Abstract
Background: Fostering a culture of clinical effectiveness among healthcare professionals (HCPs) is crucial to achieving optimal patient health outcomes. To our knowledge, there is a lack of robust evidence-based practice (EBP) tools to assess the competence of HCPs in EBP in the Eastern Mediterranean Region (EMR). Aim: This study aims to comprehensively investigate the construct validity and internal reliability of the evidence-based practice questionnaire (EBPQ) among HCPs in the EMR. Methods: This multinational and multi-disciplinary cross-sectional study was conducted between 27 April and 11 May 2023. Convenience and snowball sampling methods were used to recruit a sample of HCPs (physicians, nurses, physiotherapists, dentists, and pharmacists) using an electronic survey questionnaire for data capture. To assess the reliability of the instrument, Cronbach’s alpha, inter-item reliability, and split-half reliability analyses were conducted. Furthermore, the convergent and discriminant validity of the questionnaire was ensured by calculating the average variance extracted (AVE) and the correlation coefficient between the different constructs, respectively. Factor loadings and cross-loadings of different indicators within each construct were calculated by performing both exploratory and confirmatory factor analyses. Results: A total of 1536 HCPs from 18 countries in the EMR (response rate = 96.786%) with a median age of 28 years participated; 47% were female, and 55% had Arabic as their first language. English was the most common language for a bachelor’s degree in science (54%). The construct validity of the EBPQ was investigated using exploratory factor analysis (EFA), which yielded four loaded factors. The confirmatory factor analysis (CFA) confirmed the four loaded factors. The CFA model showed that the root mean square error of approximation = 0.066, comparative fit index = 0.95, Tucker–Lewis’s index = 0.94, standardized root mean square residual = 0.033, normal fit index = 0.94, goodness of fit = 0.91, and χ2 test statistic= 22,553, with p < 0.001. The AVE values of the four factors were close to 1 (knowledge = 0.6, practice = 0.6, attitude = 0.5, and sharing = 0.7), thus supporting the convergent validity of the EBPQ. The four domains had Cronbach’s alpha coefficients and Omega ≥ 0.7 (knowledge = 0.9, practice = 0.9, attitude = 0.7, and sharing = 0.8), suggesting that the items within each domain had good internal consistency. These results support the discriminant validity of the EBPQ. Conclusions: The EBPQ is a robust questionnaire that can be completed in less than 10 min by EMR HCPs and can be used as a gold-standard questionnaire to collect valid data on the attitudes, knowledge, and proficiency of HCPs in making clinical decisions based on evidence. Future studies are recommended to investigate the retest reliability.
1. Introduction
Implementing evidence-based practice (EBP) according to international standards not only ensures the delivery of optimal care to clients [1] but also equips healthcare professionals (HCPs) with a problem-solving approach that enhances the quality of the provided health services [2]. The delivery of consistent and high-quality healthcare services is a major challenge for healthcare systems [3]. There is global recognition of integrating EBP in decision making in health [4,5] and non-health fields [6], which enables individuals to enhance their critical thinking skills, make informed decisions, and practice based on a wide range of trustworthy evidence from multiple reliable sources [6].
EBP initially emerged in medicine as a response to address the practice gap and reduce overreliance on clinical expertise alone in clinical decision making. It aims to shift the focus toward a more reliable and evidence-based approach, where decisions are informed by trustworthy evidence rather than solely relying on individual expertise [6]. In the 1990s, researchers from McMaster University introduced the term EBM, and in 1996, it was defined as a systemic approach to analyze published research as the basis of clinical decision making [7]. Later, Sacket et al. formally defined EBM as ‘the conscientious, explicit, and judicious use of the current best evidence in making decisions about the care of individual patients [8]. Evidence-based medicine (EBM) has been used in various forms such as EBP, evidence-based care (EBC), evidence-based health (EBH), and evidence-based nursing (EBN). However, they share the common premise that patient care should be guided by robust and reliable evidence [9]. The definition of EBP in the nursing profession has evolved from a strict clinical basis to a more holistic approach, based on the full spectrum of nursing research and practice, considering the values of individuals, clinical judgment, ethics and legislation, clinical experience, and practice environments [9]. Therefore, in our study, we used the term EBP to be more applicable to HCPs, regardless of their specialty.
Indeed, fostering a culture of clinical effectiveness among HCPs is crucial to achieve optimal patient health outcomes. Recognizing the significance of EBP, it has been declared an essential element of the health education curriculum [10,11]. Research has shown that a well-developed EBP course can improve undergraduate attitudes toward applying EBP after graduation. The EBP course equips undergraduate students with the necessary knowledge, skills, and confidence to engage in evidence-based decision making in their future practice [12].
Despite the potential benefits of EBP, its application remains limited in many healthcare settings especially in the Eastern Mediterranean Region (EMR) [13]. The EMR faces numerous challenges, including critical deficits in human resource development, resources, and research training. These limitations hinder the translation of the research into policy and practice. One of the key factors contributing to this issue is the weakness of institutional and financial inducements within the research and development systems [13].
