Age-Related Decline in Cervical Proprioception and Its Correlation with Functional Mobility and Limits of Stability Assessed Using Computerized Posturography: A Cross-Sectional Study Comparing Older (65+ Years) and Younger Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Subjects
2.2. Assessment of Cervical Joint Position Sense
2.3. Assessment of Limits of Stability
2.4. Assessment of Functional Mobility
2.4.1. Berg Balance Scale (BBS)
2.4.2. Timed Up and Go (TUG) Test
2.5. Sample Size Calculation
2.6. Statistical Analysis
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhang, L.; Zeng, Y.; Weng, C.; Yan, J.; Fang, Y. Epidemiological characteristics and factors influencing falls among elderly adults in long-term care facilities in Xiamen, China. Medicine 2019, 98, e14375. [Google Scholar] [CrossRef] [PubMed]
- Neri, S.G.R.; Oliveira, J.S.; Dario, A.B.; Lima, R.M.; Tiedemann, A. Does obesity increase the risk and severity of falls in people aged 60 years and older? A systematic review and meta-analysis of observational studies. J. Gerontol. Ser. A 2020, 75, 952–960. [Google Scholar] [CrossRef] [PubMed]
- Chalise, H.N. Aging: Basic concept. Am. J. Biomed. Sci. Res. 2019, 1, 8–10. [Google Scholar] [CrossRef]
- Kirwan, R.; McCullough, D.; Butler, T.; de Heredia, F.P.; Davies, I.G.; Stewart, C. Sarcopenia during COVID-19 lockdown restrictions: Long-term health effects of short-term muscle loss. GeroScience 2020, 42, 1547–1578. [Google Scholar] [CrossRef]
- Torres-Guzman, R.A.; Paulson, M.R.; Avila, F.R.; Maita, K.; Garcia, J.P.; Forte, A.J.; Maniaci, M.J. Smartphones and threshold-based monitoring methods effectively detect falls remotely: A systematic review. Sensors 2023, 23, 1323. [Google Scholar] [CrossRef]
- Kasch, J.D. Implementing STEADI to Enhance Fall Preventative Measures in Aging Community-Dwelling Veterans; The University of Arizona: Tucson, AZ, USA, 2022. [Google Scholar]
- Song, Q.; Zhang, X.; Mao, M.; Sun, W.; Zhang, C.; Chen, Y.; Li, L. Relationship of proprioception, cutaneous sensitivity, and muscle strength with the balance control among older adults. J. Sport Heal. Sci. 2021, 10, 585–593. [Google Scholar] [CrossRef]
- Reddy, R.S.; Tedla, J.S.; Dixit, S.; Raizah, A.; Al-Otaibi, M.L.; Gular, K.; Ahmad, I.; Sirajudeen, M.S. Cervical Joint Position Sense and Its Correlations with Postural Stability in Subjects with Fibromyalgia Syndrome. Life 2022, 12, 1817. [Google Scholar] [CrossRef]
- Reddy, R.S.; Meziat-Filho, N.; Ferreira, A.S.; Tedla, J.S.; Kandakurti, P.K.; Kakaraparthi, V.N. Comparison of neck extensor muscle endurance and cervical proprioception between asymptomatic individuals and patients with chronic neck pain. J. Bodyw. Mov. Ther. 2021, 26, 180–186. [Google Scholar] [CrossRef]
