Waist-to-Height Ratio: A Sensitive Tool for Assessing the Need for Nutritional Risk Management in Elderly Populations from Brazil
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Study Variables
2.3. Research Team
2.4. Sample Size Calculation and Statistical Analysis
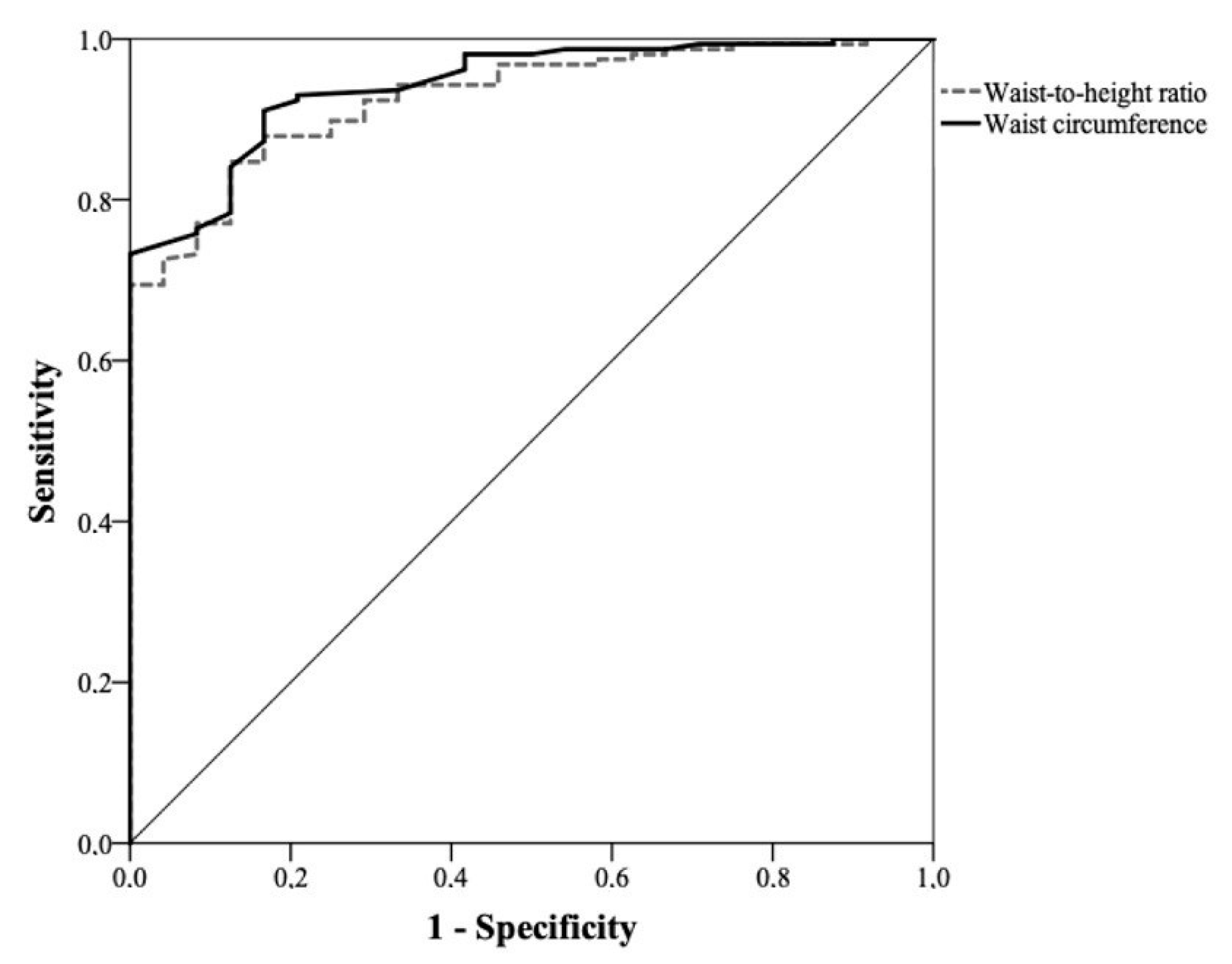
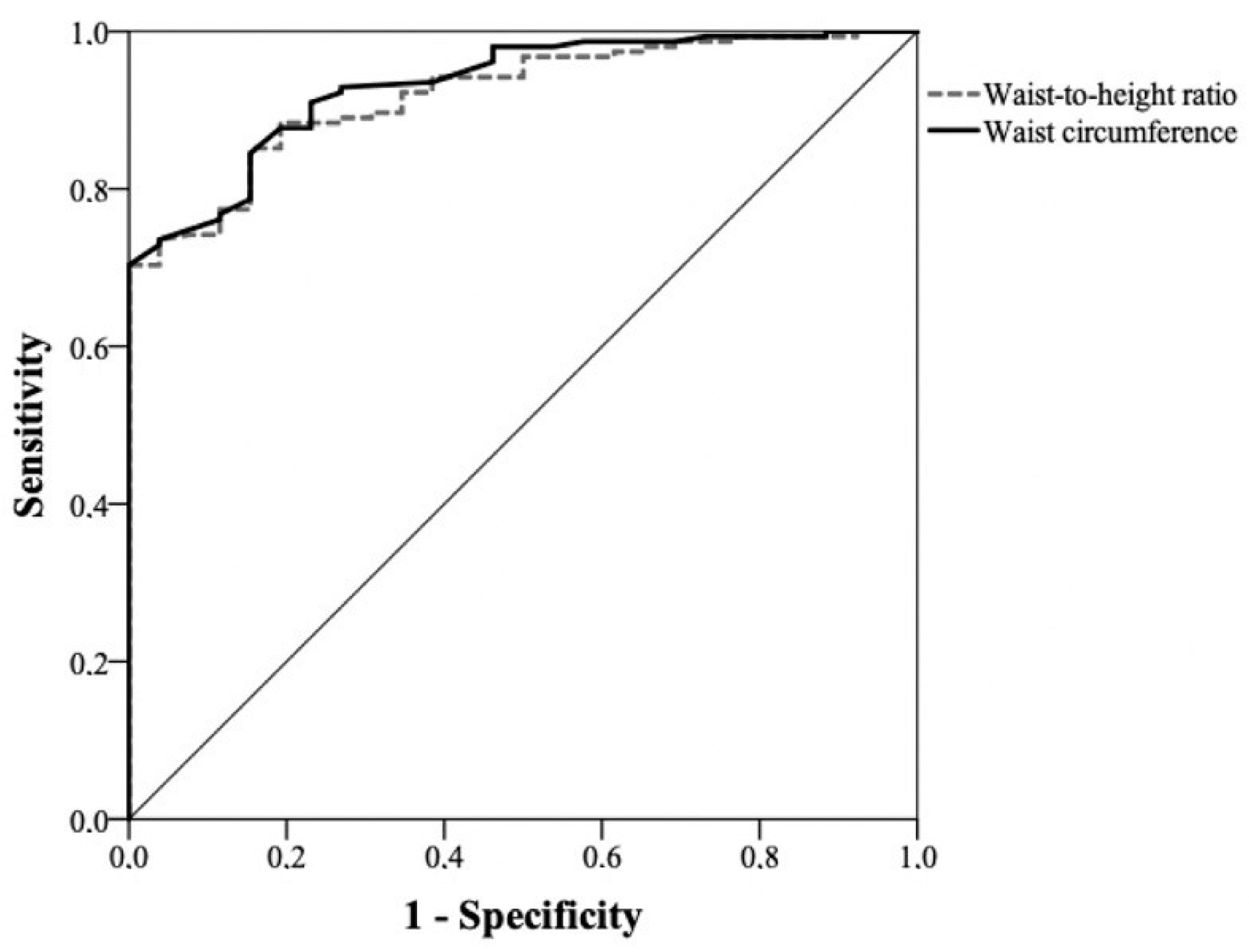
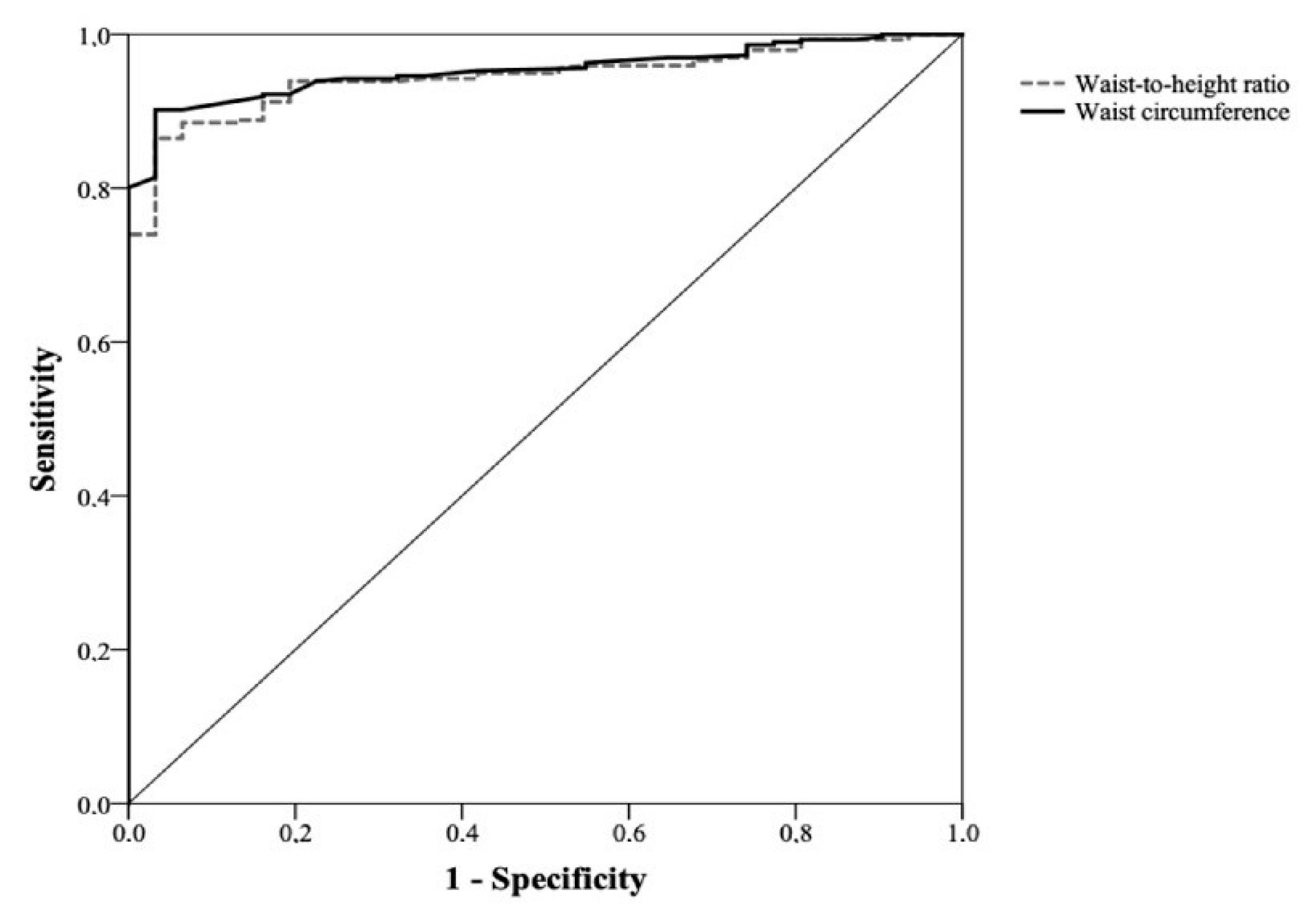
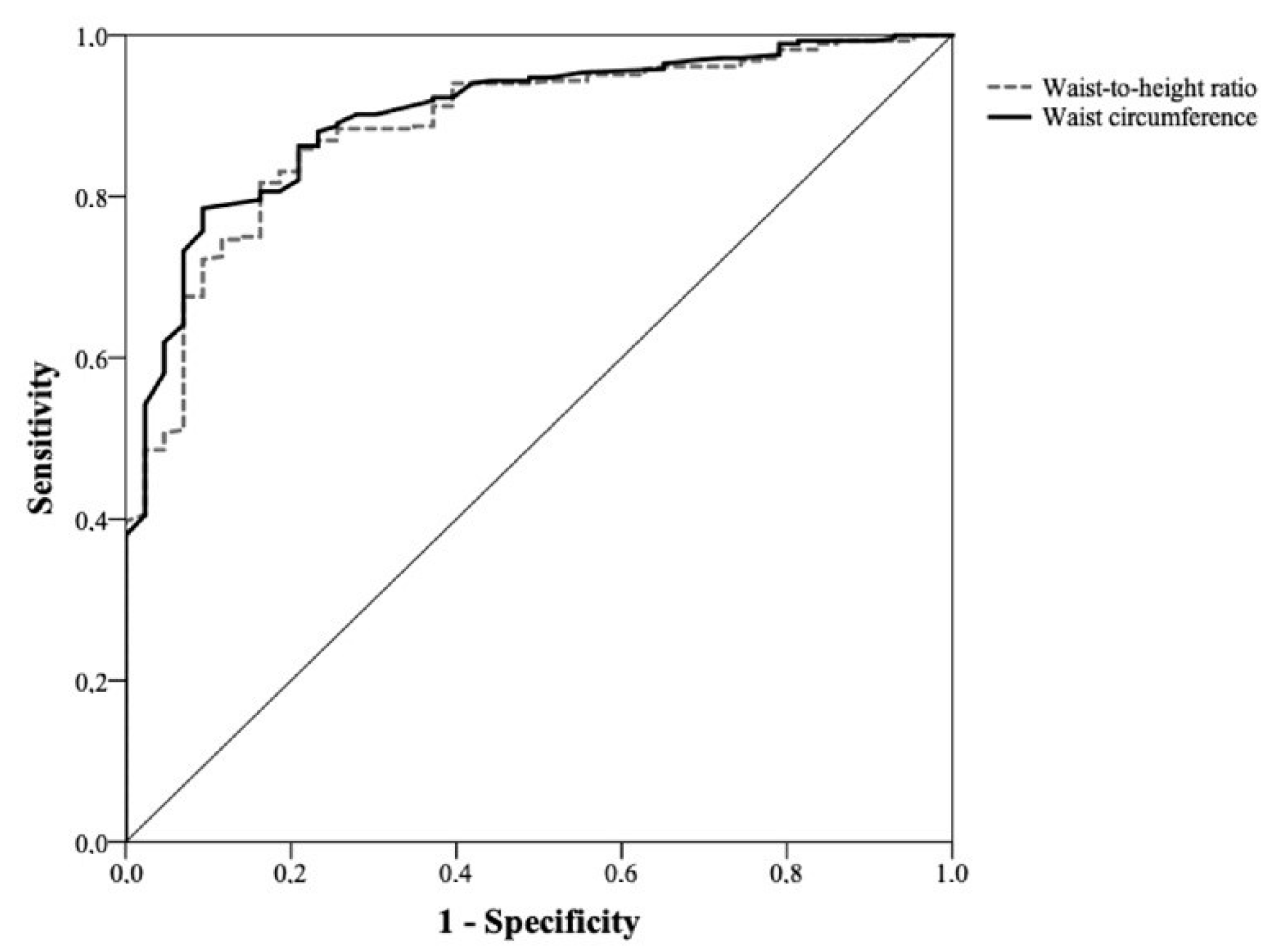
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Piqueras, P.; Ballester, A.; Durá-Gil, J.V.; Martinez-Hervas, S.; Redón, J.; Real, J.T. Anthropometric Indicators as a Tool for Diagnosis of Obesity and Other Health Risk Factors: A Literature Review. Front. Psychol. 2021, 12, 631179. [Google Scholar] [CrossRef]
- Bramhankar, M.; Pandey, M.; Rana, G.S.; Rai, B.; Mishra, N.L.; Shukla, A. An assessment of anthropometric indices and its association with NCDs among the older adults of India: Evidence from LASI Wave-1. BMC Public Health 2021, 21, 1357. [Google Scholar] [CrossRef]
- Lahey, R.; Khan, S.S. Trends in Obesity and Risk of Cardiovascular Disease. Curr. Epidemiol. Rep. 2018, 5, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Després, J.-P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation 2021, 143, e984–e1010. [Google Scholar] [CrossRef]
- Gnatiuc, L.; Alegre-Díaz, J.; Wade, R.; Ramirez-Reyes, R.; Tapia-Conyer, R.; Garcilazo-Ávila, A.; Chiquete, E.; Gonzáles-Carballo, C.; Solano-Sanchez, M.; Clarke, R.; et al. General and Abdominal Adiposity and Mortality in Mexico City. Ann. Intern. Med. 2019, 171, 397. [Google Scholar] [CrossRef]
- Who.int. Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation. Available online: https://www.who.int/publications-detail-redirect/9789241501491 (accessed on 14 December 2022).
- Adegbija, O.; Hoy, W.E.; Wang, Z. Waist circumference values equivalent to body mass index points for predicting absolute cardiovascular disease risks among adults in an Aboriginal community: A prospective cohort study. BMJ Open 2015, 5, e009185. [Google Scholar] [CrossRef] [PubMed]