In the rapidly evolving healthcare field, it is vital to regularly assess the attitudes, skills, and knowledge of HCPs regarding EBP. This ongoing evaluation helps us to identify obstacles and challenges that enable appropriate actions to be taken. Moreover, determining HCPs’ readiness and willingness to implement EBP is crucial for sustaining a culture of EBP [14]. Given the lack of evidence concerning the competence of HCPs in the EMR regarding EBP and the perceived barriers to its adoption in clinical decision making, it is essential to conduct a large survey among HCPs in the EMR. Our study is part of a multinational project in the EMR, which aims to identify the barriers facing EBP implementation in the region. Therefore, it was essential to search and find a well-constructed and reliable scale that can achieve our study objectives.
Several EBP scales have been developed, including the Health Sciences Evidence-Based Practice questionnaire (HS-EBP) (60 items) [15], Evidence-based Practice Competence Questionnaire (EBP-COQ) (25 items) [16], McEvoy trans-professional instrument of evidence-based practice profile (EBP2) (49 items) questionnaire [17], Competencies, Beliefs, Facilitators, Barriers, Implementation of Evidence-Based Practice (EBP-CBFRI) (55 items) [18], and Evidence-Based Practice Questionnaire (EBPQ) (24 items) [19]. However, while some are too long [15,17,18], available in Spanish [15,16], and for nursing students [16], the EBPQ is a concise and comprehensive tool in English [19]. Moreover, the EBPQ contains all the EBP domains, which makes it a widely used tool among HCPs [20,21,22]. However, in the EMR, the validity and reliability of the EBPQ among HCPs have not been reported yet until the current study, which could provide essential new information about the attitude and competence of HCPs in the EMR regarding EBP.
Since most EMR countries speak Arabic as their first language and study the degree of health sciences in English, it was appropriate to administer the EBPQ in its original language (English) to investigate its validity and reliability. Additionally, the EBP is a model that is used globally under the same themes, terms, and processes, and it is taught and administered in English among HCPs in the majority of EMR countries. Therefore, it is logical to administer the EBPQ in its original language without translation in order to assess its validity and reliability before use in the main project.
Aim
This study thoroughly examined the construct validity and internal reliability of the EBPQ (English version) among EMR HCPs.
2. Construct Validity and Internal Reliability of the EBPQ
This study was conducted in the following three phases.
2.1. Phase-1: Ensuring Face and Content Validity of the EBPQ
A panel of experts of eight HCPs, who were specialists in medicine, nursing, and pharmacology, was invited to check and provide feedback on the content, readability, and understandability of the EBPQ (English version). As shown in Table A1, the panel committee was selected from three of the EMR regions, and their first language is not English, but they studied for their undergraduate degree in English as participants from Egypt and Pakistan, and one from a country where the health sciences are taught in Arabic, but they use English as a second language, like a panel member from Syria. The panel reported that the questionnaire items were clear, simple, and understandable and that they were familiar with them. As a result, there was no change in the EBPQ’s words or sentence structure, and they approved of its face and content validity.
2.2. Phase-2: Conducting the Cognitive Debriefing by Pilot Sample
We sent an electronic version of the English EBPQ to 26 HCPs from 13 countries (Afghanistan, Djibouti, Egypt, Jordan, Lebanon, Libya, Morocco, Pakistan, Saudi Arabia, Somalia, Syrian Arab Republic, Tunisia, and Yemen) via WhatsApp, requesting them to complete the questionnaire and report its clarity, readability, understandability, and the time taken to complete it. All participants completed the questionnaire within 3–6 min. All participants considered the questionnaire to be easy to read, clear, and relevant. None of the participants suggested any modification.
2.3. Phase-3: Assessment of the Validity and Reliability of the EBPQ
Construct validity and internal reliability of the EBPQ were investigated using a cross-sectional survey. The ‘Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)’ was followed while conducting this study [23].
3. Materials and Methods
3.1. Design and Setting
A multinational cross-sectional study was conducted from 27 April to 11 May 2023 to recruit a representative and suitable sample from the EMR countries to investigate the construct validity and internal reliability of the EBPQ.
3.2. Population and Sampling Method
Convenience and snowball sampling methods were used to recruit a sample of HCPs (physicians, nurses, physiotherapists, dentists, and pharmacists) who met the following eligibility criteria for participation: age ≥ 18 years, HCPs (in the internship year or post-graduation), residence/work in an EMR country during the data collection period, and agreed to fill out the electronic questionnaire.
