Ultrasound Imaging of Subtalar Joint Instability for Chronic Ankle Instability
Abstract
1. Introduction
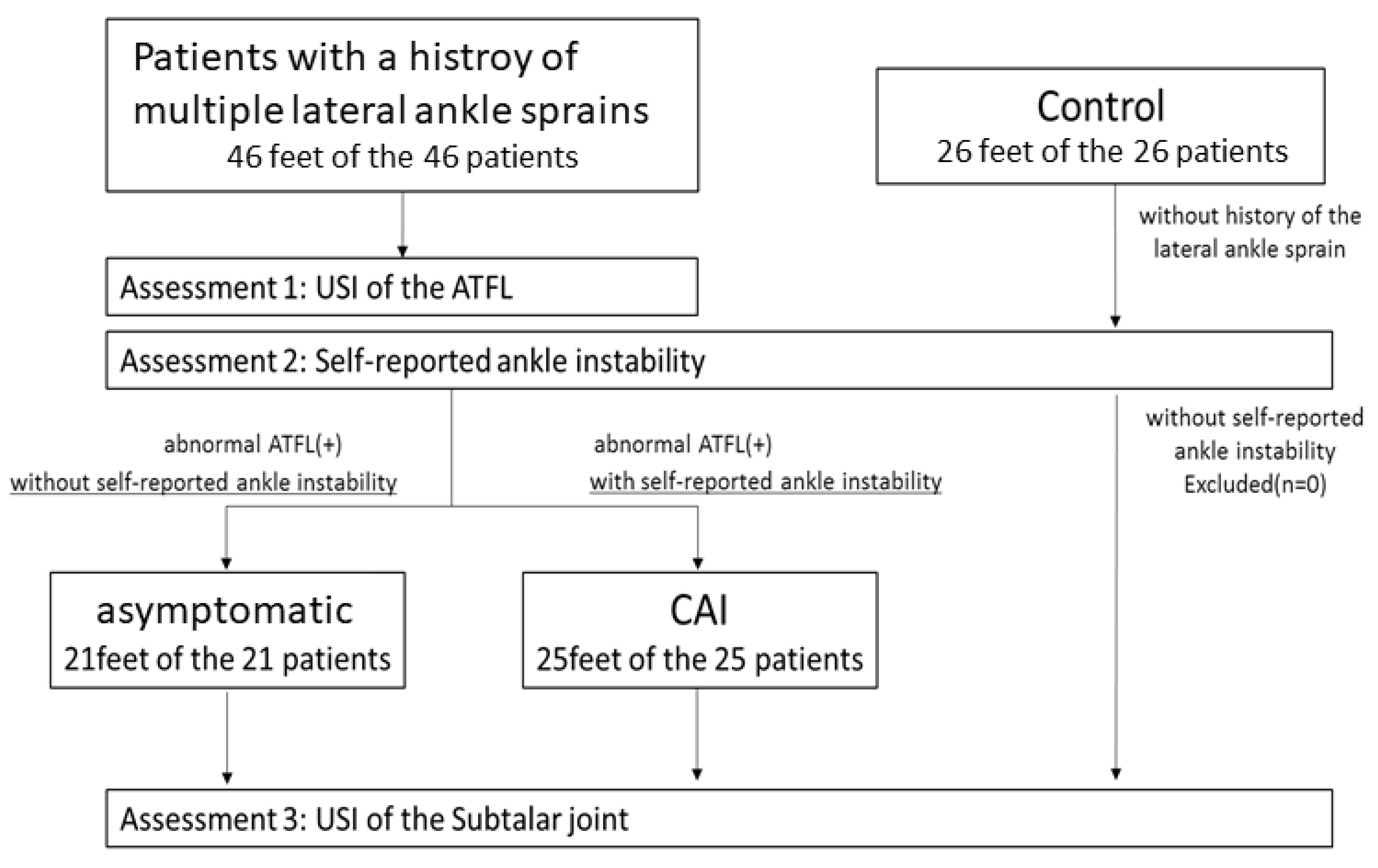
2. Materials and Methods
2.1. Participants
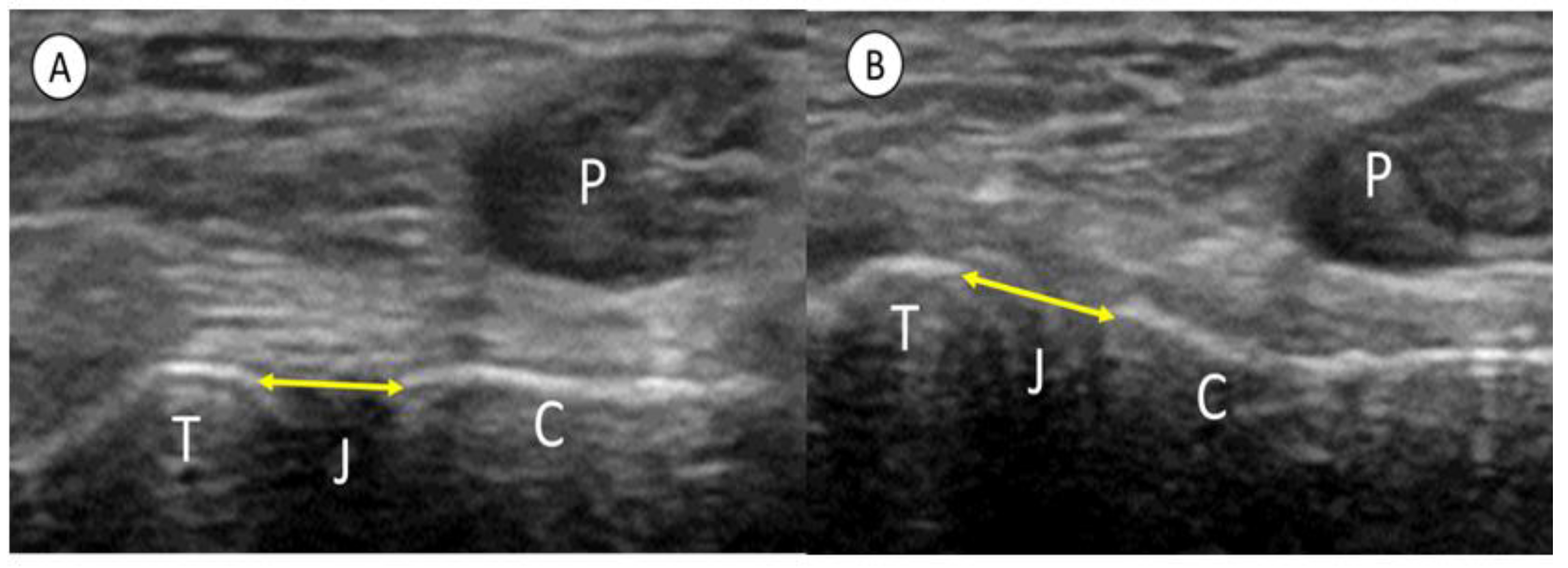
2.2. Procedures
2.3. Reliability Assessment
2.4. Statistical Analysis
3. Results
3.1. Differences in General Characteristics among the Three Groups
3.2. Reliability
3.3. Comparisons among the Three Groups
3.4. Correlation between STJE and Subjective Ankle Instability
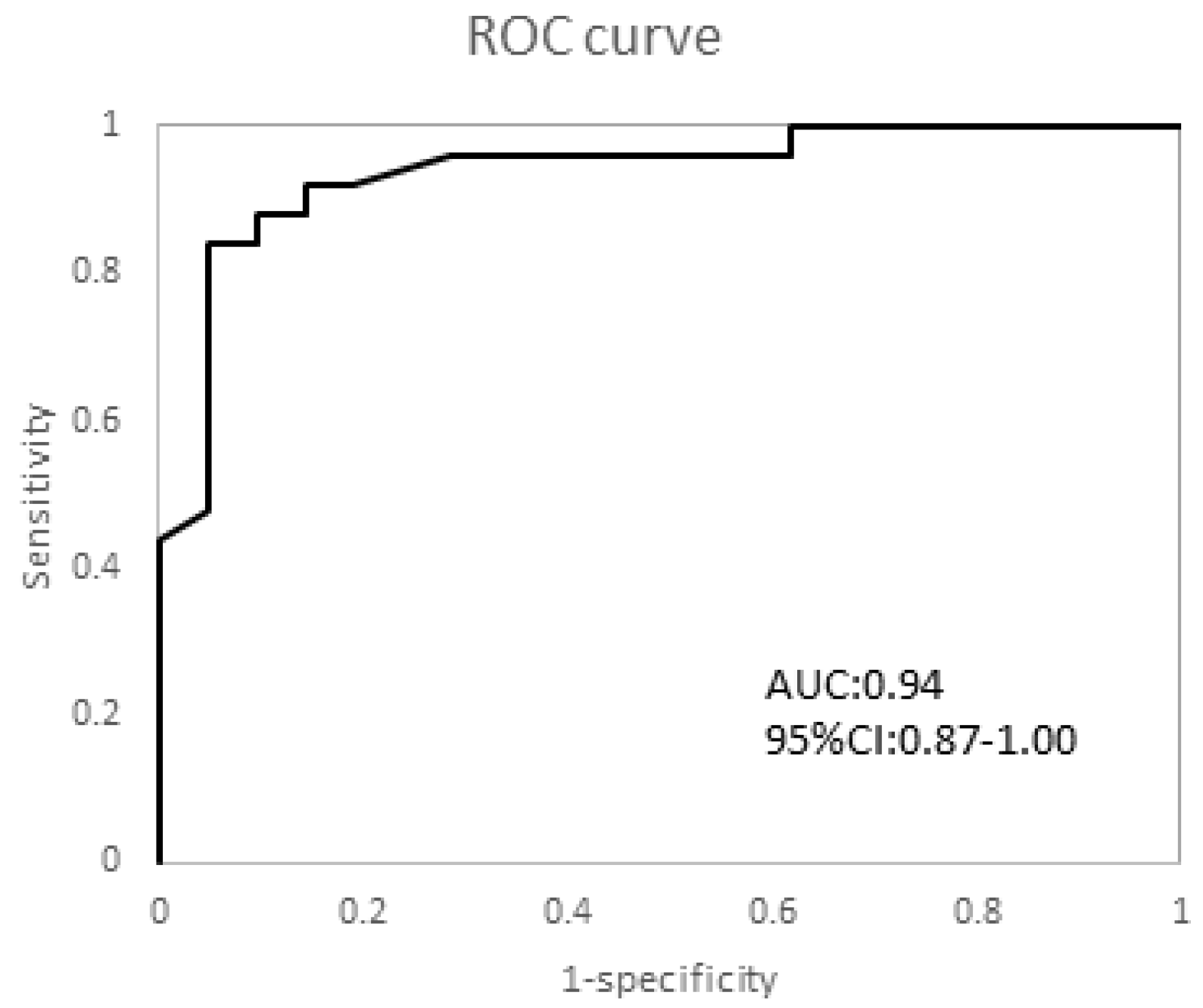
3.5. Cut-Off Value
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kobayashi, T.; Gamada, K. Lateral Ankle Sprain and Chronic Ankle Instability: A Critical Review. Foot Ankle Spec. 2014, 7, 298–326. [Google Scholar] [CrossRef] [PubMed]
- Powden, C.J.; Hoch, J.M.; Hoch, M.C. Rehabilitation and Improvement of Health-Related Quality-of-Life Detriments in Individuals With Chronic Ankle Instability: A Meta-Analysis. J. Athl. Train. 2017, 52, 753–765. [Google Scholar] [CrossRef] [PubMed]
- Michels, F.; Pereira, H.; Calder, J.; Matricali, G.; Glazebrook, M.; Guillo, S.; Karlsson, J.; ESSKA-AFAS Ankle Instability Group; Acevedo, J.; Batista, J.; et al. Searching for consensus in the approach to patients with chronic lateral ankle instability: Ask the expert. Knee Surg. Sports Traumatol. Arthrosc. 2017, 26, 2095–2102. [Google Scholar] [CrossRef]
- Lee, B.H.; Choi, K.-H.; Seo, D.Y.; Choi, S.M.; Kim, G.L. Diagnostic validity of alternative manual stress radiographic technique detecting subtalar instability with concomitant ankle instability. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 1029–1039. [Google Scholar] [CrossRef] [PubMed]
- Tochigi, Y.; Yoshinaga, K.; Wada, Y.; Moriya, H. Acute Inversion Injury of the Ankle: Magnetic Resonance Imaging and Clinical Outcomes. Foot Ankle Int. 1998, 19, 730–734. [Google Scholar] [CrossRef] [PubMed]
