Impact of the First Year of the COVID-19 Pandemic on Pediatric Emergency Department Attendance in a Tertiary Center in South Italy: An Interrupted Time-Series Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Data Source and Setting
2.2. Period Definitions
2.3. Outcomes
2.4. Statistical Analysis
3. Results
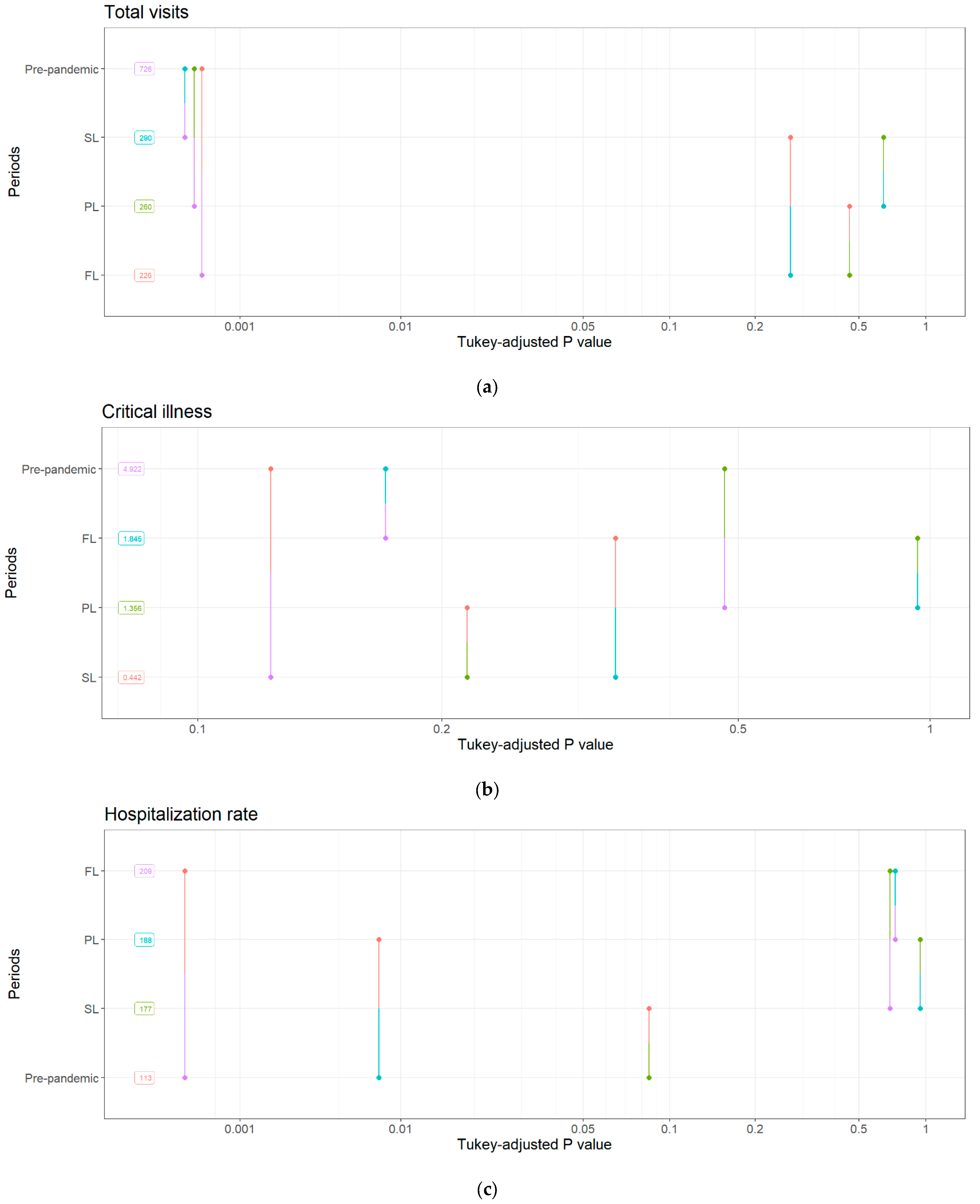
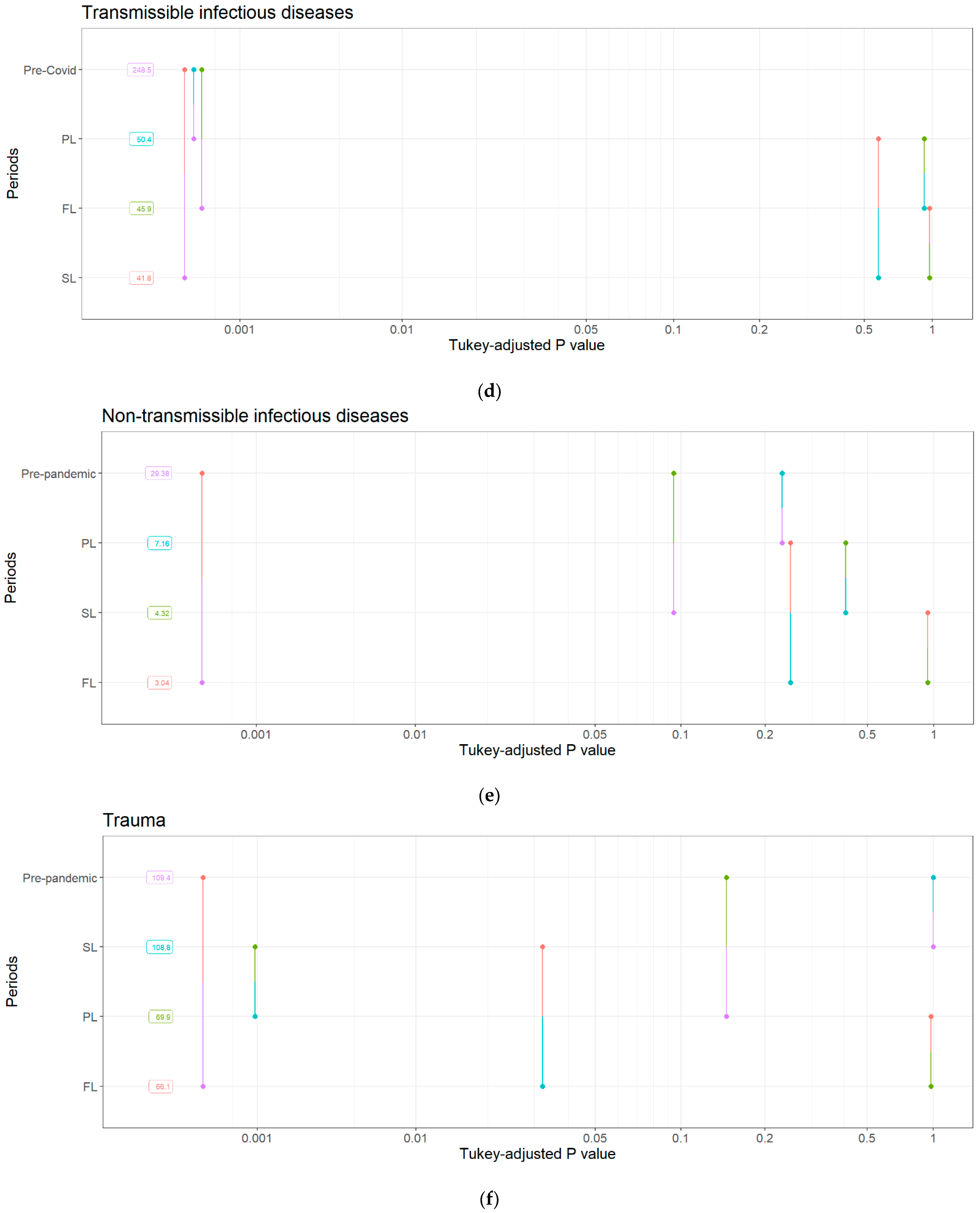
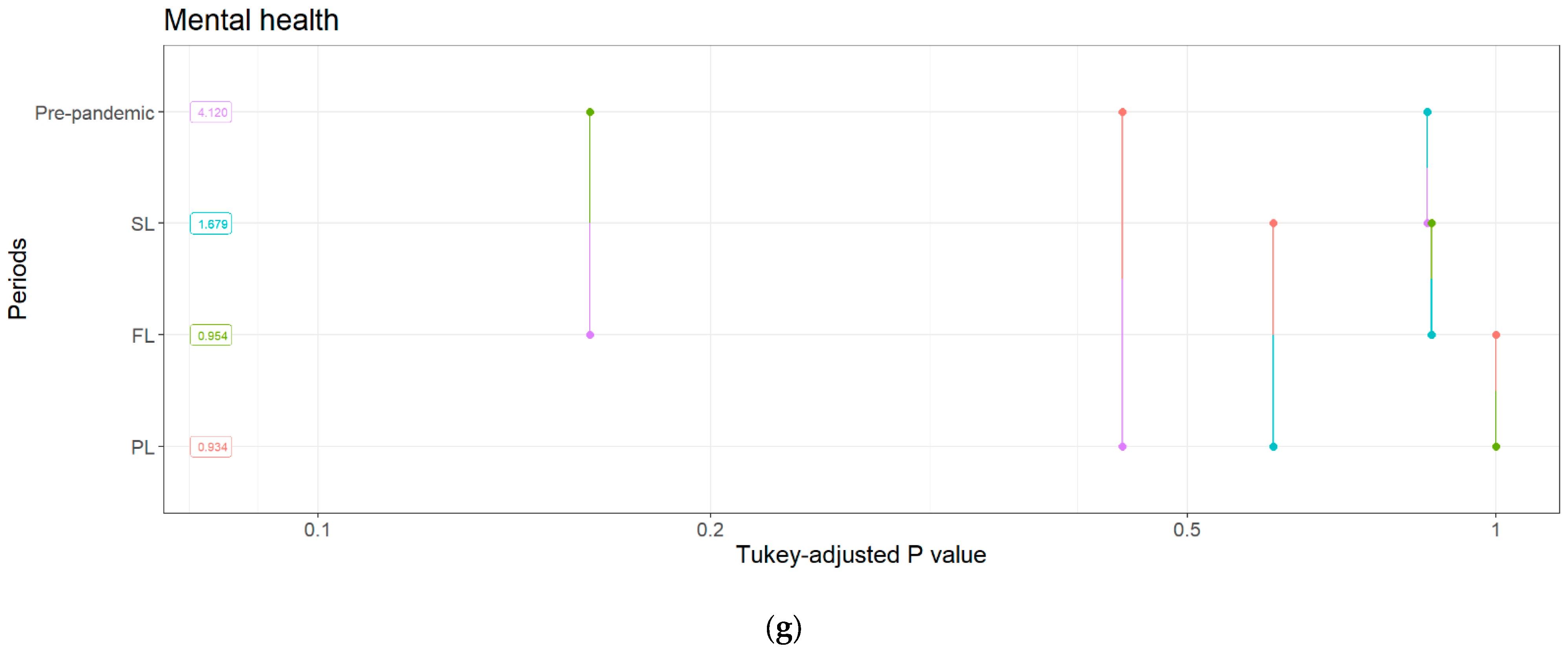
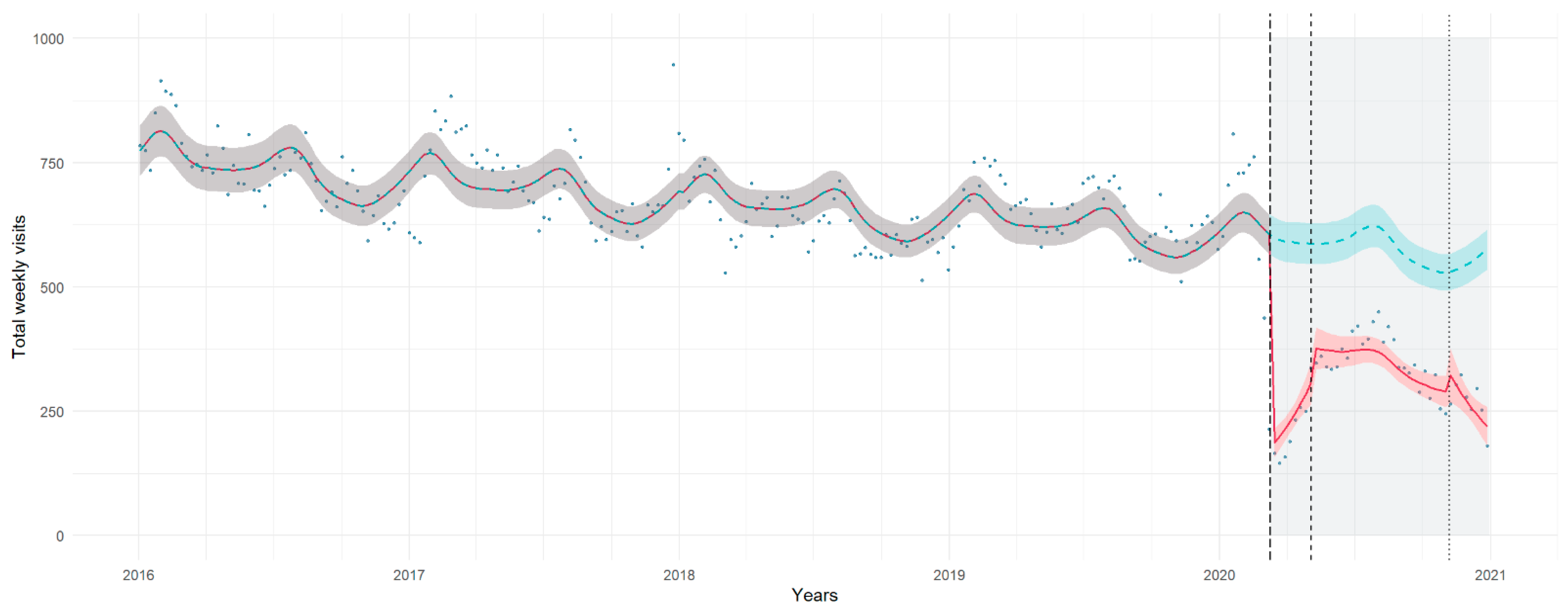
3.1. Total Visits
3.2. Critical Illness Visits
3.3. Hospitalization Rate
3.4. Cause-Specific Visits
3.4.1. Transmissible Infectious Diseases
3.4.2. Non-Transmissible Infectious Diseases
3.4.3. Trauma
3.4.4. Mental Health
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. ICD-10 Codes Used to Classify Visits in Etiological Categories
Appendix B
| Outcome | Model | Distribution | Offset | Seasonality Adjustment | Correlation Structure |
|---|---|---|---|---|---|
| Total visits | GAMM | Negative binomial | - | Spline of week (k = 52), time | AR(1) with random intercept for month |
| Critical illness | GLM | Poisson | - | Dummy variable for month | - |
| Hospitaliza-tions | GAMM | Negative binomial | Total visits | Spline of week (k = 52), time | AR(1) with random intercept for month |
| Transmissible infectious diseases | GAMM | Negative binomial | - | Spline of week (k = 52), time | AR(1) with random intercept for month |
| Non-transmissible infectious diseases | GAM | Negative binomial | - | Spline of week (k = 52), time | - |
| Trauma | GAM | Negative binomial | - | Spline of week (k = 52), time | - |
| Mental health | GLM | Zero-inflated Poisson (ZIP) | - | Dummy variable for month | - |
Appendix C
| Response Variable | Contrast | EMMs Ratio | S.E. | d.f | T Ratio | p Value |