3.3. Sample Size
The sample size calculation depended on the number of questions included in the validation (24 items) and the estimated Cronbach’s alpha, with a 95% confidence interval. The equation suggested by Bonett (2002) [24] was used to calculate the sample size: n = {8k/(k − 1)}{Z critical/ln((1 − pk − e/2)/(1 − pk + e/2))}^2 + 2, where n is the sample size, k is the number of the questions used in the validation, Z critical is the critical value of the Z score at a significance level of 5%, pk is the estimated Cronbach’s alpha level, and e is the absolute difference between the upper and lower bounds of the confidence interval of the estimated alpha level. It was estimated that the alpha level is 0.7 (acceptable level), the absolute difference in CI (e) is 0.2, and after substitution in the equation, the sample size would be n = (8 × 24/23) ((1.96/ln (2))^2 + 2 = 8.4 × 8 + 2 = 69 participants per each of the EMR countries. In total, 1587 HCPs from 18 countries in the EMR accessed the questionnaire, and 51 refused to participate, ending with 1536 actual participants (a response rate of 96.786%). Our sample was larger than the computed size, which could also be used to run a confirmatory factor analysis test.
3.4. Instruments
The electronic survey used to collect data included two questionnaires.
3.4.1. Sheet of Background Data about the Participants
This part of the questionnaire consisted of nine questions about the demographic and academic characteristics of the participants and training in EBP (i.e., age, gender, country of residence, first language, highest education degree, field of practice, language of the Bachelor of Science, current work status, and type of hospital where their current training or work was conducted). In addition, four questions were used to collect data about HCP training in EBP, as recommended by [16]: (1) studying the EBP course in college before graduation, (2) attending training in EBP, (3) number of studies carried out in the last three years, and (4) number of research articles that they read in the last month. For participants with a native language other than English, an additional item was added to evaluate whether their ability in English is a barrier to using research-based evidence, as recommended by [25].
3.4.2. The Evidence-Based Practice Questionnaire (EBPQ)
The EBPQ measures knowledge, skills, and attitudes toward EBP. It includes 24 items comprising three subscales: (i) self-reported practice or use of EBP (practice subscale) (6 items), (ii) EBP attitudes (attitude subscale) (4 items), and (iii) EBP knowledge and skills (knowledge subscale) (14 items) [19]. All items were rated on a Likert scale ranging from 1 to 7. The instrument score was calculated by adding the response values to each question, giving a total of 168 points, with higher scores indicating more positive attitudes toward EBP [26]. The practice (42 points), attitude (28 points), and knowledge (98 points) subscales were used in this study. The instrument had a Cronbach’s alpha of 0.87 and satisfactory convergent validity (p < 0.001) [19]. A previous study showed that the Cronbach’s alpha of different sections of the questionnaire ranged from 0.7 to 0.9 among academic nursing educators in Egypt and Jordan [27].
3.5. Recruitment Method
An anonymous electronic self-administered survey using the ‘Google Form’ was generated. The link to the electronic survey was then sent to colleagues in the health field of each of the targeted countries. They were invited to complete the questionnaire and send it to their colleagues via WhatsApp and other social media platforms. The participants were able to fill out the questionnaire only one time.
3.6. Ethical Considerations
The Institutional Review Board (IRB) exempted the study (IRB Log Number: 23-0421) as it posed minimal risk to the participants. The purpose of the study was presented on the survey cover page. Anonymity was ensured by not collecting identifiable personal data, such as names and workplace names, and by ensuring that their data were confidentially protected and that the collected data would only be accessed by the study researcher. The confidentiality of the participants was also ensured by only using the coded responses while analyzing the results of the survey. Participants were informed that they had the right to withdraw from the study without any consequences and that their participation was voluntary. The collected data were protected by saving them on a secured laptop which was only available to the researchers.
3.7. Data Analysis
Statistical analyses were performed using IBM SPSS version 26 (IBM SPSS, Armonk, NY, USA). Descriptive statistics were used to determine the frequency, prevalence, percentage, mean, and standard deviation. The Shapiro–Wilk test was used to check the normality of continuous data. As all continuous data did not follow parametric assumptions, they were described using medians and interquartile ranges. All categorical variables were described as counts and percentages. An independent t-test was performed to compare the EBP domains between groups who experienced difficulties in the English language and those who did not, as well as between those who took EBP courses at the university and those who did not. The internal consistency of the questionnaire was assessed by calculating the Cronbach’s alpha, inter-item correlations, and split-half reliability. The acceptable alpha levels start from 0.7, and when the levels reach closer to 1, the internal consistency is better explained [28]. To assess convergent validity, the average variance extracted (AVE), which is the average variance in indicator variables explained by a construct, was calculated. If the AVE is greater than or equal to 0.5, convergent validity is confirmed [29]. Discriminant validity was assessed by calculating the correlation coefficients between the different constructs. Discriminant validity was ensured when the correlations were not statistically significant. Factor loadings and cross-loadings were produced using exploratory factor analysis (EFA). Confirmatory factor analysis (CFA) was performed to verify the overall factor structure and calculate the significance level of the loadings. R software (version 4.1.1) was used to calculate the model fit of the CFA that was used to assess the construct validity of the questionnaire. Statistical significance was set at p < 0.05.
4. Results
4.1. Characteristics of HCPs
A total of 1536 HCPs participated in this study, with a median age of 28 years (range 25–32 years). Of the total participants, 47% were female, and nearly half (55%) had Arabic as their first language. The distribution of education degrees shows that 9.4% had a doctoral degree, 27% had a master’s degree, 47% had a bachelor’s degree, and 16% were still in their internship years. The participants had diverse fields of practice, with dentistry (18%), medicine (36%), nursing (21%), pharmacy (13%), and health and rehabilitation sciences (12%) being the main areas. English was the most common language for a bachelor’s degree in science (54%), followed by Arabic (17%).
