Exercise Training in Non-Hospitalized Patients with Post-COVID-19 Syndrome—A Narrative Review
Abstract
1. Introduction
2. Methods
3. Results
3.1. Characteristics and Participants of Included Studies
3.2. Exercise Interventions
3.3. Physical Function
3.4. Symptoms and Patient Reported Outcomes
3.5. Safety
4. Practical Recommendations and Discussion
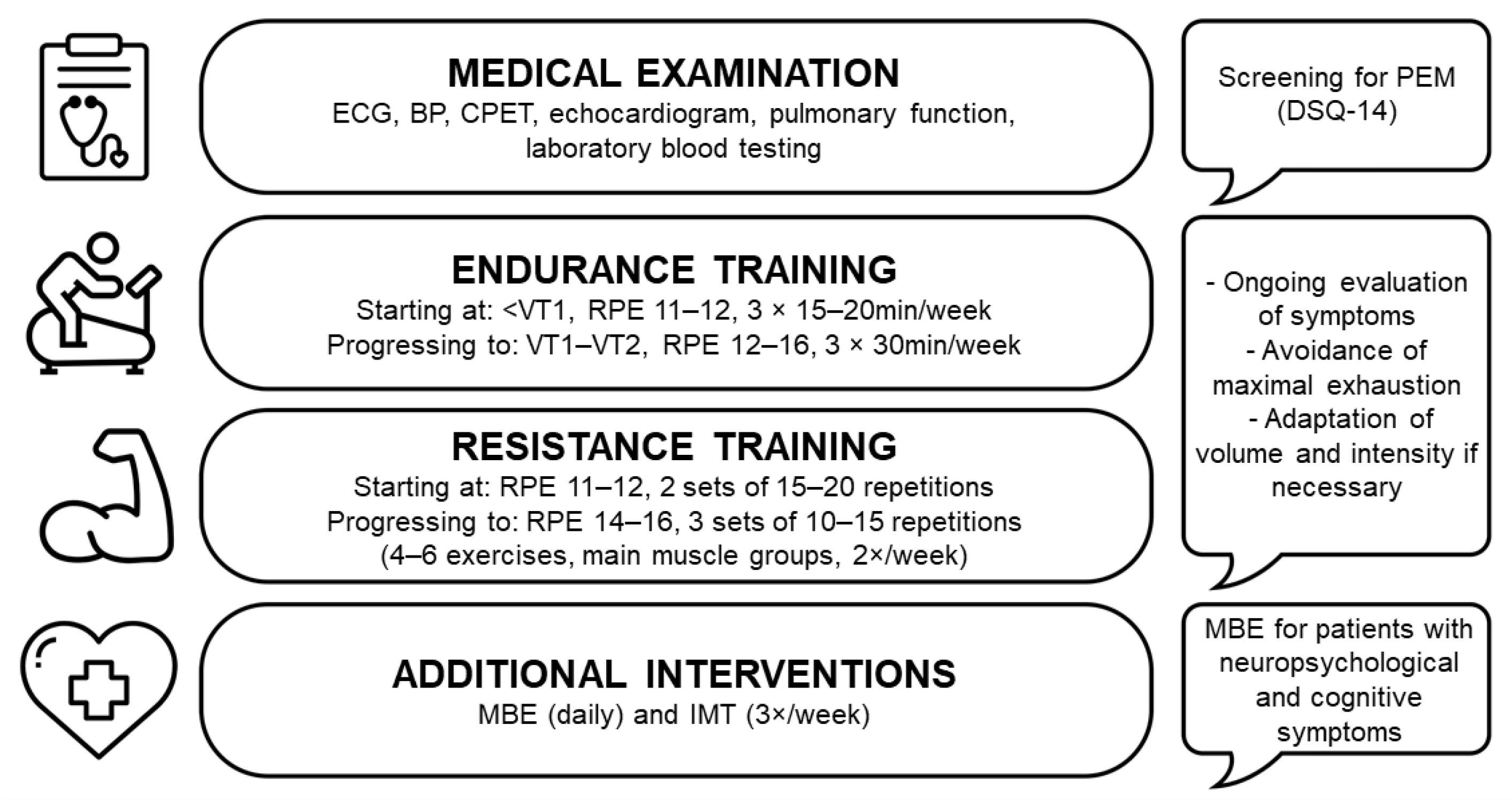
4.1. Medical Examinations
4.2. Exercise Intolerance and ME/CFS
4.3. Rehabilitation Approaches
4.4. Exercise Programs
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Callard, F.; Perego, E. How and why patients made Long Covid. Soc. Sci. Med. 2021, 268, 113426. [Google Scholar] [CrossRef] [PubMed]
- Fernández-de-Las-Peñas, C.; Palacios-Ceña, D.; Gómez-Mayordomo, V.; Cuadrado, M.L.; Florencio, L.L. Defining Post-COVID Symptoms (Post-Acute COVID, Long COVID, Persistent Post-COVID): An Integrative Classification. Int. J. Environ. Res. Public Health 2021, 18, 2621. [Google Scholar] [CrossRef] [PubMed]
- Yong, S.J. Long COVID or post-COVID-19 syndrome: Putative pathophysiology, risk factors, and treatments. Infect. Dis. 2021, 53, 737–754. [Google Scholar] [CrossRef] [PubMed]
- Shah, W.; Hillman, T.; Playford, E.D.; Hishmeh, L. Managing the long term effects of covid-19: Summary of NICE, SIGN, and RCGP rapid guideline. BMJ 2021, 372, n136. [Google Scholar] [CrossRef] [PubMed]
- Alkodaymi, M.S.; Omrani, O.A.; Fawzy, N.A.; Shaar, B.A.; Almamlouk, R.; Riaz, M.; Obeidat, M.; Obeidat, Y.; Gerberi, D.; Taha, R.M.; et al. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2022, 28, 657–666. [Google Scholar] [CrossRef]
- Augustin, M.; Schommers, P.; Stecher, M.; Dewald, F.; Gieselmann, L.; Gruell, H.; Horn, C.; Vanshylla, K.; Cristanziano, V.D.; Osebold, L.; et al. Post-COVID syndrome in non-hospitalised patients with COVID-19: A longitudinal prospective cohort study. Lancet Reg. Health Eur. 2021, 6, 100122. [Google Scholar] [CrossRef]
- Blomberg, B.; Mohn, K.G.; Brokstad, K.A.; Zhou, F.; Linchausen, D.W.; Hansen, B.A.; Lartey, S.; Onyango, T.B.; Kuwelker, K.; Sævik, M.; et al. Long COVID in a prospective cohort of home-isolated patients. Nat. Med. 2021, 27, 1607–1613. [Google Scholar] [CrossRef] [PubMed]
- Orrù, G.; Bertelloni, D.; Diolaiuti, F.; Mucci, F.; Di Giuseppe, M.; Biella, M.; Gemignani, A.; Ciacchini, R.; Conversano, C. Long-COVID Syndrome? A Study on the Persistence of Neurological, Psychological and Physiological Symptoms. Healthcare 2021, 9, 575. [Google Scholar] [CrossRef] [PubMed]
- Scherlinger, M.; Felten, R.; Gallais, F.; Nazon, C.; Chatelus, E.; Pijnenburg, L.; Mengin, A.; Gras, A.; Vidailhet, P.; Arnould-Michel, R.; et al. Refining “Long-COVID” by a Prospective Multimodal Evaluation of Patients with Long-Term Symptoms Attributed to SARS-CoV-2 Infection. Infect. Dis. Ther. 2021, 10, 1747–1763. [Google Scholar] [CrossRef] [PubMed]
- O’Mahoney, L.L.; Routen, A.; Gillies, C.; Ekezie, W.; Welford, A.; Zhang, A.; Karamchandani, U.; Simms-Williams, N.; Cassambai, S.; Ardavani, A.; et al. The prevalence and long-term health effects of Long Covid among hospitalised and non-hospitalised populations: A systematic review and meta-analysis. EClinicalMedicine 2023, 55, 101762. [Google Scholar] [CrossRef]
