Effectiveness of a Preventative Program for Groin Pain Syndrome in Elite Youth Soccer Players: A Prospective, Randomized, Controlled, Single-Blind Study
Abstract
:1. Introduction
2. Materials and Methods
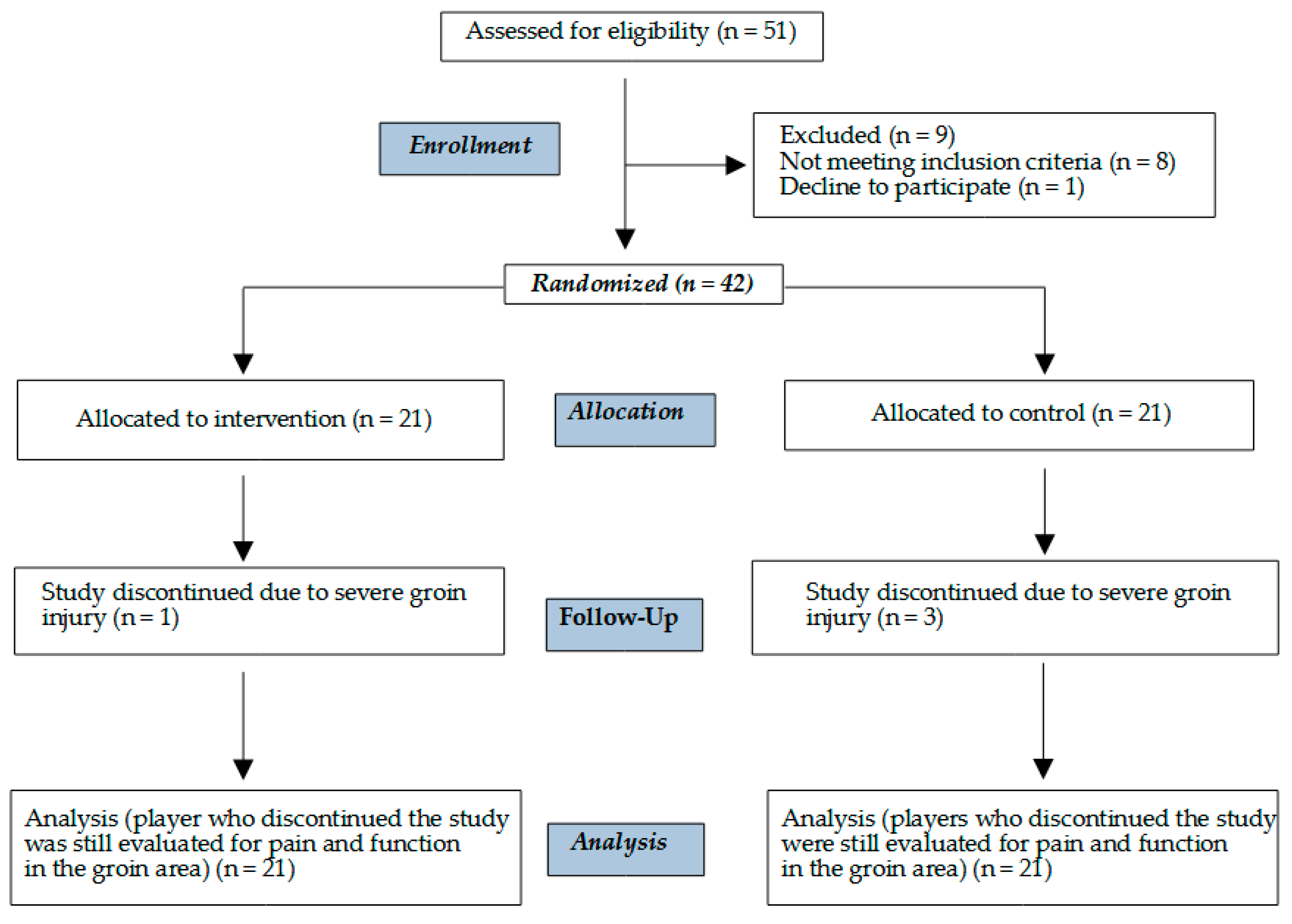
2.1. Study Protocol and Study Design
2.2. Clinical Assessment
2.3. Preventive Program Protocol
2.4. A Priori Sample Size and Power Analysis
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Program Effectiveness
4.2. Groin Pain Rate
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Taylor, D.C.; Meyers, W.C.; Moylan, J.A.; Lohnes, J.; Bassett, F.H.; Garrett, W.E., Jr. Abdominal Musculature Abnormalities as a Cause of Groin Pain in Athletes. Inguinal Hernias and Pubalgia. Am. J. Sports Med. 1991, 19, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Zuckerbraun, B.S.; Cyr, A.R.; Mauro, C.S. Groin Pain Syndrome Known as Sports Hernia: A Review. JAMA Surg. 2020, 155, 340. [Google Scholar] [CrossRef] [PubMed]
- Weir, A.; Robinson, P.; Hogan, B.; Franklyn-Miller, A. MRI Investigation for Groin Pain in Athletes: Is Radiological Terminology Clarifying or Confusing? Br. J. Sports Med. 2017, 51, 1185–1186. [Google Scholar] [CrossRef] [PubMed]
- Bisciotti, G.N.; Auci, A.; Di Marzo, F.; Galli, R.; Pulici, L.; Carimati, G.; Quaglia, A.; Volpi, P. Groin Pain Syndrome: An Association of Different Pathologies and a Case Presentation. Muscles Ligaments Tendons. J. 2015, 5, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Morelli, V.; Weaver, V. Groin Injuries and Groin Pain in Athletes: Part 1. Prim. Care 2005, 32, 163–183. [Google Scholar] [CrossRef]
- Werner, J.; Hagglund, M.; Walden, M.; Ekstrand, J. UEFA Injury Study: A Prospective Study of Hip and Groin Injuries in Professional Football over Seven Consecutive Seasons. Br. J. Sports Med. 2009, 43, 1036–1040. [Google Scholar] [CrossRef] [PubMed]
- Mosler, A.B.; Weir, A.; Eirale, C.; Farooq, A.; Thorborg, K.; Whiteley, R.J.; Hӧlmich, P.; Crossley, K.M. Epidemiology of Time Loss Groin Injuries in a Men’s Professional Football League: A 2-Year Prospective Study of 17 Clubs and 606 Players. Br. J. Sports Med. 2018, 52, 292–297. [Google Scholar] [CrossRef]