Nearly two-thirds (58%) of the participants worked full-time, 29% worked part-time, and 12% were not currently working (on vacation, retired, or volunteering). The median number of work experiences reported by the participants was four (2–7) years. Participants worked or were trained in various types of hospitals, including public/teaching/government hospitals (39%), private hospitals (23%), private and public hospitals (22%), and others (16%) (Table 1).

Table 1.
Sociodemographic characteristics (N = 1536).
4.2. Experience of HCPs in Research and EBP
A total of 52% had studied EBP in college before graduation, whereas 55% had attended EBP training. The median number of research studies conducted in the last three years was 1.0 (0.0–3.0). Additionally, participants read a median of two research articles in the last month (0–5). A total of 52.6% (n = 808) reported that the research articles in English were not difficult to read, whereas the rest (n = 728, 47.4%) reported that it was difficult (Table 1).
4.3. Reliability and Divergent Validity of the EBPQ
Descriptive statistics, Cronbach’s alpha, item-total score correlation, and split-half reliability for each domain are presented in Table 2.

Table 2.
Reliability and divergent validity of the Evidence-Based Practice Questionnaire (EBPQ) and its three domains.
The practice domain consisted of six items (P1–P5). The raw alpha coefficient for each item in the practice domain was 0.8, indicating good internal consistency. The item-total domain correlation ranged from 0.6 to 0.7, suggesting that the items were moderately correlated with the overall domain (convergent validity). The overall Cronbach’s alpha for the practice domain was 0.86 (with a 95% CI: 0.85–0.87), indicating high internal consistency. The split-half reliability was 0.8, indicating a high level of internal consistency between the two halves of the questionnaire. The Spearman–Brown correction was 0.9, suggesting that if the questionnaire length increased or decreased, the reliability of the measure would remain relatively stable (Table 2).
The attitude domain included three items (A1–A3). The raw alpha coefficient for each item of the attitude domain ranged from 0.6 to 0.7, indicating acceptable internal consistency. The item-total domain correlation ranged from 0.5 to 0.6, indicating moderate correlations with the overall domain (convergent validity). The overall Cronbach’s alpha for the attitude domain was 0.74 (with a 95% confidence interval of 0.72–0.76), suggesting good internal consistency. The split-half reliability was 0.6, and the Spearman–Brown correction was 0.7 (Table 2).
The knowledge domain comprised 13 items (K1–K13). The raw alpha coefficient for each item in the knowledge domain was 0.9, indicating excellent internal consistency. The item-total domain correlation ranged from 0.7 to 0.8, indicating strong correlations with the overall domain (convergent validity). The overall Cronbach’s alpha for the knowledge domain was 0.95 (with a 95% confidence interval of 0.94–0.95), indicating high internal consistency. The split-half reliability was 0.9, and the Spearman–Brown correction was 0.9 (Table 2).
Three items were removed from the EBPQ, which had a high uniqueness value (r > 0.6): (1) item 6 of the practice ‘shared this information with colleagues’, (2) item 1 of the attitude ‘My workload is too great for me to keep up to date with all the new evidence’, and (3) item 14 of knowledge ‘Ability to review your own practice’.
4.4. Construct Validity of the EBPQ
4.4.1. Exploratory Factor Analysis
The ‘Kaiser–Meyer–Olkin factor adequacy and Bartlett test’ showed that the overall measure of sampling adequacy (MSA) was 0.97, suggesting that the data used in the factor analysis were highly suitable for conducting the analysis. The MSA values were closer to 1, indicating that the variables in the analysis were highly correlated and provided a good basis for factor extraction. The Bartlett test was <0.05, indicating rejection of the null hypothesis, as there was a significant correlation among the variables. Factor analysis revealed that four factors (Factor 1, Factor 2, Factor 3, and Factor 4) were extracted. Factor 1 had relatively high loadings for items K1–K11. Factor 2 had relatively high loadings for items P1–P4. Factor 3 showed high loadings for items A1–A3. Factor 4 had high loadings for items K12–K13. The uniqueness values of the items ranged from 0.3 to 0.6, indicating that each item had a moderate-to-high level of uniqueness (Table 3).

Table 3.
Factor loadings and uniqueness of the EBPQ items.
4.4.2. Confirmatory Factor Analysis (CFA)
Construct validity and model fit measures were investigated using confirmatory factor analysis (CFA). The fit of the model was evaluated using several indicators: root mean square error of approximation (RMSEA = 0.066), comparative fit index (CFI = 0.95), Tucker–Lewis index (TLI = 0.94), standardized root mean square residual (SRMR = 0.033), normal fit index (NFI = 0.94), goodness of fit (GFI = 0.91), and χ2 test statistic = 22,553 with 210 degrees of freedom and p < 0.001 (Figure 1 and Figure 2).