- Kamal, M.; Abo Omirah, M.; Hussein, A.; Saeed, H. Assessment and characterisation of post-COVID-19 manifestations. Int. J. Clin. Pract. 2021, 75, e13746. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, A.; Nirantharakumar, K.; Hughes, S.; Myles, P.; Williams, T.; Gokhale, K.M.; Taverner, T.; Chandan, J.S.; Brown, K.; Simms-Williams, N.; et al. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat. Med. 2022, 28, 1706–1714. [Google Scholar] [CrossRef] [PubMed]
- Sudre, C.H.; Murray, B.; Varsavsky, T.; Graham, M.S.; Penfold, R.S.; Bowyer, R.C.; Pujol, J.C.; Klaser, K.; Antonelli, M.; Canas, L.S.; et al. Attributes and predictors of long COVID. Nat. Med. 2021, 27, 626–631. [Google Scholar] [CrossRef]
- Lemes, I.R.; Smaira, F.I.; Ribeiro, W.J.D.; Favero, N.K.; Matos, L.; Pinto, A.L.S.; Dolan, E.; Gualano, B. Acute and post-acute COVID-19 presentations in athletes: A systematic review and meta-analysis. Br. J. Sports Med. 2022, 56, 941–947. [Google Scholar] [CrossRef]
- Vollrath, S.; Bizjak, D.A.; Zorn, J.; Matits, L.; Jerg, A.; Munk, M.; Schulz, S.V.W.; Kirsten, J.; Schellenberg, J.; Steinacker, J.M. Recovery of performance and persistent symptoms in athletes after COVID-19. PLoS ONE 2022, 17, e0277984. [Google Scholar] [CrossRef] [PubMed]
- Brito, G.M.; do Prado, D.M.L.; Rezende, D.A.; de Matos, L.; Loturco, I.; Vieira, M.L.C.; de Sá Pinto, A.L.; Alô, R.O.B.; de Albuquerque, L.C.A.; Bianchini, F.R.; et al. The utility of cardiopulmonary exercise testing in athletes and physically active individuals with or without persistent symptoms after COVID-19. Front. Med. 2023, 10, 1128414. [Google Scholar] [CrossRef] [PubMed]
- Stavrou, V.T.; Kyriaki, A.; Vavougios, G.D.; Fatouros, I.G.; Metsios, G.S.; Kalabakas, K.; Karagiannis, D.; Daniil, Z.; Gourgoulianis, K.I.; Βasdekis, G. Athletes with mild post-COVID-19 symptoms experience increased respiratory and metabolic demands: A cross-sectional study. Sports Med. Health Sci. 2023, 5, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Castanares-Zapatero, D.; Chalon, P.; Kohn, L.; Dauvrin, M.; Detollenaere, J.; Maertens de Noordhout, C.; Primus-de Jong, C.; Cleemput, I.; Van den Heede, K. Pathophysiology and mechanism of long COVID: A comprehensive review. Ann. Med. 2022, 54, 1473–1487. [Google Scholar] [CrossRef]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef]
- Ramakrishnan, R.K.; Kashour, T.; Hamid, Q.; Halwani, R.; Tleyjeh, I.M. Unraveling the Mystery Surrounding Post-Acute Sequelae of COVID-19. Front. Immunol. 2021, 12, 686029. [Google Scholar] [CrossRef]
- Yong, S.J.; Liu, S. Proposed subtypes of post-COVID-19 syndrome (or long-COVID) and their respective potential therapies. Rev. Med. Virol. 2022, 32, e2315. [Google Scholar] [CrossRef] [PubMed]
- Jason, L.A.; Dorri, J.A. ME/CFS and Post-Exertional Malaise among Patients with Long COVID. Neurol. Int. 2022, 15, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Poenaru, S.; Abdallah, S.J.; Corrales-Medina, V.; Cowan, J. COVID-19 and post-infectious myalgic encephalomyelitis/chronic fatigue syndrome: A narrative review. Ther. Adv. Infect. Dis. 2021, 8, 20499361211009385. [Google Scholar] [CrossRef] [PubMed]
- Reina-Gutiérrez, S.; Torres-Costoso, A.; Martínez-Vizcaíno, V.; Núñez de Arenas-Arroyo, S.; Fernández-Rodríguez, R.; Pozuelo-Carrascosa, D.P. Effectiveness of Pulmonary Rehabilitation in Interstitial Lung Disease, Including Coronavirus Diseases: A Systematic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2021, 102, 1989–1997.e3. [Google Scholar] [CrossRef]