- Laurin, C.A.; Ouellet, R.; St-Jacques, R. Talar and subtalar tilt: An experimental investigation. Can. J. Surg. 1968, 11, 270–279. [Google Scholar]
- Krähenbühl, N.; Weinberg, M.W.; Davidson, N.P.; Mills, M.K.; Hintermann, B.; Saltzman, C.L.; Barg, A. Currently used imaging options cannot accurately predict subtalar joint instability. Knee Surg. Sports Traumatol. Arthrosc. 2018, 27, 2818–2830. [Google Scholar] [CrossRef]
- Michels, F.; Clockaerts, S.; Van Der Bauwhede, J.; Stockmans, F.; Matricali, G. Does subtalar instability really exist? A systematic review. Foot Ankle Surg. 2020, 26, 119–127. [Google Scholar] [CrossRef]
- Kim, T.H.; Moon, S.G.; Jung, H.-G.; Kim, N.R. Subtalar instability: Imaging features of subtalar ligaments on 3D isotropic ankle MRI. BMC Musculoskelet. Disord. 2017, 18, 475. [Google Scholar] [CrossRef]
- DeMoss, A.; Millard, N.; McIlvain, G.; Beckett, J.A.; Jasko, J.J.; Timmons, M.K. Ultrasound-Assisted Assessment of Medial Elbow Stability. J. Ultrasound Med. 2018, 37, 2769–2775. [Google Scholar] [CrossRef]
- Rozmaryn, L.M. The Collateral Ligament of the Digits of the Hand: Anatomy, Physiology, Biomechanics, Injury, and Treatment. J. Hand Surg. 2017, 42, 904–915. [Google Scholar] [CrossRef] [PubMed]
- Cao, S.; Wang, C.; Ma, X.; Wang, X.; Huang, J.; Zhang, C. Imaging diagnosis for chronic lateral ankle ligament injury: A systemic review with meta-analysis. J. Orthop. Surg. Res. 2018, 13, 122. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Cai, Y.; Wang, Y. Value of ultrasonography for detecting chronic injury of the lateral ligaments of the ankle joint compared with ultrasonography findings. Br. J. Radiol. 2014, 87, 20130406. [Google Scholar] [CrossRef] [PubMed]