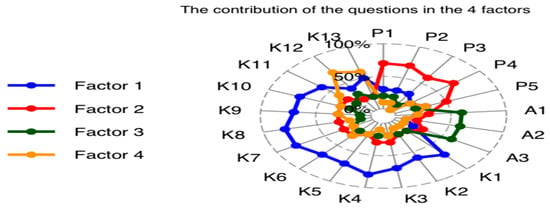
Figure 1.
Radar plot to show the factor loadings.
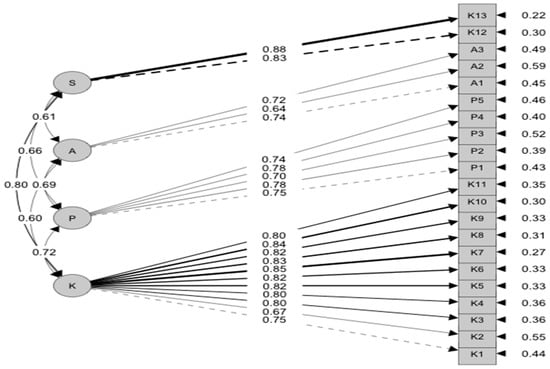
Figure 2.
Confirmatory factor analysis.
4.4.3. Convergent Validity of EBPQ
The AVE is a measure of convergent validity that represents the average amount of variance captured by the items within each variable. The AVE values ranged from 0 to 1, with higher values indicating stronger convergent validity (knowledge = 0.6, practice = 0.6, attitude = 0.5, and sharing = 0.7). These values suggest that the items within each variable capture moderate-to-high variance, which supports convergent validity.
4.5. The Internal Reliability
The four domains had Cronbach’s alpha coefficients and Omega ≥ 0.7 (knowledge = 0.9, practice = 0.9, attitude = 0.7, and sharing = 0.8), suggesting that the items within each domain had good internal consistency. Omega is another measure of internal consistency reliability that showed values for the four domains similar to the alpha values, which indicates that the EBPQ has a strong internal consistency.
4.6. Divergent (Discriminant) Validity
The correlation between the four domains using the Pearson method showed that the correction between knowledge and practice was −0.5, and between knowledge and attitude, it was −0.6, indicating a moderately negative relationship. The correlation between practice and attitude was −0.2, indicating a weak negative relationship. The correlations between sharing and the other three domains (knowledge, practice, and attitude) were relatively weak and non-significant (0.1, −0.4, −0.1, respectively). These findings indicate that the EBPQ has good divergent validity.
4.7. Known Group Validity
Known group validity is the ability of a questionnaire to discriminate between groups that are known to have significant differences. We hypothesized that the mean scores on the EBPQ subscales would be significantly lower among participants who had fewer years of work experience, had experienced difficulty in English research articles, read fewer research articles, and did not receive EBP training before graduation. The results in Table 4 and Table 5 support the discriminant validity of the EBPQ.

Table 4.
Comparison of EBP between groups who experienced difficulty in English and those who studied the EBP course in college.

Table 5.
Correlation between the EBPQ domains and other variables.
5. Discussion
Our study is the first to investigate the construct validity and internal reliability of the EBPQ among HCPs in the EMR. The original EBPQ was developed in English to assess United Kingdom (UK) nurses’ knowledge, skills, and attitudes toward EBP [19]. The EBPQ is a short questionnaire that is widely used to evaluate attitudes, knowledge, and skills of EBP [20,21,22,27]. This makes it an appropriate tool that can be used as a standardized questionnaire to compare the attitudes, knowledge, skills, and practice of EBP by HCPs in EMR countries because the majority of HCPs in the EMR use English as a secondary language in health sciences colleges and clinical practice. Thus, the original version of the EBPQ was applied without translation into Arabic. We assume that HCPs should be well-prepared to adopt EBP in clinical decision making and that they must critically understand the scientific research and guidelines that are usually available in English.
5.1. Construct Validity
First, the 24 items of the EBPQ were tested for uniqueness using a correlation test. Three items were removed from the EBPQ, as they had a high correlational value that decreased the construct validity of the tool. When the 21 items were entered into the EFA, four factors were extracted, and the CFA proved that Factor 1: Knowledge, Factor 2: Practice, Factor 3: Attitude, and Factor 4: Sharing. The fourth newly extracted domain had two items that were loaded under knowledge in the original EBPQ: (1) item 12 ‘Share of ideas and information with colleagues’ and (2) item 13 ‘Dissemination of new ideas about care to colleagues’. This finding makes sense since these two items assess the same construct related to the sharing and dissemination of research ideas and are not related to the ‘knowledge domain’ as in the original EBPQ. Therefore, the fourth domain was labeled as ‘sharing EBP’. This finding proved the internal stability and construct validity of the EBPQ among the study participants. Therefore, the final version of our EBPQ had 21 items that could be integrated into four domains.
