Nursing Interventions in the Perioperative Pathway of the Patient with Breast Cancer: A Scoping Review
Abstract
1. Introduction
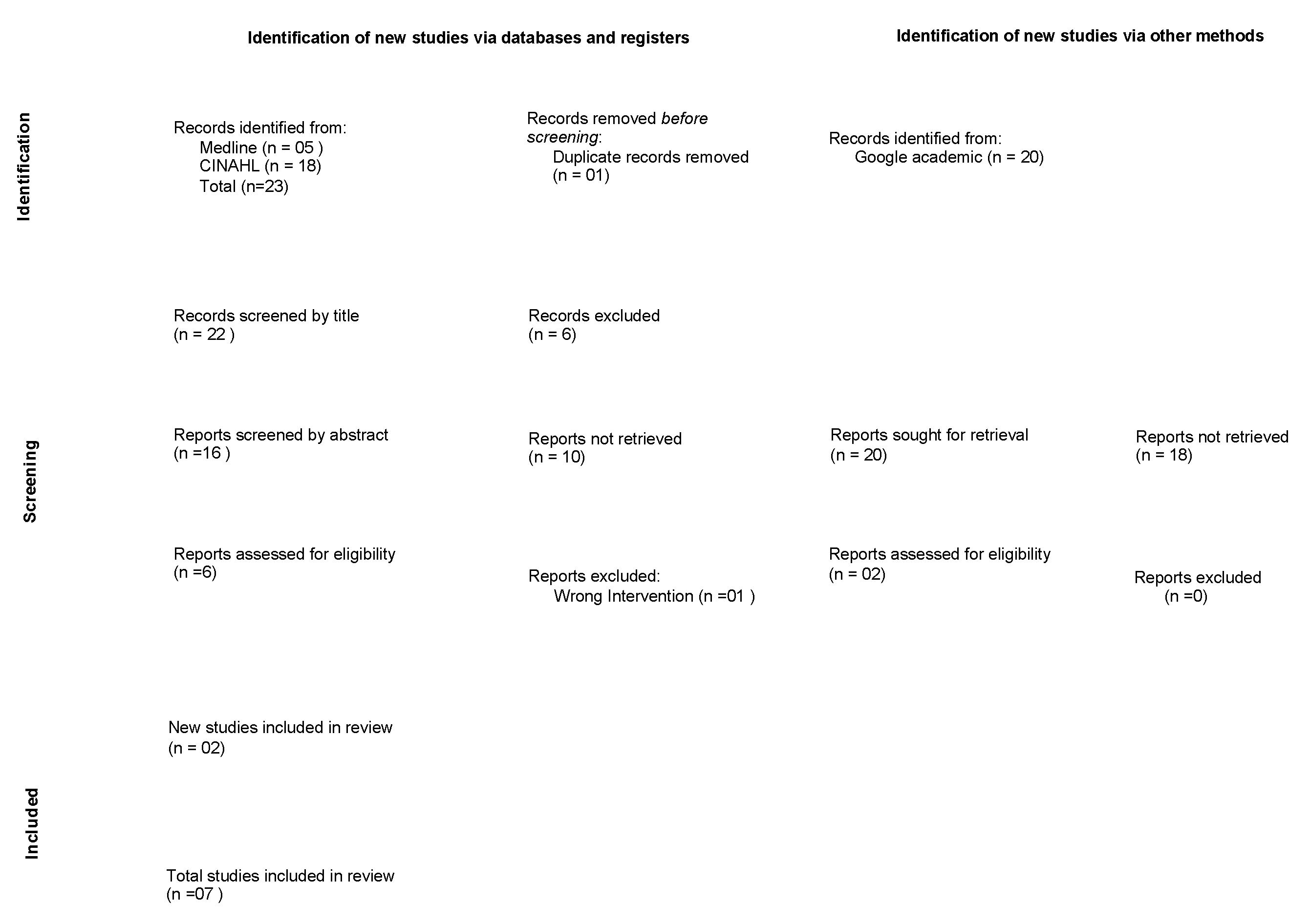
2. Materials and Methods
2.1. Study Design
2.2. Eligibility Criteria
2.3. Data Collection
2.4. Data Processing and Analysis
3. Results
3.1. Nursing Interventions throughout the Preoperative Consultation
3.2. Nursing Interventions during the Patient’s Reception in the Operating Room
3.3. Nursing Interventions troughout the Postoperative Consultation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Direção Geral da Saúde. Programa Nacional para as Doenças Oncológicas—Recursos do SNS em Oncologia—Relatório de Inquérito; Direção Geral da Saúde: Lisbon, Portugal, 2020. [Google Scholar]
- Direção Geral da Saúde. Programa Nacional para as Doenças Oncológicas; Direção Geral da Saúde: Lisbon, Portugal, 2017. [Google Scholar]
- World Health Organization. International Agency for Researcher on Cancer. Cancer Today 2022. Available online: https://gco.iarc.fr/today/online-analysis-table?v=2020&mode=cancer&mode_population=continents&population=900&populations=620&key=asr&sex=2&cancer=39&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&group_cancer=1&i (accessed on 22 February 2023).
