Effects of Diamond Steps Exercises on Balance Improvement in Healthy Young and Older Adults: A Protocol Proposal †
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
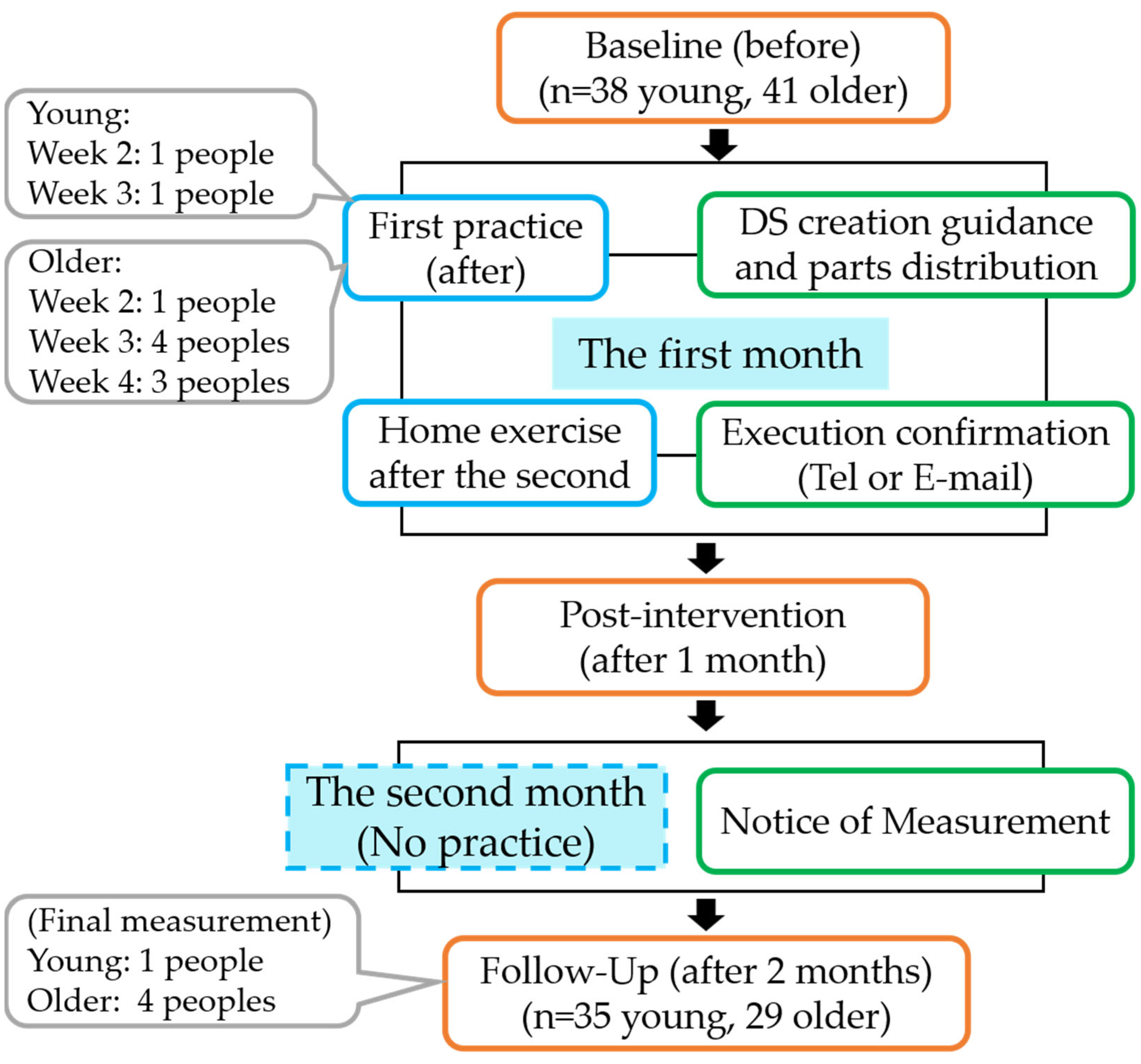
2.2. Study Design and Implementation Procedure
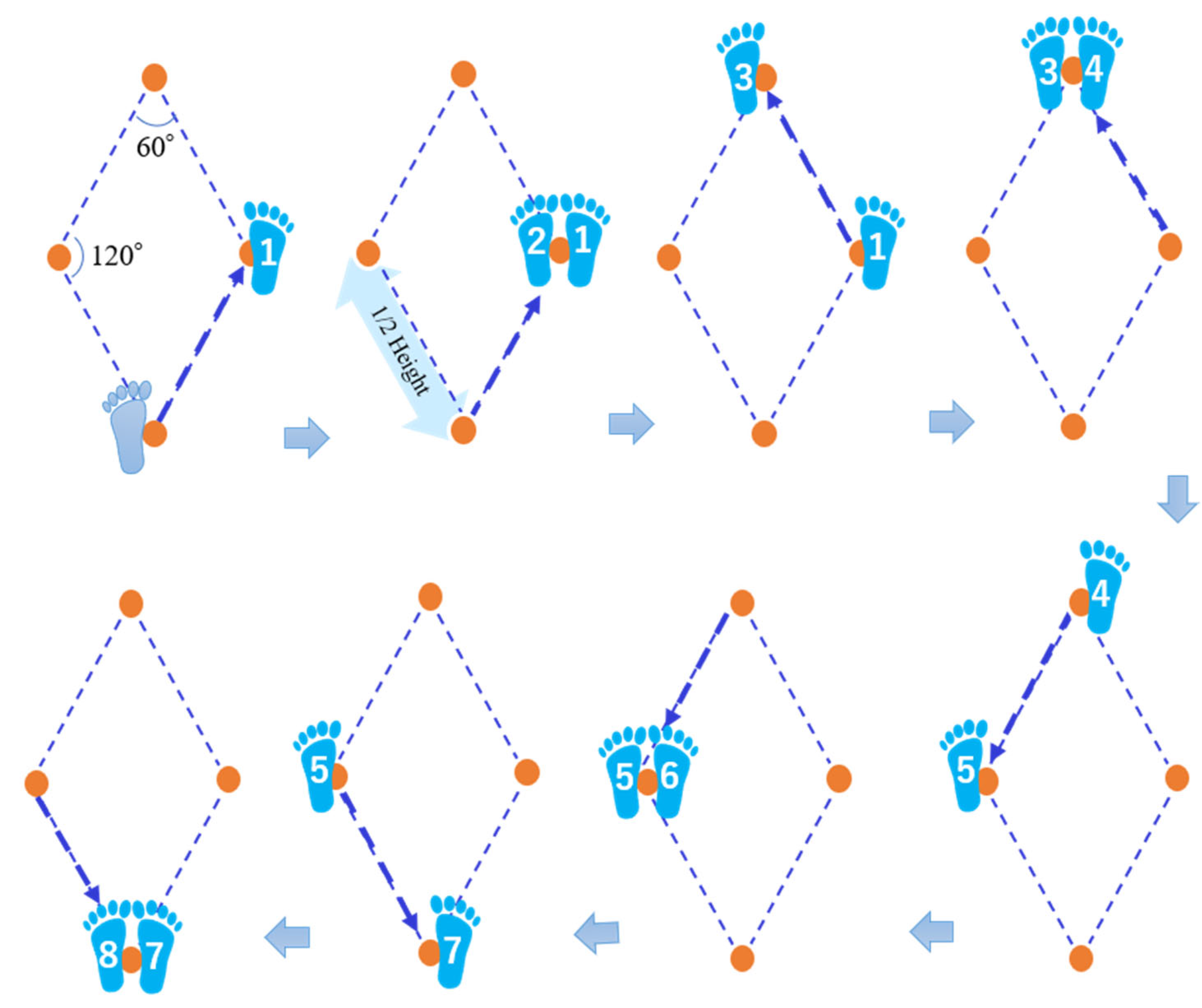
2.2.1. DS Exercises
2.2.2. Assessment of Physical Performance
2.2.3. Lower Limb Muscle Strength
2.2.4. Static Balance
2.2.5. Dynamic Balance
2.2.6. Agility
2.2.7. Flexibility
2.3. Subjective Evaluation of DS Exercises
2.4. Statistical Analysis
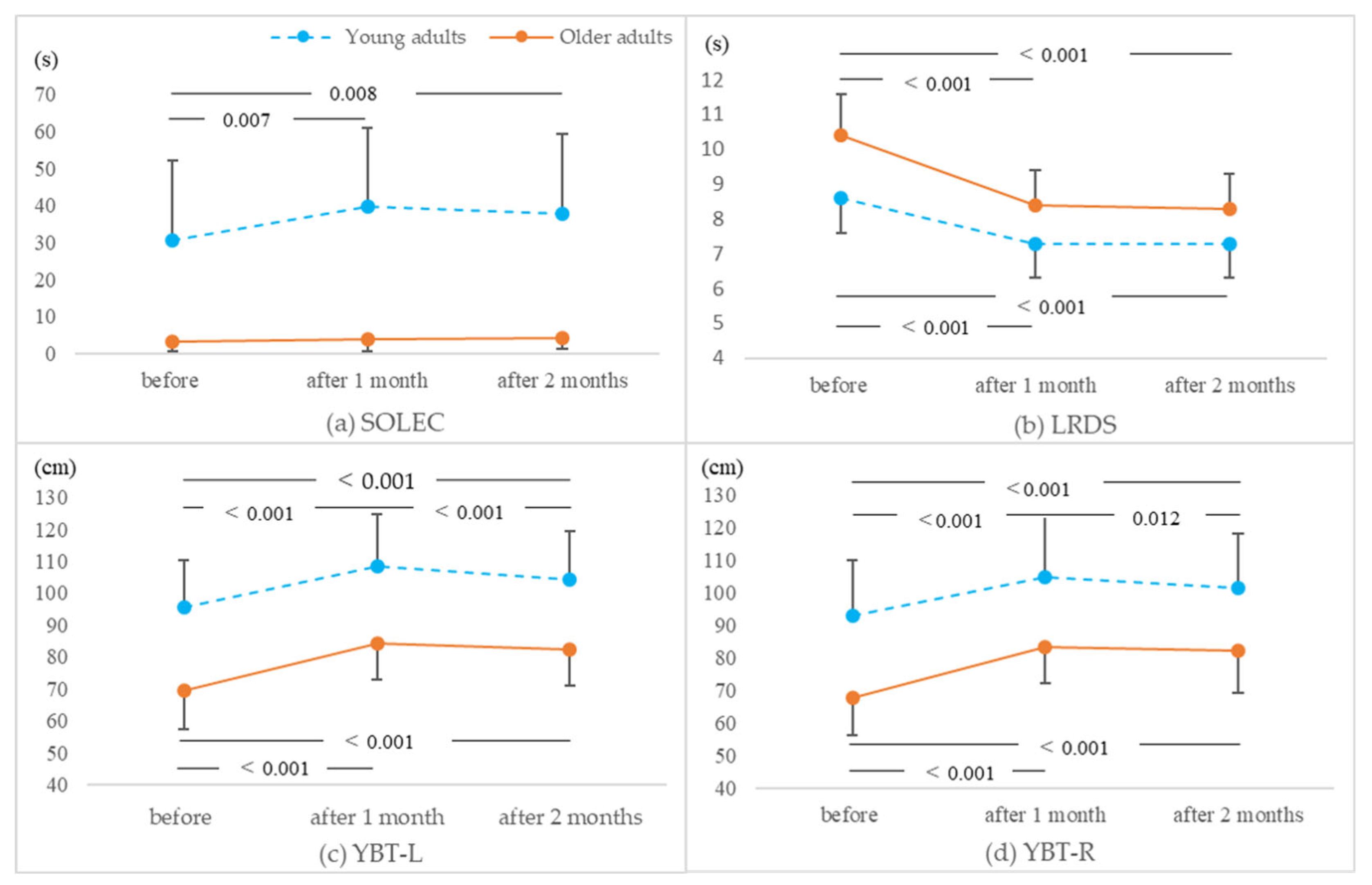
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Milanović, Z.; Pantelić, S.; Trajković, N.; Sporiš, G.; Kostić, R.; James, N. Age-related decrease in physical activity and functional fitness among elderly men and women. Clin. Interv. Aging 2013, 8, 549–556. [Google Scholar] [CrossRef]
- American Geriatrics Society; British Geriatrics Society; American Academy of Orthopaedic Surgeons Panel on Falls Prevention. Guideline for the prevention of falls in older persons. J. Am. Geriatr. Soc. 2001, 49, 664–672. [Google Scholar] [CrossRef]
- Binda, S.M.; Culham, E.G.; Brouwer, B. Balance, Muscle Strength, and Fear of Falling in Older Adults. Exp. Aging Res. 2003, 29, 205–219. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Agostini, D.; Gervasi, M.; Ferrini, F.; Bartolacci, A.; Stranieri, A.; Piccoli, G.; Barbieri, E.; Sestili, P.; Patti, A.; Stocchi, V.; et al. An Integrated Approach to Skeletal Muscle Health in Aging. Nutrients 2023, 15, 1802. [Google Scholar] [CrossRef] [PubMed]
- Chase, J.-A.D. Interventions to Increase Physical Activity Among Older Adults: A Meta-Analysis. Gerontol. 2015, 55, 706–718. [Google Scholar] [CrossRef] [PubMed]
- Suleiman-Martos, N.; García-Lara, R.; Albendín-García, L.; Romero-Béjar, J.L.; La Fuente, G.A.C.; Monsalve-Reyes, C.; Gomez-Urquiza, J.L. Effects of active video games on physical function in independent community-dwelling older adults: A systematic review and meta-analysis. J. Adv. Nurs. 2022, 78, 1228–1244. [Google Scholar] [CrossRef]