- Coqueiro, R.d.S.; Barbosa, A.R.; Borgatto, A.F. Anthropometric measurements in the elderly of Havana, Cuba: Age and sex differences. Nutrition 2009, 25, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Santos, J.L.; Albala, C.; Lera, L.; García, C.; Arroyo, P.; Pérez-Bravo, F.; Angel, B.; Peláez, M. Anthropometric measurements in the elderly population of Santiago, Chile. Nutrition 2004, 20, 452–457. [Google Scholar] [CrossRef]
- Lean, M.E.; Han, T.S.; Morrison, C.E. Waist circumference as a measure for indicating need for weight management. BMJ 1995, 311, 158–161. [Google Scholar] [CrossRef] [PubMed]
- Han, T.S.; van Leer, E.M.; Seidell, J.C.; Lean, M.E.J. Waist circumference action levels in the identification of cardiovascular risk factors: Prevalence study in a random sample. BMJ 1995, 311, 1401–1405. [Google Scholar] [CrossRef]
- Ross, R.; Neeland, I.J.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; Cuevas, A.; Hu, F.B.; et al. Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 2020, 16, 177–189. [Google Scholar] [CrossRef]
- Ashwell, M.; Gunn, P.; Gibson, S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: Systematic review and meta-analysis. Obes. Rev. 2011, 13, 275–286. [Google Scholar] [CrossRef]
- Momin, M.; Fan, F.; Li, J.; Jia, J.; Zhang, L.; Zhang, Y.; Huo, Y. Joint Effects of Body Mass Index and Waist Circumference on the Incidence of Hypertension in a Community-Based Chinese Population. Obes. Facts 2020, 13, 245–255. [Google Scholar] [CrossRef]
- Green, M.A. Do we need to think beyond BMI for estimating population-level health risks? J. Public Health 2015, 38, 192–193. [Google Scholar] [CrossRef] [PubMed]
- Seo, D.-C.; Choe, S.; Torabi, M.R. Is waist circumference ≥ 102/88 cm better than body mass index ≥ 30 to predict hypertension and diabetes development regardless of gender, age group, and race/ethnicity? Meta-analysis. Prev. Med. 2017, 97, 100–108. [Google Scholar] [CrossRef]
- Marcadenti, A.; Fuchs, F.D.; Moreira, L.B.; Gus, M.; Fuchs, S.C. Adiposity phenotypes are associated with type-2 diabetes: LAP index, body adiposity index, and neck circumference. Atherosclerosis 2017, 266, 145–150. [Google Scholar] [CrossRef]
- Silveira, E.A.; Pagotto, V.; Barbosa, L.S.; de Oliveira, C.; Pena, G.d.G.; Velasquez-Melendez, G. Accuracy of BMI and waist circumference cut-off points to predict obesity in older adults. Cienc. Saude Coletiva 2020, 25, 1073–1082. [Google Scholar] [CrossRef] [PubMed]
