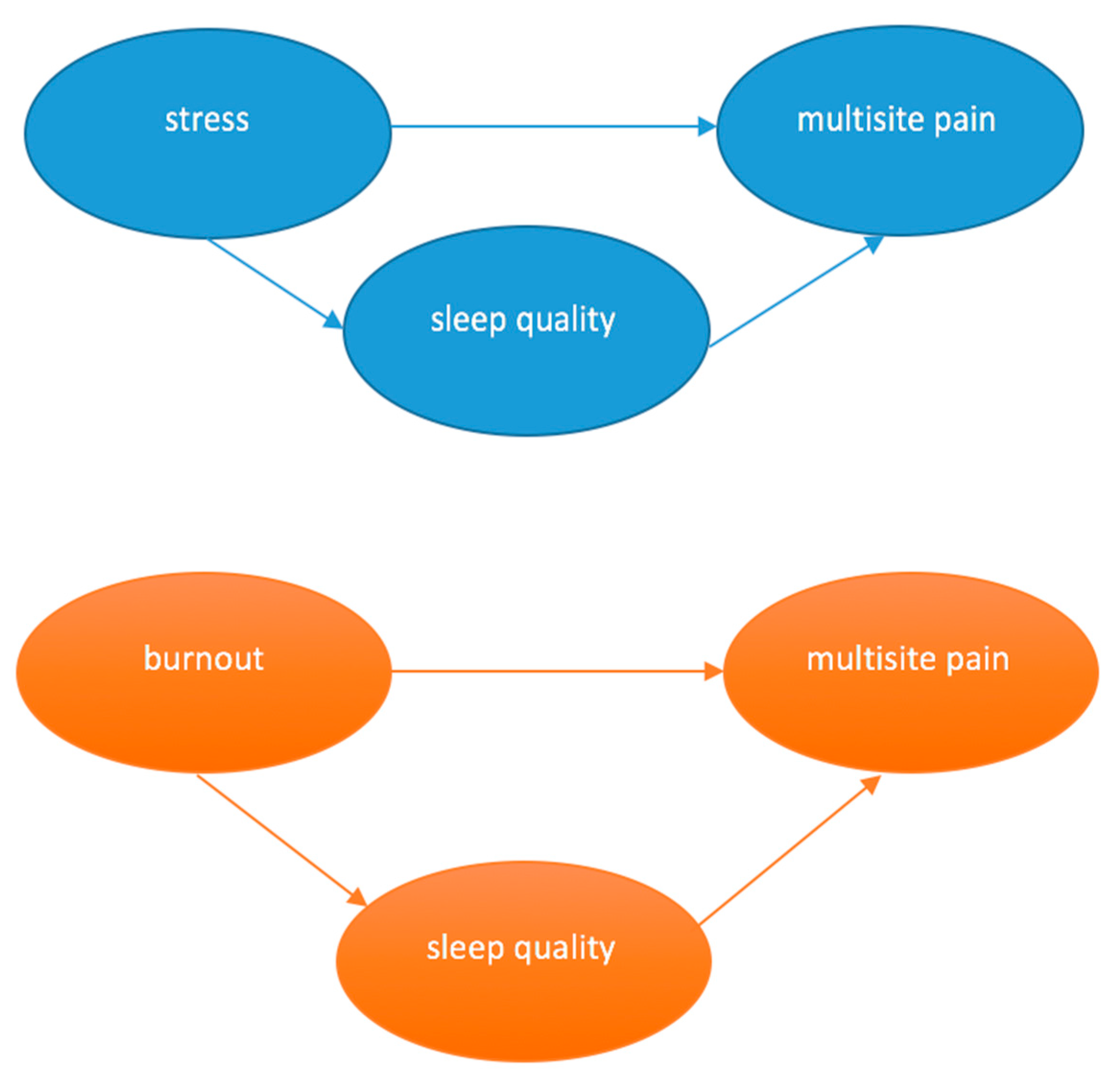
2.4. Data Analysis
3. Results
4. Discussion
Limitations and Strengths of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vittori, A.; Marinangeli, F.; Bignami, E.G.; Simonini, A.; Vergallo, A.; Fiore, G.; Petrucci, E.; Cascella, M.; Pedone, R. Analysis on burnout, job conditions, alexithymia, and other psychological symptoms in a sample of italian anesthesiologists and intensivists, assessed just before the COVID-19 pandemic: An AAROI-EMAC study. Healthcare 2022, 10, 1370. [Google Scholar] [CrossRef] [PubMed]
- Serrano-Ripoll, M.J.; Meneses-Echavez, J.F.; Ricci-Cabello, I.; Fraile-Navarro, D.; Fiol-deRoque, M.A.; Pastor-Moreno, G.; Castro, A.; Ruiz-Pérez, I.; Zamanillo Campos, R.; Gonçalves-Bradley, D.C. Impact of viral epidemic outbreaks on mental health of healthcare workers: A rapid systematic review and meta-analysis. J. Affect. Disord. 2020, 277, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Edú-Valsania, S.; Laguía, A.; Moriano, J.A. Burnout: A review of theory and measurement. Int. J. Environ. Res. Public Health 2022, 19, 1780. [Google Scholar] [CrossRef] [PubMed]
- Danhof-Pont, M.B.; van Veen, T.; Zitman, F.G. Biomarkers in burnout: A systematic review. J. Psychosom. Res. 2011, 70, 505–524. [Google Scholar] [CrossRef]
- Kärkkäinen, R.; Saaranen, T.; Hiltunen, S.; Ryynänen, O.P.; Räsänen, K. Systematic review: Factors associated with return to work in burnout. Occup. Med. 2017, 67, 461–468. [Google Scholar] [CrossRef]
- Pacheco, J.P.; Giacomin, H.T.; Tam, W.W.; Ribeiro, T.B.; Arab, C.; Bezerra, I.M.; Pinasco, G.C. Mental health problems among medical students in Brazil: A systematic review and meta-analysis. Braz. J. Psychiatry 2017, 39, 369–378. [Google Scholar] [CrossRef]
- Usas, H.; Weilenmann, S.; Princip, M.; Fuchs, W.J.; van Nuffel, M.; von Känel, R.; Spiller, T.R. Physician-specific symptoms of burnout compared to a non-physicians group. Int. J. Environ. Res. Public Health 2023, 20, 2693. [Google Scholar] [CrossRef]
- Busch, I.M.; Moretti, F.; Mazzi, M.; Wu, A.W.; Rimondini, M. What We Have Learned from Two Decades of Epidemics and Pandemics: A Systematic Review and Meta-Analysis of the Psychological Burden of Frontline Healthcare Workers. Psychother. Psychosom. 2021, 90, 178–190. [Google Scholar] [CrossRef]
- Dantzer, R. Stress theories and the somatization process. L’encephale 1995, 21, 3–9. [Google Scholar]
- ILO 2016. International Labour Organization 2016. Available online: https://www.ilo.org/wcmsp5/groups/public/---ed_protect/---protrav/---safework/documents/publication/wcms_466547.pdf (accessed on 19 July 2023).
- Appiani, F.J.; Cairoli, F.R.; Sarotto, L.; Yaryour, C.; Basile, M.E.; Duarte, J.M. Prevalence of stress, burnout syndrome, anxiety and depression among physicians of a teaching hospital during the COVID-19 pandemic. Arch. Argent. Pediatr. 2021, 119, 317–324. [Google Scholar] [CrossRef]
- Prasad, K.; McLoughlin, C.; Stillman, M.; Poplau, S.; Goelz, E.; Taylor, S.; Nankivil, N.; Brown, R.; Linzer, M.; Cappelucci, K.; et al. Prevalence and correlates of stress and burnout among U.S. healthcare workers during the COVID-19 pandemic: A national cross-sectional survey study. eClinicalMedicine 2021, 35, 100879. [Google Scholar] [CrossRef] [PubMed]