- Peng, B.; Yang, L.; Li, Y.; Liu, T.; Liu, Y. Cervical proprioception impairment in neck pain-pathophysiology, clinical evaluation, and management: A narrative review. Pain Ther. 2021, 10, 143–164. [Google Scholar] [CrossRef]
- Kandakurti, P.K.; Reddy, R.S.; Kakarparthy, V.N.; Rengaramanujam, K.; Tedla, J.S.; Dixit, S.; Gautam, A.P.; Silvian, P.; Gular, K.; Eapen, C.; et al. Comparison and association of neck extensor muscles’ endurance and postural function in subjects with and without chronic neck pain—A cross-sectional study. Phys. Med. Rehabil. Kurortmed. 2021, 31, 295–301. [Google Scholar] [CrossRef]
- Clark, B.C. Neuromuscular changes with aging and sarcopenia. J. Frailty Aging 2019, 8, 7–9. [Google Scholar] [CrossRef]
- Rao, N.; Mehta, N.; Patel, P.; Parikh, P.J. Effects of aging on conditional visuomotor learning for grasping and lifting eccentrically weighted objects. J. Appl. Physiol. 2021, 131, 937–948. [Google Scholar] [CrossRef]
- Asiri, F.; Reddy, R.S.; Alshahrani, M.S.; Tedla, J.S.; Dixit, S.; Alshahrani, A.; Gular, K.; Raizah, A. Mediation Effect of Pain on the Relationship between Kinesiophobia and Postural Control: Comparison and Correlations in Individuals with Fibromyalgia Syndrome and Asymptomatic Individuals—A Cross-Sectional Study. Life 2023, 13, 175. [Google Scholar] [CrossRef]
- Story, M.R.; Haussler, K.K.; Nout-Lomas, Y.S.; Aboellail, T.A.; Kawcak, C.E.; Barrett, M.F.; Frisbie, D.D.; McIlwraith, C.W. Equine cervical pain and dysfunction: Pathology, diagnosis and treatment. Animals 2021, 11, 422. [Google Scholar] [CrossRef]
- Osoba, M.Y.; Rao, A.K.; Agrawal, S.K.; Lalwani, A.K. Balance and gait in the elderly: A contemporary review. Laryngoscope Investig. Otolaryngol. 2019, 4, 143–153. [Google Scholar] [CrossRef]
- Monfort, S.M.; Pan, X.; Loprinzi, C.L.; Lustberg, M.B.; Chaudhari, A.M.W. Impaired postural control and altered sensory organization during quiet stance following neurotoxic chemotherapy: A preliminary study. Integr. Cancer Ther. 2019, 18, 1534735419828823. [Google Scholar] [CrossRef]
- Neri, S.G.; Harvey, L.A.; Tiedemann, A.; Gadelha, A.B.; Lima, R.M. Obesity and falls in older women: Mediating effects of muscle quality, foot loads and postural control. Gait Posture 2020, 77, 138–143. [Google Scholar] [CrossRef]
- Zanotto, T.; Gobbo, S.; Bullo, V.; Vendramin, B.; Roma, E.; Duregon, F.; Bocalini, D.S.; Di Blasio, A.; Cugusi, L.; Furian, L.; et al. Postural balance, muscle strength, and history of falls in end-stage renal disease patients living with a kidney transplant: A cross-sectional study. Gait Posture 2020, 76, 358–363. [Google Scholar] [CrossRef]
- Chantanachai, T.; Taylor, M.E.; Lord, S.R.; Menant, J.; Delbaere, K.; Sachdev, P.S.; Kochan, N.A.; Brodaty, H.; Sturnieks, D.L. Risk factors for falls in community-dwelling older people with mild cognitive impairment: A prospective one-year study. PeerJ 2022, 10, e13484. [Google Scholar] [CrossRef]