- Alves, R.S.; Bártolo, J. Tratamento cirúrgico do carcinoma da mama. In Manual de Oncologia SPO: Abordagem e Tratamento do Cancro da Mama; Sociedade de Portuguesa de Oncologia: Lisbon, Portugal, 2020; pp. 107–126. [Google Scholar]
- Seiler, A.; Jenewein, J. Resilience in cancer patients. Front. Psychiatry 2019, 10, 208. [Google Scholar] [CrossRef] [PubMed]
- Associação dos Enfermeiros de Sala de Operações Portugueses. Enfermagem Perioperatória: Da Filosofia à Prática de Cuidados; Lusodidacta: Loures, Portugal, 2006. [Google Scholar]
- Kaptain, K.; Ulsøe, M.; Dreyer, P. Surgical perioperative pathways—Patient experiences of unmet needs show that a person-centred approach is needed. J. Clin. Nurs. 2019, 28, 2214–2224. [Google Scholar] [CrossRef] [PubMed]
- Nowak, M.; Lee, S.; Karbach, U.; Pfaff, H.; Groß, S.E. Short length of stay and the discharge process: Preparing breast cancer patients appropriately. Patient Educ. Couns. 2019, 102, 2318–2324. [Google Scholar] [CrossRef] [PubMed]
- Carli, F.; Gillis, C.; Scheede-Bergdahl, C. Promoting a culture of prehabilitation for the surgical cancer patient. Acta Oncol. 2017, 56, 128–133. [Google Scholar] [CrossRef]
- Boudreaux, A.; Simmons, J. Prehabilitation and Optimization of Modifiable Patient Risk Factors: The Importance of Effective Preoperative Evaluation to Improve Surgical Outcomes. AORN J. 2019, 109, 500–507. [Google Scholar] [CrossRef]
- Brahmbhatt, P.; Sabiston, C.M.; Lopez, C.; Chang, E.; Goodman, J.; Jones, J.; McCready, D.; Randall, I.; Rotstein, S.; Santa Mina, D. Feasibility of Prehabilitation Prior to Breast Cancer Surgery: A Mixed-Methods Study. Front. Oncol. 2020, 10, 571091. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Peters, M.D.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Wilson, D.J. Exercise for the patient after breast cancer surgery. Semin. Oncol. Nurs. 2017, 33, 98–105. [Google Scholar] [CrossRef]
- Brown, J.; Refeld, G.; Cooper, A. Timing and mode of breast care nurse consultation from the patient’s perspective. Oncol. Nurs. Forum 2018, 45, 389–398. [Google Scholar] [CrossRef]
- Nemli, A.; Kartin, P.T. Effects of exercise training and follow-up calls at home on physical activity and quality of life after a mastectomy. Jpn. J. Nurs. Sci. 2019, 16, 322–328. [Google Scholar] [CrossRef] [PubMed]
- Trescher, G.P.; Amante, L.N.; Rosa, L.M.; Balbinot Reis Girondi, J.; Severo Varela, A.I.; Oro, J.; Mancia Rolim, J.; dos Santos, M.J. Needs of women with breast cancer in the pre-operative period. J. Nurs. 2019, 13, 1288–1294. [Google Scholar] [CrossRef]
- Ghaffari, F.; Ghahramanian, A.; Zamanzadeh, V.; Onyeka, T.C.; Davoodi, A.; Mazaheri, E.; Asghari-Jafarabadi, M. Patient-centred communication for women with breast cancer: Relation to body image perception. J. Clin. Nurs. 2020, 29, 4674–4684. [Google Scholar] [CrossRef] [PubMed]
- Trescher, G.P.; Amante, L.N.; Da Rosa, L.M.; Girondi, J.B.R.; Miranda, G.M.; Santos, M.J.D.; Zuanazzi, E.C.; Mohr, H.S.S. Sistematização da consulta de enfermagem em pré-operatório às mulheres com câncer de mama. Enferm. Foco 2020, 11, 40–47. Available online: http://revista.cofen.gov.br/index.php/enfermagem/article/view/3400/1022 (accessed on 23 May 2023).