- Edama, M.; Kageyama, I.; Kikumoto, T.; Nakamura, M.; Ito, W.; Nakamura, E.; Hirabayashi, R.; Takabayashi, T.; Inai, T.; Onishi, H. The effects on calcaneofibular ligament function of differences in the angle of the calcaneofibular ligament with respect to the long axis of the fibula: A simulation study. J. Foot Ankle Res. 2017, 10, 60. [Google Scholar] [CrossRef]
- Waldecker, U.; Blatter, G. Sonographic measurement of instability of the subtalar joint. Foot Ankle Int. 2001, 22, 42–46. [Google Scholar] [CrossRef]
- Hua, Y.; Yang, Y.; Chen, S.; Cai, Y. Ultrasound Examination for the Diagnosis of Chronic Anterior Talofibular Ligament Injury. Acta Radiol. 2012, 53, 1142–1145. [Google Scholar] [CrossRef]
- Kunugi, S.; Masunari, A.; Noh, B.; Mori, T.; Yoshida, N.; Miyakawa, S. Cross-cultural adaptation, reliability, and validity of the Japanese version of the Cumberland ankle instability tool. Disabil. Rehabil. 2016, 39, 50–58. [Google Scholar] [CrossRef]
- Hiller, C.E.; Refshauge, K.M.; Bundy, A.C.; Herbert, R.D.; Kilbreath, S.L. The Cumberland Ankle Instability Tool: A Report of Validity and Reliability Testing. Arch. Phys. Med. Rehabil. 2006, 87, 1235–1241. [Google Scholar] [CrossRef]
- Docherty, C.L.; Gansneder, B.M.; Arnold, B.L.; Hurwitz, S.R. Development and reliability of the ankle instability instrument. J. Athl. Train. 2006, 41, 154–158. [Google Scholar]
- Renstrom, P.A.; Konradsen, L. Ankle ligament injuries. Br. J. Sports Med. 1997, 31, 11–20. [Google Scholar] [CrossRef]
- Meyer, J.M.; Garcia, J.; Hoffmeyer, P.; Fritschy, D. The subtalar sprain. A roentgenographic study. Clin. Orthop. Relat. Res. 1988, 226, 169–173. [Google Scholar] [CrossRef]
- Brantigan, J.; Pedegana, L.; Lippert, F. Instability of the subtalar joint. Diagnosis by stress tomography in three cases. J. Bone Jt. Surg. 1977, 59, 321–324. [Google Scholar] [CrossRef]