- Chen, Z.; Lan, W.; Yang, G.; Li, Y.; Ji, X.; Chen, L.; Zhou, Y.; Li, S. Exercise Intervention in Treatment of Neuropsychological Diseases: A Review. Front. Psychol. 2020, 11, 569206. [Google Scholar] [CrossRef] [PubMed]
- Chandan, J.S.; Brown, K.R.; Simms-Williams, N.; Bashir, N.Z.; Camaradou, J.; Heining, D.; Turner, G.M.; Rivera, S.C.; Hotham, R.; Minhas, S.; et al. Non-Pharmacological Therapies for Post-Viral Syndromes, Including Long COVID: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 3477. [Google Scholar] [CrossRef]
- Jimeno-Almazán, A.; Pallarés, J.G.; Buendía-Romero, Á.; Martínez-Cava, A.; Franco-López, F.; Sánchez-Alcaraz Martínez, B.J.; Bernal-Morel, E.; Courel-Ibáñez, J. Post-COVID-19 Syndrome and the Potential Benefits of Exercise. Int. J. Environ. Res. Public Health 2021, 18, 5329. [Google Scholar] [CrossRef]
- Araújo, B.T.S.; Barros, A.; Nunes, D.T.X.; Remígio de Aguiar, M.I.; Mastroianni, V.W.; de Souza, J.A.F.; Fernades, J.; Campos, S.L.; Brandão, D.C.; Dornelas de Andrade, A. Effects of continuous aerobic training associated with resistance training on maximal and submaximal exercise tolerance, fatigue, and quality of life of patients post-COVID-19. Physiother. Res. Int. 2023, 28, e1972. [Google Scholar] [CrossRef]
- Daynes, E.; Gerlis, C.; Chaplin, E.; Gardiner, N.; Singh, S.J. Early experiences of rehabilitation for individuals post-COVID to improve fatigue, breathlessness exercise capacity and cognition—A cohort study. Chronic Respir. Dis. 2021, 18, 14799731211015691. [Google Scholar] [CrossRef]
- Li, J.; Xia, W.; Zhan, C.; Liu, S.; Yin, Z.; Wang, J.; Chong, Y.; Zheng, C.; Fang, X.; Cheng, W.; et al. A telerehabilitation programme in post-discharge COVID-19 patients (TERECO): A randomised controlled trial. Thorax 2022, 77, 697–706. [Google Scholar] [CrossRef]
- Chen, H.; Shi, H.; Liu, X.; Sun, T.; Wu, J.; Liu, Z. Effect of Pulmonary Rehabilitation for Patients With Post-COVID-19: A Systematic Review and Meta-Analysis. Front. Med. 2022, 9, 837420. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi Hekmatikar, A.H.; Ferreira Júnior, J.B.; Shahrbanian, S.; Suzuki, K. Functional and Psychological Changes after Exercise Training in Post-COVID-19 Patients Discharged from the Hospital: A PRISMA-Compliant Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 2290. [Google Scholar] [CrossRef]
- Haunhorst, S.; Bloch, W.; Wagner, H.; Ellert, C.; Krüger, K.; Vilser, D.C.; Finke, K.; Reuken, P.; Pletz, M.W.; Stallmach, A.; et al. Long COVID: A narrative review of the clinical aftermaths of COVID-19 with a focus on the putative pathophysiology and aspects of physical activity. Oxf. Open Immunol. 2022, 3, iqac006. [Google Scholar] [CrossRef]
- Schwendinger, F.; Knaier, R.; Radtke, T.; Schmidt-Trucksäss, A. Low Cardiorespiratory Fitness Post-COVID-19: A Narrative Review. Sports Med. 2023, 53, 51–74. [Google Scholar] [CrossRef]
- Nopp, S.; Moik, F.; Klok, F.A.; Gattinger, D.; Petrovic, M.; Vonbank, K.; Koczulla, A.R.; Ay, C.; Zwick, R.H. Outpatient Pulmonary Rehabilitation in Patients with Long COVID Improves Exercise Capacity, Functional Status, Dyspnea, Fatigue, and Quality of Life. Respiration 2022, 101, 593–601. [Google Scholar] [CrossRef] [PubMed]
