Empirical Analysis of Preferences of Older Adults for Care Facilities in Japan: Focusing on Household Structure and Economic Status
Abstract
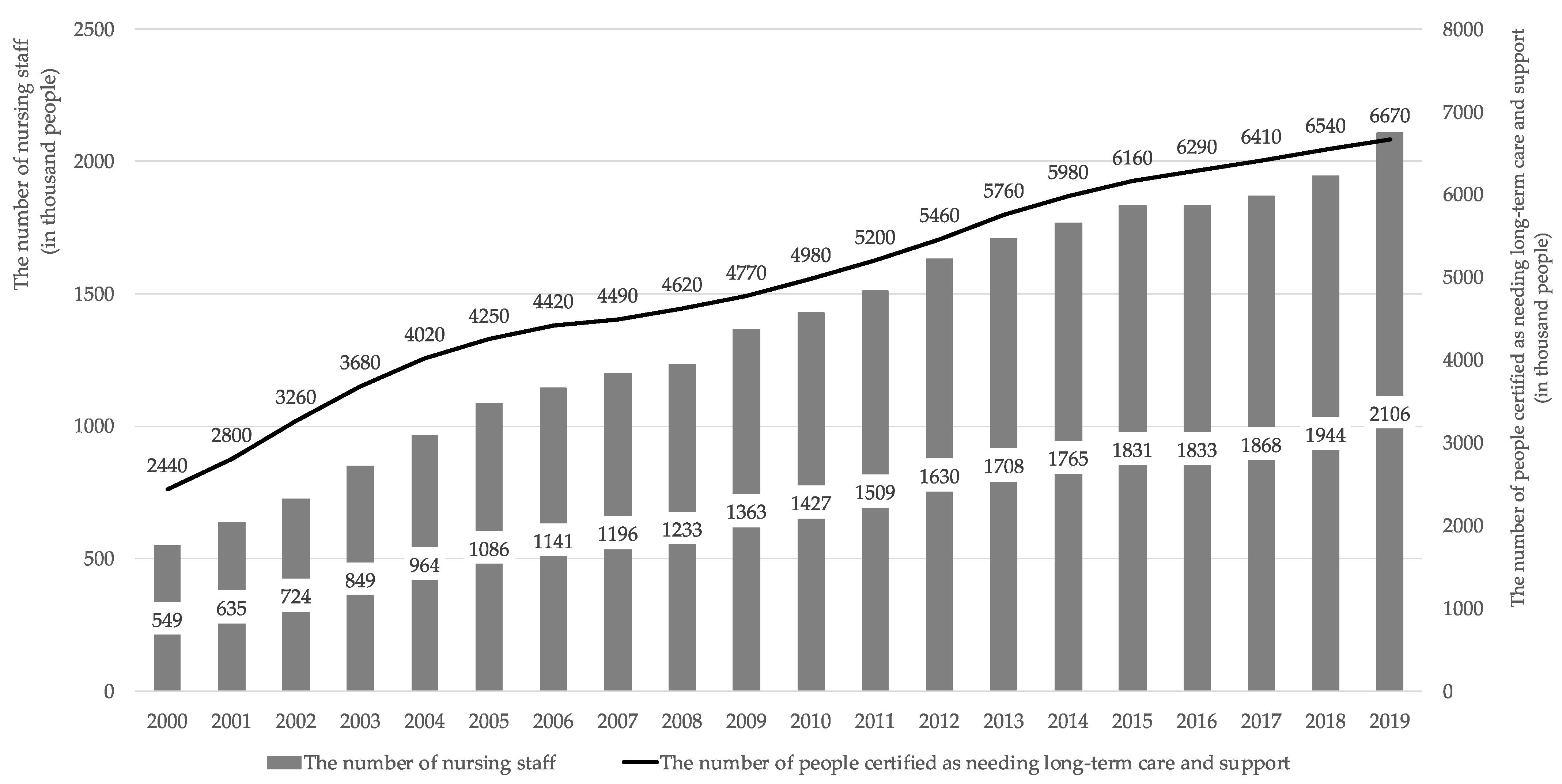
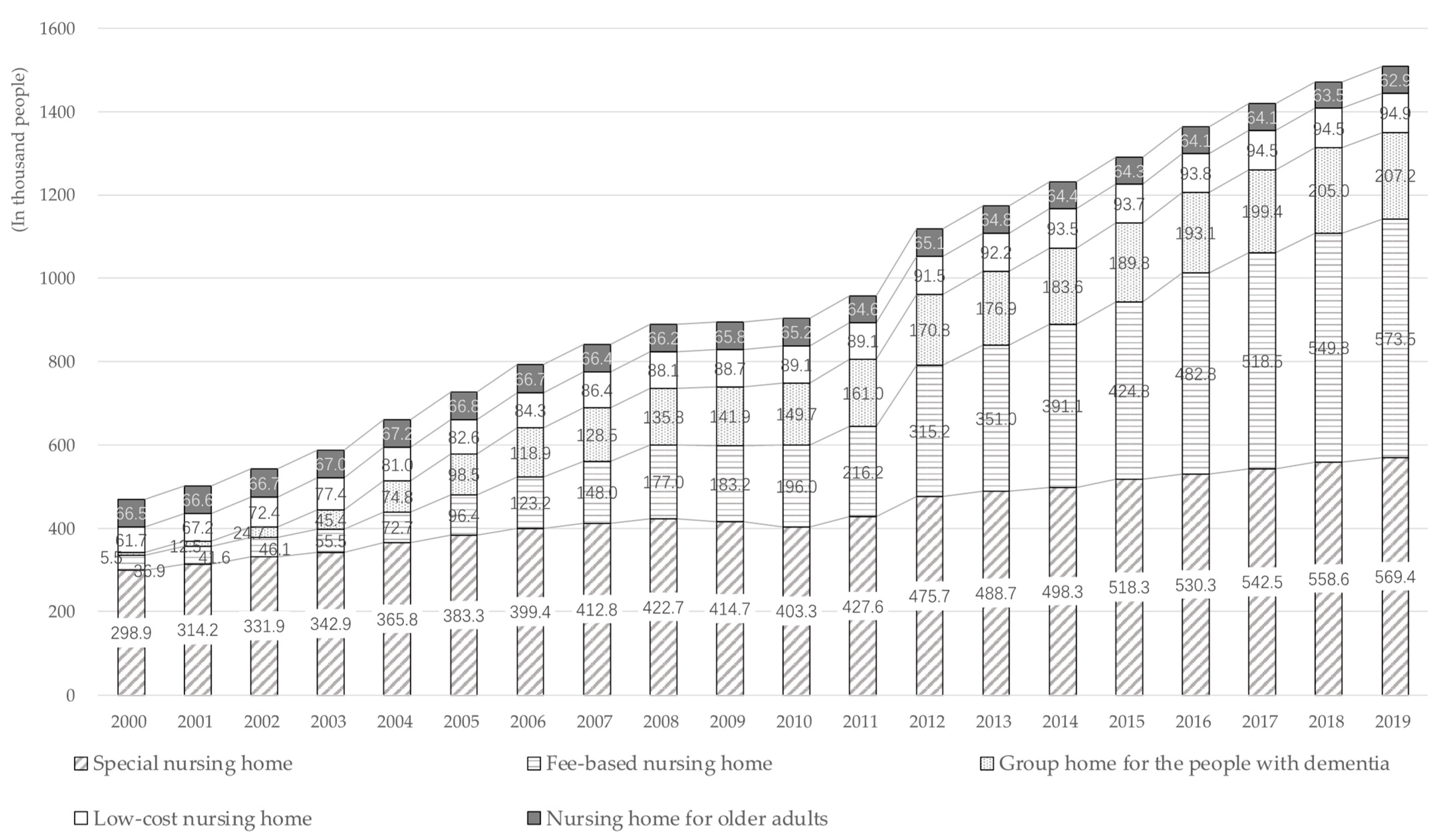
1. Introduction
2. Materials and Methods
2.1. Data
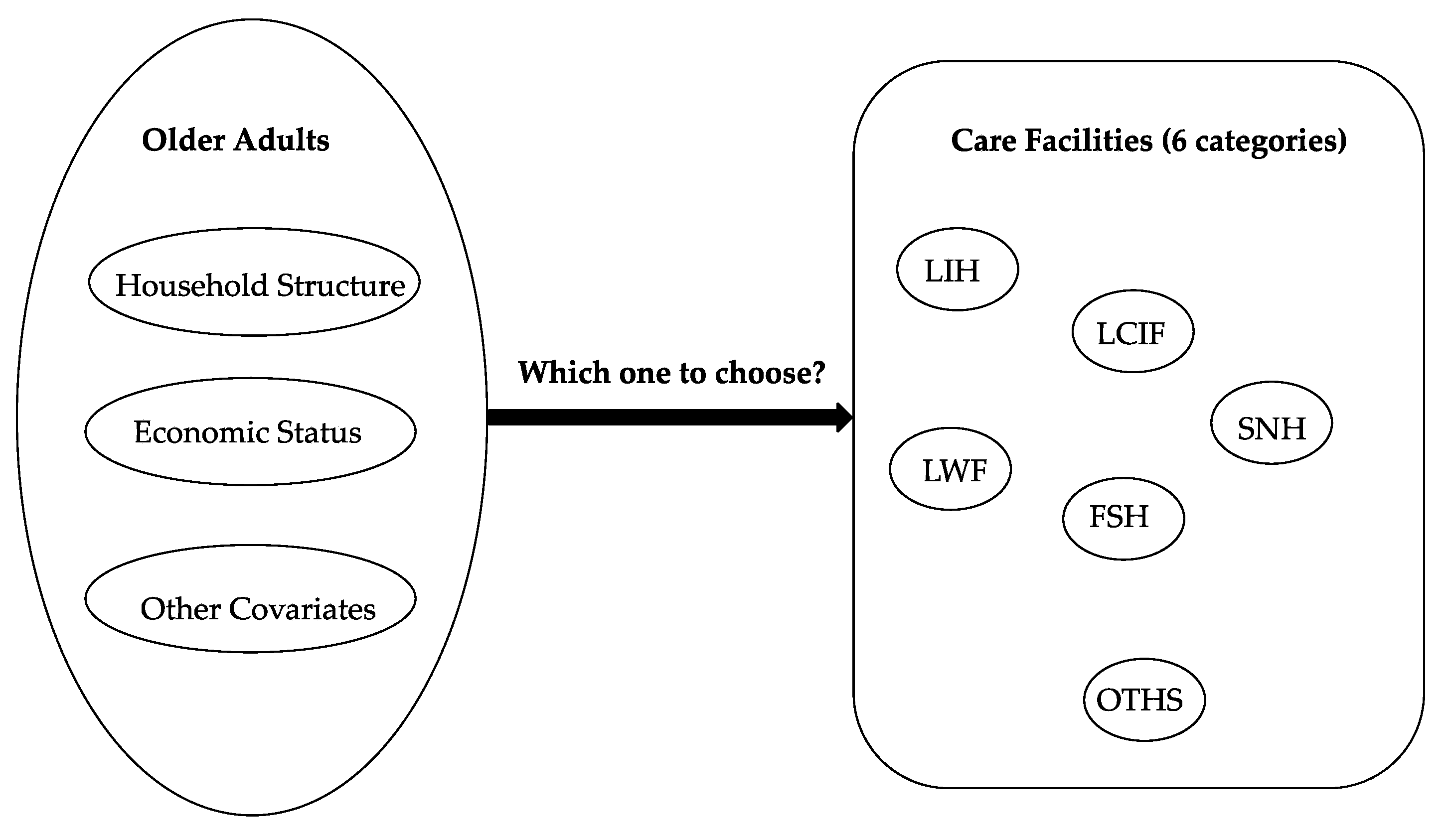
2.2. Dependent Variables
- “I want to continue living in my current house (LIH).”
- “I want to live in an LTCI care facility for people certified as requiring long-term care, such as a special nursing home for older adults (LCIF).”
- “I want to live in a relatively small-scale special nursing home for older adults or a group home for people with dementia (SNH).”
- “I want to live in a welfare facility for low-income older adults, such as a low-cost nursing home (care house), etc. (LWF).”
- “I want to live in a fee-based nursing home or nursing home with diverse services and high cost for the older adults (FSH).”
- “Other, such as living with relatives, etc. (OTHS).”