- Karmakar, A.; Garg, S.; Dasgupta, A.; Paul, B.; Maharana, S.P. Sensitivity and specificity of waist circumference as a single screening tool for assessment of overweight and obesity. Int. J. Community Med. Public Health 2017, 4, 4254. [Google Scholar] [CrossRef]
- Misra, A.; Vikram, N.K.; Gupta, R.; Pandey, R.M.; Wasir, J.S.; Gupta, V.P. Waist circumference cutoff points and action levels for Asian Indians for identification of abdominal obesity. Int. J. Obes. 2005, 30, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Molarius, A.; Seidell, J.C.; Sans, S.; Tuomilehto, J.; Kuulasmaa, K. Varying Sensitivity of Waist Action Levels to Identify Subjects with Overweight or Obesity in 19 Populations of The WHO MONICA Project. J. Clin. Epidemiol. 1999, 52, 1213–1224. [Google Scholar] [CrossRef]
- Kodama, S.; Horikawa, C.; Fujihara, K.; Heianza, Y.; Hirasawa, R.; Yachi, Y.; Sugawara, A.; Tanaka, S.; Shimano, H.; Iida, K.T.; et al. Comparisons of the Strength of Associations With Future Type 2 Diabetes Risk Among Anthropometric Obesity Indicators, Including Waist-to-Height Ratio: A Meta-Analysis. Am. J. Epidemiol. 2012, 176, 959–969. [Google Scholar] [CrossRef]
- Thomas, D.M.; Bredlau, C.; Bosy-Westphal, A.; Mueller, M.; Shen, W.; Gallagher, D.; Maeda, Y.; McDougall, A.; Peterson, C.M.; Ravussin, E.; et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity 2013, 21, 2264–2271. [Google Scholar] [CrossRef]
- Liu, S.; Cao, W.; Li, Z.; Wang, S.; Yang, S.; Lu, M.; Li, H.; Song, Y.; Chen, S.; Li, X.; et al. Association between different adiposity measures and all-cause mortality risk among centenarians: A prospective cohort study. Clin. Nutr. 2023, 42, 1219–1226. [Google Scholar] [CrossRef] [PubMed]
- Carmienke, S.; Freitag, M.H.; Pischon, T.; Schlattmann, P.; Fankhaenel, T.; Goebel, H.; Gensichen, J. General and abdominal obesity parameters and their combination in relation to mortality: A systematic review and meta-regression analysis. Eur. J. Clin. Nutr. 2013, 67, 573–585. [Google Scholar] [CrossRef]
- de Hollander, E.L.; Bemelmans, W.J.; Boshuizen, H.C.; Friedrich, N.; Wallaschofski, H.; Guallar-Castillón, P.; Walter, S.; Zillikens, M.C.; Rosengren, A.; Lissner, L.; et al. The association between waist circumference and risk of mortality considering body mass index in 65- to 74-year-olds: A meta-analysis of 29 cohorts involving more than 58 000 elderly persons. Leuk. Res. 2012, 41, 805–817. [Google Scholar] [CrossRef] [PubMed]