|---|---|---|---|---|---|---|
| Total visits | (Pre-pandemic)—FL | 3.210 | 0.2652 | 246 | 14.116 | <0.001 |
| (Pre-pandemic)—PL | 2.799 | 0.3950 | 246 | 7.292 | <0.001 | |
| (Pre-pandemic)—SL | 2.508 | 0.4320 | 246 | 5.337 | <0.001 | |
| FL—PL | 0.872 | 0.0813 | 246 | −1.470 | 0.457 | |
| FL—SL | 0.781 | 0.1064 | 246 | −1.813 | 0.269 | |
| PL—SL | 0.896 | 0.0829 | 246 | −1.187 | 0.635 | |
| Critical illness | (Pre-pandemic)—FL | 2.67 | 1.278 | Inf | 2.050 | 0.169 |
| (Pre-pandemic)—PL | 3.63 | 3.264 | Inf | 1.434 | 0.477 | |
| (Pre-pandemic)—SL | 11.13 | 12.180 | Inf | 2.202 | 0.122 | |
| FL—PL | 1.36 | 0.788 | Inf | 0.531 | 0.951 | |
| FL—SL | 4.17 | 3.555 | Inf | 1.676 | 0.336 | |
| PL—SL | 3.07 | 1.779 | Inf | 1.931 | 0.215 | |
| Hospitalizations | (Pre-pandemic)—FL | 0.541 | 0.0475 | 249 | −6.999 | <0.001 |
| (Pre-pandemic)—PL | 0.603 | 0.0947 | 249 | −3.218 | 0.007 | |
| (Pre-pandemic)—SL | 0.638 | 0.1206 | 249 | −2.375 | 0.084 | |
| FL—PL | 1.115 | 0.1145 | 249 | 1.056 | 0.716 | |
| FL—SL | 1.179 | 0.1735 | 249 | 1.119 | 0.678 | |
| PL—SL | 1.058 | 0.1016 | 249 | 0.585 | 0.936 | |
| Transmissible infectious diseases | (Pre-pandemic)—FL | 5.42 | 0.709 | 245 | 12.921 | <0.001 |
| (Pre-pandemic)—PL | 4.93 | 1.093 | 7.194 | <0.001 | ||
| (Pre-pandemic)—SL | 5.95 | 1.612 | 245 | 6.583 | <0.001 | |
| FL—PL | 0.91 | 0.133 | 245 | −0.647 | 0.916 | |
| FL—SL | 1.10 | 0.235 | 245 | 0.435 | 0.972 | |
| PL—SL | 1.21 | 0.176 | 245 | 1.286 | 0.572 | |
| Non-transmissible infectious diseases | (Pre-pandemic)—FL | 9.653 | 3.910 | 246 | 5.597 | <0.001 |
| (Pre-pandemic)—PL | 4.105 | 3.051 | 246 | 1.900 | 0.230 | |
| (Pre-pandemic)—SL | 6.802 | 5.598 | 246 | 2.329 | 0.094 | |