- Akova, I.; Kiliç, E.; Özdemir, M.E. Prevalence of Burnout, Depression, Anxiety, Stress, and Hopelessness Among Healthcare Workers in COVID-19 Pandemic in Turkey. Inq. J. Health Care Organ. Provis. Financ. 2022, 59, 469580221079684. [Google Scholar] [CrossRef] [PubMed]
- de Medeiros, A.I.C.; de Mesquita, R.B.; Macêdo, F.D.S.; Matos, A.G.D.C.; Pereira, E.D. Prevalence of burnout among healthcare workers in six public referral hospitals in northeastern Brazil during the COVID-19 pandemic: A cross-sectional study. Sao Paulo Med. J. 2022, 140, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Pappa, S.; Athanasiou, N.; Sakkas, N.; Patrinos, S.; Sakka, E.; Barmparessou, Z.; Tsikrika, S.; Adraktas, A.; Pataka, A.; Migdalis, I.; et al. From Recession to Depression? Prevalence and Correlates of Depression, Anxiety, Traumatic Stress and Burnout in Healthcare Workers during the COVID-19 Pandemic in Greece: A Multi-Center, Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 2390. [Google Scholar] [CrossRef]
- Chen, Y.-H.; Yeh, C.-J.; Lee, C.-M.; Jong, G.-P. Mediation Effect of Musculoskeletal Pain on Burnout: Sex-Related Differences. Int. J. Environ. Res. Public Health 2022, 19, 12872. [Google Scholar] [CrossRef] [PubMed]
- Hämmig, O. Work- and stress-related musculoskeletal and sleep disorders among health professionals: A cross-sectional study in a hospital setting in Switzerland. BMC Musculoskelet. Disord. 2020, 21, 319. [Google Scholar] [CrossRef]
- Nguyen, T.H.; Hoang, D.L.; Hoang, T.G.; Pham, M.K.; Bodin, J.; Dewitte, J.D.; Roquelaure, Y. Prevalence and Characteristics of Multisite Musculoskeletal Symptoms among District Hospital Nurses in Haiphong, Vietnam. BioMed Res. Int. 2020, 2020, 3254605. [Google Scholar] [CrossRef]
- Epstein, S.; Sparer, E.H.; Tran, B.N.; Ruan, Q.Z.; Dennerlein, J.T.; Singhal, D.; Lee, B.T. Prevalence of Work-Related Musculoskeletal Disorders Among Surgeons and Interventionalists: A systematic review and meta-analysis. JAMA Surg. 2018, 153, e174947. [Google Scholar] [CrossRef]
- Dalager, T.; Søgaard, K.; Boyle, E.; Jensen, P.T.; Mogensen, O. Surgery Is Physically Demanding and Associated With Multisite Musculoskeletal Pain: A Cross-Sectional Study. J. Surg. Res. 2019, 240, 30–39. [Google Scholar] [CrossRef]
- dos Santos, E.C.; Andrade, R.D.; Lopes, S.G.R.; Valgas, C. Prevalence of musculoskeletal pain in nursing professionals working in orthopedic setting. Rev. Dor 2017, 18, 298–306. [Google Scholar] [CrossRef]
- Salvagioni, D.A.J.; Melanda, F.N.; Mesas, A.E.; González, A.D.; Gabani, F.L.; De Andrade, S.M. Physical, psychological and occupational consequences of job burnout: A systematic review of prospective studies. PLoS ONE 2017, 12, e0185781. [Google Scholar] [CrossRef] [PubMed]
- Grossi, G.; Perski, A.; Osika, W.; Savic, I. Stress-related exhaustion disorder—Clinical manifestation of burnout? A review of assessment methods, sleep impairments, cognitive disturbances, and neuro-biological and physiological changes in clinical burnout. Scand. J. Psychol. 2015, 56, 626–636. [Google Scholar] [CrossRef] [PubMed]
- Ekstedt, M.; Söderström, M.; Åkerstedt, T. Sleep physiology in recovery from burnout. Biol. Psychol. 2009, 82, 267–273. [Google Scholar] [CrossRef]