- Ostrowska, M.; Rzepka-Cholasińska, A.; Pietrzykowski, Ł.; Michalski, P.; Kosobucka-Ozdoba, A.; Jasiewicz, M.; Kasprzak, M.; Kryś, J.; Kubica, A. Effects of Multidisciplinary Rehabilitation Program in Patients with Long COVID-19: Post-COVID-19 Rehabilitation (PCR SIRIO 8) Study. J. Clin. Med. 2023, 12, 420. [Google Scholar] [CrossRef]
- Jimeno-Almazán, A.; Franco-López, F.; Buendía-Romero, Á.; Martínez-Cava, A.; Sánchez-Agar, J.A.; Sánchez-Alcaraz Martínez, B.J.; Courel-Ibáñez, J.; Pallarés, J.G. Rehabilitation for post-COVID-19 condition through a supervised exercise intervention: A randomized controlled trial. Scand. J. Med. Sci. Sports 2022, 32, 1791–1801. [Google Scholar] [CrossRef] [PubMed]
- Jimeno-Almazán, A.; Buendía-Romero, Á.; Martínez-Cava, A.; Franco-López, F.; Sánchez-Alcaraz, B.J.; Courel-Ibáñez, J.; Pallarés, J.G. Effects of a concurrent training, respiratory muscle exercise, and self-management recommendations on recovery from post-COVID-19 conditions: The RECOVE trial. J. Appl. Physiol. 2023, 134, 95–104. [Google Scholar] [CrossRef]
- Estebanez-Pérez, M.J.; Pastora-Bernal, J.M.; Martín-Valero, R. The Effectiveness of a Four-Week Digital Physiotherapy Intervention to Improve Functional Capacity and Adherence to Intervention in Patients with Long COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 9566. [Google Scholar] [CrossRef]
- Smith, J.L.; Deighton, K.; Innes, A.Q.; Holl, M.; Mould, L.; Liao, Z.; Doherty, P.; Whyte, G.; King, J.A.; Deniszczyc, D.; et al. Improved clinical outcomes in response to a 12-week blended digital and community-based long-COVID-19 rehabilitation programme. Front. Med. 2023, 10, 1149922. [Google Scholar] [CrossRef]
- Hasenoehrl, T.; Palma, S.; Huber, D.F.; Kastl, S.; Steiner, M.; Jordakieva, G.; Crevenna, R. Post-COVID: Effects of physical exercise on functional status and work ability in health care personnel. Disabil. Rehabil. 2022, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.L.; Bonikowske, A.R.; Olson, T.P. Optimizing Outcomes in Cardiac Rehabilitation: The Importance of Exercise Intensity. Front. Cardiovasc. Med. 2021, 8, 734278. [Google Scholar] [CrossRef] [PubMed]
- Evaristo, S.; Moreira, C.; Lopes, L.; Oliveira, A.; Abreu, S.; Agostinis-Sobrinho, C.; Oliveira-Santos, J.; Póvoas, S.; Santos, R.; Mota, J. Muscular fitness and cardiorespiratory fitness are associated with health-related quality of life: Results from labmed physical activity study. J. Exerc. Sci. Fit. 2019, 17, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Machado, F.V.C.; Meys, R.; Delbressine, J.M.; Vaes, A.W.; Goërtz, Y.M.J.; van Herck, M.; Houben-Wilke, S.; Boon, G.; Barco, S.; Burtin, C.; et al. Construct validity of the Post-COVID-19 Functional Status Scale in adult subjects with COVID-19. Health Qual. Life Outcomes 2021, 19, 40. [Google Scholar] [CrossRef] [PubMed]
- Salman, D.; Vishnubala, D.; Le Feuvre, P.; Beaney, T.; Korgaonkar, J.; Majeed, A.; McGregor, A.H. Returning to physical activity after covid-19. BMJ 2021, 372, m4721. [Google Scholar] [CrossRef]