- Henry, M.; Baudry, S. Age-related changes in leg proprioception: Implications for postural control. J. Neurophysiol. 2019, 122, 525–538. [Google Scholar] [CrossRef]
- Lin, J. Challenging the Role of Proprioception in Non-Specific Low Back Pain. Ph.D. Thesis, The University of Sydney, Sydney, Australia, 2021. [Google Scholar]
- Madsalae, T.; Thongprong, T.; Chinkulprasert, C.; Boonsinsukh, R. Can the balance evaluation systems test be used to identify system-specific postural control impairments in older adults with chronic neck pain? Front. Med. 2022, 9, 3226. [Google Scholar] [CrossRef] [PubMed]
- Reddy, R.S.; Alahmari, K.A.; Silvian, P.S. Test-retest reliability of assessing cervical proprioception using cervical range of motion device. Saudi J. Sports Med. 2016, 16, 118. [Google Scholar] [CrossRef]
- Keogh, J.W.L.; Cox, A.; Anderson, S.; Liew, B.; Olsen, A.; Schram, B.; Furness, J. Reliability and validity of clinically accessible smartphone applications to measure joint range of motion: A systematic review. PLoS ONE 2019, 14, e0215806. [Google Scholar] [CrossRef] [PubMed]
- Alahmari, K.; Reddy, R.S.; Silvian, P.; Ahmad, I.; Nagaraj, V.; Mahtab, M. Intra-and inter-rater reliability of neutral head position and target head position tests in patients with and without neck pain. Braz. J. Phys. Ther. 2017, 21, 259–267. [Google Scholar] [CrossRef]
- Viveiro, L.A.P.; Gomes, G.C.V.; Bacha, J.M.R.; Junior, N.C.; Kallas, M.E.; Reis, M.; Filho, W.J.; Pompeu, J.E. Reliability, validity, and ability to identity fall status of the Berg Balance Scale, Balance Evaluation Systems Test (BESTest), Mini-BESTest, and Brief-BESTest in older adults who live in nursing homes. J. Geriatr. Phys. Ther. 2019, 42, E45–E54. [Google Scholar] [CrossRef]
- Chen, H.; Smith, S.S. Item distribution in the Berg balance scale: A problem for use with community-living older adults. J. Geriatr. Phys. Ther. 2019, 42, 275–280. [Google Scholar] [CrossRef]
- Chua, K.Y.; Lim, W.S.; Lin, X.; Yuan, J.-M.; Koh, W.-P. Handgrip strength and timed up-and-go (TUG) test are predictors of short-term mortality among elderly in a population-based cohort in Singapore. J. Nutr. Health Aging 2020, 24, 371–378. [Google Scholar] [CrossRef]
- Christopher, A.; Kraft, E.; Olenick, H.; Kiesling, R.; Doty, A. The reliability and validity of the Timed Up and Go as a clinical tool in individuals with and without disabilities across a lifespan: A systematic review: Psychometric properties of the Timed Up and Go. Disabil. Rehabil. 2021, 43, 1799–1813. [Google Scholar] [CrossRef]
- Stanton, T.R.; Leake, H.B.; Chalmers, K.J.; Moseley, G.L. Evidence of impaired proprioception in chronic, idiopathic neck pain: Systematic review and meta-analysis. Phys. Ther. 2016, 96, 876–887. [Google Scholar] [CrossRef]