- Yella, T.; Dmello, M.K. Burnout and sleep quality among community health workers during the pandemic in selected city of Andhra Pradesh. Clin. Epidemiol. Glob. Health 2022, 16, 101109. [Google Scholar] [CrossRef]
- Stimpfel, A.W.; Goldsamt, L.; Liang, E.; Costa, D.K. Work Organization Factors Associated With Nurses’ Stress, Sleep, and Performance: A Pre-pandemic Analysis. J. Nurs. Regul. 2022, 13, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Zarei, S.; Fooladvand, K. Mediating effect of sleep disturbance and rumination on work-related burnout of nurses treating patients with coronavirus disease. BMC Psychol. 2022, 10, 197. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.J.; Wehrlen, L.; Ding, Y.; Ross, A. Professional quality of life, sleep disturbance and health among nurses: A mediation analysis. Nurs. Open 2021, 9, 2771–2780. [Google Scholar] [CrossRef]
- Matre, D.; Nilsen, K.B.; Katsifaraki, M.; Waage, S.; Pallesen, S.; Bjorvatn, B. Pain complaints are associated with quick returns and insomnia among Norwegian nurses, but do not differ between shift workers and day only workers. Int. Arch. Occup. Environ. Health 2020, 93, 291–299. [Google Scholar] [CrossRef]
- Dong, H.; Zhang, Q.; Zhang, Z.; Zhu, C. Association of sleep disturbance with shift work, occupational stress, and musculoskeletal pain in Chinese public hospital emergency workers: A multicentre cross-sectional study. Chronobiol. Int. 2022, 39, 886–894. [Google Scholar] [CrossRef]
- AlHamam, N.M.; Buhalim, R.A.; AlSaeed, M.N.; AlFuraikh, B.F.; AlJughaiman, M.S. Low back pain and its correlations with poor sleep quality among health care providers. J. Taibah Univ. Med. Sci. 2021, 17, 28–37. [Google Scholar] [CrossRef]
- Chin, W.; Chen, Y.; Lin, T.; Guo, Y.L.; Shiao, J.S.C. Short sleep and chronic neck and shoulder discomfort in nurses. J. Occup. Health 2021, 63, e12236. [Google Scholar] [CrossRef] [PubMed]
- Garnæs, K.K.; Mørkved, S.; Tønne, T.; Furan, L.; Vasseljen, O.; Johannessen, H.H. Mental health among patients with chronic musculoskeletal pain and its relation to number of pain sites and pain intensity, a cross-sectional study among primary health care patients. BMC Musculoskelet. Disord. 2022, 23, 1115. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis a Regression-Based Approach, 3rd ed.; Guilford Press: London, UK, 2022. [Google Scholar]
- Liu, J.; Ulrich, C. Mediation analysis in nursing research: A methodological review. Contemp. Nurse 2016, 52, 643–656. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, R.R.N.; Cashin, A.G.; Bagg, M.K.; Gustin, S.M.; Lee, H.; McAuley, J.H. A Systematic Review of the Reporting Quality of Observational Studies That Use Mediation Analyses. Prev. Sci. 2022, 23, 1041–1052. [Google Scholar] [CrossRef]
- Koch, P.; Schablon, A.; Latza, U.; Nienhaus, A. Musculoskeletal pain and effort-reward imbalance—A systematic review. BMC Public Health 2014, 14, 37. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M.; Strobe Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. PLoS Med. 2007, 4, e297. [Google Scholar] [CrossRef]
- Sato, T.D.O.; de Faria, B.S.F.; Albuquerque, B.B.; da Silva, F.L.; Rohwedder, L.S.; de Azevedo, R.T.; Gonçalves, J.S.; Vieira, L.M.S.M.D.A.; Triches, M.I.; de Sousa, R.A.; et al. Poor Health Conditions among Brazilian Healthcare Workers: The Study Design and Baseline Characteristics of the HEROES Cohort. Healthcare 2022, 10, 2096. [Google Scholar] [CrossRef]