- Gervasi, S.F.; Pengue, L.; Damato, L.; Monti, R.; Pradella, S.; Pirronti, T.; Bartoloni, A.; Epifani, F.; Saggese, A.; Cuccaro, F.; et al. Is extensive cardiopulmonary screening useful in athletes with previous asymptomatic or mild SARS-CoV-2 infection? Br. J. Sports Med. 2021, 55, 54–61. [Google Scholar] [CrossRef]
- Hughes, D.C.; Orchard, J.W.; Partridge, E.M.; La Gerche, A.; Broderick, C. Return to exercise post-COVID-19 infection: A pragmatic approach in mid-2022. J. Sci. Med. Sport 2022, 25, 544–547. [Google Scholar] [CrossRef] [PubMed]
- Cattadori, G.; Di Marco, S.; Baravelli, M.; Picozzi, A.; Ambrosio, G. Exercise Training in Post-COVID-19 Patients: The Need for a Multifactorial Protocol for a Multifactorial Pathophysiology. J. Clin. Med. 2022, 11, 2228. [Google Scholar] [CrossRef] [PubMed]
- Durstenfeld, M.S.; Sun, K.; Tahir, P.; Peluso, M.J.; Deeks, S.G.; Aras, M.A.; Grandis, D.J.; Long, C.S.; Beatty, A.; Hsue, P.Y. Use of Cardiopulmonary Exercise Testing to Evaluate Long COVID-19 Symptoms in Adults: A Systematic Review and Meta-analysis. JAMA Netw. Open 2022, 5, e2236057. [Google Scholar] [CrossRef]
- Thompson, P.D.; Arena, R.; Riebe, D.; Pescatello, L.S. ACSM’s new preparticipation health screening recommendations from ACSM’s guidelines for exercise testing and prescription, ninth edition. Curr. Sports Med. Rep. 2013, 12, 215–217. [Google Scholar] [CrossRef]
- Fairbank, R. Long COVID exercise trials proposed by NIH raise alarm. Nature 2023, 616, 228–229. [Google Scholar] [CrossRef]
- Davis, H.E.; Assaf, G.S.; McCorkell, L.; Wei, H.; Low, R.J.; Re’em, Y.; Redfield, S.; Austin, J.P.; Akrami, A. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 2021, 38, 101019. [Google Scholar] [CrossRef]
- Twomey, R.; DeMars, J.; Franklin, K.; Culos-Reed, S.N.; Weatherald, J.; Wrightson, J.G. Chronic Fatigue and Postexertional Malaise in People Living With Long COVID: An Observational Study. Phys. Ther. 2022, 102, pzac005. [Google Scholar] [CrossRef] [PubMed]
- Cotler, J.; Holtzman, C.; Dudun, C.; Jason, L.A. A Brief Questionnaire to Assess Post-Exertional Malaise. Diagnostics 2018, 8, 66. [Google Scholar] [CrossRef] [PubMed]
- Murdock, K.W.; Wang, X.S.; Shi, Q.; Cleeland, C.S.; Fagundes, C.P.; Vernon, S.D. The utility of patient-reported outcome measures among patients with myalgic encephalomyelitis/chronic fatigue syndrome. Qual. Life Res. 2017, 26, 913–921. [Google Scholar] [CrossRef] [PubMed]
- Twisk, F.N.; Maes, M. A review on cognitive behavorial therapy (CBT) and graded exercise therapy (GET) in myalgic encephalomyelitis (ME)/chronic fatigue syndrome (CFS): CBT/GET is not only ineffective and not evidence-based, but also potentially harmful for many patients with ME/CFS. Neuro Endocrinol. Lett. 2009, 30, 284–299. [Google Scholar]
- Parker, M.; Sawant, H.B.; Flannery, T.; Tarrant, R.; Shardha, J.; Bannister, R.; Ross, D.; Halpin, S.; Greenwood, D.C.; Sivan, M. Effect of using a structured pacing protocol on post-exertional symptom exacerbation and health status in a longitudinal cohort with the post-COVID-19 syndrome. J. Med. Virol. 2023, 95, e28373. [Google Scholar] [CrossRef]
- Dowman, L.; Hill, C.J.; May, A.; Holland, A.E. Pulmonary rehabilitation for interstitial lung disease. Cochrane Database Syst. Rev. 2021, 2, Cd006322. [Google Scholar] [CrossRef]