- Tola, Y.O.; Chow, K.M.; Liang, W. Effects of non-pharmacological interventions on preoperative anxiety and postoperative pain in patients undergoing breast cancer surgery: A systematic review. J. Clin. Nurs. 2021, 30, 3369–3384. [Google Scholar] [CrossRef]
- Palmer, J.B.; Lane, D.; Mayo, D.; Schluchter, M.; Leeming, R. Effects of music therapy on anesthesia requirements and anxiety in women undergoing ambulatory breast surgery for cancer diagnosis and treatment: A randomized controlled trial. J. Clin. Oncol. 2015, 33, 3162–3168. [Google Scholar] [CrossRef]
- Gonçalves, M.A.; Cerejo, M.N.; Martins, J.C. The influence of the information provided by nurses on preoperative anxiety. RER 2017, IV, 17–29. [Google Scholar] [CrossRef]
- Yeon, S.; Jeong, A.; Min, J.; Byeon, J.; Yoon, Y.J.; Heo, J.; Lee, C.; Kim, J.; Park, S.; Kim, S.I.; et al. Tearing down the barriers to exercise after mastectomy: A qualitative inquiry to facilitate exercise among breast cancer survivors. BMJ Open 2022, 12, e055157. [Google Scholar] [CrossRef]
- Carli, F.; Silver, J.K.; Feldman, L.S.; McKee, A.; Gilman, S.; Gillis, C.; Scheede-Bergdahl, C.; Gamsa, A.; Stout, N.; Hirsch, B. Surgical prehabilitation in patients with cancer: State-of-the-science and recommendations for future research from a panel of subject matter experts. Phys. Med. Rehabil. Clin. N. Am. 2017, 28, 49–64. [Google Scholar] [CrossRef]
- Fuentes-Ramírez, A.; Laverde-Contreras, O.L. Nursing intervention to meet the family members’ needs during the surgery waiting time. Rev. Lat. Am. Enferm. 2021, 29, e3483. [Google Scholar] [CrossRef]
- Kurniasih, D.A.A.; Setiawati, E.P.; Pradipta, I.S.; Subarnas, A. Patients’ Perspectives of Interprofessional Collaboration in Breast Cancer Unit. Healthcare 2023, 11, 332. [Google Scholar] [CrossRef] [PubMed]
- Fernández Fernández, E.; Fernández-Ordoñez, E.; García-Gamez, M.; Guerra-Marmolejo, C.; Iglesias-Parra, R.; Soler, N.G.; González-Cano-Caballero, M. Indicators and predictors modifiable by the nursing department during the preoperative period: A scoping review. J. Clin. Nurs. 2023, 32, 2339–2360. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.; Laza-Cagigas, R.; Pagarkar, A.; Olaoke, A.; El Gammal, M.; Rampal, T. The Feasibility of Prehabilitation as Part of the Breast Cancer Treatment Pathway. PM&R 2021, 13, 1237–1246. [Google Scholar] [CrossRef]
- Toohey, K.; Hunter, M.; McKinnon, K.; Casey, T.; Turner, M.; Taylor, S.; Paterson, C. A systematic review of multimodal prehabilitation in breast cancer. Breast Cancer Res. Treat. 2023, 197, 1–37. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, E.D.; McKenzie, M.; Schmocker, S.; Jeffs, L.; Cusimano, M.D.; Pooni, A.; Nenshi, R.; Scheer, A.S.; Forbes, T.L.; McLeod, R.S. Patient engagement study to identify and improve surgical experience. Br. J. Surg. 2021, 108, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Cruz, C.S.R.; Baixinho, C.L.; Bernardes, R.A.; Ferreira, Ó.R. Nursing Interventions for Head and Neck Cancer Patients That Promote Embracement in the Operating Room/Surgery Unit: A Near-Empty Scoping Review. Nurs. Rep. 2022, 12, 912–921. [Google Scholar] [CrossRef]
| PCC | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| P | Adult female (≥19 years) with breast cancer | Teenagers |