| FL—PL | 0.425 | 0.196 | 246 | −1.860 | 0.248 | |
| FL—SL | 0.705 | 0.409 | 246 | −0.603 | 0.931 | |
| PL—SL | 1.657 | 0.537 | 246 | 1.556 | 0.405 | |
| Trauma | (Pre-pandemic)—FL | 1.656 | 0.1969 | 246 | 4.240 | <0.001 |
| (Pre-pandemic)—PL | 1.565 | 0.3282 | 246 | 2.135 | 0.144 | |
| (Pre-pandemic)—SL | 1.006 | 0.2470 | 246 | 0.025 | 1.000 | |
| FL—PL | 0.945 | 0.1211 | 246 | −0.440 | 0.971 | |
| FL—SL | 0.608 | 0.1100 | 246 | −2.751 | 0.032 | |
| PL—SL | 0.643 | 0.0742 | 246 | −3.825 | <0.001 | |
| Mental health | (Pre-pandemic)—FL | 4.321 | 3.033 | 243 | 2.085 | 0.161 |
| (Pre-pandemic)—PL | 4.411 | 4.354 | 1.504 | 0.436 | ||
| (Pre-pandemic)—SL | 2.454 | 2.736 | 0.805 | 0.852 | ||
| FL—PL | 1.021 | 0.487 | 0.043 | 1.000 | ||
| FL—SL | 0.568 | 0.401 | −0.801 | 0.853 | ||
| PL—SL | 0.556 | 0.263 | −1.242 | 0.600 |
| Age Stratum | Variables | Total Visits | Critical Illness | Hospitalization Rates | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| IRR | 95% CI | p | IRR | 95% CI | p | IRR | 95% CI | p | ||
| 0–6 years | Level | |||||||||
| FL | 0.29 | 0.25, 0.35 | <0.001 | 0.37 | 0.10, 1.02 | 0.086 | 1.84 | 1.52, 2.21 | <0.001 | |
| PL | 0.33 | 0.25, 0.46 | <0.001 | 0.31 | 0.03, 2.63 | 0.300 | 1.68 | 1.19, 2.36 | 0.003 | |
| SL | 0.36 | 0.25, 0.53 | <0.001 | 0.14 | 0.01, 1.76 | 0.130 | 1.52 | 1.01, 2.29 | 0.045 | |
| Trend | ||||||||||
| FL | 1.07 | 1.03, 1.11 | <0.001 | 1.07 | 0.83, 1.40 | 0.600 | 0.96 | 0.92, 1.00 | 0.069 | |
| PL | 0.93 | 0.89, 0.97 | <0.001 | 0.97 | 0.74, 1.26 | 0.800 | 1.05 | 1.01, 1.10 | 0.018 | |
| SL | 0.93 | 0.89, 0.98 | 0.003 | 0.84 | 0.61, 1.16 | 0.300 | 0.99 | 0.95, 1.03 | 0.600 | |
| 7–12 years | Level | |||||||||
| FL | 0.26 | 0.22, 0.32 | <0.001 | 0.56 | 0.03, 3.21 | 0.600 | 2.24 | 1.69, 2.98 | <0.001 | |