- Gonçalves, J.S.; Moriguchi, C.S.; Chaves, T.C.; Sato, T.D.O. Cross-cultural adaptation and psychometric properties of the short version of COPSOQ II-Brazil. Rev. Saúde Públ. 2021, 55, 69. [Google Scholar] [CrossRef]
- Kristensen, T.S.; Hannerz, H.; Høgh, A.; Borg, V. The Copenhagen Psychosocial Questionnaire—A tool for the assessment and improvement of the psychosocial work environment. Scand. J. Work Environ. Health 2005, 31, 438–449. [Google Scholar] [CrossRef]
- Pejtersen, J.H.; Søndergå, T.; Kristensen, R.D.; Borg, V.; Bjorner, J.B. The second version of the Copenhagen Psychosocial Questionnaire. Scand. J. Public Health 2010, 38, 8–24. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef] [PubMed]
- Bertolazi, A.N.; Fagondes, S.C.; Hoff, L.S.; Dartora, E.G.; Miozzo, I.C.D.S.; de Barba, M.E.F.; Barreto, S.S.M. Validation of the Brazilian Portuguese version of the Pittsburgh Sleep Quality Index. Sleep Med. 2011, 12, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sørensen, F.; Andersson, G.; Jørgensen, K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- De Barros, E.N.C.; Alexandre, N.M.C. Cross-cultural adaptation of the Nordic musculoskeletal questionnaire. Int. Nurs. Rev. 2003, 50, 101–108. [Google Scholar] [CrossRef]
- Fritz, M.S.; MacKinnon, D.P. Required Sample Size to Detect the Mediated Effect. Psychol. Sci. 2007, 18, 233–239. [Google Scholar] [CrossRef]
- Crofford, L.J. Chronic Pain: Where the Body Meets the Brain. Trans. Am. Clin. Climatol. Assoc. 2015, 126, 167–183. [Google Scholar]
- Membrive-Jiménez, M.J.; Gómez-Urquiza, J.L.; Suleiman-Martos, N.; Velando-Soriano, A.; Ariza, T.; De la Fuente-Solana, E.I.; la Fuente, G.A.C.-D. Relation between Burnout and Sleep Problems in Nurses: A Systematic Review with Meta-Analysis. Healthcare 2022, 10, 954. [Google Scholar] [CrossRef]
- Vidotti, V.; Ribeiro, R.P.; Galdino, M.J.Q.; Martins, J.T. Burnout Syndrome and shift work among the nursing staff. Rev. Latino-Am. Enferm. 2018, 26, e3022. [Google Scholar] [CrossRef] [PubMed]
- Waich, A.; Barahona-Correa, J.E.; Figueredo, M.D.C.; Rondón-Sepúlveda, M.A.; Ruiz, A.J.; Castellanos, J.C.; Hidalgo-Martínez, P. Sleep Quality, Insomnia, and Perceived Stress among Colombian Healthcare Workers during the COVID-19 Pandemic. Sleep Sci. 2023, 16, 44–50. [Google Scholar] [CrossRef]
- Danet, A.D. Psychological impact of COVID-19 pandemic in Western frontline healthcare professionals. A systematic review. Med. Clin. 2021, 156, 449–458. [Google Scholar] [CrossRef]
- Qin, A.; Hu, F.; Qin, W.; Dong, Y.; Li, M.; Xu, L. Educational degree differences in the association between work stress and depression among Chinese healthcare workers: Job satisfaction and sleep quality as the mediators. Front. Public Health 2023, 11, 1138380. [Google Scholar] [CrossRef] [PubMed]
- Jahrami, H.; Haji, E.A.; Saif, Z.Q.; Aljeeran, N.O.; Aljawder, A.I.; Shehabdin, F.N.; Fekih-Romdhane, F.; Trabelsi, K.; BaHammam, A.S.; Vitiello, M.V. Sleep Quality Worsens While Perceived Stress Improves in Healthcare Workers over Two Years during the COVID-19 Pandemic: Results of a Longitudinal Study. Healthcare 2022, 10, 1588. [Google Scholar] [CrossRef]
