Analysis of Heart Rate, Perception of Physical Effort and Performance of Individuals with Down Syndrome Submitted to a Protocol of Virtual Games for Home-Based Telerehabilitation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
- (1)
- The first phase consisted of DS and TD individuals (paired by sex and age) performing one day of the game task for 20 min (with three matches of the game), and comparisons between the groups in terms of HR, RPE, and motor performance were made during the practice.
- (2)
- The second phase, only for the DS individuals, consisted of a 10-day practice protocol in addition to the first day, scheduled two times a week according to participant availability (thus, the protocol for DS individuals consisted of 11 days): participants played the game for approximately 20 min each day (with three matches of the game), and their HR and RPE during the practice were registered. After the 10th session of the protocol, the participants were allowed a 15-day break before another day of practice was scheduled with the intention of analyzing whether participants maintained their performance.
2.2. Participants
2.3. Assessment Instruments
2.4. Intervention Protocol: MoveHero
2.5. Procedures
2.6. Statistical Analysis
3. Results
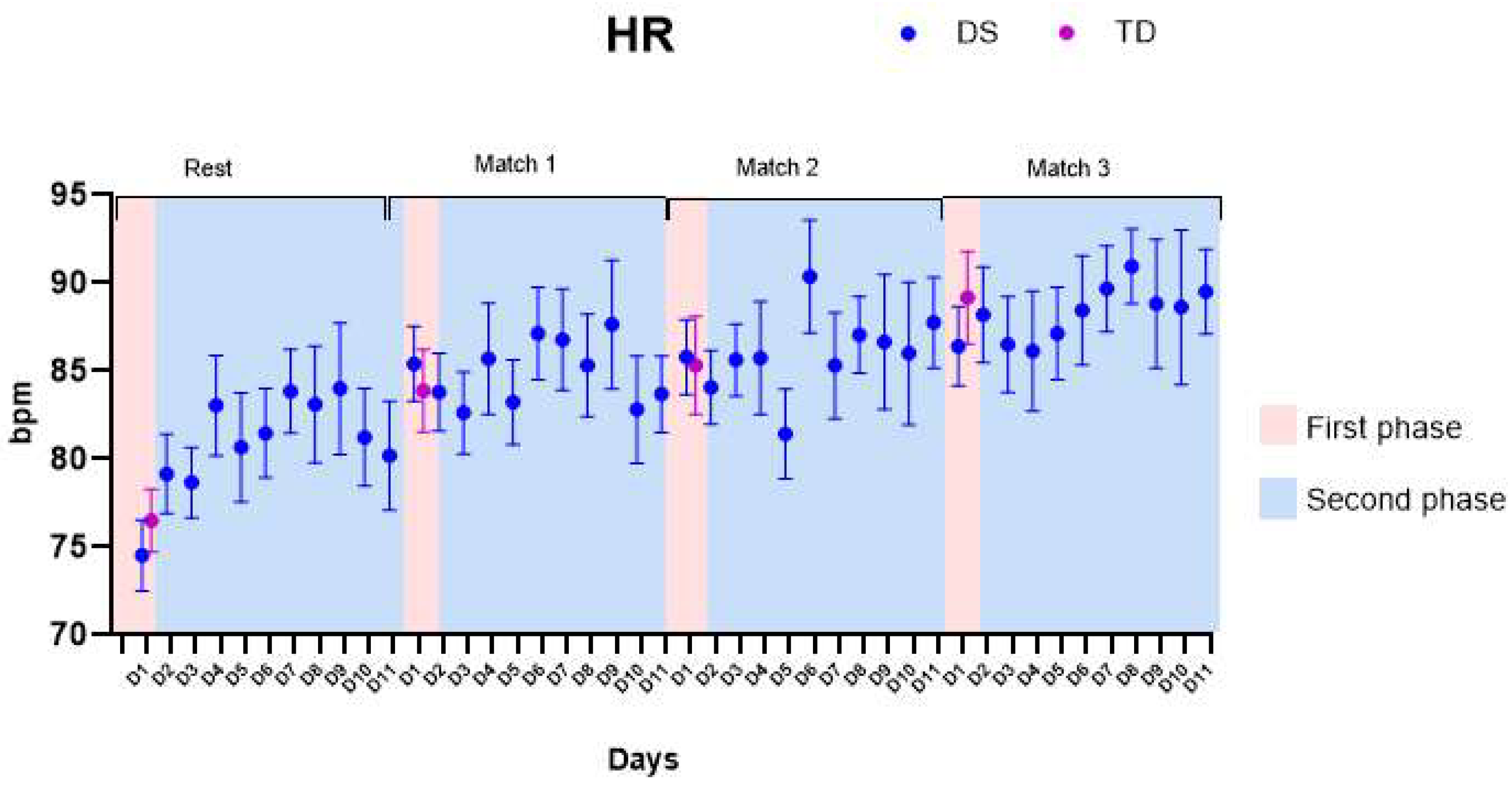
3.1. Heart Rate (HR)
- (1)
- First phase: No significant differences were found comparing the HR of both groups (the DS group presented average increases of 13.7 ± 2.4 beats per minute (bpm), and the TD group presented average increases of 12.7 ± 3.2 bpm). We found main effects for matches within-groups: both DS and TD enhanced their HR values comparing rest with Match 1 and Rest with Match 3 (p-values and descriptive statistics are provided in Table S1).
- (2)
- Second phase: We found main effects for Matches (p-values and descriptive statistics are provided in Table S2). No significant differences were found for HR comparing the days of the protocol.
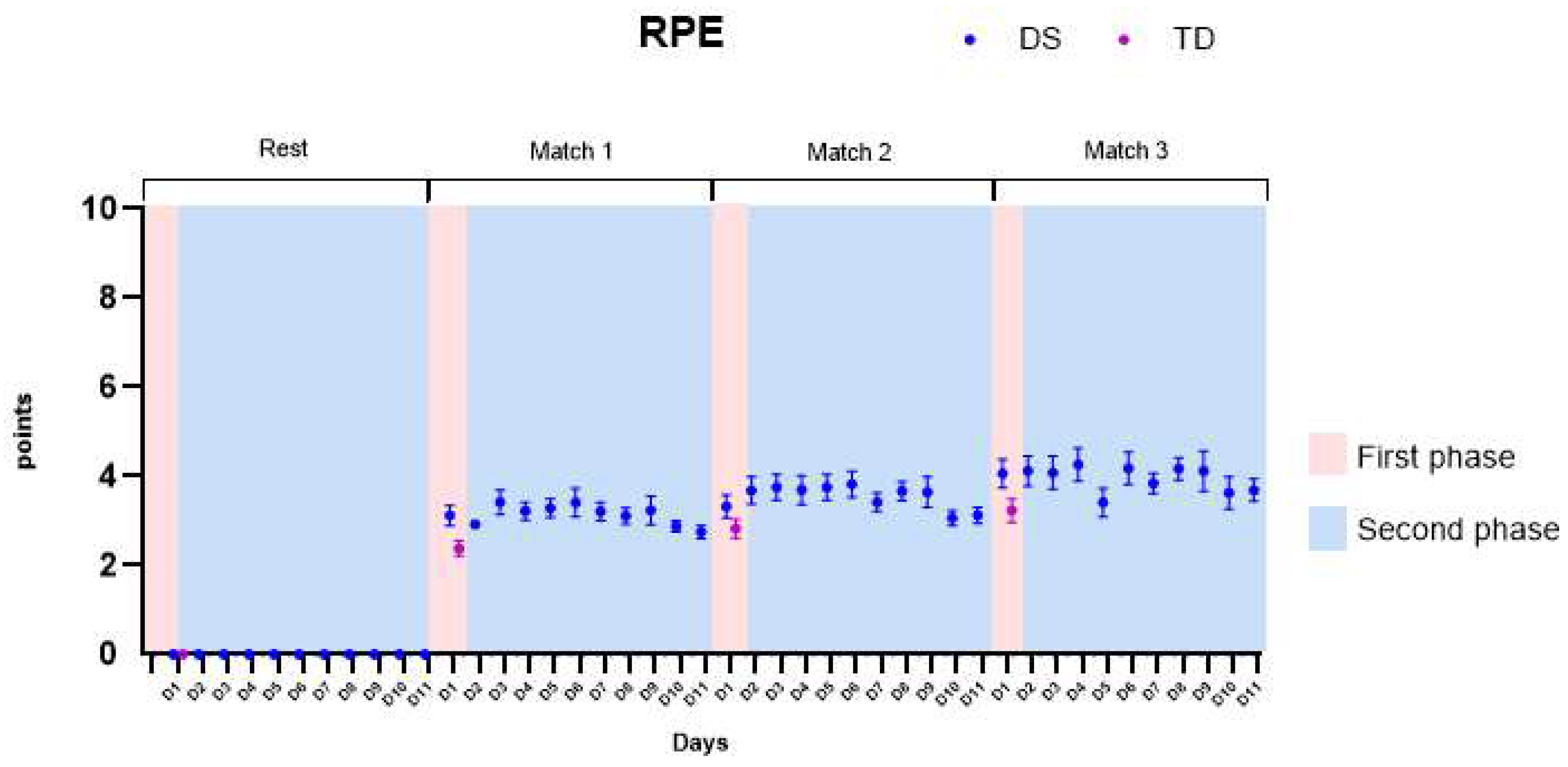
3.2. Borg Rating of Perceived Exertion (RPE)
- (1)