- Alahmari, K.A.; Reddy, R.S.; Tedla, J.S.; Samuel, P.S.; Kakaraparthi, V.N.; Rengaramanujam, K.; Ahmed, I. The effect of Kinesio taping on cervical proprioception in athletes with mechanical neck pain—A placebo-controlled trial. BMC Musculoskelet. Disord. 2020, 21, 648. [Google Scholar] [CrossRef]
- Asiri, F.; Reddy, R.S.; Tedla, J.S.; Almohiza, M.A.; Alshahrani, M.S.; Govindappa, S.C.; Sangadala, D.R. Kinesiophobia and its correlations with pain, proprioception, and functional performance among individuals with chronic neck pain. PLoS ONE 2021, 16, e0254262. [Google Scholar] [CrossRef]
- Reddy, R.S.; Tedla, J.S.; Alshahrani, M.S.; Asiri, F.; Kakaraparthi, V.N. Comparison and correlation of cervical proprioception and muscle endurance in general joint hypermobility participants with and without non-specific neck pain—A cross-sectional study. PeerJ 2022, 10, e13097. [Google Scholar] [CrossRef]
- Reddy, R.S.; Tedla, J.S.; Dixit, S.; Abohashrh, M. Cervical proprioception and its relationship with neck pain intensity in subjects with cervical spondylosis. BMC Musculoskelet. Disord. 2019, 20, 447. [Google Scholar] [CrossRef]
- Landelle, C.; Chancel, M.; Blanchard, C.; Guerraz, M.; Kavounoudias, A. Contribution of muscle proprioception to limb movement perception and proprioceptive decline with ageing. Curr. Opin. Physiol. 2021, 20, 180–185. [Google Scholar] [CrossRef]
- Alahmari, K.A.; Reddy, R.S.; Silvian, P.S.; Ahmad, I.; Kakaraparthi, V.N.; Alam, M.M. Association of age on cervical joint position error. J. Adv. Res. 2017, 8, 201–207. [Google Scholar] [CrossRef]
- Chen, X.; Qu, X. Age-related differences in the relationships between lower-limb joint proprioception and postural balance. Hum. Factors 2019, 61, 702–711. [Google Scholar] [CrossRef]
- Alahmari, K.A.; Reddy, R.S.; Silvian, P.; Ahmad, I.; Nagaraj, V.; Mahtab, M. Influence of chronic neck pain on cervical joint position error (JPE): Comparison between young and elderly subjects. J. Back Musculoskelet. Rehabil. 2017, 30, 1265–1271. [Google Scholar] [CrossRef]
- Reddy, R.S.; Maiya, A.G.; Rao, S.K. Effect of dorsal neck muscle fatigue on cervicocephalic kinaesthetic sensibility. Hong Kong Physiother. J. 2012, 20, 105–109. [Google Scholar] [CrossRef]
- Reddy, R.S.; Alahmari, K.A.; Samuel, P.S.; Tedla, J.S.; Kakaraparthi, V.N.; Rengaramanujam, K. Intra-rater and inter-rater reliability of neutral and target lumbar positioning tests in subjects with and without non-specific lower back pain. J. Back Musculoskelet. Rehabil. 2021, 34, 289–299. [Google Scholar] [CrossRef]
- Reddy, R.S.; Alshahrani, M.S.; Tedla, J.S.; Asiri, F.; Nambi, G.; Kakaraparthi, V.N. Cervical Joint Position Sense in Individuals with Type 2 Diabetes and Its Correlations with Glycated Hemoglobin Levels: A Cross-Sectional Study. J. Manip. Physiol. Ther. 2022, 45, 273–281. [Google Scholar] [CrossRef]