- Abraham, T.M.; Pedley, A.; Massaro, J.M.; Hoffmann, U.; Fox, C.S. Association Between Visceral and Subcutaneous Adipose Depots and Incident Cardiovascular Disease Risk Factors. Circulation 2015, 132, 1639–1647. [Google Scholar] [CrossRef]
- Neeland, I.J.; Poirier, P.; Després, J.-P. Cardiovascular and Metabolic Heterogeneity of Obesity: Clinical Challenges and Implications for Management. Circulation 2018, 137, 1391–1406. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, V.C.H.d.S.d.; Rossato, S.L.; Fuchs, F.D.; Harzheim, E.; Fuchs, S.C. Assessment of primary health care received by the elderly and health related quality of life: A cross-sectional study. BMC Public Health 2013, 13, 605. [Google Scholar] [CrossRef][Green Version]
- Fuchs, S.C.; Moreira, L.B.; Camey, S.A.; Moreira, M.B.; Fuchs, F.D. Clustering of risk factors for cardiovascular disease among women in Southern Brazil: A population-based study. Cad. Saude Publica 2008, 24, s285–s293. [Google Scholar] [CrossRef]
- World Health Organization. Physical Status: The Use and Interpretation of Anthropometry. Report of a Who Expert Committee; World Health Organization: Geneva, Switzerland, 1995; Volume 854, pp. 1–452. [Google Scholar]
- Fletcher, R.H.; Fletcher, S.W.; Wagner, E.H. Clinical Epidemiology, 3rd ed.; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 1996. [Google Scholar]
- Geng, S.; Chen, X.; Shi, Z.; Bai, K.; Shi, S. Association of anthropometric indices with the development of multimorbidity in middle-aged and older adults: A retrospective cohort study. PLoS ONE 2022, 17, e0276216. [Google Scholar] [CrossRef]
- Marcadenti, A.; Fuchs, S.C.; Moreira, L.B.; Wiehe, M.; Gus, M.; Fuchs, F.D. Accuracy of Anthropometric Indexes of Obesity to Predict Diabetes Mellitus Type 2 Among Men and Women With Hypertension. Am. J. Hypertens. 2011, 24, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Gus, M.; Fuchs, S.C.; Moreira, L.B.; Moraes, R.S.; Wiehe, M.; Silva, A.F.; Albers, F.; Fuchs, F.D. Association between different measurements of obesity and the incidence of hypertension. Am. J. Hypertens. 2004, 17, 50–53. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, F.D.; Gus, M.; Moreira, L.B.; Moraes, R.S.; Wiehe, M.; Pereira, G.M.; Fuchs, S.C. Anthropometric Indices and the Incidence of Hypertension: A Comparative Analysis. Obes. Res. 2005, 13, 1515–1517. [Google Scholar] [CrossRef] [PubMed]