2.3. Independent Variables
2.4. Estimation Framework
3. Results
3.1. Estimation Results of Analysis I
3.2. Estimation Results of Analysis II
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ministry of Internal Affairs and Communications, Population Estimates. 2021. Available online: https://www.stat.go.jp/data/jinsui/2021np/index.html (accessed on 16 May 2023). (In Japanese).
- National Institute of Population and Social Security Research (IPSS). Population Projections for Japan. Available online: https://www.ipss.go.jp/syoushika/tohkei/Mainmenu.asp (accessed on 6 June 2023). (In Japanese)
- Campbell, J.C.; Ikegami, N. Long-term care insurance comes to Japan. Health Aff. 2000, 19, 26–39. [Google Scholar] [CrossRef] [PubMed]
- Tamiya, N.; Noguchi, H.; Nishi, A.; Reich, M.R.; Ikegami, N.; Hashimoto, H.; Shibuya, K.; Kawachi, I.; Campbell, J.C. Population ageing and wellbeing: Lessons from Japan’s long-term care insurance policy. Lancet 2011, 378, 1183–1192. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labor and Welfare. Overview of Survey on Nursing Care Service Facilities and Businesses. 2000–2019. Available online: https://www.e-stat.go.jp/stat-search/files?page=1&toukei=00450042&tstat=000001029805 (accessed on 16 May 2023). (In Japanese)
- Ministry of Health, Labor and Welfare. Long-Term Care Insurance Business Status Report. 2000–2019. Available online: https://www.mhlw.go.jp/topics/0103/tp0329-1.html (accessed on 16 May 2023). (In Japanese)
- Ministry of Health, Labor and Welfare. About the Situation Surrounding the Nursing Care Field. 2020. Available online: https://www.mhlw.go.jp/content/12300000/000608284.pdf (accessed on 12 June 2023). (In Japanese)
- Cabinet Office. White Paper on the Aging Society (Whole Version). 2020. Available online: https://www8.cao.go.jp/kourei/whitepaper/w-2022/html/zenbun/s1_2_2.html (accessed on 12 June 2023). (In Japanese)
- Takashi, M. Two Major Constraints Faced by the Long-Term Care Insurance System: How to Use Science-Based Nursing to Address Financial and Human Resource Shortages. J-STAGE. 2022. Available online: https://doi.org/10.57538/consumercoopstudies.558.0_15 (accessed on 6 June 2023). (In Japanese).
- Ministry of Health, Labor and Welfare. Overview of the Long-Term Care Insurance System. 2021. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/hukushi_kaigo/kaigo_koureisha/gaiyo/index.html (accessed on 6 June 2023). (In Japanese)
- Ministry of Health, Labor and Welfare. Recent Trends in the Long-Term Care Insurance System. 2022. Available online: https://www.mhlw.go.jp/content/12300000/000917423.pdf (accessed on 6 June 2023). (In Japanese)
- Ministry of Health, Labor and Welfare. Efforts to Secure Nursing Workers. Available online: https://www.mhlw.go.jp/stf/newpage_02977.html (accessed on 6 June 2023). (In Japanese)
- Higginson, I.J.; Daveson, B.A.; Morrison, R.S.; Yi, D.; Meier, D.; Smith, M.; Ryan, K.; McQuillan, R.; Johnston, B.M.; Normand, C.; et al. Social and clinical determinants of preferences and their achievement at the end of life: Prospective cohort study of older adults receiving palliative care in three countries. BMC Geriatr. 2017, 17, 271. Available online: https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-017-0648-4 (accessed on 6 June 2023). [CrossRef] [PubMed]
- World Health Organization. Integrated Care for Older People: Guidelines on Community-Level Interventions to Manage Declines in Intrinsic Capacity. 2017. Available online: https://www.who.int/publications/i/item/9789241550109 (accessed on 6 June 2023).
- Jun, K. The Effects of Social Networks on Wishes for Long-Term Care among the Elderly. The Quarterly of Social Security Research. 2014. Available online: https://www.ipss.go.jp/syoushika/bunken/data/pdf/19919005.pdf (accessed on 9 June 2023). (In Japanese).