- Dragioti, E.; Li, H.; Tsitsas, G.; Lee, K.H.; Choi, J.; Kim, J.; Choi, Y.J.; Tsamakis, K.; Estradé, A.; Agorastos, A.; et al. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J. Med. Virol. 2022, 94, 1935–1949. [Google Scholar] [CrossRef] [PubMed]
- Dzierzewski, J.M.; Williams, J.M.; Roditi, D.; Marsiske, M.; McCoy, K.; McNamara, J.; Dautovich, N.; Robinson, M.E.; McCrae, C.S. Daily Variations in Objective Nighttime Sleep and Subjective Morning Pain in Older Adults with Insomnia: Evidence of Covariation over Time. J. Am. Geriatr. Soc. 2010, 58, 925–930. [Google Scholar] [CrossRef]
- Finan, P.H.; Goodin, B.R.; Smith, M.T. The Association of Sleep and Pain: An Update and a Path Forward. J. Pain 2013, 14, 1539–1552. [Google Scholar] [CrossRef]
- Lautenbacher, S.; Kundermann, B.; Krieg, J.-C. Sleep deprivation and pain perception. Sleep Med. Rev. 2006, 10, 357–369. [Google Scholar] [CrossRef] [PubMed]
- Vgontzas, A.N.; Zoumakis, E.; Bixler, E.O.; Lin, H.-M.; Follett, H.; Kales, A.; Chrousos, G.P. Adverse Effects of Modest Sleep Restriction on Sleepiness, Performance, and Inflammatory Cytokines. J. Clin. Endocrinol. Metab. 2004, 89, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S. Protective and damaging effects of stress mediators: Central role of the brain. Dialogues Clin. Neurosci. 2006, 8, 367–381. [Google Scholar] [CrossRef]
- Lisman, P.; Ritland, B.M.; Burke, T.M.; Sweeney, L.; A Dobrosielski, D. The Association Between Sleep and Musculoskeletal Injuries in Military Personnel: A Systematic Review. Mil. Med. 2022, 187, 1318–1329. [Google Scholar] [CrossRef]
- Lindell, M.; Grimby-Ekman, A. Stress, non-restorative sleep, and physical inactivity as risk factors for chronic pain in young adults: A cohort study. PLoS ONE 2022, 17, e0262601. [Google Scholar] [CrossRef]
- Walton, D.M.; Pourkazemi, F.; Ghodrati, M.; Elliott, J.M. A Mediational Analysis of Stress, Inflammation, Sleep, and Pain in Acute Musculoskeletal Trauma. Clin. J. Pain 2020, 36, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Hess, A.; Porter, M.; Byerly, S. Environmental Factors Impacting Wellness in the Trauma Provider. Curr. Trauma Rep. 2023, 9, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Elfering, A.; Kottwitz, M.U.; Tamcan, Ö.; Müller, U.; Mannion, A.F. Impaired sleep predicts onset of low back pain and burnout symptoms: Evidence from a three-wave study. Psychol. Health Med. 2018, 23, 1196–1210. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total | No Pain/Single-Site Pain (n = 24) | Multisite Pain (n = 101) | p |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Age, years 1 | 37.5 (8.3) | 39.6 (9.0) | 36.9 (8.1) | 0.16 |
| Sex | 0.07 | |||
| female | 104 (83.2) | 17 (70.8) | 87 (86.1) | |
| male | 21 (16.8) | 7 (29.2) | 14 (13.9) | |
| Marital status | 0.87 | |||
| single/widower/divorced | 54 (43.2) | 10 (41.7) | 44 (43.6) | |
| married/with a partner | 71 (56.8) | 14 (58.3) | 57 (56.4) | |
| Education level | 0.50 | |||
| Primary/high school education | 25 (20.0) | 6 (25.0) | 19 (18.8) | |
| University | 100 (80.0) | 18 (75.0) | 82 (81.2) | |
| Use medication | 83 (66.4) | 16 (66.7) | 67 (66.3) | 0.98 |
| Smoke | 14 (11.2) | 3 (12.5) | 11 (10.9) | 0.82 |
| Occupation | 0.07 | |||