- Fong, D.T.; Ha, S.C.; Mok, K.M.; Chan, C.W.; Chan, K.M. Kinematics analysis of ankle inversion ligamentous sprain injuries in sports: Five cases from televised tennis competitions. Am. J. Sports Med. 2012, 40, 2627–2632. [Google Scholar] [CrossRef]
- Hertel, J. Functional Anatomy, Pathomechanics, and Pathophysiology of Lateral Ankle Instability. J. Athl. Train. 2002, 37, 364–375. [Google Scholar] [PubMed]
- Tochigi, Y.; Amendola, A.; Rudert, M.J.; Baer, T.E.; Brown, T.D.; Hillis, S.L.; Saltzman, C.L. The Role of the Interosseous Talocalcaneal Ligament in Subtalar Joint Stability. Foot Ankle Int. 2004, 25, 588–596. [Google Scholar] [CrossRef] [PubMed]
- Lundberg, A.; Goldie, I.; Kalin, B.; Selvik, G. Kinematics of the Ankle/Foot Complex: Plantarflexion and Dorsiflexion. Foot Ankle 1989, 9, 194–200. [Google Scholar] [CrossRef]
- Deodato, M.; Coan, L.; Buoite Stella, A.; Ajčević, M.; Martini, M.; Di Lenarda, L.; Ratti, C.; Accardo, A.; Murena, L. Inertial sensors-based assessment to detect hallmarks of chronic ankle instability during single-leg standing: Is the healthy limb “healthy”? Clin. Biomech. 2023, 107, 106036. [Google Scholar] [CrossRef]
- Hertel, J.; Corbett, R.O. An Updated Model of Chronic Ankle Instability. J. Athl. Train. 2019, 54, 572–588. [Google Scholar] [CrossRef]
- Rein, S.; Manthey, S.; Zwipp, H.; Witt, A. Distribution of sensory nerve endings around the human sinus tarsi: A cadaver study. J. Anat. 2014, 224, 499–508. [Google Scholar] [CrossRef]
- Rockar, P.A. The Subtalar Joint: Anatomy and Joint Motion. J. Orthop. Sports Phys. Ther. 1995, 21, 361–372. [Google Scholar] [CrossRef]
- Gribble, P.A.; Delahunt, E.; Bleakley, C.; Caulfield, B.; Docherty, C.L.; Fourchet, F.; Fong, D.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; et al. Selection Criteria for Patients With Chronic Ankle Instability in Controlled Research: A Position Statement of the International Ankle Consortium. J. Orthop. Sports Phys. Ther. 2013, 43, 585–591. [Google Scholar] [CrossRef]