- Sugisawa, H.; Sugihara, Y.; Nakatani, Y. Long-term care preference among Japanese older adults: Differences by age, period and cohort. Ageing Soc. 2020, 40, 1309–1333. [Google Scholar] [CrossRef]
- Zhang, Z.; Kato, C.; Yoshiomi, O. Factors influencing the preferences of older Japanese people for long-term care. Home Health Care Manag. Pract. 2023, 35. [Google Scholar] [CrossRef]
- Ministry of Internal Affairs and Communications. The Summary of Results of 2019 National Household Structure Survey Results on Annual Income, Asset Distribution. 2021. Available online: https://www.stat.go.jp/data/zenkokukakei/2019/pdf/gaiyou0831.pdf (accessed on 6 June 2023). (In Japanese)
- Gender Equality Bureau Cabinet Office. White Paper on Gender Equality. 2012. Available online: https://www.gender.go.jp/about_danjo/whitepaper/h24/zentai/html/honpen/b1_s05_01.html (accessed on 6 June 2023). (In Japanese)
- Jeon, B.; Noguchi, H.; Kwon, S.; Ito, T.; Tamiya, N. Disability, poverty, and role of the basic livelihood security system on health services utilization among the elderly in South Korea. Soc. Sci. Med. 2017, 178, 175–183. Available online: https://pubmed.ncbi.nlm.nih.gov/28237862/ (accessed on 16 May 2023). [CrossRef] [PubMed]
- Health and Welfare Bureau of Sakai. Osaka Prefecture, Japan. A Survey on Older Adults of Sakai City. Conducted by Longevity Support Division of Longevity Society Department. 2019. Available online: https://www.city.sakai.lg.jp/shisei/gyosei/shishin/fukushi/kourei-kaigo_keikaku/75402820211117160542577.html (accessed on 16 May 2023). (In Japanese).
- Yifan, L.; Mercedes, B. Change of health and change of preferences on life-sustaining treatment: Evidence from a longitudinal study. Innov. Aging 2021, 5 (Suppl. 1), 19–20. [Google Scholar] [CrossRef]
- Ministry of Health, Labor and Welfare. Overview of the 2019 Comprehensive Survey of Living Conditions. 2019. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa19/index.html (accessed on 16 May 2023). (In Japanese)
- Etkind, S.N.; Bone, A.E.; Lovell, N.; Higginson, I.J.; Murtagh, F.E.M. Influences on care preferences of older people with advanced illness: A systematic review and thematic synthesis. J. Am. Geriatr. Soc. 2018, 66, 1031–1039. [Google Scholar] [CrossRef] [PubMed]
- Costa-Font, J.; Elvira, D.; Mascarilla-Miró, O. ‘Ageing in Place’? Exploring Elderly People’s Housing Preferences in Spain. Urban Stud. 2009, 46, 295–316. [Google Scholar] [CrossRef]
- Cameron, A.C.; Trivedi, P. Microeconometrics Methods and Applications; Cambridge University Press: Cambridge, UK, 2005; pp. 467–494. [Google Scholar]
- Ministry of Health, Labor and Welfare. Recent Trends in the Field of Nursing Care. 2016. Available online: https://www.mhlw.go.jp/file/05-Shingikai-12601000-Seisakutoukatsukan-Sanjikanshitsu_Shakaihoshoutantou/0000112916.pdf (accessed on 16 May 2023).