| PL | 0.32 | 0.22, 0.45 | <0.001 | 1.55 | 0.01, 910 | 0.900 | 2.14 | 1.27, 3.63 | 0.005 | |
| SL | 0.36 | 0.23, 0.55 | <0.001 | 0.48 | 0.00, 378 | 0.800 | 2.22 | 1.18, 4.18 | 0.014 | |
| Trend | ||||||||||
| FL | 1.11 | 1.06, 1.15 | <0.001 | 0.84 | 0.38, 1.53 | 0.600 | 0.91 | 0.86, 0.97 | 0.005 | |
| PL | 0.89 | 0.86, 0.94 | <0.001 | 1.25 | 0.68, 2.75 | 0.500 | 1.11 | 1.04, 1.18 | 0.001 | |
| SL | 0.95 | 0.90, 1.00 | 0.039 | 1.08 | 0.72, 1.68 | 0.700 | 1.01 | 0.95, 1.09 | 0.700 | |
| >12 years | Level | |||||||||
| FL | 0.22 | 0.17, 0.28 | <0.001 | 0.26 | 0.02, 4.22 | 0.300 | 1.8 | 1.36, 2.39 | <0.001 | |
| PL | 0.26 | 0.16, 0.42 | <0.001 | 0.05 | 0.00, 4.98 | 0.200 | 1.32 | 0.76, 2.31 | 0.300 | |
| SL | 0.34 | 0.19, 0.60 | <0.001 | 0 | 0.00, Inf | 1.000 | 1.29 | 0.66, 2.52 | 0.500 | |
| Trend | ||||||||||
| FL | 1.15 | 1.09, 1.22 | <0.001 | 1.38 | 0.80, 2.38 | 0.200 | 0.97 | 0.91, 1.04 | 0.400 | |
| PL | 0.86 | 0.81, 0.91 | <0.001 | 0.75 | 0.43, 1.32 | 0.300 | 1.04 | 0.97, 1.11 | 0.300 | |
| SL | 0.96 | 0.90, 1.02 | 0.200 | 51,626 | 0.00, Inf | 1.000 | 1.04 | 0.97, 1.11 | 0.300 | |
Appendix D
References
- Moynihan, R.; Sanders, S.; Michaleff, Z.A.; Scott, A.M.; Clark, J.; To, E.J.; Jones, M.; Kitchener, E.; Fox, M.; Johansson, M.; et al. Impact of COVID-19 Pandemic on Utilisation of Healthcare Services: A Systematic Review. BMJ Open 2021, 11, e045343. [Google Scholar] [CrossRef] [PubMed]
- Isba, R.; Edge, R.; Jenner, R.; Broughton, E.; Francis, N.; Butler, J. Where Have All the Children Gone? Decreases in Paediatric Emergency Department Attendances at the Start of the COVID-19 Pandemic of 2020. Arch. Dis. Child. 2020, 105, 704. [Google Scholar] [CrossRef] [PubMed]