| nurse | 45 (36.0) | 9 (37.5) | 36 (35.6) | |
| nurse technician/auxiliary | 28 (22.4) | 4 (16.7) | 24 (23.80 | |
| physical therapist | 26 (20.8) | 2 (8.3) | 24 (23.8) | |
| physician | 8 (6.4) | 3 (12.5) | 5 (5.0) | |
| dentist | 4 (3.2) | 0 (0.0) | 4 (4.0) | |
| other | 14 (11.2) | 6 (25.0) | 8 (7.9) | |
| Workplace | 0.39 | |||
| primary care | 40 (32.0) | 7 (29.2) | 33 (32.7) | |
| hospital | 61 (48.8) | 9 (37.5) | 52 (51.5) | |
| emergency care | 12 (9.6) | 5 (20.8) | 7 (6.9) | |
| ambulatorial care | 4 (3.2) | 1 (4.2) | 3 (3.0) | |
| psychosocial care | 5 (4.0) | 1 (4.2) | 4 (4.0) | |
| home care | 3 (2.4) | 1 (4.2) | 2 (2.0) | |
| Weekly working hours | 0.65 | |||
| up to 30 h | 36 (28.8) | 6 (16.7) | 18 (20.2) | |
| more than 30 h | 89 (71.2) | 30 (83.3) | 71 (79.8) | |
| Burnout (0–8 points) 1 | 5.3 (1.8) | 3.9 (1.3) | 5.6 (1.8) | <0.01 |
| Stress (0–8 points) 1 | 4.9 (1.9) | 3.6 (1.3) | 5.3 (1.8) | <0.01 |
| Pittsburg Sleep Quality Index (PSQI) Components | Total | No Pain/Single-Site Pain (n = 24) | Multisite Pain (n = 101) | p |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Subjective sleep quality | <0.01 | |||
| very good | 13 (10.4) | 4 (16.7) | 9 (8.9) | |
| fairly good | 60 (48.0) | 18 (75.0) | 42 (41.6) | |
| fairly bad | 38 (30.4) | 2 (8.3) | 36 (35.6) | |
| very bad | 14 (11.2) | 0 (0.0) | 14 (13.9) | |
| Sleep latency | <0.01 | |||
| 0 | 16 (12.8) | 5 (20.8) | 11 (10.9) | |
| 1 | 49 (39.2) | 16 (66.7) | 33 (32.7) | |
| 2 | 29 (23.2) | 2 (8.3) | 27 (26.7) | |
| 3 | 31 (24.8) | 1 (4.2) | 30 (29.7) | |
| Sleep duration | 0.21 | |||
| >7 h | 33 (26.4) | 10 (41.7) | 23 (22.8) | |
| 6–7 h | 35 (28.0) | 6 (25.0) | 29 (28.7) | |
| 5–6 h | 33 (26.4) | 6 (25.0) | 27 (26.7) | |
| <5 h | 24 (19.2) | 2 (8.3) | 22 (21.80 | |
| Habitual sleep efficiency | 0.11 | |||
| >85% | 77 (61.6) | 20 (83.3) | 57 (56.4) | |
| 75–84% | 24 (19.2) | 2 (8.3) | 22 (21.8) | |
| 65–74% | 10 (8.0) | 1 (4.2) | 9 (8.9) | |
| <65% | 14 (11.2) | 1 (4.2) | 13 (12.9) | |
| Sleep disturbances | 0.03 | |||
| 0 | 1 (0.8) | 1 (4.2) | 0 (0.0) | |
| 1 | 55 (44.0) | 15 (62.5) | 40 (39.6) | |
| 2 | 57 (45.6) | 7 (29.2) | 50 (49.5) | |
| 3 | 12 (9.6) | 1 (4.2) | 11 (10.9) | |
| Use of sleeping medication | 0.05 | |||
| none | 82 (65.6) | 20 (83.3) | 62 (61.4) | |
| less than once a week | 17 (13.6) | 4 (16.7) | 13 (12.9) | |
| once or twice a week | 9 (7.2) | 0 (0.0) | 9 (8.9) | |
| 3 or more times a week | 17 (13.6) | 0 (0.0) | 17 (16.8) | |
| Daytime dysfunction | 0.02 | |||
| 0 | 17 (13.6) | 7 (29.2) | 10 (9.9) | |
| 1 | 55 (44.0) | 12 (50.0) | 43 (42.6) | |
| 2 | 42 (33.6) | 3 (12.5) | 39 (38.6) | |
| 3 | 11 (8.8) | 2 (8.3) | 9 (8.9) | |
| PSQI score 1 | 8.80 (4.14) | 5.67 (2.41) | 9.54 (4.13) | <0.01 |
| PSQI category | <0.01 | |||
| good sleepers | 32 (25.6) | 12 (50.0) | 20 (19.8) | |
| bad sleepers | 93 (74.4) | 12 (50.0) | 81 (80.2) |
| Number of Pain Sites | Baseline n = 125 | 3 Months n = 80 | 6 Months n = 65 | 9 Months n = 63 | 12 Months n = 61 |
|---|---|---|---|---|---|
| Last 12 months | n (%) | n (%) | n (%) | n (%) | n (%) |
| 0 | 14 (11.2) | 4 (5.0) | 5 (7.7) | 6 (9.5) | 10 (16.4) |
| 1 | 10 (8.0) | 4 (5.0) | 4 (6.2) | 7 (11.1) | 4 (6.6) |
| 2 | 13 (10.4) | 10 (12.5) | 10 (15.4) | 4 (6.3) | 8 (13.1) |