| C | Nursing interventions provided to the patient with breast cancer in the preoperative consultation, in the reception to the operating room, and in the postoperative consultation. | Inpatient nursing interventions. Nursing interventions in late postoperative period |
| C | Preoperative consultation, reception of the patient in the operating room, and postoperative consultation | Primary health care. Nursing homes. Rehabilitation units. |
| Search Strategy | Number Articles | |
|---|---|---|
| #1 | ((((((((((((((((adult[Title/Abstract])) OR (elderly[Title/Abstract]))) OR (older person[Title/Abstract])) OR (older people[Title/Abstract])) OR (age[Title/Abstract])) OR (aged[Title/Abstract])) OR (elder*[Title/Abstract])) OR (adult[MeSH Terms])) OR (aged[MeSH Terms])) OR (frail older adult[MeSH Terms]))) AND (woman[Title/Abstract])) NOT (adolescent[Title/Abstract]) Filters: Free full text, from 2017–2022 | 21,448 |
| #2 | ((breast cancer[Title/Abstract])) OR (breast cancer[MeSH Terms]) Filters: Free full text, from 2017–2022 | 76,142 |
| #3 | ((((((((((((((((nursing[Title/Abstract])) OR (nurs*[Title/Abstract])) OR (interv*[Title/Abstract])) OR (advanced Nurs*[Title/Abstract])) OR (educacional interventions[Title/Abstract])) OR (educat*[Title/Abstract])) OR (capacit*[Title/Abstract])) OR (nursing support[Title/Abstract])) OR (surgical nursing[Title/Abstract])) OR (advanced Nurs*[Title/Abstract])) OR (humanization[Title/Abstract])) OR (advanced practice nursing[MeSH Terms])) OR (early intervention[MeSH Terms])) OR (activities, educational[MeSH Terms])) OR (building, capacity[MeSH Terms])) Filters: Free full text, from 2017–2022 | 875,933 |
| #4 | (((((((((((((consultation[Title/Abstract]) OR (consult*[Title/Abstract])) OR (preoperative consult*[Title/Abstract])) OR (postoperative consult*[Title/Abstract])) OR (admission to the operating room[Title/Abstract])) OR (operating room[Title/Abstract])) OR (ambulatory surgery[Title/Abstract])) OR (operating room[Title/Abstract])) OR (operating theater[Title/Abstract])) OR (care, postoperative[MeSH Terms])) OR (care, preoperative[MeSH Terms])) OR (period, preoperative[MeSH Terms])) OR (ambulatory surgery[MeSH Terms])) OR (ambulatory care facilities, hospital[MeSH Terms])Filters: Free full text, from 2017–2022 | 44,718 |
| #5 | #1 AND #2 AND #3 AND #4 | 5 |
| Study/Country/Year | Study Design and Aim | Results |
|---|---|---|
| Wilson [15]. USA (2017) | Systematic review of literature To describe how mobilization stretches and exercise decrease shoulder impairments, a complication related to breast cancer surgery, thus improving quality of life. | Prevent lymphedema. Observe patient’s posture. Measure the circumference of both arms. Assess shoulder range. Measure BMI. Check exercise habits: type of exercise, duration, frequency, and intensity. Educate for exercise in the postoperative period. Reinforce the information about the exercises. Clarify doubts |
| Brown, Refeld, and Cooper [16]. Australia (2018) | Mixed descriptive study To understand what, if any, differences exist in the perception of a breast care nurse (BCN) consultation between women who experienced a preoperative, face-to-face counselling and education opportunity with a BCN and those who required a telephone consultation or were unable to experience a preoperative BCN consultation. | Offer knowledge and understanding; Psychological support, empathy; Help with practical questions, information about breast implants, supportive bras, and support groups. |