- Moosaie, F.; Abhari, S.M.F.; Deravi, N.; Behnagh, A.K.; Esteghamati, S.; Firouzabadi, F.D.; Rabizadeh, S.; Nakhjavani, M.; Esteghamati, A. Waist-To-Height Ratio Is a More Accurate Tool for Predicting Hypertension Than Waist-To-Hip Circumference and BMI in Patients With Type 2 Diabetes: A Prospective Study. Front. Public Health 2021, 9, 726288. [Google Scholar] [CrossRef] [PubMed]
- Sommer, I.; Teufer, B.; Szelag, M.; Nussbaumer-Streit, B.; Titscher, V.; Klerings, I.; Gartlehner, G. The performance of anthropometric tools to determine obesity: A systematic review and meta-analysis. Sci. Rep. 2020, 10, 12699. [Google Scholar] [CrossRef]
- Marini, E.; Buffa, R.; Gobbo, L.A.; Salinas-Escudero, G.; Stagi, S.; García-Peña, C.; Sánchez-García, S.; Carrillo-Vega, M.F. Interpopulation Similarity of Sex and Age-Related Body Composition Variations Among Older Adults. Int. J. Environ. Res. Public Health 2020, 17, 6047. [Google Scholar] [CrossRef]
- Corrêa, M.M.; Facchini, L.A.; Thumé, E.; de Oliveira, E.R.A.; Tomasi, E. The ability of waist-to-height ratio to identify health risk. Rev. Saúde Publica 2019, 53, 66. [Google Scholar] [CrossRef]
- Browning, L.M.; Hsieh, S.D.; Ashwell, M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0·5 could be a suitable global boundary value. Nutr. Res. Rev. 2010, 23, 247–269. [Google Scholar] [CrossRef]
- Cai, L.; Liu, A.; Zhang, Y.; Wang, P. Waist-to-Height Ratio and Cardiovascular Risk Factors among Chinese Adults in Beijing. PLoS ONE 2013, 8, e69298. [Google Scholar] [CrossRef]
- Wakabayashi, I.; Daimon, T. Receiver-operated characteristics (ROCs) of the relationships between obesity indices and multiple risk factors (MRFs) for atherosclerosis at different ages in men and women. Arch. Gerontol. Geriatr. 2012, 55, 96–100. [Google Scholar] [CrossRef] [PubMed]
| Nutritional Risk Level 1 * | ||
|---|---|---|
| BMI (kg/m2) | BMI (kg/m2) and WHR | |
| Men | ≥25 or <25 and WHR ≥ 0.90 | |