- Donath, L.; Faude, O.; Roth, R.; Zahner, L. Effects of stair-climbing on balance, gait, strength, resting heart rate, and submaximal endurance in healthy seniors. Scand. J. Med. Sci. Sports 2014, 24, e93–e101. [Google Scholar] [CrossRef]
- Yang, F.; King, G.A.; Dillon, L.; Su, X. Controlled whole-body vibration training reduces risk of falls among community-dwelling older adults. J. Biomech. 2015, 48, 3206–3212. [Google Scholar] [CrossRef]
- Hwang, P.W.; Braun, K.L. The effectiveness of dance interventions to improve older adults’ health: A systematic literature review. Altern Ther Health Med. 2015, 21, 64–70. [Google Scholar]
- Harper, S.A.; Beethe, A.Z.; Dakin, C.J.; Bolton, D.A.E. Promoting Generalized Learning in Balance Recovery Interventions. Brain Sci. 2021, 11, 402. [Google Scholar] [CrossRef]
- Lesinski, M.; Hortobágyi, T.; Muehlbauer, T.; Gollhofer, A.; Granacher, U. Effects of Balance Training on Balance Performance in Healthy Older Adults: A Systematic Review and Meta-analysis. Sports Med. 2015, 45, 1721–1738. [Google Scholar] [CrossRef] [PubMed]
- Carta, M.G.; Cossu, G.; Pintus, E.; Zaccheddu, R.; Callia, O.; Conti, G.; Pintus, M.; Gonzalez, C.I.A.; Massidda, M.V.; Mura, G.; et al. Moderate Exercise Improves Cognitive Function in Healthy Elderly People: Results of a Randomized Controlled Trial. Clin. Pract Epidemiol. Ment. Health 2021, 17, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Kerr, Z.Y.; Nedimyer, A.K.; Simon, J.E.; Kossman, M.K.; Corbett, R.O.; Chandran, A. The Epidemiology of Ankle Sprains in US High School Sports, 2011–2012 to 2018–2019 Academic Years. J. Athl. Train. 2022, 57, 1030–1038. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-I.; Mayer, F.; Wippert, P.-M. The prevalence of chronic ankle instability in basketball athletes: A cross-sectional study. BMC Sports Sci. Med. Rehabil. 2022, 14, 27. [Google Scholar] [CrossRef]