- First phase: We found main effects for groups and in the interaction groups by matches. The DS group presented significantly higher values of RPE when compared to the TD group, presenting higher values of RPE in the first (M1—mean difference of 0.8 ± 0.2), second (M2—mean difference of 0.4 ± 0.2), and third matches (M3—mean difference of 0.7 ± 0.2). All p-values and descriptive statistics are provided in Table S1.
- (2)
- Second phase: We found significant increases in RPE in the DS individuals when comparing matches. The differences were also found when comparing the first day (D1) and the last day of the protocol (D11), enhancing the RPE. All p-values and descriptive statistics are provided in Table S2.
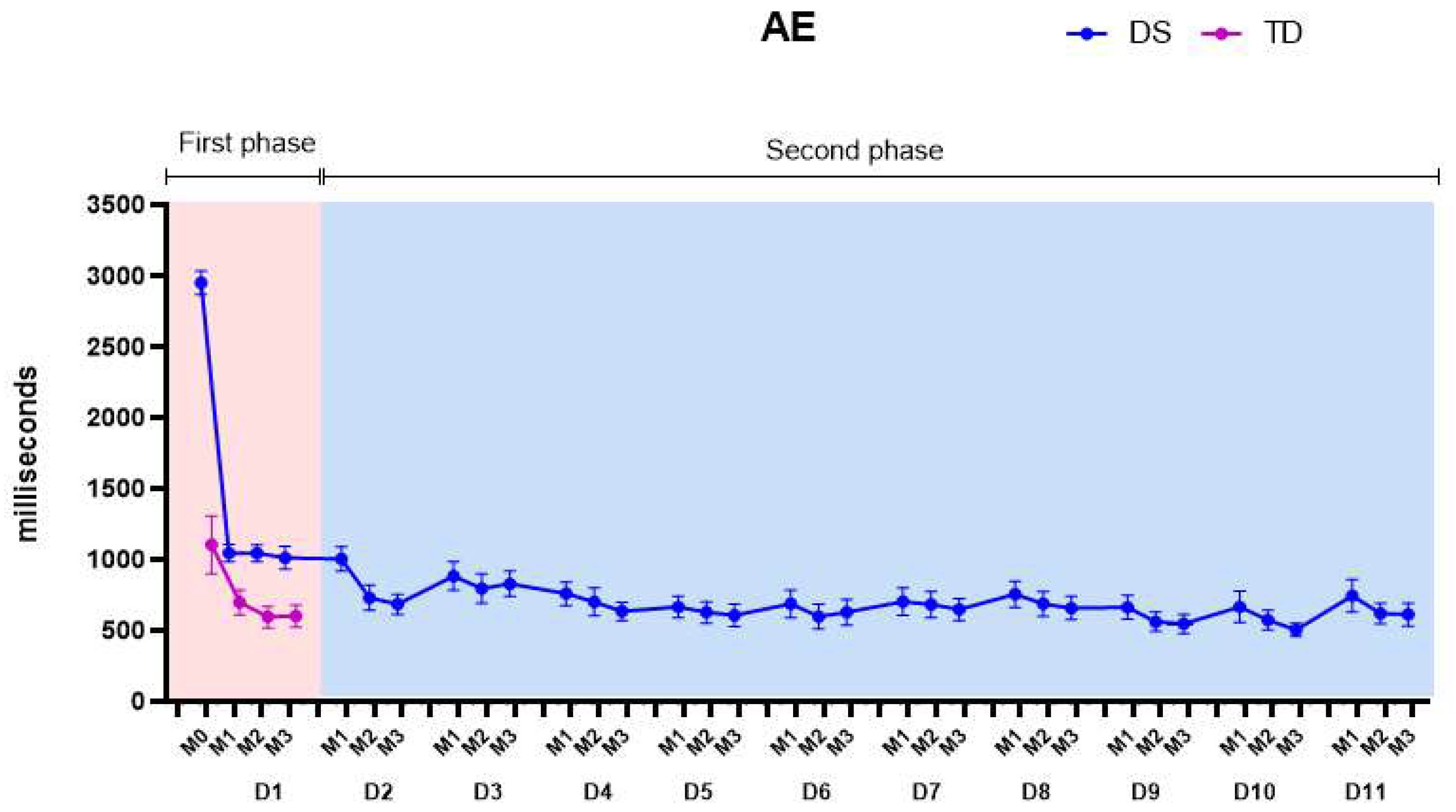
3.3. Absolute Error (AE)
- (1)
- First phase: We found main effects for groups, matches, and for the groups by matches interaction. Comparisons between groups showed that the DS group started the practice with higher mean values of AE than the TD group, with a mean difference between groups of 763.2 (±54.9) ms (p-values and descriptive statistics are provided in Table S1).
- (2)
- Second phase: Significant differences were found comparing the days and matches of the protocol. On the fourth day of practice, the AEs of the DS group reached the values of the TD group and maintained the decrease in errors, presenting lower values than the TD group from the fifth day on (639.0 ± 53.2 ms). A significant decrease in the AEs was found comparing D1 with D10 and D1 with D11. All p-values and descriptive statistics are provided in Table S2.
3.4. Variable Error (VE)
- (1)
- First phase: We found main effects for matches and in the groups by matches interaction. Comparing the familiarization match (M0) between the DS and TD groups, the DS group showed significantly lower values (363.9 ± 57.1) of VE than the TD group (771.4 ± 69.1), which is the opposite of what occurred for the AE. All p-values and descriptive statistics are provided in Table S1.
- (2)
- Second phase: Over the days, the mean VE values of the DS group increased, varying between 770.4 ± 44.6 ms and 849.3 ± 45.3 ms but not reaching the mean values of the TD group (664.6 ± 30.4 ms). These results are further discussed below. All p-values and descriptive statistics are provided in Table S2.