- Hölmich, P.; Thorborg, K.; Dehlendorff, C.; Krogsgaard, K.; Gluud, C. Incidence and Clinical Presentation of Groin Injuries in Sub-Elite Male Soccer. Br. J. Sports Med. 2014, 48, 1245–1250. [Google Scholar] [CrossRef]
- Engebretsen, A.H.; Myklebust, G.; Holme, I.; Engebretsen, L.; Bahr, R. Prevention of Injuries among Male Soccer Players: A Prospective, Randomized Intervention Study Targeting Players with Previous Injuries or Reduced Function. Am. J. Sports Med. 2008, 36, 1052–1060. [Google Scholar] [CrossRef]
- Franklyn-Miller, A.; Richter, C.; King, E.; Gore, S.; Moran, K.; Strike, S.; Falvey, E.C. Athletic Groin Pain (Part 2): A Prospective Cohort Study on the Biomechanical Evaluation of Change of Direction Identifies Three Clusters of Movement Patterns. Br. J. Sports Med. 2017, 51, 460–468. [Google Scholar] [CrossRef]
- Sedaghati, P.; Alizadeh, M.-H.; Shirzad, E.; Ardjmand, A. Review of Sport-Induced Groin Injuries. Trauma Mon. 2013, 18, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Candela, V.; De Carli, A.; Longo, U.G.; Sturm, S.; Bruni, G.; Salvatore, G.; Denaro, V. Hip and Groin Pain in Soccer Players. Joints 2019, 07, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Jones, N.S. Update: Soccer Injury and Prevention, Concussion, and Chronic Groin Pain. Curr. Sports Med. Rep. 2014, 13, 319–325. [Google Scholar] [CrossRef]
- Drew, M.K.; Lovell, G.; Palsson, T.S.; Chiarelli, P.E.; Osmotherly, P.G. Australian Football Players Experiencing Groin Pain Exhibit Reduced Subscale Scores of Activities of Daily Living and Sport and Recreation on the HAGOS Questionnaire: A Case-Control Study. Phys. Ther. Sport 2017, 26, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Carolan, D.; Richter, C.; Thorborg, K.; Franklyn-Miller, A.; O’Donovan, J.; McDonald, C.; King, E. Hip and Groin Pain Prevalence and Prediction in Elite Gaelic Games: 2703 Male Athletes across Two Seasons. Scand. Med. Sci. Sports 2022, 32, 924–932. [Google Scholar] [CrossRef]
- Tyler, T.F.; Silvers, H.J.; Gerhardt, M.B.; Nicholas, S.J. Groin Injuries in Sports Medicine. Sports Health 2010, 2, 231–236. [Google Scholar] [CrossRef]