5.2. Divergent Validity of the EBPQ
Our findings indicated that the EBPQ had good discriminant validity, as it could differ between groups that were hypothesized to have different attitudes, knowledge, skills, and sharing. For example, our findings showed that HCPs who experienced difficulty with English research articles had lower EBPQ scores than those who reported no difficulty. Furthermore, the mean score for sharing research ideas (domain 4) significantly increased with increasing age, work experience, previous study of EBP courses, the number of research articles they published, and the number of research articles they read. In addition, scores for the attitude domain significantly increased with increasing age and work experience. Interestingly, scores for the practice domain increased significantly with an increase in reading research articles and previous study of EBP. This finding is important because it reflects the necessity of reading more research articles which, at the same time, requires high English proficiency and the importance of impeding EBP courses in the undergraduate curriculum. Attitude varies significantly with age and experience but not with the number of research studies carried out or the number of research articles read. This finding supports that our study participants have a good attitude toward EBP regardless of whether they have research experience; however, this experience seems necessary to improve their attitude toward EBP. In the United Arab Emirates, older nurses with more years of experience and higher education levels had significantly higher mean EBP scores. In addition, gender is significantly linked to practice and knowledge [30].
The critical factor significantly associated with practice, skill, and sharing was the number of research articles read. A recent systematic review concluded that research training is an important factor in practice-based research among pharmacists [31]. In Qatar, post-graduate qualifications were associated with readiness to practice research after adjusting for gender and time since the completion of the undergraduate study [32]. These findings support the importance of practicing research through reading and engaging in research activities to enhance practice-based research.
5.3. Internal Reliability
Descriptive statistics, Cronbach’s alpha, item-total score correlation, and split-half reliability were calculated for each domain. Cronbach’s alpha showed that the EBPQ reliability for the attitude, practice, and knowledge domains (ranging from 0.74 to 0.95, respectively) exceeded the set criteria, indicating its high internal consistency, which was almost higher or similar to that of a previous study [19,33,34].
However, attitude had the lowest Cronbach’s value, similar to the original study by Upton and Upton [19], even in a study that translated and tested the same tool among Indonesians, where its overall Cronbach’s α was 0.92 (with α of practice = 0.81, attitude = 0.81, and knowledge = 0.94) [21].
6. Conclusions
Our study showed that the EBPQ may be a useful scale that can be used among HCPs in the EMR, especially those who study health sciences in English. The EBPQ is a robust and self-administered questionnaire that can be completed in 10 min by EMR HCPs. Therefore, the EBPQ can be used by health researchers and policymakers as a gold-standard questionnaire to collect valid data on the attitudes, knowledge, and proficiency of HCPs in making clinical decisions based on evidence to improve the quality of healthcare. Moreover, it can be used to compare EMR countries and evaluate the effectiveness of EBP training programs.
7. Limitations and Recommendations
Our study is the first to evaluate the validity and reliability of the English EBPQ among a large sample of HCPs from five general health fields in EMR countries, which makes our study a valuable contribution to the existing literature. However, several limitations of this study should be considered in the future. First, since our study recruited the sample using an anonymous electronic survey, participants who could understand English were more willing to fill out the questionnaire than those who could not. Therefore, the English version of the EBPQ is unsuitable for HCPs who do not speak English. Therefore, future studies are needed to translate and adapt the EBPQ to EMR HCPs, who have limitations in the English language. Second, although we recruited a sample larger than the calculated size from 18 countries, using a nonrandom method may limit the generalizability of the study findings to all HCPs in the EMR. Third, investigating the retest reliability was impossible because collecting personal information, such as email, was prohibited to maintain the confidentiality of the participants. Therefore, a future study is recommended to investigate retest reliability, as this was not examined in the present study.
Author Contributions
Study design and conceptualization: N.Y.; Data collection: N.Y., A.G. and R.M.G.; Data management N.Y. and M.S.; Data analysis: N.Y. and M.S.; Interpretation and visualization: N.Y., M.S. and R.M.G.; Resources: N.Y.; First-draft writing: N.Y.; Critical review and editing of the manuscript: N.Y., M.S. and R.M.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The Institutional Review Board (IRB) at Princess Nourah bint Abdulrahman University exempted the study (IRB Log Number: 23-0421) as it posed minimal risk to the participants. All participants provided written informed consent before completing the survey. This study was conducted in accordance with the principles of the Declaration of Helsinki.
Informed Consent Statement
Permission to use the EBPQ was obtained from Professor Upton.
Data Availability Statement
Data can be obtained from the corresponding author by email.
Acknowledgments
This study was supported by the Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2023R177), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia. The authors thank the HCPs who provided their time and completed the survey. The authors also express their deepest gratitude to the Global Researcher Club (https://globalresearcherclub.org)—an international non-profit scientific research community for their support during the data collection process, which was arranged by the co-author (A.G.).
Conflicts of Interest
No conflict of interest to disclose.
Appendix A

Table A1.
Characteristics of the panel committee.
Table A1.