- Ahmed, I.; Mustafaoglu, R.; Yeldan, I.; Yasaci, Z.; Erhan, B. Effect of Pulmonary Rehabilitation Approaches on Dyspnea, Exercise Capacity, Fatigue, Lung Functions, and Quality of Life in Patients With COVID-19: A Systematic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2022, 103, 2051–2062. [Google Scholar] [CrossRef]
- Anderson, L.; Oldridge, N.; Thompson, D.R.; Zwisler, A.D.; Rees, K.; Martin, N.; Taylor, R.S. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease: Cochrane Systematic Review and Meta-Analysis. J. Am. Coll. Cardiol. 2016, 67, 1–12. [Google Scholar] [CrossRef]
- Biazus-Sehn, L.F.; Schuch, F.B.; Firth, J.; Stigger, F.S. Effects of physical exercise on cognitive function of older adults with mild cognitive impairment: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2020, 89, 104048. [Google Scholar] [CrossRef]
- Dauwan, M.; Begemann, M.J.H.; Slot, M.I.E.; Lee, E.H.M.; Scheltens, P.; Sommer, I.E.C. Physical exercise improves quality of life, depressive symptoms, and cognition across chronic brain disorders: A transdiagnostic systematic review and meta-analysis of randomized controlled trials. J. Neurol. 2021, 268, 1222–1246. [Google Scholar] [CrossRef] [PubMed]
- Buoite Stella, A.; Furlanis, G.; Frezza, N.A.; Valentinotti, R.; Ajcevic, M.; Manganotti, P. Autonomic dysfunction in post-COVID patients with and witfhout neurological symptoms: A prospective multidomain observational study. J. Neurol. 2022, 269, 587–596. [Google Scholar] [CrossRef] [PubMed]
- McNarry, M.A.; Berg, R.M.G.; Shelley, J.; Hudson, J.; Saynor, Z.L.; Duckers, J.; Lewis, K.; Davies, G.A.; Mackintosh, K.A. Inspiratory muscle training enhances recovery post-COVID-19: A randomised controlled trial. Eur. Respir. J. 2022, 60, 2103101. [Google Scholar] [CrossRef] [PubMed]
- Ammous, O.; Feki, W.; Lotfi, T.; Khamis, A.M.; Gosselink, R.; Rebai, A.; Kammoun, S. Inspiratory muscle training, with or without concomitant pulmonary rehabilitation, for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst. Rev. 2023, 1, Cd013778. [Google Scholar] [CrossRef]
- Norweg, A.; Yao, L.; Barbuto, S.; Nordvig, A.S.; Tarpey, T.; Collins, E.; Whiteson, J.; Sweeney, G.; Haas, F.; Leddy, J. Exercise intolerance associated with impaired oxygen extraction in patients with long COVID. Respir. Physiol. Neurobiol. 2023, 313, 104062. [Google Scholar] [CrossRef]
- Guntur, V.P.; Nemkov, T.; de Boer, E.; Mohning, M.P.; Baraghoshi, D.; Cendali, F.I.; San-Millán, I.; Petrache, I.; D’Alessandro, A. Signatures of Mitochondrial Dysfunction and Impaired Fatty Acid Metabolism in Plasma of Patients with Post-Acute Sequelae of COVID-19 (PASC). Metabolites 2022, 12, 1026. [Google Scholar] [CrossRef]
- MacInnis, M.J.; Gibala, M.J. Physiological adaptations to interval training and the role of exercise intensity. J. Physiol. 2017, 595, 2915–2930. [Google Scholar] [CrossRef]
- Fluge, Ø.; Tronstad, K.J.; Mella, O. Pathomechanisms and possible interventions in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). J. Clin. Investig. 2021, 131. [Google Scholar] [CrossRef]
- Rayhan, R.U.; Baraniuk, J.N. Submaximal Exercise Provokes Increased Activation of the Anterior Default Mode Network During the Resting State as a Biomarker of Postexertional Malaise in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Front. Neurosci. 2021, 15, 748426. [Google Scholar] [CrossRef]