| 3 | 12 (9.6) | 11 (13.8) | 6 (9.2) | 9 (14.3) | 11 (18.0) |
| 4 | 21 (16.8) | 17 (21.3) | 18 (27.7) | 9 (14.3) | 9 (14.8) |
| 5 | 22 (17.6) | 9 (11.3) | 9 (13.8) | 10 (15.9) | 7 (11.5) |
| 6 | 13 (10.4) | 9 (11.3) | 6 (9.2) | 8 (12.7) | 6 (9.8) |
| 7 | 11 (8.8) | 8 (10.0) | 4 (6.2) | 3 (4.8) | 2 (3.3) |
| 8 | 7 (5.6) | 8 (10.0) | 2 (3.1) | 5 (7.9) | 4 (6.6) |
| 9 | 2 (1.6) | - | 1 (1.5) | 2 (3.2) | - |
| Last 7 days | |||||
| 0 | 35 (28.0) | 29 (36.3) | 22 (33.8) | 22 (34.9) | 22 (36.1) |
| 1 | 27 (21.6) | 12 (15.0) | 17 (26.2) | 13 (20.6) | 16 (26.2) |
| 2 | 19 (15.2) | 14 (17.5) | 9 (13.8) | 12 (19.0) | 10 (16.4) |
| 3 | 19 (15.2) | 11 (13.8) | 5 (7.7) | 7 (11.1) | 5 (8.2) |
| 4 | 12 (9.6) | 7 (8.8) | 9 (13.8) | 3 (4.8) | 2 (3.3) |
| 5 | 7 (5.6) | 3 (3.8) | 2 (3.1) | 5 (7.9) | 2 (3.3) |
| 6 | 3 (2.4) | 1 (1.3) | 1 (1.5) | - | 2 (3.3) |
| 7 | 3 (2.4) | 2 (2.5) | - | - | - |
| 8 | - | 1 (1.3) | - | 1 (1.6) | 2 (3.3) |
| 9 | - | - | - | - | - |
| Predictor: Burnout | Burnout–Pain (c) | Burnout–Sleep (a) | Sleep–Pain (b) | Burnout–Sleep–Pain (c’) |
|---|---|---|---|---|
| Pain in the last 12 months | ||||
| baseline (n = 125) | ||||
| mediated effect | 20.4% | |||
| b | 0.65 | 1.19 | 0.11 | 0.52 |
| 95% CI | 0.44–0.86 | 0.84–1.54 | 0.01–0.21 | 0.28–0.76 |
| R2 | 24% | 27% | 26% | 26% |
| p | <0.01 | <0.01 | 0.04 | <0.01 |
| 3 months (n = 80) | ||||
| mediated effect | 14.8% | |||
| b | 0.65 | 1.32 | 0.07 | 0.56 |
| 95% CI | 0.42–0.88 | 0.87–1.76 | −0.05–0.19 | 0.28–0.84 |
| R2 | 29% | 31% | 30% | 30% |
| p | <0.01 | <0.01 | 0.24 | <0.01 |
| 6 months (n = 65) | ||||
| mediated effect | 19.3% | |||
| b | 0.69 | 1.35 | 0.10 | 0.56 |
| 95% CI | 0.44–0.94 | 0.82–1.88 | −0.02–0.21 | 0.27–0.85 |
| R2 | 33% | 29% | 36% | 36% |
| p | <0.01 | <0.01 | 0.10 | <0.01 |
| 9 months (n = 63) | ||||
| mediated effect | 13.6% | |||
| b | 0.75 | 1.19 | 0.08 | 0.66 |
| 95% CI | 0.48–1.01 | 0.72–1.66 | −0.07–0.22 | 0.34–0.97 |
| R2 | 34% | 29% | 36% | 36% |
| p | <0.01 | <0.01 | 0.29 | <0.01 |
| 12 months (n = 61) | ||||
| mediated effect | 18.6% | |||
| b | 0.74 | 1.24 | 0.11 | 0.60 |
| 95% CI | 0.48–1.00 | 0.75–1.73 | −0.02–0.25 | 0.29–0.90 |
| R2 | 35% | 30% | 38% | 38% |
| p | <0.01 | <0.01 | 0.10 | <0.01 |
| Pain in the last 7 days | ||||
| baseline (n = 125) | ||||
| b | 0.48 | 1.19 | 0.02 | 0.45 |
| 95% CI | 0.32–0.64 | 0.84–1.54 | −0.06–0.11 | 0.26–0.64 |
| R2 | 22% | 27% | 22% | 22% |
| p | <0.01 | <0.01 | 0.55 | <0.01 |
| 3 months (n = 80) | ||||
| b | 0.35 | 1.32 | −0.01 | 0.35 |
| 95% CI | 0.12–0.57 | 0.87–1.76 | −0.12–0.11 | 0.08–0.63 |
| R2 | 11% | 31% | 11% | 11% |
| p | <0.01 | <0.01 | 0.92 | <0.01 |
| 6 months (n = 65) | ||||
| b | 0.31 | 1.35 | 0.03 | 0.27 |
| 95% CI | 0.09–0.53 | 0.82–1.88 | −0.08–0.13 | 0.01–0.53 |
| R2 | 11% | 29% | 11% | 11% |
| p | 0.01 | <0.01 | 0.62 | 0.04 |
| 9 months (n = 63) | ||||
| b | 0.29 | 1.19 | 0.07 | 0.21 |
| 95% CI | 0.07–0.51 | 0.72–1.66 | −0.05–0.19 | −0.05–0.47 |
| R2 | 10% | 29% | 12% | 12% |
| p | 0.01 | <0.01 | 0.26 | 0.12 |
| 12 months (n = 61) | ||||
| b | 0.40 | 1.24 | 0.03 | 0.36 |
| 95% CI | 0.15–0.65 | 0.75–1.73 | −0.11–0.16 | 0.06–0.66 |
| R2 | 15% | 30% | 15% | 15% |
| p | <0.01 | <0.01 | 0.68 | 0.02 |
| Predictor: Stress | Stress–Pain (c) | Stress–Sleep (a) | Sleep–Pain (b) | Stress–Sleep–Pain (c’) |