- Kostopoulou, E.; Gkentzi, D.; Papasotiriou, M.; Fouzas, S.; Tagalaki, A.; Varvarigou, A.; Dimitriou, G. The Impact of COVID-19 on Paediatric Emergency Department Visits. A One-Year Retrospective Study. Pediatr. Res. 2022, 91, 1257–1262. [Google Scholar] [CrossRef] [PubMed]
- Kruizinga, M.D.; Peeters, D.; van Veen, M.; van Houten, M.; Wieringa, J.; Noordzij, J.G.; Bekhof, J.; Tramper-Stranders, G.; Vet, N.J.; Driessen, G.J.A. The Impact of Lockdown on Pediatric ED Visits and Hospital Admissions during the COVID19 Pandemic: A Multicenter Analysis and Review of the Literature. Eur. J. Pediatr. 2021, 180, 2271–2279. [Google Scholar] [CrossRef]
- Davis, A.L.; Sunderji, A.; Marneni, S.R.; Seiler, M.; Hall, J.E.; Cotanda, C.P.; Klein, E.J.; Brown, J.C.; Gelernter, R.; Griffiths, M.A.; et al. Caregiver-Reported Delay in Presentation to Pediatric Emergency Departments for Fear of Contracting COVID-19: A Multi-National Cross-Sectional Study. Can. J. Emerg. Med. 2021, 23, 778–786. [Google Scholar] [CrossRef]
- Prem, K.; Liu, Y.; Russell, T.W.; Kucharski, A.J.; Eggo, R.M.; Davies, N.; Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group; Jit, M.; Klepac, P. The Effect of Control Strategies to Reduce Social Mixing on Outcomes of the COVID-19 Epidemic in Wuhan, China: A Modelling Study. Lancet Public Health 2020, 5, e261–e270. [Google Scholar] [CrossRef]
- Rabbone, I.; Tagliaferri, F.; Carboni, E.; Crotti, B.; Ruggiero, J.; Monzani, A.; Bonetti, L.; Soliani, M.; Bellone, S.; Cavalli, C.; et al. Changing Admission Patterns in Pediatric Emergency Departments during the COVID-19 Pandemic in Italy Were Due to Reductions in Inappropriate Accesses. Children 2021, 8, 962. [Google Scholar] [CrossRef]