- Westcott, W.L. Resistance training is medicine: Effects of strength training on health. Curr. Sports Med. Rep. 2012, 11, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Grgic, J.; Schoenfeld, B.J.; Orazem, J.; Sabol, F. Effects of resistance training performed to repetition failure or non-failure on muscular strength and hypertrophy: A systematic review and meta-analysis. J. Sport Health Sci. 2022, 11, 202–211. [Google Scholar] [CrossRef] [PubMed]
- Hickmott, L.M.; Chilibeck, P.D.; Shaw, K.A.; Butcher, S.J. The Effect of Load and Volume Autoregulation on Muscular Strength and Hypertrophy: A Systematic Review and Meta-Analysis. Sports Med. Open 2022, 8, 9. [Google Scholar] [CrossRef]
- Lovegrove, S.; Hughes, L.J.; Mansfield, S.K.; Read, P.J.; Price, P.; Patterson, S.D. Repetitions in Reserve Is a Reliable Tool for Prescribing Resistance Training Load. J. Strength Cond. Res. 2022, 36, 2696–2700. [Google Scholar] [CrossRef] [PubMed]
| Author | Type of Study | Subjects | Physical Function Outcomes | Patient Reported Outcomes | Conclusion of Authors |
|---|---|---|---|---|---|
| Nopp et al. [35] | Prospective observational cohort study | n = 58 (25 females); 46.8 ± 12.6 years; 4.4 ± 2.0 months post COVID-19.; 62.0% non-hospitalized; among hospitalized: average length of stay 19.6 days, 11 severe and 11 critical cases | Maximal workload ↑ 6MWT ↑ STS ↑ | mMRC ↓ PCFS ↓ FAS ↓ EQ-5D index score ↔ EQ-5D VAS ↑ | Significant improvements in exercise capacity, symptoms and quality of life |
| Ostrowska et al. [36] | Prospective observational single-center study | n = 97 (53 females); 60 (50–68) years; 3–12 months post COVID-19; 60.8% non-hospitalized; among hospitalized 24.7% with respiratory failure | VO2peak ↔ 6MWT ↑ STS ↑ SPPB ↑ | mMRC ↓ MFIS ↓ | Significant improvements in symptoms and physical capacity in a majority of patients after rehabilitation |
| Jimeno-Almazán et al. [37] | RCT (CT vs. self-management rehabilitation recommendations) | n = 39 (29 females); 45.2 ± 9.5 years; 33 ± 20.5 weeks post COVID-19; non-hospitalized | estimated VO2max ↑* (EX) STS ↑* (EX & C) BP ↑* (EX) HSQ ↑* (EX & C) Handgrip ↔ Leg extension ↔ | mMRC ↓ (EX & C) ↔* PCFS ↓* (EX & C) CFQ-11 ↓* (EX) FSS ↓* (EX) SF-12 PA ↑* (EX) MH ↔* GAD-7 ↓ (EX & C) ↔* PHQ-9 ↓* (EX & C) DSQ-14 ↔ | Significant improvements in health and performance markers after exercise compared to rehabilitation recommendations |
| Jimeno-Almazán et al. [38] | RCT (CT vs. RM vs. CTRM vs. self-management rehabilitation recommendations) | n = 80 (55 females); 45.3 ± 8.0 years; 39.3 ± 23.3 weeks post COVID-19; non-hospitalized | estimated VO2max ↑ (CT & CTRM) ↔* BP ↑* (CT & CTRM) HSQ ↑ (CT & CTRM) ↔* Handgrip ↔ | mMRC ↓ (CT & CTRM) ↔* PCFS ↓ (CT) ↔* FSS ↓* CFS ↓* (CT&CTRM) SF-12 PA ↑ (CT, CTRM & RM) ↔* SF-12 MH ↑ (CTRM) ↔* GAD-7 ↓ (CTRM) ↔* PHQ-9 ↓* (CT & CTRM) | Significant improvements in fitness, symptom severity and health status after concurrent training with and without inspiratory muscle training |
| Estebanez-Pérez et al. [39] | Quasi-experimental pre–post study | n = 32 (23 females); 45.9 ± 10.7 years; >12 weeks post COVID; 90.6% non-hospitalized; among hospitalized 2 out of 3 admitted to ICU | STS ↑ SPPB ↑ | N/A | Significant improvements in functional capacity and high adherence rate |