- Reddy, R.S.; Alshahrani, M.S.; Tedla, J.S.; Dixit, S.; Asiri, F.; Al-Otaibi, M.L.; Kakaraparthi, V.N.; Assiri, S.M.A. Comparison of Cervical Joint Position Sense in Computer Users with Neck Pain, Forward Head Posture, Asymptomatic and Non-Computer Users—A Cross-Sectional Study. Phys. Med. Rehabil. Kurortmed. 2022. [Google Scholar] [CrossRef]
- Reddy, R.S.Y.; Maiya, A.G.; Rao, S.K.; Alahmari, K.A.; Tedla, J.S.; Kandakurti, P.K.; Kakaraparthi, V.N. Effectiveness of kinaesthetic exercise program on position sense, pain, and disability in chronic neck pain patients with cervical spondylosis—A randomized comparative trial. Phys. Med. Rehabil. Kurortmed. 2020, 31, 242–250. [Google Scholar] [CrossRef]
- Quek, J.; Treleaven, J.; Clark, R.A.; Brauer, S.G. An exploratory study examining factors underpinning postural instability in older adults with idiopathic neck pain. Gait Posture 2018, 60, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Tieland, M.; Trouwborst, I.; Clark, B.C. Skeletal muscle performance and ageing. J. Cachexia Sarcopenia Muscle 2017, 9, 3–19. [Google Scholar] [CrossRef]
- Fragala, M.S.; Cadore, E.L.; Dorgo, S.; Izquierdo, M.; Kraemer, W.J.; Peterson, M.D.; Ryan, E.D. Resistance training for older adults: Position statement from the national strength and conditioning association. J. Strength Cond. Res. 2019, 33, 2019–2052. [Google Scholar] [CrossRef]
- Phu, S.; Vogrin, S.; Al Saedi, A.; Duque, G. Balance training using virtual reality improves balance and physical performance in older adults at high risk of falls. Clin. Interv. Aging 2019, 14, 1567–1577. [Google Scholar] [CrossRef]
- Soubra, R.; Chkeir, A.; Novella, J.-L. A systematic review of thirty-one assessment tests to evaluate mobility in older adults. BioMed Res. Int. 2019, 2019, 1354362. [Google Scholar] [CrossRef]
- Yacchirema, D.; de Puga, J.S.; Palau, C.; Esteve, M. Fall detection system for elderly people using IoT and ensemble machine learning algorithm. Pers. Ubiquitous Comput. 2019, 23, 801–817. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; Speechley, M. Falls in cognitively impaired older adults: Implications for risk assessment and prevention. J. Am. Geriatr. Soc. 2018, 66, 367–375. [Google Scholar] [CrossRef]
- Gucmen, B.; Kocyigit, B.F.; Nacitarhan, V.; Berk, E.; Koca, T.T.; Akyol, A. The relationship between cervical proprioception and balance in patients with fibromyalgia syndrome. Rheumatol. Int. 2022, 42, 311–318. [Google Scholar] [CrossRef]
- Lord, S.R.; Fitzpatrick, R.C. Choice stepping reaction time: A composite measure of falls risk in older people. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M627–M632. [Google Scholar] [CrossRef]