- Gribble, A.P.; Bleakley, C.M.; Caulfield, B.M.; Docherty, C.L.; Fourchet, F.; Fong, D.T.-P.; Hertel, J.; Hiller, E.C.; Kaminski, T.W.; McKeon, O.P.; et al. 2016 consensus statement of the International Ankle Consortium: Prevalence, impact and long-term consequences of lateral ankle sprains. Br. J. Sports Med. 2016, 50, 1493–1495. [Google Scholar] [CrossRef]
- Konradsen, L.; Bech, L.; Ehrenbjerg, M.; Nickelsen, T. Seven years follow-up after ankle inversion trauma. Scand. J. Med. Sci. Sports 2002, 12, 129–135. [Google Scholar] [CrossRef]
- Verhagen, E.; van der Beek, A.; Twisk, J.; Bouter, L.; Bahr, R.; van Mechelen, W. The Effect of a Proprioceptive Balance Board Training Program for the Prevention of Ankle Sprains: A prospective controlled trial. Am. J. Sports Med. 2004, 32, 1385–1393. [Google Scholar] [CrossRef]
- Jiang, C.; Huang, D.-B.; Li, X.-M.; Guo, J.-H.; Guo, M.-M.; Yu, S.-X.; Huang, S.; Lin, Z.-H. Effects of balance training on dynamic postural stability in patients with chronic ankle instability: Systematic review and meta-analysis of randomized controlled trials. J. Sports Med. Phys. Fit. 2022, 62, 1707–1715. [Google Scholar] [CrossRef]
- Mohamadi, S.; Rahmani, N.; Ebrahimi, I.; Salavati, M.; Dadgoo, M. The Effect of Leg Dominance and Group Difference in Star Excursion Balance Test between Individuals with Chronic Ankle Instability, Ankle Sprain Copers and Healthy Controls. Arch. Bone Jt. Surg. 2023, 11, 206–211. [Google Scholar] [CrossRef]
- Horak, F.B. Postural orientation and equilibrium: What do we need to know about neural control of balance to prevent falls? Age Ageing 2006, 35 (Suppl. 2), ii7–ii11. [Google Scholar] [CrossRef]
- Shao, S.; Maruyama, H. Testing the Validity of the Diamond Steps Test for Balance in Healthy Adults. Arch. Rehabil. Res. Clin. Transl. 2020, 2, 100091. [Google Scholar] [CrossRef] [PubMed]