- Liguoro, I.; Pilotto, C.; Vergine, M.; Pusiol, A.; Vidal, E.; Cogo, P. The Impact of COVID-19 on a Tertiary Care Pediatric Emergency Department. Eur. J. Pediatr. 2021, 180, 1497–1504. [Google Scholar] [CrossRef]
- Cheng, C.-W.; Huang, Y.-B.; Chao, H.-Y.; Ng, C.-J.; Chen, S.-Y. Impact of the COVID-19 Pandemic on Pediatric Emergency Medicine: A Systematic Review. Medicina 2022, 58, 1112. [Google Scholar] [CrossRef]
- Dean, P.; Zhang, Y.; Frey, M.; Shah, A.; Edmunds, K.; Boyd, S.; Schwartz, H.; Frey, T.; Stalets, E.; Schaffzin, J.; et al. The Impact of Public Health Interventions on Critical Illness in the Pediatric Emergency Department during the SARS-CoV-2 Pandemic. J. Am. Coll. Emerg. Physicians Open 2020, 1, 1542–1551. [Google Scholar] [CrossRef]
- Nijman, R.G.; Honeyford, K.; Farrugia, R.; Rose, K.; Bognar, Z.; Buonsenso, D.; Dalt, L.D.; De, T.; Maconochie, I.K.; Parri, N.; et al. Presentations of Children to Emergency Departments across Europe and the COVID-19 Pandemic: A Multinational Observational Study. PLoS Med. 2022, 19, e1003974. [Google Scholar] [CrossRef]
- Rivera-Sepulveda, A.; Maul, T.; Dong, K.; Crate, K.; Helman, T.; Bria, C.; Martin, L.; Bogers, K.; Pearce, J.W.; Glass, T.F. Effect of the COVID-19 Pandemic on the Pediatric Emergency Department Flow. Disaster Med. Public Health Prep. 2021, 17, e83. [Google Scholar] [CrossRef]
- Mullan, P.C.; Vazifedan, T. Changing Temporal Trends in Patient Volumes in a Pediatric Emergency Department during a COVID-19 Pandemic Lockdown: A Retrospective Cohort Study. PLoS ONE 2022, 17, e0271708. [Google Scholar] [CrossRef]
- Volume and Acuity of Emergency Department Visits Prior to and after COVID-19—ScienceDirect. Available online: https://www.sciencedirect.com/science/article/pii/S0736467920308556 (accessed on 2 February 2023).