- Huys, C. The Predictive Value of Cervical Proprioception and Cervical Mobility in the Detection of an Increased Fall Risk in Elderly. Master’s Thesis, Ghent University, Ghent, Belgium, 2021. [Google Scholar]
- De Vestel, C.; Vereeck, L.; Reid, S.A.; Van Rompaey, V.; Lemmens, J.; De Hertogh, W. Systematic review and meta-analysis of the therapeutic management of patients with cervicogenic dizziness. J. Man. Manip. Ther. 2022, 30, 273–283. [Google Scholar] [CrossRef]
- Kristjansson, E.; Treleaven, J. Sensorimotor function and dizziness in neck pain: Implications for assessment and management. J. Orthop. Sports Phys. Ther. 2009, 39, 364–377. [Google Scholar] [CrossRef]
- Reid, S.; Callister, R.; Katekar, M.G.; Rivett, D.A. Effects of cervical spine manual therapy on range of motion, head repositioning, and balance in participants with cervicogenic dizziness: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2014, 95, 1603–1612. [Google Scholar] [CrossRef]
- Dunsky, A. The effect of balance and coordination exercises on quality of life in older adults: A mini-review. Front. Aging Neurosci. 2019, 11, 318. [Google Scholar] [CrossRef]
- Thomas, E.; Battaglia, G.; Patti, A.; Brusa, J.; Leonardi, V.; Palma, A.; Bellafiore, M. Physical activity programs for balance and fall prevention in elderly: A systematic review. Medicine 2019, 98, e16218. [Google Scholar] [CrossRef]
- Gilani, M.; Torkaman, G.; Bahrami, F.; Bayat, N. Virtual Reality Exergaming Capability to Change Muscle Strategy during the Limits of Stability Test and Reduce Fear of Falling in Primary Osteoporotic Women. Games Health J. 2023. [Google Scholar] [CrossRef]




| Variables | Older Group (>65 Years) (n = 100) | Younger Group (<65 Years) (n = 100) | p-Value |
|---|---|---|---|
| Age (years) | 69.53 ± 4.32 | 52.30 ± 4.23 | <0.001 |
| Gender (M:F) | 59:41 | 52:48 | <0.001 |
| Height (m) | 1.68 ± 0.09 | 1.73 ± 0.05 | 0.002 |
| Weight (kg) | 71.24 ± 5.96 | 69.58 ± 5.24 | 0.030 |
| BMI (kg/m2) | 24.50 ± 3.80 | 23.38 ± 2.74 | 0.201 |
| Variables | Older Group (>65 Years) (n = 100) | Younger Group (<65 Years) (n = 100) | MD | t | 95% CI | p-Value | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| JPE in flexion (°) | 4.28 ± 1.29 | 1.48 ± 1.37 | 3.00 | 1.97 | 2.64 | 3.36 | <0.001 |
| JPE in extension (°) | 5.29 ± 1.50 | 2.16 ± 0.99 | 3.25 | 2.13 | 2.86 | 3.64 | <0.001 |
| JPE in right rotation (°) | 4.27 ± 1.38 | 1.86 ± 0.98 | 2.43 | 1.67 | 2.12 | 2.74 | <0.001 |
| JPE in left rotation (°) | 4.02 ± 1.35 | 1.99 ± 0.83 | 2.26 | 1.98 | 1.97 | 2.25 | <0.001 |
| BBS test score | 46.48 ± 4.13 | 53.11 ± 5.29 | −6.53 | 2.23 | −6.87 | −6.19 | <0.001 |
| TUG test (s) | 10.39 ± 1.43 | 7.86 ± 1.56 | 1.45 | 2.34 | 1.12 | 1.78 | <0.001 |
| Reaction time (s) | 1.39 ± 0.29 | 0.59 ± 0.19 | 0.79 | 1.01 | 0.72 | 0.87 | <0.001 |
| Maximum excursion (%) | 5.12 ± 0.41 | 8.56 ± 0.53 | −2.57 | −2.64 | −2.66 | −2.48 | <0.001 |