- Akatsu, H.; Manabe, T.; Kawade, Y.; Masaki, Y.; Hoshino, S.; Jo, T.; Kobayashi, S.; Hayakawa, T.; Ohara, H. Effect of Ankle Weights as a Frailty Prevention Strategy in the Community-Dwelling Elderly: A Preliminary Report. Int. J. Environ. Res. Public Health 2022, 19, 7350. [Google Scholar] [CrossRef] [PubMed]
- Plisky, P.J.; Gorman, P.P.; Butler, R.J.; Kiesel, K.B.; Underwood, F.B.; Elkins, B. The reliability of an instrumented device for measuring components of the star excursion balance test. N Am. J. Sports Phys. Ther. 2009, 4, 92–99. [Google Scholar] [PubMed]
- Foldager, F.N.; Aslerin, S.; Bæ Kdahl, S.; Tønning, L.U.; Mechlenburg, I. Interrater, test-retest reliability of the Y balance test: A reliability study including 51 healthy participants. Int. J. Exerc. Sci. 2023, 16, 182–192. [Google Scholar] [PubMed]
- Bauer, J.; Panzer, S.; Gruber, M.; Muehlbauer, T. Associations between upper quarter Y-balance test performance and sport-related injuries in adolescent handball players. Front. Sports Act. Living 2023, 5, 1076373. [Google Scholar] [CrossRef]
- Wang, C.C.; Lo, J.; Geraghty, S.; Yang, A.W.H. Effects of Tai Chi on the quality of life, mental wellbeing, and physical function of adults with chronic diseases: Protocol for a single-blind, two-armed, randomised controlled trial. PLoS ONE 2022, 17, e0270212. [Google Scholar] [CrossRef]
- Tan, M.; Li, H.; Wang, X. Analysis of the current status of rehabilitation motivation and its influencing factors in older adults with stroke: A cross-sectional study. Front. Aging Neurosci. 2023, 15, 1186681. [Google Scholar] [CrossRef]
- Karmali, F.; Whitman, G.T.; Lewis, R.F. Bayesian optimal adaptation explains age-related human sensorimotor changes. J. Neurophysiol. 2018, 119, 509–520. [Google Scholar] [CrossRef]
- Magill, R.A.; Anderson, D.I. Motor Learning and Control: Concepts and Applications; McGraw-Hill: New York, NY, USA, 2013. [Google Scholar]
- Costello, E.; Kafchinski, M.; Vrazel, J.; Sullivan, P. Motivators, Barriers, and Beliefs Regarding Physical Activity in an Older Adult Population. J. Geriatr. Phys. Ther. 2011, 34, 138–147. [Google Scholar] [CrossRef]