4. Discussion
4.1. First Phase: Heart Rate (HR) and Rating of Perceived Effort (RPE) with Game Practice
4.2. Second Phase: Motor Performance during Game Practice
4.3. Absolute and Variable Errors: Accuracy and Precision When Practicing a Timing Coincident Task
5. Limitations and Future Studies
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Weijerman, M.E.; Winter, J.P. Clinical practice: The care of Children with Down syndrome. Eur. J. Pediatr. 2010, 169, 445–1452. [Google Scholar] [CrossRef] [PubMed]
- Dupre, C.; Weidman-Evans, E. Musculoskeletal development in patients with Down syndrome. J. Am. Acad. Physician Assist. 2017, 30, 38–40. [Google Scholar] [CrossRef] [PubMed]
- Izquierdo-Gomez, R.; Veiga, O.L.; Villagra, A.; Diaz-Cueto, M. Correlates of sedentary behaviour in youths with Down syndrome: The up&down study. J. Sport. Sci. 2015, 33, 1504–1514. [Google Scholar]
- Shields, N.; Hussey, J.; Murphy, J.; Gormley, J.; Hoey, H. An exploratory study of the association between physical activity, cardiovascular fitness and body size in children with Down syndrome. Dev. Neurorehabilit. 2017, 20, 92–98. [Google Scholar] [CrossRef]
- Fox, B.; Moffett, G.E.; Kinnison, C.; Brooks, G.; Case, L.E. Physical activity levels of children with Down syndrome. Pediatr. Phys. Ther. 2019, 31, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Grieco, J.; Pulsifier, M.; Seligsohn, K.; Skotko, B.; Schwartz, A. Down syndrome: Cognitive and behavioral functioning across the lifespan. Am. J. Med. Genet. Part C Semin. Med. Genet. 2015, 169, 2. [Google Scholar] [CrossRef]
- World Health Organization. World Health Organization Guidelines on Physical Activity and Sedentary Behavior: At a Glance; World Health Organization: Geneva, Switzerland, 2020.
- Singhal, T. A Review of Coronavirus Disease-2019 (COVID-19). Indian J. Pediatr. 2020, 87, 281–286. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Boldrini, T.; Lomoriello, A.S.; Corno, F.; Lingiardi, V.; Salcuni, S. Psychotherapy during COVID-19: How the clinical practice of Italian psychotherapists changed during the pandemic. Front. Psychol. 2020, 11, 591170. [Google Scholar] [CrossRef]
- Hosseiniravandi, M.; Kahlaee, A.; Karim, H.; Ghamkhar, L.; Safdari, R. Home-based telerehabilitation software systems for remote supervising: A systematic review. Int. J. Technol. Assess. Health Care 2020, 36, 113–125. [Google Scholar] [CrossRef]
- Santos, M.T.; Moura, S.C.; Gomes, L.M.X.; Lima, A.H.; Moreira, R.S.; Silva, C.D.; Guimarães, E.M.P. Telehealth application on the rehabilitation of children and adolescents. Rev. Paul. Pediatr. 2014, 32, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Novak, I.; Morgan, C.; Fahey, M.; Finch-Edmondson, M.; Galea, C.; Hines, A.; Langdon, K.; Mc Namara, M.; Paton, M.C.B.; Popat, H.; et al. State of the evidence traffic lights 2019: Systematic review of interventions for preventing and treating children with cerebral palsy. Curr. Neurol. Neurosci. Rep. 2020, 20, 3. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.B.M.; Silva, T.D.; Abreu, L.C.; Fregni, F.; Araujo, L.V.; Ferreira, F.H.I.B.; Leone, C. Short-term motor learning through non-immersive virtual reality task in individuals with down syndrome. BMC Neurol. 2017, 17, 71. [Google Scholar]
- Leighton, R.J.; Shortell, S.M. Interactive games to promote behavior change in prevention and treatment. JAMA 2011, 305, 1704–1705. [Google Scholar] [CrossRef]