Characteristics of the panel committee.
| Country | Specialty (No) | First Language | Second Language | Undergraduate Study Language |
|---|---|---|---|---|
| Egypt | Medicines (2) | Arabic | English | English |
| Nursing (3) | ||||
| Pharmacy (1) | ||||
| Syria | Medicine (1) | Arabic | English | Arabic |
| Pakistan | Medicine (1) | Ordo | English | English |
References
- Lyons, C.; Brown, T.; Tseng, M.H.; Casey, J.; McDonald, R. Evidence-based practice and research utilisation: Perceived research knowledge, attitudes, practices and barriers among Australian paediatric occupational therapists. Aust. Occup. Ther. J. 2011, 58, 178–186. [Google Scholar] [CrossRef]
- Grimshaw, J.; Eccles, M.; Thomas, R.; MacLennan, G.; Ramsay, C.; Fraser, C.; Vale, L. Toward evidence-based quality improvement: Evidence (and its limitations) of the effectiveness of guideline dissemination and implementation strategies 1966–1998. J. Gen. Intern. Med. 2006, 21, S14–S20. [Google Scholar]
- Shortell, S.M.; Rundall, T.G.; Hsu, J. Improving patient care by linking evidence-based medicine and evidence-based management. JAMA 2007, 298, 673–676. [Google Scholar] [CrossRef] [PubMed]
- Akkawi, F.; Suleiman, S.; Alkaiyat, S.K.A. Nurses’ Competency in Implementing Evidence-Based Practice: A Survey Study from a Governmental Hospital in the United Arab Emirates: Nurses’ Competency in Implementing Evidence-Based Practice. East. J. Healthc. 2023, 3, 32–38. [Google Scholar] [CrossRef]
- Alakhras, M.; Al-Mousa, D.S.; Al Mohammad, B.; Spuur, K.M. Knowledge, attitude, understanding and implementation of evidence-based practice among Jordanian radiographers. Radiography 2023, 29, 760–766. [Google Scholar] [CrossRef] [PubMed]
- Capezio, A.; Decosta, P.L. Evidence-Based Decision-Making and Practice in Organizations; Oxford Research Encyclopedia of Psychology: New York, NY, USA, 2023. [Google Scholar]
- Claridge, J.A.; Fabian, T.C. History and development of evidence-based medicine. World J. Surg. 2005, 29, 547–553. [Google Scholar] [CrossRef]
- Sackett, D.L.; Rosenberg, W.M.; Gray, J.M.; Haynes, R.B.; Richardson, W.S. Evidence based medicine: What it is and what it isn’t. BMJ 1996, 312, 71–72. [Google Scholar] [CrossRef]
- Mackey, A.; Bassendowski, S. The history of evidence-based practice in nursing education and practice. J. Prof. Nurs. 2017, 33, 51–55. [Google Scholar] [CrossRef]
- André, B.; Aune, A.G.; Brænd, J.A. Embedding evidence-based practice among nursing undergraduates: Results from a pilot study. Nurse Educ. Pract. 2016, 18, 30–35. [Google Scholar] [CrossRef]
- Tilson, J.K.; Kaplan, S.L.; Harris, J.L.; Hutchinson, A.; Ilic, D.; Niederman, R.; Potomkova, J.; Zwolsman, S.E. Sicily statement on classification and development of evidence-based practice learning assessment tools. BMC Med. Educ. 2011, 11, 78. [Google Scholar] [CrossRef]
- Sin, M.; Bliquez, R. Teaching evidence based practice to undergraduate nursing students. J. Prof. Nurs. 2017, 33, 447–451. [Google Scholar] [CrossRef] [PubMed]
- Ismail, S.A.; McDonald, A.; Dubois, E.; Aljohani, F.G.; Coutts, A.P.; Majeed, A.; Rawaf, S. Assessing the state of health research in the Eastern Mediterranean Region. J. R. Soc. Med. 2013, 106, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Patton, L.J.; Garcia, M.; Young, V.; Bradfield, C.; Gosdin, A.; Chen, P.; Webb, T.; Tidwell, J. Exploring nurse beliefs and perceived readiness for system wide integration of evidence based practice in a large pediatric health care system. J. Pediatr. Nurs. 2022, 63, 46–51. [Google Scholar] [CrossRef]
- Fernández-Domínguez, J.C.; de Pedro-Gómez, J.E.; Morales-Asencio, J.M.; Bennasar-Veny, M.; Sastre-Fullana, P.; Sesé-Abad, A. Health Sciences-Evidence Based Practice questionnaire (HS-EBP) for measuring transprofessional evidence-based practice: Creation, development and psychometric validation. PLoS ONE 2017, 12, e0177172. [Google Scholar] [CrossRef]
- Ruzafa-Martinez, M.; Lopez-Iborra, L.; Moreno-Casbas, T.; Madrigal-Torres, M. Development and validation of the competence in evidence based practice questionnaire (EBP-COQ) among nursing students. BMC Med. Educ. 2013, 13, 19. [Google Scholar] [CrossRef]