| Nemli & Kartin [17]. Turkey (2019) | Quasi-experimental study To determine the effects of exercise training that was supported with follow-up calls at home on the postoperative level of physical activity and quality of life of women with breast cancer. | Measurement of the upper limbs; Training of the exercises available in the brochure, clarifying doubts; Reinforce the importance of exercise and clarify doubts; |
| Trescher, et al. [18]. Brazil (2019) | Qualitative study To know the care needs in the preoperative period for tumour resection in the perception of women with breast cancer and nurses | Attentive listening; emotional support. Transmission of information about the patient’s pathway, clarification of doubts about therapy, and surgical preparation. Design guides and strategies for providing patient orientation. Understanding the spiritual dimension and its place in the treatment of the person. |
| Ghaffari, et al. [19]. Iran (2020) | Correlational predictive study To determine the predictive values of patient-centred communication (PCC) and patient characteristics on body image (BI) perception in postmastectomy patients. | Build a trusting relationship; Enhance the patient’s involvement in decision-making; Information exchange; Respond to emotional needs; Help manage uncertainty; Support the patient’s independence by providing appropriate resources. |
| Trescher, et al. Brazil [20]. (2020) | Methodological study Development of a model for nursing consultation in the preoperative period of women with breast cancer at an oncological outpatient. | List of nursing interventions according to the NANDA-I taxonomy; Planned activities; Expected results |
| Tola, Chow, and Liang [21]. Nigeira (2021) | Systematic review of literature To identify, analyse, and synthesise the effects of non-pharmacological interventions on preoperative anxiety and acute postoperative pain in women undergoing breast cancer surgery. | Use of music therapy to reduce pre- and postoperative anxiety; Postoperative aromatherapy in pain management; Acupuncture to reduce anxiety and pain. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cardoso, M.M.; Baixinho, C.L.; Silva, G.T.R.; Ferreira, Ó. Nursing Interventions in the Perioperative Pathway of the Patient with Breast Cancer: A Scoping Review. Healthcare 2023, 11, 1717. https://doi.org/10.3390/healthcare11121717
Cardoso MM, Baixinho CL, Silva GTR, Ferreira Ó. Nursing Interventions in the Perioperative Pathway of the Patient with Breast Cancer: A Scoping Review. Healthcare. 2023; 11(12):1717. https://doi.org/10.3390/healthcare11121717
Chicago/Turabian StyleCardoso, Mafalda Martins, Cristina Lavareda Baixinho, Gilberto Tadeu Reis Silva, and Óscar Ferreira. 2023. "Nursing Interventions in the Perioperative Pathway of the Patient with Breast Cancer: A Scoping Review" Healthcare 11, no. 12: 1717. https://doi.org/10.3390/healthcare11121717
APA StyleCardoso, M. M., Baixinho, C. L., Silva, G. T. R., & Ferreira, Ó. (2023). Nursing Interventions in the Perioperative Pathway of the Patient with Breast Cancer: A Scoping Review. Healthcare, 11(12), 1717. https://doi.org/10.3390/healthcare11121717