- Lakicevic, N.; Gentile, A.; Mehrabi, S.; Cassar, S.; Parker, K.; Roklicer, R.; Bianco, A.; Drid, P. Make Fitness Fun: Could Novelty Be the Key Determinant for Physical Activity Adherence? Front. Psychol. 2020, 11, 577522. [Google Scholar] [CrossRef] [PubMed]
- Marcos-Pardo, P.J.; Martínez-Rodríguez, A.; Gil-Arias, A. Impact of a motivational resistance-training programme on adherence and body composition in the elderly. Sci. Rep. 2018, 8, 1370. [Google Scholar] [CrossRef] [PubMed]
- Vleugels, L.W.E.; Swinnen, S.P.; Hardwick, R.M. Skill acquisition is enhanced by reducing trial-to-trial repetition. J. Neurophysiol. 2020, 123, 1460–1471. [Google Scholar] [CrossRef] [PubMed]
- Falck, R.S.; Davis, J.C.; Best, J.R.; Crockett, R.A.; Liu-Ambrose, T. Impact of exercise training on physical and cognitive function among older adults: A systematic review and meta-analysis. Neurobiol. Aging 2019, 79, 119–130. [Google Scholar] [CrossRef]
- Sherrington, C.; Fairhall, N.J.; Wallbank, G.K.; Tiedemann, A.; Michaleff, A.Z.; Howard, K.; Clemson, L.; Hopewell, S.; Lamb, E.S. Exercise for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2019, 1, CD012424. [Google Scholar] [CrossRef]
- Hou, Z.-C.; Ao, Y.-F.; Hu, Y.-L.; Jiao, C.; Guo, Q.-W.; Li, N.; Jiang, Y.-F.; Jiang, D. Balance training benefits chronic ankle instability with generalized joint hypermobility: A prospective cohort study. BMC Musculoskelet. Disord. 2023, 24, 71. (accessed on 1 February 2018). [Google Scholar] [CrossRef]
- Singh, A.K.; Singh, M.S.; Makhija, M. Role of interventions targeting plantar cutaneous receptors in improving postural control in chronic ankle instability: A systematic review with meta-analysis. Foot 2023, 56, 102034. [Google Scholar] [CrossRef]
| Test (Units) | Young Adults | Older Adults | ||||
|---|---|---|---|---|---|---|
| Before | After 1 Month | After 2 Months | Before | After 1 Month | After 2 Months | |
| CS-30 (no. of times) | 25.5 ± 6.2 | 30.9 ± 6.3 | 30.5 ± 6.5 | 19.3 ± 6.7 | 25.2 ± 7.9 | 25.1 ± 6.7 |