- McEvoy, M.P.; Williams, M.T.; Olds, T.S. Development and psychometric testing of a trans-professional evidence-based practice profile questionnaire. Med. Teach. 2010, 32, e373–e380. [Google Scholar] [CrossRef]
- Abuadas, M.H.; Albikawi, Z.F.; Abuadas, F. Development and validation of questionnaire measuring registered nurses’ competencies, beliefs, facilitators, barriers, and implementation of Evidence-Based Practice (EBP-CBFRI). J. Nurs. Meas. 2021. [Google Scholar] [CrossRef]
- Upton, D.; Upton, P. Development of an evidence-based practice questionnaire for nurses. J. Adv. Nurs. 2006, 53, 454–458. [Google Scholar] [CrossRef]
- Diery, A.; Vogel, F.; Knogler, M.; Seidel, T. Evidence-Based Practice in Higher Education: Teacher Educators’ Attitudes, Challenges, and Uses; Frontiers in Education; Frontiers Media SA: Lausanne, Switzerland, 2020; Volume 5, p. 62. [Google Scholar]
- Fajarini, M.; Rahayu, S.; Setiawan, A. Translating, Adapting and Testing the Indonesian Version of Evidence-based Practice Questionnaire (EBPQ). OSF Preprints 2018. [Google Scholar] [CrossRef]
- Rice, K.; Hwang, J.; Abrefa-Gyan, T.; Powell, K. Evidence-based practice questionnaire: A confirmatory factor analysis in a social work sample. Adv. Soc. Work. 2010, 11, 158–173. [Google Scholar] [CrossRef]
- Bolignano, D.; Mattace-Raso, F.; Torino, C.; D’Arrigo, G.; ElHafeez, S.A.; Provenzano, F.; Zoccali, C.; Tripepi, G. The quality of reporting in clinical research: The CONSORT and STROBE initiatives. Aging Clin. Exp. Res. 2013, 25, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Bonett, D.G. Sample size requirements for testing and estimating coefficient alpha. J. Educ. Behav. Stat. 2002, 27, 335–340. [Google Scholar] [CrossRef]
- Dalheim, A.; Harthug, S.; Nilsen, R.M.; Nortvedt, M.W. Factors influencing the development of evidence-based practice among nurses: A self-report survey. BMC Health Serv. Res. 2012, 12, 367. [Google Scholar] [CrossRef]
- Rospendowiski, K.; Alexandre, N.M.C.; Cornélio, M.E. Cultural adaptation to Brazil and psychometric performance of the “Evidence-Based Practice Questionnaire”. Acta Paul. De Enferm. 2014, 27, 405–411. [Google Scholar] [CrossRef]
- Youssef, N.F.; Alshraifeen, A.; Alnuaimi, K.; Upton, P. Egyptian and Jordanian nurse educators’ perception of barriers preventing the implementation of evidence-based practice: A cross-sectional study. Nurse Educ. Today 2018, 64, 33–41. [Google Scholar] [CrossRef]
- Cortina, J.M. What is coefficient alpha? An examination of theory and applications. J. Appl. Psychol. 1993, 78, 98. [Google Scholar] [CrossRef]
- Hair, J.F., Jr.; Hult, G.T.M.; Ringle, C.M.; Sarstedt, M.; Danks, N.P.; Ray, S. Partial Least Squares Structural Equation Modeling (PLS-SEM) Using R: A Workbook; Springer Nature: Berlin/Heidelberg, Germany, 2021. [Google Scholar]
- Alblooshi, S.M.; Razzak, H.A.; Hijji, F.H.; Wishah, M.A.M.; Alkarbi, M.; Harbi, A.Z. Knowledge, Attitude and Implementation of Evidence-Based Practice among Nurses; A National Survey. Res. Sq. 2022. [Google Scholar] [CrossRef]
- Reali, S.; Lee, T.; Bishop, J.; Mirkov, S.; Johnson, J.; McCourt, E.; Hughes, J.; Pont, L.; Page, A.T.; Penm, J. Attitudes, barriers and facilitators of hospital pharmacists conducting practice-based research: A systematic review. J. Pharm. Pract. Res. 2021, 51, 192–202. [Google Scholar] [CrossRef]
- Stewart, D.; Al Hail, M.; Abdul Rouf, P.V.; El Kassem, W.; Diack, L.; Thomas, B.; Awaisu, A. Building hospital pharmacy practice research capacity in Qatar: A cross-sectional survey of hospital pharmacists. Int. J. Clin. Pharm. 2015, 37, 511–521. [Google Scholar] [CrossRef]
- Ammouri, A.A.; Raddaha, A.A.; Dsouza, P.; Geethakrishnan, R.; Noronha, J.A.; Obeidat, A.A.; Shakman, L. Evidence-based practice: Knowledge, attitudes, practice and perceived barriers among nurses in Oman. Sultan Qaboos Univ. Med. J. 2014, 14, e537. [Google Scholar]
- Zhou, F.; Hao, Y.; Guo, H.; Liu, H. Attitude, knowledge, and practice on evidence-based nursing among registered nurses in traditional Chinese medicine hospitals: A multiple center cross-sectional survey in China. Evid.-Based Complement. Altern. Med. 2016, 2016, 5478086. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).