- Mura, G.; Carta, M.; Sancassiani, F.; Machado, S.; Prosperini, L. Active exergames to improve cognitive functioning in neurological disabilities: A systematic review and meta-analysis. Eur. J. Phys. Rehabil. Med. 2018, 54, 450–462. [Google Scholar] [CrossRef]
- Mancini, M.C.; Gonçalves, S.C.; Martins, S.M. Comparison of functional performance among children with Down syndrome and children with age-appropriate development at 2 and 5 years of age. Arq. Neuro-Psiquiatr. 2003, 61, 409–415. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjostorm, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sport. Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Nashimoto, S.; Morishita, S.; Iida, S.; Hotta, K.; Tsubaki, A. Relationship between the face scale for rating of perceived exertion and physiological parameters in older adults and patients with atrial fibrillation. Physiol. Rep. 2021, 9, e14759. [Google Scholar] [CrossRef]
- Zwaard, S.; Graafland, F.H.; van Middelkoop, C.; Lintmeijer, L. Validity and Reliability of Facial Rating of Perceived Exertion Scales for Training Load Monitoring. J. Strength Cond. Res. 2022, 10, 1519. [Google Scholar]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Galuska, D.A.; George, S.M.; Olson, R.D. The physical activity guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, K.; Graff, M.; Hedt, C.; Simmons, J. Reliability and validity of a smartphone pulse rate application for the assessment of resting and elevated pulse rate. Physiother. Theory Pract. 2016, 32, 494–499. [Google Scholar] [CrossRef]
- Silva, T.D.; da Silva, P.L.; Valenzuela, E.J.; Dias, E.D.; Simcsik, A.O.; Carvalho, M.G.; Fontes, A.M.G.F.; Alberissi, C.A.O.; Araújo, L.V.; Brandão, M.V.C.; et al. Serious game platform as a possibility for home-based telerehabilitation for individuals with Cerebral Palsy during COVID-19 quarantine–A cross-sectional pilot study. Front. Psychol. 2021, 12, 622678. [Google Scholar] [CrossRef]
- Araújo, A.V.L.; Neiva, J.F.O.; Monteiro, C.B.M.; Magalhães, F.H. Efficacy of virtual reality rehabilitation after spinal cord injury: A systematic review. BioMed Res. Int. 2019, 2019, 7106951. [Google Scholar] [CrossRef] [PubMed]
- Silveira, A.C.; Moraes, I.A.P.; Vidigal, G.P.; Simcsik, A.O.; Rosa, R.M.; Favero, F.M.; Fernandes, S.M.S.; Garner, D.M.; Araújo, L.V.; Massa, M.; et al. Cardiac Autonomic Modulation in Subjects with Amyotrophic Lateral Sclerosis (ALS) during an Upper Limb Virtual Reality Task: A Prospective Control Trial. BioMed Res. Int. 2022, 2022, 4439681. [Google Scholar] [CrossRef] [PubMed]
- González-Agüero, A.; Vicente-Rodríguez, G.; Moreno, L.A.; Casajús, J.A. Bone mass in male and female children and adolescents with Down syndrome. Osteoporos. Int. 2011, 22, 2151–2157. [Google Scholar] [CrossRef]
- Menezes, R.T.; Amorim, A.R.A.; Blascovi-Assis, S.M. Atividade física e lazer na síndrome de Down: Uma revisão integrativa. Cad. Pós-Grad. Distúrbios Desenvolv. 2021, 21, 144–165. [Google Scholar] [CrossRef]
- Jover, M.; Ayoun, C.; Berton, C.; Carlier, M. Development of motor planning for dexterity tasks in trisomy 21. Res. Dev. Disabil. 2014, 35, 1562–1570. [Google Scholar] [CrossRef] [PubMed]
- Gunbey, H.B.; Bilgici, M.C.; Aslan, K.; Has, A.C.; Ogur, M.G.; Alhan, A.; Incesu, L. Structural brain alterations of Down’s syndrome in early childhood evaluation by DTI and volumetric analyses. Eur. Radiol. 2017, 27, 3013–3021. [Google Scholar] [CrossRef] [PubMed]
- Latash, M.L.; Anson, J.G. Synergies in health and disease: Relations to adaptive changes in motor coordination. Phys. Ther. 2006, 86, 1151–1160. [Google Scholar] [CrossRef]