| FRT (cm) | 38.8 ± 5.6 | 41.5 ± 4.7 | 40.7 ± 4.5 | 28.5 ± 5.9 | 32.5 ± 4.7 | 31.2 ± 4.9 |
| SOLEC (s) | 30.5 ± 21.6 | 39.8 ± 21.1 | 37.8 ± 21.4 | 3.2 ± 2.5 | 4.0 ± 3.3 | 4.1 ± 2.9 |
| 5-DS (s) | 23.3 ± 3.7 | 17.7 ± 2.4 | 18.0 ± 2.7 | 26.9 ± 6.5 | 20.5 ± 3.5 | 21.2 ± 3.7 |
| LRDS (s) | 8.6 ± 1.2 | 7.3 ± 1.0 | 7.3 ± 1.0 | 10.4 ± 2.3 | 8.4 ± 1.6 | 8.3 ± 1.4 |
| YBT-L (cm) | 95.6 ± 14.9 | 108.6 ± 16.3 | 104.1 ± 15.2 | 69.3 ± 11.9 | 84.2 ± 11.5 | 82.3 ± 11.4 |
| YBT-R (cm) | 92.8 ± 17.2 | 104.8 ± 18.4 | 101.5 ± 16.5 | 67.7 ± 11.3 | 83.4 ± 11.3 | 82.1 ± 12.8 |
| OCS-10 (no. of times) | 16.6 ± 2.8 | 19.4 ± 2.7 | 19.4 ± 2.7 | 13.6 ± 2.0 | 16.2 ± 2.4 | 16.1 ± 2.5 |
| FFD (cm) | 2.1 ± 9.5 | 5.3 ± 9.1 | 3.9 ± 9.3 | 5.9 ± 7.9 | 9.5 ± 7.0 | 9.0 ± 7.5 |
| Test (Units) | Age Group | Time Lapse | Age Group × Time Lapse | ||||||
|---|---|---|---|---|---|---|---|---|---|
| F-Value | p-Value | ηp2 | F-Value | p-Value | ηp2 | F-Value | p-Value | ηp2 | |
| CS-30 (no. of times) | 12.613 | 0.001 | 0.169 | 114.838 | <0.001 | 0.649 | 0.435 | 0.648 | 0.007 |
| FRT (cm) | 68.921 | <0.001 | 0.526 | 29.231 | <0.001 | 0.320 | 1.137 | 0.324 | 0.018 |
| SOLEC (s) | 76.571 | <0.001 | 0.553 | 7.677 | 0.001 | 0.110 | 5.045 | 0.008 | 0.075 |
| 5-DS (s) | 13.623 | <0.001 | 0.180 | 141.244 | <0.001 | 0.695 | 0.430 | 0.652 | 0.007 |
| LRDS (s) | 15.324 | <0.001 | 0.198 | 109.602 | <0.001 | 0.639 | 4.762 | 0.010 | 0.071 |
| YBT-L (cm) | 52.795 | <0.001 | 0.460 | 133.568 | <0.001 | 0.683 | 3.127 | 0.047 | 0.048 |
| YBT-R (cm) | 36.772 | <0.001 | 0.372 | 108.966 | <0.001 | 0.637 | 4.180 | 0.018 | 0.063 |
| OCS-10 (no. of times) | 27.560 | <0.001 | 0.308 | 125.835 | <0.001 | 0.670 | 0.234 | 0.792 | 0.004 |
| FFD (cm) | 4.333 | 0.042 | 0.065 | 62.433 | <0.001 | 0.502 | 2.373 | 0.097 | 0.037 |
| Not at All | A Little | Somewhat | Very Much | Greatly | Cramer’s V | p-Value | ||
|---|---|---|---|---|---|---|---|---|
| Young adults (n = 35) | ||||||||
| Difficulty | After | 7 (20%) | 15 (43%) | 9 (26%) | 4 (11%) | 0 (0%) | 0.236 | 0.274 |