- de la Calle, O.; Rodríguez, M.Á.; Del Valle, M.; Crespo, I.; Olmedillas, H. Exercise Interventions on Athletes with Longstanding Adductor-Related Groin Pain: A Critically Appraised Topic. Med. Sport 2023, 75, 620–629. [Google Scholar] [CrossRef]
- Weir, A.; Brukner, P.; Delahunt, E.; Ekstrand, J.; Griffin, D.; Khan, K.M.; Lovell, G.; Meyers, W.C.; Muschaweck, U.; Orchard, J.; et al. Doha Agreement Meeting on Terminology and Definitions in Groin Pain in Athletes. Br. J. Sports Med. 2015, 49, 768–774. [Google Scholar] [CrossRef]
- Esteve, E.; Rathleff, M.S.; Bagur-Calafat, C.; Urrútia, G.; Thorborg, K. Prevention of Groin Injuries in Sports: A Systematic Review with Meta-Analysis of Randomised Controlled Trials. Br. J. Sports Med. 2015, 49, 785–791. [Google Scholar] [CrossRef]
- Page, P. Beyond Statistical Significance: Clinical Interpretation of Rehabilitation Research Literature. Int. J. Sports Phys. Ther. 2014, 9, 726–736. [Google Scholar]
- Castle, J.P.; Kessler, A.; Abbas, M.J.; Wager, S.; Khalil, L.S.; Okoroha, K.R.; Mehran, N. High Return to Play Rate and Reduced Career Longevity Following Surgical Management of Athletic Pubalgia in National Basketball Association Players. Arthrosc. Sports Med. Rehabil. 2021, 3, e1359–e1365. [Google Scholar] [CrossRef] [PubMed]
- Ramazzina, I.; Bernazzoli, B.; Braghieri, V.; Costantino, C. Groin Pain in Athletes and Non-Interventional Rehabilitative Treatment: A Systematic Review. J. Sports Med. Phys. Fit. 2019, 59, 1001–1010. [Google Scholar] [CrossRef] [PubMed]
- Charlton, P.C.; Drew, M.K.; Mentiplay, B.F.; Grimaldi, A.; Clark, R.A. Exercise Interventions for the Prevention and Treatment of Groin Pain and Injury in Athletes: A Critical and Systematic Review. Sports Med. 2017, 47, 2011–2026. [Google Scholar] [CrossRef]
- Serner, A.; van Eijck, C.H.; Beumer, B.R.; Hölmich, P.; Weir, A.; de Vos, R.-J. Study Quality on Groin Injury Management Remains Low: A Systematic Review on Treatment of Groin Pain in Athletes. Br. J. Sports Med. 2015, 49, 813. [Google Scholar] [CrossRef]