| Women | ≥25 or <25 and WHR ≥ 0.85 | |
| Nutritional risk level 2 * | ||
| BMI (kg/m2) | BMI (kg/m2) and WHR | |
| Men | ≥30 or <30 and WHR ≥ 0.90 | |
| Women | ≥30 or <30 and WHR ≥ 0.85 | |
| Total n = 509 | Men n = 182 | Women n = 327 | p-Value | |
|---|---|---|---|---|
| Age (years) | 72.8 ± 8.2 | 73.0 ± 8.2 | 72.6 ± 8.2 | 0.7 |
| Age range (years) | 60.1–103.4 | 60.3–93.6 | 60.1–103.4 | |
| Schooling (years) | 1.0 | |||
| 0 | 241(47.3) | 85 (46.7) | 156 (47.7) | |
| 1 to 4 | 190 (37.3) | 68 (37.4) | 122 (37.3) | |
| ≥5 | 78 (15.3) | 29 (15.9) | 49 (15.0) | |
| Body mass index (kg/m2) | 26.6 ± 5.3 | 25.3 ± 4.2 | 27.3 ± 5.7 | <0.001 |
| Waist circumference (cm) | 90.3 ± 13.4 | 91.1 ± 12.8 | 89.9 ± 13.7 | 0.4 |
| Waist-hip ratio | 0.94 ± 0.09 | 0.98 ± 0.10 | 0.92 ± 0.09 | <0.001 |
| Waist-to-height ratio | 0.58 ± 0.09 | 0.56 ± 0.07 | 0.59 ± 0.09 | <0.001 |
| Hypertension | 144 (28.3) | 45 (24.9) | 99 (30.2) | 0.2 |
| Diabetes mellitus | 67 (13.2) | 18 (9.9) | 49 (14.9) | 0.12 |
| Mental disorder | 9 (1.8) | 5 (2.8) | 4 (1.2) | 0.2 |
| Chronic pain | 126 (24.9) | 47 (26.0) | 79 (24.3) | 0.7 |
| Main health problem: CVD | 204 (40.1) | 63 (34.6) | 141 (43.1) | 0.06 |
| Nutritional Risk Level 1 | ||
|---|---|---|
| BMI ≥ 25 kg/m2 | BMI < 25 kg/m2 and High WHR | |
| Men | n = 89 | n = 68 |
| WC > 94 cm | 60 (67.4) * | 14 (20.6) * |
| WHtR ≥ 0.5 | 87 (97.8) * | 58 (85.3) ƒ |
| Women | n = 212 | n = 84 |
| WC > 80 cm | 201 (94.8) * | 43 (51.2) * |
| WHtR ≥ 0.5 | 207 (97.6) * | 68 (81.0) ƒƒ |
| Total | n = 301 | n = 152 |
| WC > 94/>80 cm | 261 (86.7) * | 57 (37.5) * |
| WHtR ≥ 0.5 | 294 (97.7) * | 126 (82.9) ƒƒƒ |
| Nutritional Risk Level 2 | ||
| BMI ≥ 30 kg/m2 | BMI < 30 kg/m2 and high WHR | |
| Men | n = 26 | n = 129 |
| WC > 102 cm | 17 (65.4) * | 18 (14.0) **** |
| WHtR ≥ 0.5 | 26 (100.0) ** | 117 (90.7) * |
| Women | n = 96 | n = 188 |
| WC > 88 cm | 90 (93.8) * | 92 (48.9) * |
| WHtR ≥ 0.5 | 96 (100.0) * | 168 (89.4) *** |
| Total | n = 122 | n = 317 |
| WC > 102/> 88 cm | 107 (87.7) * | 110 (34.7) * |
| WHtR ≥ 0.5 | 122 (100.0) * | 285 (89.9) * |
| Cutoff Point | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | |
|---|---|---|---|---|---|
| Level 1: BMI ≥ 25 kg/m2 or BMI < 25 kg/m2 and high WHR | |||||