- Pellegrini, M.J.; Glisson, R.R.; Wurm, M.; Ousema, P.H.; Romash, M.M.; Nunley, J.A., 2nd; Easley, M.E. Systematic Quantification of Stabilizing Effects of Subtalar Joint Soft-Tissue Constraints in a Novel Cadaveric Model. J. Bone Jt. Surg. Am. 2016, 98, 842–848. [Google Scholar] [CrossRef] [PubMed]
- Kamiya, T.; Kura, H.; Suzuki, D.; Uchiyama, E.; Fujimiya, M.; Yamashita, T. Mechanical stability of the subtalar joint after lateral ligament sectioning and ankle brace application: A biomechanical experimental study. Am. J. Sport. Med. 2009, 37, 2451–2458. [Google Scholar] [CrossRef]
- Staats, K.; Sabeti-Aschraf, M.; Apprich, S.; Platzgummer, H.; Puchner, S.E.; Holinka, J.; Windhager, R.; Schuh, R. Preoperative MRI is helpful but not sufficient to detect associated lesions in patients with chronic ankle instability. Knee Surg. Sports Traumatol. Arthrosc. 2017, 26, 2103–2109. [Google Scholar] [CrossRef] [PubMed]

| Control | Asymptomatic | CAI | p-Value | |
|---|---|---|---|---|
| 26 persons | 21 persons | 25 persons | ||
| Age (y) | 18.9 ± 7.0 | 21.0 ± 7.4 | 21.2 ± 5.9 | 0.43 |
| Height (cm) | 164.5 ± 7.4 | 166.7 ± 8.8 | 164.3 ± 7.8 | 0.53 |
| Weight (kg) | 59.0 ± 8.8 | 59.7 ± 8.8 | 56.6 ± 8.8 | 0.48 |
| Sex M/F | 9/17 | 9/12 | 7/17 | 0.62 |
| Side (R/L) | 8/18 | 11/10 | 13/11 | 0.17 |
| AIIT | 0.1 ± 1.0 | 3.2 ± 0.9 | 6.3 ± 0.4 | <0.001 * |
| CAIT | 29.4 ± 5.7 | 24.9 ± 4.3 | 14.1 ± 2.0 | <0.01 * |
| Reliability Type | ICC (95%CI) | SEM | MDC95 | |
|---|---|---|---|---|
| STJ rest | Intra-rater | 0.95 (0.89–0.98) | 0.08 (0.06–0.10) | 0.22 |
| Inter-rater | 0.81 (−0.02–0.96) | 0.17 (0.12–0.31) | 0.47 | |
| STJ inversion | Intra-rater | 0.87 (0.73–0.96) | 0.23 (0.19–0.30) | 0.63 |