- Mercurio, M.; Corona, K.; Galasso, O.; Cerciello, S.; Morris, B.J.; Guerra, G.; Gasparini, G. Soccer Players Show the Highest Seasonal Groin Pain Prevalence and the Longest Time Loss from Sport among 500 Athletes from Major Team Sports. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 2149–2157. [Google Scholar] [CrossRef] [PubMed]
- Hölmich, P.; Larsen, K.; Krogsgaard, K.; Gluud, C. Exercise Program for Prevention of Groin Pain in Football Players: A Cluster-Randomized Trial: Exercise Program for Prevention of Groin Pain in Football Players. Scand. Med. Sci. Sports 2010, 20, 814–821. [Google Scholar] [CrossRef] [PubMed]
- Harøy, J.; Clarsen, B.; Wiger, E.G.; Øyen, M.G.; Serner, A.; Thorborg, K.; Hölmich, P.; Andersen, T.E.; Bahr, R. The Adductor Strengthening Programme Prevents Groin Problems among Male Football Players: A Cluster-Randomised Controlled Trial. Br. J. Sports Med. 2019, 53, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Schulz, K.F.; Altman, D.G.; Moher, D.; for the CONSORT Group. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef]
- Thorborg, K.; Branci, S.; Nielsen, M.P.; Langelund, M.T.; Hölmich, P. Copenhagen Five-Second Squeeze: A Valid Indicator of Sports-Related Hip and Groin Function. Br. J. Sports Med. 2017, 51, 594–599. [Google Scholar] [CrossRef]
- Shanmugaraj, A.; Shell, J.R.; Horner, N.S.; Duong, A.; Simunovic, N.; Uchida, S.; Ayeni, O.R. How Useful Is the Flexion–Adduction–Internal Rotation Test for Diagnosing Femoroacetabular Impingement: A Systematic Review. Clin. J. Sport Med. 2018. Publish Ahead of Print. [Google Scholar] [CrossRef]
- Serner, A.; Lichau, O.; Reboul, G. Evaluation of the Bent Knee Fall out Test Pre- and Post- an Adductor Longus Tenotomy. Phys. Ther. Sport 2021, 48, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, M.F.; Thorborg, K.; Krommes, K.; Thornton, K.B.; Hölmich, P.; Peñalver, J.J.J.; Ishøi, L. Hip Adduction Strength and Provoked Groin Pain: A Comparison of Long-Lever Squeeze Testing Using the ForceFrame and the Copenhagen 5-Second-Squeeze Test. Phys. Ther. Sport 2022, 55, 28–36. [Google Scholar] [CrossRef]