| Men | WC >94 cm | 46.8 (38.7–54.9) | 100.0 (97.9–100.0) | 100.0 (99.3–100.0) | 22.4 (14.1–30.8) |
| WHtR ≥ 0.50 | 91.8 (81.2–96.4) | 70.8 (50.6–91.1) | 95.4 (91.7–99.1) | 56.7 (37.3–76.1) | |
| Women | WC >80 cm | 82.4 (77.9–86.9) | 96.8 (88.9–100) | 99.6 (98.6–100.0) | 36.6 (25.6–47.6) |
| WHtR ≥ 0.50 | 92.9 (89.8–96.0) | 80.7 (65.1–96.2) | 97.9 (96.0–99.7) | 54.4 (38.9–69.8) | |
| Level 2: BMI ≥ 30 kg/m2 or BMI < 30 kg/m2 and high WHR | |||||
| Men | WC > 102 cm | 22.6 (15.7–29.5) | 100.0 (98.1–100.0) | 100.0 (98.6–100.0) | 17.8 (11.3–24.4) |
| WHtR ≥ 0.50 | 91.7 (87.0–96.3) | 65.4 (45.2–85.6) | 94.1 (90.0–98.2) | 56.7 (37.3–76.1) | |
| Women | WC >88 cm | 64.1 (58.3–69.8) | 93.0 (84.3–100.0) | 98.4 (96.3–100.0) | 28.2 (20.4–35.9) |
| WHtR ≥ 0.50 | 93.0 (89.8–96.1) | 60.5 (44.7–76.2) | 94.0 (91.0–96.9) | 56.5 (41.1–71.9) | |
| Cutoff Point | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | |
|---|---|---|---|---|---|
| Level 1: BMI ≥ 25 kg/m2 or BMI < 25 kg/m2 and high WHR | |||||
| Men | WC >94 cm | 76.2 (69.5–82.8) | 100.0 (96.4–100.0) | 100.0 (99.6–100.0) | 25.5 (13.0–37.9) |
| WHtR ≥0.50 | 97.7 (95.1–100.0) | 64.3 (35.6–93.0) | 97.1 (94.3–99.9) | 69.2 (40.3–98.2) | |
| Women | WC >80 cm | 93.3 (90.5–96.1) | 81.0 (70.5–91.4) | 96.4 (94.2–98.5) | 68.9 (57.7–80.1) |
| WHtR ≥ 0.50 | 96.2 (94.0–98.4) | 68.3 (56.0–80.5) | 94.3 (91.7–96.8) | 76.8 (64.8–88.7) | |
| Level 2: BMI ≥ 30 kg/m2 or BMI < 30 kg/m2 and high WHR | |||||
| Men | WC >102 cm | 43.1 (35.3–50.9) | 100.0 (97.4–100.0) | 100.0 (99.3–100.0) | 16.7 (9.4–24.0) |
| WHtR ≥ 0.50 | 97.6 (95.0–100.0) | 47.4 (22.3–72.5) | 94.2 (90.5–98.0) | 69.2 (40.3–98.2) | |
| Women | WC >88 cm | 78.0 (73.1–82.9) | 90.1 (84.1–96.1) | 95.4 (92.6–98.3) | 60.6 (52.9–68.4) |
| WHtR ≥ 0.50 | 98.0 (96.2–99.7) | 45.0 (35.3–54.8) | 82.5 (78.3–86.6) | 89.3 (80.3–98.3) | |
| Total n = 599 | Men n = 187 | Women n = 412 | p-Value | |
|---|---|---|---|---|
| Age (years) | 70.7 ± 7.2 | 70.3 ± 6.6 | 70.9 ± 7.6 | 0.3 |
| Schooling (years) | <0.001 | |||
| 0 | 49 (8.2) | 5 (2.7) | 44 (10.7) | |
| 1 to 4 | 155 (25.9) | 39 (20.9) | 116 (28.2) | |
| ≥5 | 394 (65.9) | 143 (76.5) | 251 (61.1) | |
| Body mass index (kg/m2) | 28.0 ± 5.0 | 27.2 ± 4.2 | 28.4 ± 5.2 | 0.007 |
| Waist circumference (cm) | 94.4 ± 13.5 | 99.7 ± 11.2 | 91.9 ± 13.7 | <0.001 |