- Anson, J.G. Neuromotor control and down syndrome. In Approaches to the Study of Motor Control and Learning; Summers, J.J., Ed.; Elsevier Science Publishers: Amsterdam, The Netherlands, 1992; pp. 387–412. [Google Scholar]
- Antonarakis, S.E.; Skotko, B.G.; Rafii, M.S.; Strydom, A.; Pape, S.E.; Bianchi, D.W.; Sherman, S.L.; Reeves, R.H. Down syndrome. Nat. Rev. Dis. Prim. 2020, 6, 9. [Google Scholar] [CrossRef]
- Kokol, P.; Vošner, H.B.; Završnik, J.; Vermeulen, J.; Shohieb, S.; Peinemann, F. Serious game-based intervention for children with developmental disabilities. Curr. Pediatr. Rev. 2020, 16, 26–32. [Google Scholar] [PubMed]
- Mon-Williams, M.; Tresilian, J.R.; Bell, V.E.; Coppard, V.L.; Jobling, A.; Carson, R.G. The preparation of reach to grasp movements in adults with Down syndrome. Hum. Mov. Sci. 2001, 20, 587–602. [Google Scholar] [CrossRef] [PubMed]
- Meegan, S.; Maraj, B.K.V.; Weeks, D.; Chua, R. Gross motor skill acquisition in adolescents with Down syndrome. Down Syndr. Res. Pract. 2006, 9, 75–80. [Google Scholar] [CrossRef] [PubMed]



| DS | TD | |
|---|---|---|
| Participants | 34 | 34 |
| Mean age | 18.9 (±6.1) | 19.0 (±1.6) |
| Active 1 | 13 (38.2%) | 10 (28.6%) |
| Very active 1 | 6 (17.6%) | 5 (14.3%) |
| Irregularly active 1 | 8 (23.5%) | 9 (25.7%) |
| Sedentary 1 | 7 (20.6%) | 10 (28.6%) |
| Cellphone 2 | 32 (94.1%) | 34 (100.0%) |
| Tablet 2 | 24 (70.6%) | 18 (51.4%) |
| Computer/laptop 2 | 23 (67.6%) | 32 (91.4%) |
| TV 2 | 33 (97.1%) | 33 (94.3%) |
| Video game 2 | 4 (11.8%) | 22 (62.9%) |
| <3 h/week 3 | 1 (2.9%) | 0 (0%) |
| 3–6 h/week 3 | 1 (2.9%) | 1 (2.9%) |
| 7–10 h/week 3 | 3 (8.8%) | 3 (8.6%) |
| >10 h/week 3 | 29 (85.3%) | 30 (85.7%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosa, R.M.; Tezza, M.H.S.; Valenzuela, E.d.J.; Dias, E.D.; de Moraes, Í.A.P.; de Araujo, L.V.; Ré, A.H.N.; da Silva, T.D.; Monteiro, C.B.d.M. Analysis of Heart Rate, Perception of Physical Effort and Performance of Individuals with Down Syndrome Submitted to a Protocol of Virtual Games for Home-Based Telerehabilitation. Healthcare 2023, 11, 1894. https://doi.org/10.3390/healthcare11131894
Rosa RM, Tezza MHS, Valenzuela EdJ, Dias ED, de Moraes ÍAP, de Araujo LV, Ré AHN, da Silva TD, Monteiro CBdM. Analysis of Heart Rate, Perception of Physical Effort and Performance of Individuals with Down Syndrome Submitted to a Protocol of Virtual Games for Home-Based Telerehabilitation. Healthcare. 2023; 11(13):1894. https://doi.org/10.3390/healthcare11131894
Chicago/Turabian StyleRosa, Renata Martins, Maria Helena Santos Tezza, Elisa de Jesus Valenzuela, Eduardo Dati Dias, Íbis Ariana Peña de Moraes, Luciano Vieira de Araujo, Alessandro Hervaldo Nicolai Ré, Talita Dias da Silva, and Carlos Bandeira de Mello Monteiro. 2023. "Analysis of Heart Rate, Perception of Physical Effort and Performance of Individuals with Down Syndrome Submitted to a Protocol of Virtual Games for Home-Based Telerehabilitation" Healthcare 11, no. 13: 1894. https://doi.org/10.3390/healthcare11131894
APA StyleRosa, R. M., Tezza, M. H. S., Valenzuela, E. d. J., Dias, E. D., de Moraes, Í. A. P., de Araujo, L. V., Ré, A. H. N., da Silva, T. D., & Monteiro, C. B. d. M. (2023). Analysis of Heart Rate, Perception of Physical Effort and Performance of Individuals with Down Syndrome Submitted to a Protocol of Virtual Games for Home-Based Telerehabilitation. Healthcare, 11(13), 1894. https://doi.org/10.3390/healthcare11131894