- Hsieh, F.Y.; Liu, A.A. Adequacy of Sample Size in Health Studies; Lemeshow, S., David, W.H., Jr., Klar, J., Stephen, K., Eds.; Wiley: Chichester, UK, 1990; pp. Xii + 233. [Google Scholar] [CrossRef]
- Lachenbruch, P.A.; Lwanga, S.K.; Lemeshow, S. Sample Size Determination in Health Studies: A Practical Manual. J. Am. Stat. Assoc. 1991, 86, 1149. [Google Scholar] [CrossRef]
- Paajanen, H.; Ristolainen, L.; Turunen, H.; Kujala, U.M. Prevalence and Etiological Factors of Sport-Related Groin Injuries in Top-Level Soccer Compared to Non-Contact Sports. Arch. Orthop. Trauma Surg. 2011, 131, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Altman, D.G. Practical Statistics for Medical Research, 1st ed.; Chapman and Hall/CRC: Boca Raton, FL, USA, 1990. [Google Scholar] [CrossRef]
- Pérez-Gómez, J.; Villafaina, S.; Adsuar, J.C.; Carlos-Vivas, J.; Garcia-Gordillo, M.Á.; Collado-Mateo, D. Copenhagen Adduction Exercise to Increase Eccentric Strength: A Systematic Review and Meta-Analysis. Appl. Sci. 2020, 10, 2863. [Google Scholar] [CrossRef]
- Van Beijsterveldt, A.M.C.; Van De Port, I.G.L.; Krist, M.R.; Schmikli, S.L.; Stubbe, J.H.; Frederiks, J.E.; Backx, F.J.G. Effectiveness of an Injury Prevention Programme for Adult Male Amateur Soccer Players: A Cluster-Randomised Controlled Trial. Br. J. Sports Med. 2012, 46, 1114–1118. [Google Scholar] [CrossRef]
- Steffen, K.; Myklebust, G.; Olsen, O.E.; Holme, I.; Bahr, R. Preventing Injuries in Female Youth Football—A Cluster-Randomized Controlled Trial: Injury Prevention in Youth Football. Scandinavian Med. Sci. Sports 2008, 18, 605–614. [Google Scholar] [CrossRef]
- Shetty, V.D.; Shetty, N.S.; Shetty, A.P. Groin Pain in Athletes: A Novel Diagnostic Approach. SICOT-J 2015, 1, 16. [Google Scholar] [CrossRef]
- Dupré, T.; Lysdal, F.G.; Funken, J.; Mortensen, K.R.L.; Müller, R.; Mayer, J.; Krahl, H.; Potthast, W. Groin Injuries in Soccer: Investigating the Effect of Age on Adductor Muscle Forces. Med. Sci. Sports Exerc. 2020, 52, 1330–1337. [Google Scholar] [CrossRef]

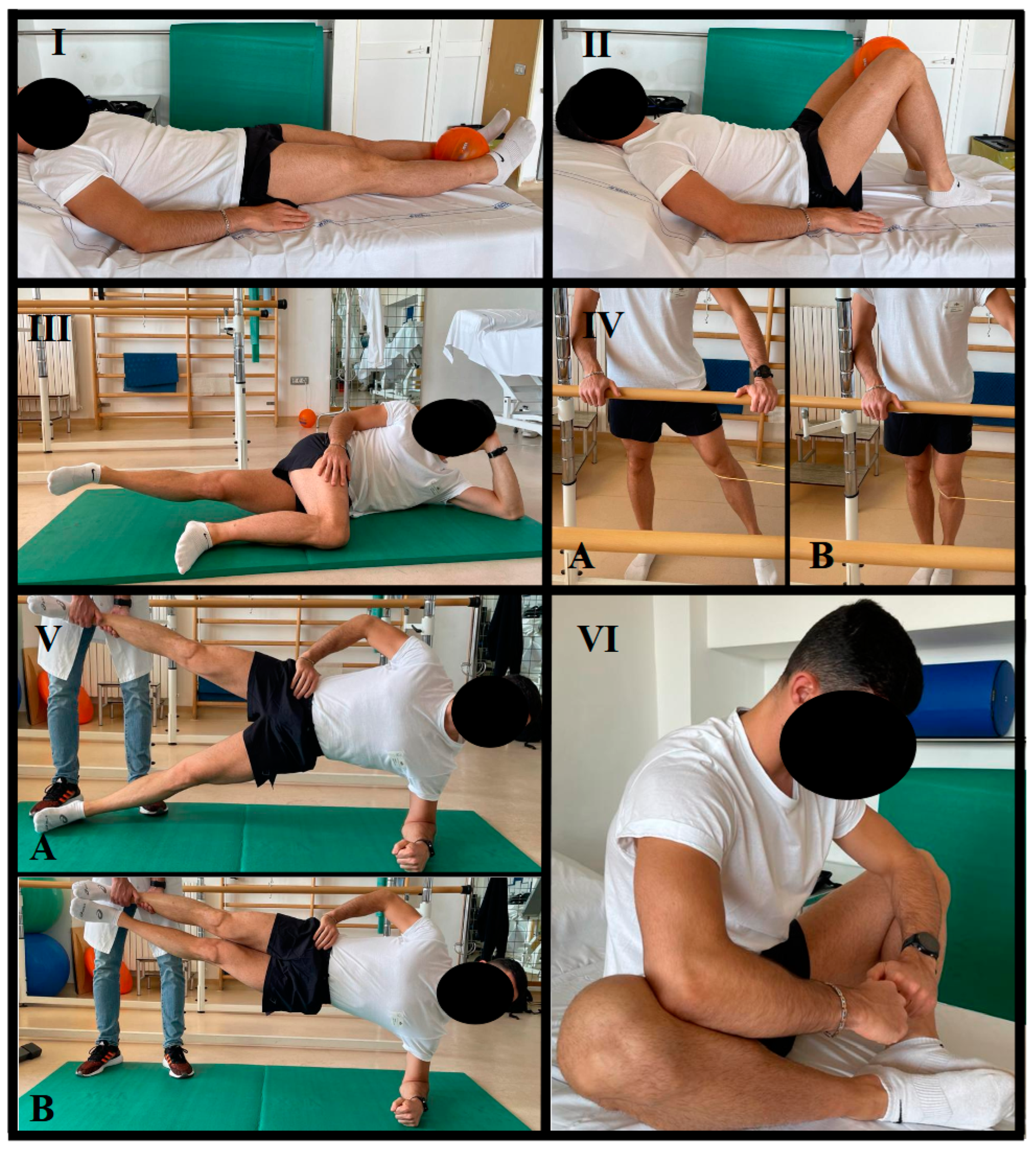
| 1–8th Weeks | 9–16th Weeks | 17–24th Weeks | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Exercises | Sets | Reps | CT–RT (s) | Sets | Reps | CT-RT (s) | Sets | Reps | CT–RT (s) | Rest (s) |