- Rotulo, G.A.; Percivale, B.; Molteni, M.; Naim, A.; Brisca, G.; Piccotti, E.; Castagnola, E. The Impact of COVID-19 Lockdown on Infectious Diseases Epidemiology: The Experience of a Tertiary Italian Pediatric Emergency Department. Am. J. Emerg. Med. 2021, 43, 115–117. [Google Scholar] [CrossRef]
- Angoulvant, F.; Ouldali, N.; Yang, D.D.; Filser, M.; Gajdos, V.; Rybak, A.; Guedj, R.; Soussan-Banini, V.; Basmaci, R.; Lefevre-Utile, A.; et al. Coronavirus Disease 2019 Pandemic: Impact Caused by School Closure and National Lockdown on Pediatric Visits and Admissions for Viral and Nonviral Infections—A Time Series Analysis. Clin. Infect. Dis. 2021, 72, 319–322. [Google Scholar] [CrossRef]
- Kuitunen, I.; Artama, M.; Haapanen, M.; Renko, M. Respiratory Virus Circulation in Children after Relaxation of COVID-19 Restrictions in Fall 2021—A Nationwide Register Study in Finland. J. Med. Virol. 2022, 94, 4528–4532. [Google Scholar] [CrossRef]
- Shi, Y.; Kvasnovsky, C.; Khan, S.; Jain, S.; Sargeant, D.; Lamoshi, A.; Prince, J.; Sathya, C. Impact of the COVID-19 Pandemic on Trauma Activations at a Pediatric Level 1 Trauma Center in New York. Pediatr. Surg. Int. 2021, 37, 1409–1414. [Google Scholar] [CrossRef]
- Raitio, A.; Ahonen, M.; Jääskelä, M.; Jalkanen, J.; Luoto, T.T.; Haara, M.; Nietosvaara, Y.; Salonen, A.; Pakkasjärvi, N.; Laaksonen, T.; et al. Reduced Number of Pediatric Orthopedic Trauma Requiring Operative Treatment during COVID-19 Restrictions: A Nationwide Cohort Study. Scand. J. Surg. 2021, 110, 254–257. [Google Scholar] [CrossRef]
- Finkelstein, Y.; Maguire, B.; Zemek, R.; Osmanlliu, E.; Kam, A.J.; Dixon, A.; Desai, N.; Sawyer, S.; Emsley, J.; Lynch, T.; et al. Effect of the COVID-19 Pandemic on Patient Volumes, Acuity, and Outcomes in Pediatric Emergency Departments: A Nationwide Study. Pediatr. Emer. Care 2021, 37, 427–434. [Google Scholar] [CrossRef]
- Sanford, E.L.; Zagory, J.; Blackwell, J.-M.; Szmuk, P.; Ryan, M.; Ambardekar, A. Changes in Pediatric Trauma during COVID-19 Stay-at-Home Epoch at a Tertiary Pediatric Hospital. J. Pediatr. Surg. 2021, 56, 918–922. [Google Scholar] [CrossRef]
- Satoskar, S.; Badaki, O.B.; Gielen, A.C.; McDonald, E.M.; Ryan, L.M. Impact of the COVID-19 Pandemic on Pediatric Emergency Department Utilization for Head Injuries. J. Investig. Med. 2022, 70, 1416–1422. [Google Scholar] [CrossRef] [PubMed]
- Masler, I.V.; Shah, N.; Duerring, S.A.; Monroe, K.R. Effects of the COVID-19 Pandemic on the Pediatric Emergency Department: A Single Institution Experience. Inj. Epidemiol. 2022, 9, 34. [Google Scholar] [CrossRef] [PubMed]
- Kuorikoski, J.; Kuitunen, I.; Uimonen, M.; Mattila, V.M.; Ponkilainen, V. Incidence of Pediatric Injury Visits Decreased While Trauma Surgeries Remained Stable during the First and Second Waves of the COVID-19 Pandemic in Finland: A Register-Based Study. World J. Pediatr. Surg. 2021, 4, e000304. [Google Scholar] [CrossRef] [PubMed]
- De Jorna, C.; Liber, M.; Khalifi, S.E.; Neggia, G.; Martinot, A.; Dubos, F. Changes in Pediatric Emergency Department Visits during a COVID-19 Lockdown Period: An Exhaustive Single-Center Analysis. Arch. Pédiatrie 2022, 29, 604–609. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Calle, D.; Andreo-Jover, J.; Curto-Ramos, J.; García Martínez, D.; Valor, L.V.; Juárez, G.; Alcamí, M.; Ortiz, A.; Iglesias, N.; Bravo-Ortiz, M.F.; et al. Pediatric Mental Health Emergency Visits During the COVID-19 Pandemic. Scand. J. Child. Adolesc. Psychiatr. Psychol. 2022, 10, 53–57. [Google Scholar] [CrossRef]