| Inter-rater | 0.88 (0.31–0.98) | 0.25 (0.17–0.46) | 0.69 | |
| STJE | Intra-rater | 0.84 (0.64–0.98) | 0.13 (0.11–0.17) | 0.36 |
| Inter-rater | 0.95 (0.81–0.98) | 0.14 (0.10–0.27) | 0.39 |
| Control | Asymptomatic | CAI | p-Value | ES (η2) | Post Hoc | ||
|---|---|---|---|---|---|---|---|
| STJ (mm) | |||||||
| rest | 2.1 ± 0.8 | 2.5 ± 0.5 | 2.4 ± 0.6 | <0.05 | 0.03 | Control-CAI Control-asymptomatic asymptomatic-CAI | 0.06 0.13 0.90 |
| inversion | 2.9 ± 0.9 | 3.5 ± 0.7 | 4.7 ± 0.8 | <0.001 | 0.50 | Control-CAI, Control-asymptomatic asymptomatic-CAI | 0.01 <0.001 <0.001 |
| STJE | 0.8 ± 0.2 | 1.0 ± 0.4 | 2.3 ± 0.8 | <0.001 | 0.64 | Control-CAI, Control-asymptomatic asymptomatic-CAI | <0.001 0.18 <0.001 |
| CAIT | AIIT | |
|---|---|---|
| STJ rest | 0.12 | −0.08 |
| STJ inversion | −0.60 * | 0.67 * |
| STJE | −0.71 * | 0.74 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kudo, S.; Aoyagi, T.; Kobayashi, T.; Koshino, Y.; Edama, M. Ultrasound Imaging of Subtalar Joint Instability for Chronic Ankle Instability. Healthcare 2023, 11, 2227. https://doi.org/10.3390/healthcare11152227
Kudo S, Aoyagi T, Kobayashi T, Koshino Y, Edama M. Ultrasound Imaging of Subtalar Joint Instability for Chronic Ankle Instability. Healthcare. 2023; 11(15):2227. https://doi.org/10.3390/healthcare11152227
Chicago/Turabian StyleKudo, Shintarou, Tsutomu Aoyagi, Takumi Kobayashi, Yuta Koshino, and Mutsuaki Edama. 2023. "Ultrasound Imaging of Subtalar Joint Instability for Chronic Ankle Instability" Healthcare 11, no. 15: 2227. https://doi.org/10.3390/healthcare11152227
APA StyleKudo, S., Aoyagi, T., Kobayashi, T., Koshino, Y., & Edama, M. (2023). Ultrasound Imaging of Subtalar Joint Instability for Chronic Ankle Instability. Healthcare, 11(15), 2227. https://doi.org/10.3390/healthcare11152227