| Smith et al. [40] | Prospective interventional trial | n = 601 (465 females); 47.0 ± 10.0 years; 9.8 ± 5.0 months post COVID-19; 86.7% non-hospitalized; among hospitalized average length of stay 10 days, 16.5% admitted to ICU | STS ↑ DASI ↑ | D-12 ↓ WHO-5 ↑ EQ-5D-5L ↑ EQ-5D VAS ↑ | Significant and clinically meaningful improvements in dyspnea, functional capacity, mental wellbeing and HR-QoL |
| Hasenoehrl et al. [41] | Intervention trial with two parallel groups (MSG vs. SSG) | n = 28 (22 females); 45.8 ± 11.0 years; 6.1 ± 3.1 months post COVID-19; no information about hospitalization | VO2peak ↑ (SSG only) 6MWT ↑ STS ↑ | PCFS ↓ BFI ↓ GAD-7 ↓ PHQ-9 ↓ PSS-10↓ BRS ↔ | Significant improvements of physical fitness and psychological outcomes, higher benefit for SSG |
| Author | Type of Intervention | Duration and Frequency | Type and Intensity of Exercise |
|---|---|---|---|
| Nopp et al. [35] | Multi-professional outpatient rehabilitation | 6 weeks; 3×/week | Endurance, strength and inspiratory muscle training according to the Austrian guidelines for outpatient pulmonary rehabilitation |
| Ostrowska et al. [36] | Multidisciplinary outpatient rehabilitation | 6 weeks; 3×/week | Aerobic, resistance and breathing exercises |
| Jimeno-Almazán et al. [37] | Multicomponentexercise program | 8 weeks; 3×/week | Resistance exercises with 3 × 8 repetitions; moderate intensity variable training (70–80%/55–65% HRR); light intensity continuous training (65–70% HRR); |
| Jimeno-Almazán et al. [38] | Multicomponent exercise program with and without inspiratory muscle training | 8 weeks; 3×/week | Resistance exercises with 3 × 8 repetitions; moderate intensity variable training (70–80%/55–65% HRR); light intensity continuous training (65–70% HRR); |
| Estebanez-Pérez et al. [39] | Personalized digital physiotherapy | 4 weeks; 3–5×/week | Progressive strength training (1–3 muscle groups, 8–12 repetitions, load increase by 5–10%/week); additionally recommended: walking, jogging or swimming at low intensities |
| Smith et al. [40] | Blended community rehabilitation program | 12 weeks; 3×/week | Combination of cardiovascular, strength-based, and mobility exercises; intensity and volume prescribed according to participants’ functional capacity |
| Hasenoehrl et al. [41] | Supervised resistance exercise and unsupervised endurance exercise | 8 weeks, 5×/week | Bodyweight and resistance band exercises, 30–60 s repetition maximum (low-intensity high-repetition); aerobic training 3 × 20 min at VT1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sick, J.; König, D. Exercise Training in Non-Hospitalized Patients with Post-COVID-19 Syndrome—A Narrative Review. Healthcare 2023, 11, 2277. https://doi.org/10.3390/healthcare11162277
Sick J, König D. Exercise Training in Non-Hospitalized Patients with Post-COVID-19 Syndrome—A Narrative Review. Healthcare. 2023; 11(16):2277. https://doi.org/10.3390/healthcare11162277
Chicago/Turabian StyleSick, Johanna, and Daniel König. 2023. "Exercise Training in Non-Hospitalized Patients with Post-COVID-19 Syndrome—A Narrative Review" Healthcare 11, no. 16: 2277. https://doi.org/10.3390/healthcare11162277
APA StyleSick, J., & König, D. (2023). Exercise Training in Non-Hospitalized Patients with Post-COVID-19 Syndrome—A Narrative Review. Healthcare, 11(16), 2277. https://doi.org/10.3390/healthcare11162277