- Gaugler, J.E.; Edwards, A.B.; Femia, E.E.; Zarit, S.H.; Stephens, M.A.; Townsend, A.; Greene, R. Predictors of institutionalization of cognitively impaired elders: Family help and the timing of placement. J. Gerontol. B Psychol. Sci. Soc. Sci. 2000, 55, P247–P255. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, A.E.; Matthias, R.E.; Kietzman, K.; Furman, W. Retention of paid related caregivers: Who stays and who leaves home care careers? Gerontologist 2008, 48, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.T.; Lam, L.C.; Kwok, T.; Ng, N.S.; Fung, A.W. The social networks of Hong Kong Chinese family caregivers of Alzheimer’s disease: Correlates with positive gains and burden. Gerontologist 2013, 53, 998–1008. [Google Scholar] [CrossRef] [PubMed]
- Schölzel-Dorenbos, C.J.; Draskovic, I.; Vernooij-Dassen, M.J.; Olde Rikkert, M.G. Quality of life and burden of spouses of Alzheimer disease patients. Alzheimer Dis. Assoc. Disord. 2009, 23, 171–177. Available online: https://journals.lww.com/alzheimerjournal/Fulltext/2009/04000/Assessment_of_Quality_of_Life_as_Outcome_in.12.aspx?casa_token=vpQnBpyidysAAAAA:pjj9N8o3G2-a6Oa1j5zWNDlCic8ARZoPDid0OTiShwKIAjrUD22E5wNK-dEYXgNC9M4GmwyLGmC2E_YrqxxM4g (accessed on 6 June 2023). [CrossRef] [PubMed]
- Hughes, S.L.; Giobbie-Hurder, A.; Weaver, F.M.; Kubal, J.D.; Henderson, W. Relationship between caregiver burden and health-related quality of life. Gerontologist 1999, 39, 534–545. [Google Scholar] [CrossRef] [PubMed]
- Clyburn, L.D.; Stones, M.J.; Hadjistavropoulos, T.; Tuokko, H. Predicting caregiver burden and depression in Alzheimer’s disease. J. Gerontol. B Psychol. Sci. Soc. Sci. 2000, 55, S2–S13. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare. Intermediate Arrangement of Discussions at the Study Group on Improving the Qualifications of Care Managers. 2013. Available online: https://www.mhlw.go.jp/stf/shingi/2r9852000002s7f7-att/2r9852000002s7go.pdf (accessed on 13 June 2023). (In Japanese)
- Tomoko, W. Factors related to the caregiving burden of informal caregivers. J. Soc. Sec. Res. 2021, 6, 33–44. Available online: https://www.komei.or.jp/km/otsu-sato-hiroshi/files/2021/08/c6de2a343c6fb49c0ff27a4415b62433.pdf (accessed on 13 June 2023). (In Japanese).
- Official Statistics Portal (Japan). National Household Structure Survey, Results on Annual Income and Asset Distribution. 2019; Volume 2019. Available online: https://www.e-stat.go.jp/dbview?sid=0003440478 (accessed on 6 June 2023). (In Japanese)
- Sawako, S. Changes in Demographic Structure and Economic Gap; The Japan Institute of Labour: Tokyo, Japan, 2018; Available online: https://www.jil.go.jp/institute/zassi/backnumber/2018/01/pdf/044-054.pdf (accessed on 6 June 2023). (In Japanese)
- Cabinet Office. White Paper on the Aging Society (Whole Version). 2010. Available online: https://www8.cao.go.jp/kourei/whitepaper/w-2010/zenbun/html/s1-3-3-02.html (accessed on 12 June 2023). (In Japanese)
- Wang, Z.; Fukayama, K.; Niu, B. Does long-term care literacy matter in evaluating older care recipients’ satisfaction with care managers? Empirical evidence from Japanese survey data. Int. J. Environ. Res. Public Health 2023, 20, 2456. [Google Scholar] [CrossRef] [PubMed]
- Cabinet Office. Survey on the Daily Life and Participation in Local Communities of Older People. 2021. Available online: https://www8.cao.go.jp/kourei/ishiki/r03/zentai/pdf_index.html (accessed on 13 June 2023). (In Japanese)
- Sakai City, Population Estimates. 2021. Available online: https://www.city.sakai.lg.jp/shisei/tokei/suikei.html (accessed on 16 May 2023). (In Japanese).
- Sakai City, Population by Age in All Cities/Areas. 2021. Available online: https://www.city.sakai.lg.jp/shisei/tokei/nenreibetsu/zensikunenrei.html (accessed on 16 May 2023). (In Japanese).