| I | 1 | 10 | 5–5 | 1 | 10 | 10–5 | 1 | 10 | 15–5 | / |
| II | 2 | 8/10 | 5–5 | 3 | 8/10 | 5–5 | 4 | 8/10 | 5–5 | 60 |
| III | 2 | 8/10 | 10–10 | 3 | 8/10 | 10–10 | 4 | 8/10 | 10–10 | 30 |
| IV | 1 | 5 | 20–10 | 1 | 5 | 30–15 | 1 | 5 | 60–30 | / |
| V | 3 | 10 | 6–6 | 3 | 15 | 6–6 | 3 | 20 | 6–6 | 60 |
| VI | 2 | 5 | 20–10 | 3 | 5 | 20–10 | 4 | 5 | 20–10 | 60 |
| Overall (n = 42) | Treatment Group (n = 21) | Control Group (n = 21) | |
|---|---|---|---|
| Age (years) | 17.0 ± 0.7 | 16.8 ± 0.5 | 17.1 ± 0.8 |
| Height (cm) | 178.9 ± 4.9 | 177.6 ± 4.4 | 180.1 ± 5.1 |
| Weight (kg) | 72.5 ± 5.3 | 72.3 ± 6.0 | 72.7 ± 4.5 |
| BMI (kg/m2) | 22.7 ± 1.3 | 22.9 ± 1.4 | 22.4 ± 1.1 |
| Dominant leg (%) (left–right) | 19–81 | 14–86 | 5–95 |
| Level of play (%) (high–medium) | 83–17 | 86–14 | 81–19 |
| Training experience (years) | 8.7 ± 2.0 | 9.0 ± 1.9 | 8.5 ± 2.0 |
| Weekly training load (hours) | 10.6 ± 2.3 | 11.0 ± 2.4 | 10.1 ± 2.3 |
| Position on field (%) | |||
| Goalkeeper | 7 | 5 | 10 |
| Defense | 33 | 33 | 33 |
| Midfield | 29 | 33 | 24 |
| Striker | 31 | 29 | 33 |
| Parameter | Treatment Group | Control Group | Difference | p-Value |
|---|---|---|---|---|
| HAGOS (overall) | 100 [99 to 100] | 100 [88.2 to 100] | 0 [0 to 1] | 0.6642 |
| HAGOS (pain) | 100 [100 to 100] | 100 [87.5 to 100] | 0 [0 to 0] | 0.2006 |
| HAGOS (symptoms) | 100 [100 to 100] | 100 [87.5 to 100] | 0 [0 to 0] | 0.2008 |
| HAGOS (participation in physical activities) | 100 [100 to 100] | 100 [87.5 to 100] | 0 [0 to 0] | 0.0419 |
| HAGOS (functional sports and recreational activities) | 100 [100 to 100] | 100 [83.6 to 100] | 0 [0 to 0] | 0.2199 |
| HAGOS (physical function) | 100 [100 to 100] | 100 [92.5 to 100] | 0 [0 to 0] | 0.2070 |
| HAGOS (quality of life) | 100 [93.8 to 100] | 100 [91.6 to 100] | 0 [0 to 0] | 0.9094 |
| R-5SST | 0 [0 to 0] | 0 [0 to 2] | 0 [0 to 0] | 0.2262 |
| L-5SST | 0 [0 to 0] | 0 [0 to 0.8] | 0 [0 to 0] | 0.3683 |
| R-FADIR | 3 (14.3%) | 6 (28.6%) | 0.4537 | |
| L-FADIR | 3 (14.3%) | 5 (23.8%) | 0.6965 | |