| Waist-hip ratio | 0.91 ± 0.10 | 0.98 ± 0.07 | 0.89 ± 0.11 | <0.001 |
| Waist-to-height ratio | 0.59 ± 0.08 | 0.59 ± 0.06 | 0.59 ± 0.09 | 0.7 |
| Main health problem: CVD | 58 (8.3) | 37 (9.0) | 21 (11.2) | 0.4 |
| Nutritional Risk Level 1 | ||
|---|---|---|
| BMI ≥ 25 kg/m2 | BMI < 25 kg/m2 and High WHR | |
| Men | n = 132 | n = 40 |
| WC > 94 cm | 118 (89.4) | 13 (32.5) |
| WHtR ≥ 0.5 | 132 (100.0) | 36 (90.0) |
| Women | n = 294 | n = 44 |
| WC > 80 cm | 280 (95.2) | 36 (81.8) |
| WHtR ≥ 0.5 | 286 (97.3) | 40 (90.9) |
| Total | n = 426 | n = 84 |
| WC > 94/>80 cm | 398 (93.4) | 49 (58.3) |
| WHtR ≥ 0.5 | 418 (98.1) | 76 (90.5) |
| Nutritional Risk Level 2 | ||
| BMI ≥ 30 kg/m2 | BMI < 30 kg/m2 and high WHR | |
| Men | n = 43 | n = 124 |
| WC > 102 cm | 41 (95.3) | 31 (25.0) |
| WHtR ≥ 0.5 | 43 (100.0) | 120 (96.8) |
| Women | n = 138 | n = 152 |
| WC > 88 cm | 136 (98.6) | 92 (60.5) |
| WHtR ≥ 0.5 | 138 (100.0) | 147 (96.7) |
| Total | n = 181 | n = 276 |
| WC > 102/>88 cm | 177 (97.8) | 123 (44.6) |
| WHtR ≥ 0.5 | 181 (100.0) | 267 (96.7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carvalho, V.C.H.d.S.; Moreira, L.B.; Luft, V.C.; Fuchs, S.C. Waist-to-Height Ratio: A Sensitive Tool for Assessing the Need for Nutritional Risk Management in Elderly Populations from Brazil. Healthcare 2023, 11, 2406. https://doi.org/10.3390/healthcare11172406
Carvalho VCHdS, Moreira LB, Luft VC, Fuchs SC. Waist-to-Height Ratio: A Sensitive Tool for Assessing the Need for Nutritional Risk Management in Elderly Populations from Brazil. Healthcare. 2023; 11(17):2406. https://doi.org/10.3390/healthcare11172406
Chicago/Turabian StyleCarvalho, Vivian C. Honorato dos Santos, Leila B. Moreira, Vivian C. Luft, and Sandra C. Fuchs. 2023. "Waist-to-Height Ratio: A Sensitive Tool for Assessing the Need for Nutritional Risk Management in Elderly Populations from Brazil" Healthcare 11, no. 17: 2406. https://doi.org/10.3390/healthcare11172406
APA StyleCarvalho, V. C. H. d. S., Moreira, L. B., Luft, V. C., & Fuchs, S. C. (2023). Waist-to-Height Ratio: A Sensitive Tool for Assessing the Need for Nutritional Risk Management in Elderly Populations from Brazil. Healthcare, 11(17), 2406. https://doi.org/10.3390/healthcare11172406