| After 1 month | 13 (37%) | 14 (40%) | 7 (20%) | 1 (3%) | 0 (0%) | |||
| Lightness and enjoyment | After | 0 (0%) | 3 (9%) | 12 (34%) | 19 (54%) | 1 (3%) | 0.250 | 0.223 |
| After 1 month | 0 (0%) | 2 (6%) | 6 (17%) | 23 (66%) | 4 (11%) | |||
| Sense of accomplishment | After | 0 (0%) | 10 (29%) | 13 (37%) | 11 (31%) | 1 (3%) | 0.234 | 0.428 |
| After 1 month | 1 (3%) | 7 (20%) | 16 (45%) | 9 (26%) | 2 (6%) | |||
| Older adults (n = 29) | ||||||||
| Difficulty | After | 3 (10%) | 15 (52%) | 10 (35%) | 1 (3%) | 0 (0%) | 0.544 | 0.001 |
| After 1 month | 18 (62%) | 6 (21%) | 4 (14%) | 1 (3%) | 0 (0%) | |||
| Lightness and enjoyment | After | 0 (0%) | 0 (0%) | 20 (69%) | 9 (31%) | 0 (0%) | 0.278 | 0.213 |
| After 1 month | 0 (0%) | 1 (3%) | 14 (48%) | 12 (41%) | 2 (7%) | |||
| Sense of accomplishment | After | 0 (0%) | 2 (7%) | 7 (24%) | 14 (48%) | 6 (21%) | 0.153 | 0.852 |
| After 1 month | 1 (3%) | 3 (10%) | 7 (24%) | 12 (41%) | 6 (21%) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shao, S.; Mitsutake, T.; Maruyama, H. Effects of Diamond Steps Exercises on Balance Improvement in Healthy Young and Older Adults: A Protocol Proposal. Healthcare 2023, 11, 1834. https://doi.org/10.3390/healthcare11131834
Shao S, Mitsutake T, Maruyama H. Effects of Diamond Steps Exercises on Balance Improvement in Healthy Young and Older Adults: A Protocol Proposal. Healthcare. 2023; 11(13):1834. https://doi.org/10.3390/healthcare11131834
Chicago/Turabian StyleShao, Shuangyan, Tsubasa Mitsutake, and Hitoshi Maruyama. 2023. "Effects of Diamond Steps Exercises on Balance Improvement in Healthy Young and Older Adults: A Protocol Proposal" Healthcare 11, no. 13: 1834. https://doi.org/10.3390/healthcare11131834
APA StyleShao, S., Mitsutake, T., & Maruyama, H. (2023). Effects of Diamond Steps Exercises on Balance Improvement in Healthy Young and Older Adults: A Protocol Proposal. Healthcare, 11(13), 1834. https://doi.org/10.3390/healthcare11131834