|---|---|---|---|---|
| Pain in the last 12 months | ||||
| baseline (n = 125) | ||||
| mediated effect | 27.0% | |||
| b | 0.54 | 1.01 | 0.15 | 0.40 |
| 95% CI | 0.33–0.75 | 0.66–1.37 | 0.04–0.25 | 0.17–0.63 |
| R2 | 18% | 20% | 23% | 23% |
| p | <0.01 | <0.01 | <0.01 | <0.01 |
| 3 months (n = 80) | ||||
| mediated effect | 25.0% | |||
| b | 0.56 | 1.23 | 0.12 | 0.41 |
| 95% CI | 0.30–0.81 | 0.75–1.71 | 0.01–0.24 | 0.12–0.70 |
| R2 | 19% | 25% | 23% | 23% |
| p | <0.01 | <0.01 | 0.05 | 0.01 |
| 6 months (n = 65) | ||||
| mediated effect | 21.8% | |||
| b | 0.69 | 1.32 | 0.11 | 0.54 |
| 95% CI | 0.42–0.95 | 0.76–1.89 | 0.00–0.23 | 0.24–0.84 |
| R2 | 30% | 26% | 34% | 34% |
| p | <0.01 | <0.01 | 0.05 | <0.01 |
| 9 months (n = 63) | ||||
| mediated effect | 26.1% | |||
| b | 0.62 | 1.16 | 0.14 | 0.45 |
| 95% CI | 0.31–0.92 | 0.65–1.67 | −0.01–0.29 | 0.11–0.80 |
| R2 | 21% | 26% | 25% | 25% |
| p | <0.01 | <0.01 | 0.07 | 0.01 |
| 12 months (n = 61) | ||||
| mediated effect | 30.6% | |||
| b | 0.64 | 1.21 | 0.17 | 0.44 |
| 95% CI | 0.34–0.94 | 0.67–1.74 | 0.03–0.31 | 0.11–0.77 |
| R2 | 24% | 26% | 31% | 31% |
| p | <0.01 | <0.01 | 0.02 | 0.01 |
| Pain in the last 7 days | ||||
| baseline (n = 125) | ||||
| b | 0.39 | 1.01 | 0.06 | 0.33 |
| 95% CI | 0.23–0.55 | 0.66–1.37 | −0.02–0.14 | 0.15–0.51 |
| R2 | 15% | 20% | 17% | 17% |
| p | <0.01 | <0.01 | 0.16 | <0.01 |
| 3 months (n = 80) | ||||
| b | 0.21 | 1.23 | 0.05 | 0.15 |
| 95% CI | −0.03–0.45 | 0.75–1.71 | −0.07–0.16 | −0.13–0.43 |
| R2 | 4% | 25% | 5% | 5% |
| p | 0.09 | <0.01 | 0.42 | 0.28 |
| 6 months (n = 65) | ||||
| b | 0.34 | 1.32 | 0.02 | 0.31 |
| 95% CI | 0.11–0.57 | 0.76–1.89 | −0.08–0.13 | 0.04–0.57 |
| R2 | 12% | 26% | 13% | 13% |
| p | <0.01 | <0.01 | 0.63 | 0.02 |
| 9 months (n = 63) | ||||
| b | 0.24 | 1.16 | 0.09 | 0.14 |
| 95% CI | 0.01–0.48 | 0.65–1.67 | −0.03–0.21 | −0.13–0.41 |
| R2 | 7% | 26% | 10% | 10% |
| p | 0.04 | <0.01 | 0.14 | 0.30 |
| 12 months (n = 61) | ||||
| b | 0.43 | 1.21 | 0.04 | 0.38 |
| 95% CI | 0.16–0.69 | 0.67–1.74 | −0.09–0.16 | 0.08–0.69 |
| R2 | 15% | 26% | 16% | 16% |
| p | <0.01 | <0.01 | 0.59 | 0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vieira, L.M.S.M.d.A.; Mininel, V.A.; Sato, T.d.O. Sleep Quality as a Mediator of Burnout, Stress and Multisite Musculoskeletal Pain in Healthcare Workers: A Longitudinal Study. Healthcare 2023, 11, 2476. https://doi.org/10.3390/healthcare11182476
Vieira LMSMdA, Mininel VA, Sato TdO. Sleep Quality as a Mediator of Burnout, Stress and Multisite Musculoskeletal Pain in Healthcare Workers: A Longitudinal Study. Healthcare. 2023; 11(18):2476. https://doi.org/10.3390/healthcare11182476
Chicago/Turabian StyleVieira, Ludmilla Maria Souza Mattos de Araújo, Vivian Aline Mininel, and Tatiana de Oliveira Sato. 2023. "Sleep Quality as a Mediator of Burnout, Stress and Multisite Musculoskeletal Pain in Healthcare Workers: A Longitudinal Study" Healthcare 11, no. 18: 2476. https://doi.org/10.3390/healthcare11182476
APA StyleVieira, L. M. S. M. d. A., Mininel, V. A., & Sato, T. d. O. (2023). Sleep Quality as a Mediator of Burnout, Stress and Multisite Musculoskeletal Pain in Healthcare Workers: A Longitudinal Study. Healthcare, 11(18), 2476. https://doi.org/10.3390/healthcare11182476