| Variable | Obs | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|---|
| Dependent Variables | |||||
| Analysis I: Care facilities (Categories of care facilities) | 5178 | 0.72 | 1.41 | 0 | 5 |
| Analysis II: Each care facility | |||||
| (1) LIH | 5332 | 0.74 | 0.44 | 0 | 1 |
| (2) LCIF | 5332 | 0.03 | 0.18 | 0 | 1 |
| (3) SNH | 5332 | 0.03 | 0.18 | 0 | 1 |
| (4) LWF | 5332 | 0.09 | 0.28 | 0 | 1 |
| (5) FSH | 5332 | 0.05 | 0.22 | 0 | 1 |
| (6) OTHS | 5332 | 0.03 | 0.17 | 0 | 1 |
| Main Independent Variables | |||||
| Household structure: | |||||
| Living alone | 5226 | 0.21 | 0.41 | 0 | 1 |
| Couple only | 5226 | 0.49 | 0.50 | 0 | 1 |
| Other structures | 5226 | 0.30 | 0.46 | 0 | 1 |
| Economic status (self-assessed): | |||||
| Experiencing poverty | 5308 | 0.34 | 0.47 | 0 | 1 |
| Normal | 5308 | 0.58 | 0.49 | 0 | 1 |
| Wealthy | 5308 | 0.08 | 0.27 | 0 | 1 |
| Interaction term: | |||||
| Living Alone and Experiencing Poverty | 5205 | 0.08 | 0.28 | 0 | 1 |
| Other Covariates | |||||
| Sex: | |||||
| Male | 5332 | 0.43 | 0.49 | 0 | 1 |
| Age: | |||||
| 65–69 y | 5332 | 0.23 | 0.42 | 0 | 1 |
| 70–74 y | 5332 | 0.28 | 0.45 | 0 | 1 |
| 75–79 y | 5332 | 0.27 | 0.45 | 0 | 1 |
| 80+ y | 5332 | 0.22 | 0.41 | 0 | 1 |
| Health status: | |||||
| IADL (dependent) | 5216 | 0.11 | 0.31 | 0 | 1 |
| Subjective health (healthy) | 5257 | 0.80 | 0.40 | 0 | 1 |
| Variable | LCIF (ref: LIH) | SNH (ref: LIH) | LWF (ref: LIH) | FSH (ref: LIH) | OTHS (ref: LIH) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | SE | OR | SE | OR | SE | OR | SE | OR | SE | ||||||
| Household structure (ref: living alone) | |||||||||||||||
| Couple only | 0.61 | ** | 0.11 | 1.08 | 0.23 | 0.51 | *** | 0.07 | 0.52 | *** | 0.08 | 0.62 | * | 0.14 | |
| Others | 0.29 | *** | 0.07 | 0.80 | 0.19 | 0.64 | *** | 0.09 | 0.46 | *** | 0.08 | 0.81 | 0.19 | ||
| Economic status (self-assessed) (ref: normal) | |||||||||||||||
| Experiencing poverty | 1.17 | 0.20 | 1.20 | 0.21 | 2.37 | *** | 0.25 | 0.54 | *** | 0.09 | 1.13 | 0.21 | |||
| Wealthy | 0.50 | ** | 0.20 | 0.67 | 0.24 | 0.26 | *** | 0.10 | 1.89 | *** | 0.34 | 1.33 | 0.37 | ||
| Sex (ref: female) | |||||||||||||||
| Male | 0.88 | 0.15 | 0.83 | 0.14 | 0.66 | *** | 0.07 | 0.79 | 0.11 | 1.02 | 0.18 | ||||
| Age (ref: 80+ y) | |||||||||||||||
| 65–69 y | 0.95 | 0.25 | 1.17 | 0.28 | 1.17 | 0.19 | 1.25 | 0.24 | 2.34 | ** | 0.66 | ||||
| 70–74 y | 1.22 | 0.28 | 1.04 | 0.24 | 1.15 | 0.17 | 0.87 | 0.17 | 2.07 | ** | 0.57 | ||||
| 75–79 y | 1.34 | 0.31 | 0.88 | 0.21 | 1.07 | 0.16 | 1.14 | 0.21 | 1.40 | 0.42 | |||||
| Health status | |||||||||||||||
| IADL (dependent) | 0.83 | 0.23 | 0.90 | 0.24 | 0.91 | 0.16 | 1.02 | 0.24 | 0.55 | ** | 0.20 | ||||
| Subjective health (healthy) | 0.56 | ** | 0.10 | 0.48 | *** | 0.09 | 0.63 | *** | 0.08 | 0.86 | 0.15 | 0.62 | * | 0.13 | |
| Constant | 0.11 | *** | 0.03 | 0.08 | *** | 0.02 | 0.21 | *** | 0.04 | 0.15 | *** | 0.03 | 0.04 | *** | 0.01 |
| Number of obs | 4906 | ||||||||||||||
| Variables | LIH | LCIF | SNH | ||||||
| ME | SE | ME | SE | ME | SE | ||||
| Household structure (ref: other categories) | |||||||||