| GPS overall GPS grade 1 GPS grade 2 | 3 (14.3%) 2 (9.5%) 1 (4.8%) | 6 (28.6%) 3 (14.3%) 3 (14.3%) | 0.4789 |
| Parameter | Treatment Group Delta | Control Group Delta | Difference between Groups | p-Value |
|---|---|---|---|---|
| L-BKFO | −0.1 [−0.2 to 0] | −0.1 [−0.3 to 0] | 0 [−0.1 to 0.1] | 0.8014 |
| R-BKFO | −0.1 [−0.2 to 0.1] | −0.2 [−0.2 to 0] | 0.1 [−0.1 to 0.2] | 0.4063 |
| L-HAS | 0.2 [0 to 0.4] | 0 [−0.2 to 0.2] | 0.2 [0 to 0.4] | 0.0277 |
| R-HAS | 0.2 [0 to 0.4] | 0 [−0.2 to 0.1] | 0.2 [0 to 0.3] | 0.0944 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cotellessa, F.; Puce, L.; Formica, M.; May, M.C.; Trompetto, C.; Perrone, M.; Bertulessi, A.; Anfossi, V.; Modenesi, R.; Marinelli, L.; et al. Effectiveness of a Preventative Program for Groin Pain Syndrome in Elite Youth Soccer Players: A Prospective, Randomized, Controlled, Single-Blind Study. Healthcare 2023, 11, 2367. https://doi.org/10.3390/healthcare11172367
Cotellessa F, Puce L, Formica M, May MC, Trompetto C, Perrone M, Bertulessi A, Anfossi V, Modenesi R, Marinelli L, et al. Effectiveness of a Preventative Program for Groin Pain Syndrome in Elite Youth Soccer Players: A Prospective, Randomized, Controlled, Single-Blind Study. Healthcare. 2023; 11(17):2367. https://doi.org/10.3390/healthcare11172367
Chicago/Turabian StyleCotellessa, Filippo, Luca Puce, Matteo Formica, Maria Cesarina May, Carlo Trompetto, Marco Perrone, Andrea Bertulessi, Vittorio Anfossi, Roberto Modenesi, Lucio Marinelli, and et al. 2023. "Effectiveness of a Preventative Program for Groin Pain Syndrome in Elite Youth Soccer Players: A Prospective, Randomized, Controlled, Single-Blind Study" Healthcare 11, no. 17: 2367. https://doi.org/10.3390/healthcare11172367
APA StyleCotellessa, F., Puce, L., Formica, M., May, M. C., Trompetto, C., Perrone, M., Bertulessi, A., Anfossi, V., Modenesi, R., Marinelli, L., Bragazzi, N. L., & Mori, L. (2023). Effectiveness of a Preventative Program for Groin Pain Syndrome in Elite Youth Soccer Players: A Prospective, Randomized, Controlled, Single-Blind Study. Healthcare, 11(17), 2367. https://doi.org/10.3390/healthcare11172367