| Direction control (%) | 73.58 ± 3.53 | 88.95 ± 2.73 | −14.14 | −6.8 | −15.17 | −13.11 | <0.001 |
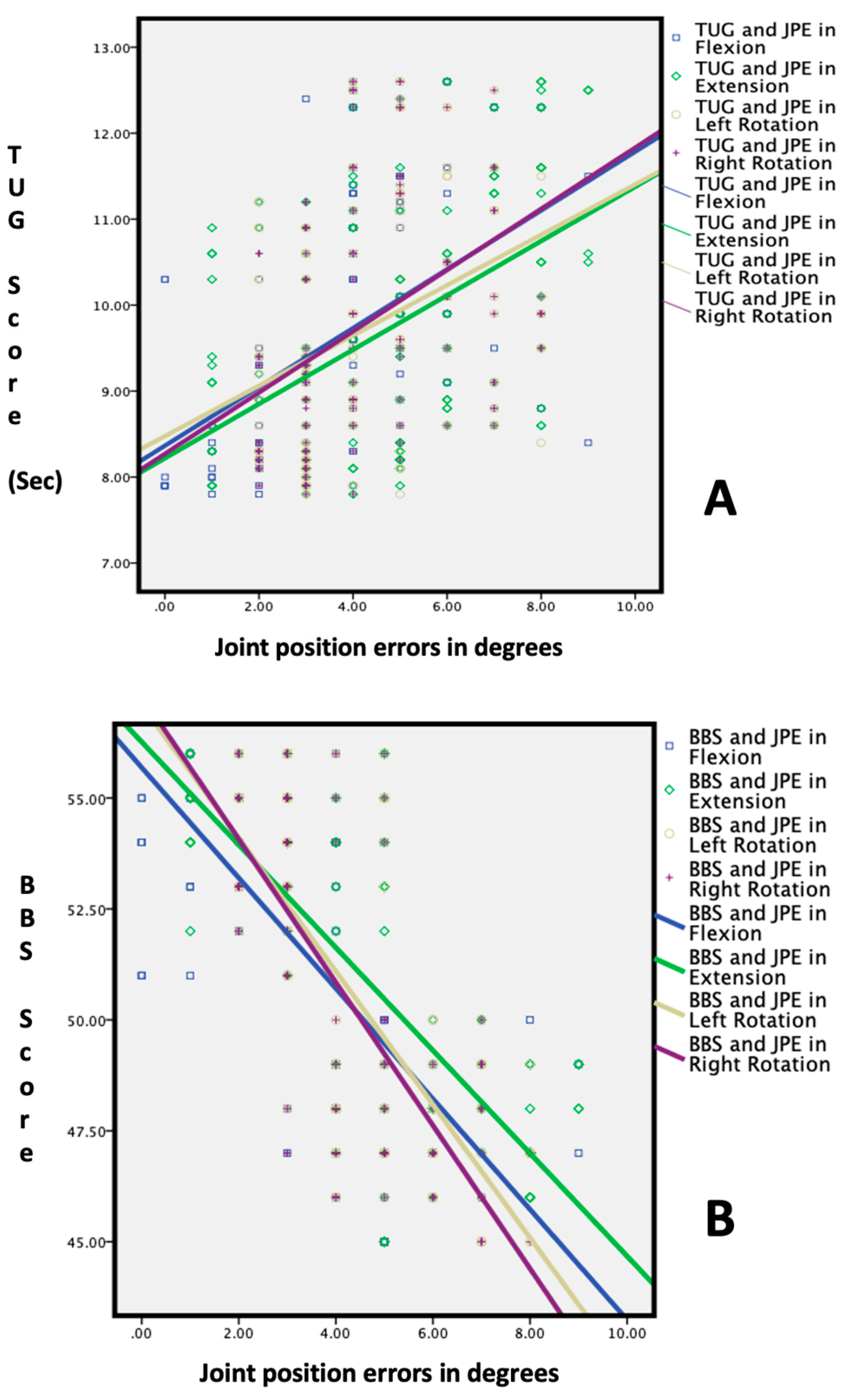
| Groups | Variables | BBS Test Score | TUG Test (s) | Reaction Time (s) | Maximum Excursion (%) | Direction Control (%) | |
|---|---|---|---|---|---|---|---|
| Above 65 years | JPE in flexion (°) | r | −0.68 ** | 0.53 ** | 0.71 ** | −0.63 ** | −0.61 ** |
| JPE in extension (°) | r | −0.72 ** | 0.56 ** | 0.62 ** | −0.62 ** | −0.62 ** | |
| JPE in right rotation (°) | r | −0.69 ** | 0.44 ** | 0.63 ** | −0.61 ** | −0.59 ** | |
| JPE in left rotation (°) | r | −0.66 ** | 0.53 ** | 0.61 ** | −0.60 ** | −0.53 ** | |
| Below 65 years | JPE in flexion (°) | r | −0.76 ** | 0.63 ** | 0.74 ** | −0.73 ** | −0.72 ** |
| JPE in extension (°) | r | −0.78 ** | 0.66 ** | 0.72 ** | −0.74 ** | −0.73 ** | |
| JPE in right rotation (°) | r | −0.81 ** | 0.54 ** | 0.73 ** | −0.71 ** | −0.71 ** | |
| JPE in left rotation (°) | r | −0.83 ** | 0.63 ** | 0.71 ** | −0.71 ** | −0.74 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reddy, R.S.; Alkhamis, B.A.; Kirmani, J.A.; Uddin, S.; Ahamed, W.M.; Ahmad, F.; Ahmad, I.; Raizah, A. Age-Related Decline in Cervical Proprioception and Its Correlation with Functional Mobility and Limits of Stability Assessed Using Computerized Posturography: A Cross-Sectional Study Comparing Older (65+ Years) and Younger Adults. Healthcare 2023, 11, 1924. https://doi.org/10.3390/healthcare11131924
Reddy RS, Alkhamis BA, Kirmani JA, Uddin S, Ahamed WM, Ahmad F, Ahmad I, Raizah A. Age-Related Decline in Cervical Proprioception and Its Correlation with Functional Mobility and Limits of Stability Assessed Using Computerized Posturography: A Cross-Sectional Study Comparing Older (65+ Years) and Younger Adults. Healthcare. 2023; 11(13):1924. https://doi.org/10.3390/healthcare11131924
Chicago/Turabian StyleReddy, Ravi Shankar, Batool Abdulelah Alkhamis, Junaid Ahmed Kirmani, Shadab Uddin, Waseem Mumtaz Ahamed, Fuzail Ahmad, Irshad Ahmad, and Abdullah Raizah. 2023. "Age-Related Decline in Cervical Proprioception and Its Correlation with Functional Mobility and Limits of Stability Assessed Using Computerized Posturography: A Cross-Sectional Study Comparing Older (65+ Years) and Younger Adults" Healthcare 11, no. 13: 1924. https://doi.org/10.3390/healthcare11131924
APA StyleReddy, R. S., Alkhamis, B. A., Kirmani, J. A., Uddin, S., Ahamed, W. M., Ahmad, F., Ahmad, I., & Raizah, A. (2023). Age-Related Decline in Cervical Proprioception and Its Correlation with Functional Mobility and Limits of Stability Assessed Using Computerized Posturography: A Cross-Sectional Study Comparing Older (65+ Years) and Younger Adults. Healthcare, 11(13), 1924. https://doi.org/10.3390/healthcare11131924