| Living alone | −0.128 | *** | 0.022 | 0.020 | ** | 0.010 | 0.001 | 0.008 | |
| Economic status (self-assessed) (ref: other categories) | |||||||||
| Experiencing poverty | −0.079 | *** | 0.016 | 0.002 | 0.006 | 0.007 | 0.006 | ||
| Interaction term | |||||||||
| Living Alone and Experiencing Poverty | 0.033 | 0.028 | 0.003 | 0.012 | −0.013 | 0.009 | |||
| Sex (ref: female) | |||||||||
| Male | 0.048 | *** | 0.013 | −0.000 | 0.005 | −0.003 | 0.005 | ||
| Age (ref: 80+ y) | |||||||||
| 65–69 y | −0.036 | * | 0.020 | −0.004 | 0.008 | 0.004 | 0.008 | ||
| 70–74 y | −0.020 | 0.019 | 0.005 | 0.008 | 0.001 | 0.007 | |||
| 75–79 y | −0.021 | 0.019 | 0.009 | 0.008 | −0.004 | 0.007 | |||
| Health status | |||||||||
| IADL (dependent) | 0.017 | 0.021 | −0.004 | 0.008 | −0.002 | 0.008 | |||
| Subjective health (healthy) | 0.097 | *** | 0.017 | −0.016 | ** | 0.008 | −0.023 | *** | 0.008 |
| Number of obs | 5036 | 5036 | 5036 | ||||||
| Variables | LWF | FSH | OTHS | ||||||
| ME | SE | ME | SE | ME | SE | ||||
| Household structure (ref: other categories) | |||||||||
| Living alone | 0.059 | *** | 0.016 | 0.038 | *** | 0.011 | −0.005 | 0.007 | |
| Economic status (self-assessed) (ref: other categories) | |||||||||
| Experiencing poverty | 0.091 | *** | 0.011 | −0.030 | *** | 0.007 | −0.007 | 0.005 | |
| Interaction term | |||||||||
| Living Alone and Experiencing Poverty | −0.027 | ** | 0.013 | −0.019 | * | 0.011 | 0.034 | * | 0.020 |
| Sex (ref: female) | |||||||||
| Male | −0.030 | *** | 0.008 | −0.007 | 0.006 | 0.001 | 0.005 | ||
| Age (ref: 80+ y) | |||||||||
| 65–69 y | 0.010 | 0.012 | 0.010 | 0.010 | 0.026 | ** | 0.010 | ||
| 70–74 y | 0.010 | 0.012 | −0.007 | 0.008 | 0.021 | ** | 0.009 | ||
| 75–79 y | 0.004 | 0.011 | 0.004 | 0.009 | 0.008 | 0.008 | |||
| Health status | |||||||||
| IADL (dependent) | −0.003 | 0.013 | −0.001 | 0.010 | −0.013 | ** | 0.006 | ||
| Subjective health (healthy) | −0.031 | *** | 0.011 | 0.000 | 0.008 | −0.010 | 0.007 | ||
| Number of obs | 5036 | 5036 | 5036 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, J.; Wang, Z.; Niu, B. Empirical Analysis of Preferences of Older Adults for Care Facilities in Japan: Focusing on Household Structure and Economic Status. Healthcare 2023, 11, 1843. https://doi.org/10.3390/healthcare11131843
Wang J, Wang Z, Niu B. Empirical Analysis of Preferences of Older Adults for Care Facilities in Japan: Focusing on Household Structure and Economic Status. Healthcare. 2023; 11(13):1843. https://doi.org/10.3390/healthcare11131843
Chicago/Turabian StyleWang, Jinhan, Ziyan Wang, and Bing Niu. 2023. "Empirical Analysis of Preferences of Older Adults for Care Facilities in Japan: Focusing on Household Structure and Economic Status" Healthcare 11, no. 13: 1843. https://doi.org/10.3390/healthcare11131843
APA StyleWang, J., Wang, Z., & Niu, B. (2023). Empirical Analysis of Preferences of Older Adults for Care Facilities in Japan: Focusing on Household Structure and Economic Status. Healthcare, 11(13), 1843. https://doi.org/10.3390/healthcare11131843