- Chadi, N.; Spinoso-Di Piano, C.; Osmanlliu, E.; Gravel, J.; Drouin, O. Mental Health–Related Emergency Department Visits in Adolescents Before and During the COVID-19 Pandemic: A Multicentric Retrospective Study. J. Adolesc. Health 2021, 69, 847–850. [Google Scholar] [CrossRef]
- Radhakrishnan, L. Pediatric Emergency Department Visits Associated with Mental Health Conditions Before and During the COVID-19 Pandemic—United States, January 2019–January 2022. Morb. Mortal. Wkly. Rep. 2022, 71, 319–324. [Google Scholar] [CrossRef]
- Leeb, R.T.; Bitsko, R.H.; Radhakrishnan, L.; Martinez, P.; Njai, R.; Holland, K.M. Mental Health–Related Emergency Department Visits Among Children Aged <18 Years During the COVID-19 Pandemic—United States, January 1–October 17, 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1675–1680. [Google Scholar] [CrossRef]
- COVID-19, Ulteriori Disposizioni Attuative Dl 6/2020, DPCM 22.03.2020: Gazzetta Ufficiale n. 76 Del 22.03.2020. Available online: http://www.regioni.it/news/2020/03/23/covid-19-ulteriori-disposizioni-attuative-dl-62020-dpcm-22-03-2020-gazzetta-ufficiale-n-76-del-22-03-2020-607770/ (accessed on 2 February 2023).
- Gazzetta Ufficiale. Available online: https://www.gazzettaufficiale.it/eli/id/2020%20/04/27/20A02352/sg (accessed on 2 February 2023).
- Giovanetti, M.; Cella, E.; Benedetti, F.; Rife Magalis, B.; Fonseca, V.; Fabris, S.; Campisi, G.; Ciccozzi, A.; Angeletti, S.; Borsetti, A.; et al. SARS-CoV-2 Shifting Transmission Dynamics and Hidden Reservoirs Potentially Limit Efficacy of Public Health Interventions in Italy. Commun. Biol. 2021, 4, 489. [Google Scholar] [CrossRef]
- Conti, S.; Ferrara, P.; Mazzaglia, G.; D’Orso, M.I.; Ciampichini, R.; Fornari, C.; Madotto, F.; Magoni, M.; Sampietro, G.; Silenzi, A.; et al. Magnitude and Time-Course of Excess Mortality during COVID-19 Outbreak: Population-Based Empirical Evidence from Highly Impacted Provinces in Northern Italy. ERJ Open Res. 2020, 6, 00458–02020. [Google Scholar] [CrossRef]
- Gazzetta Ufficiale. Available online: https://www.gazzettaufficiale.it/eli/id/2020%20/08/08/20A04399/sg (accessed on 2 February 2023).
- Manica, M.; Guzzetta, G.; Riccardo, F.; Valenti, A.; Poletti, P.; Trentini, F.; Andrianou, X.; Urdiales, A.M.; Fabiani, M.; Vescio, M.F.; et al. Effectiveness of Regional Restrictions in Reducing SARS-CoV-2 Transmission during the Second Wave of COVID-19, Italy. medRxiv 2021. [Google Scholar] [CrossRef]
- Comparisons and Contrasts in Emmeans. Available online: https://cran.r-project.org/web/packages/emmeans/vignettes/comparisons.html (accessed on 2 February 2023).
- Hartig, F.; Lohse, L. DHARMa: Residual Diagnostics for Hierarchical (Multi-Level/Mixed) Regression Models. 2022. Available online: https://CRAN.R-project.org/package=DHARMa (accessed on 8 February 2023).
- Pines, J.M.; Zocchi, M.S.; Black, B.S.; Carlson, J.N.; Celedon, P.; Moghtaderi, A.; Venkat, A. Characterizing Pediatric Emergency Department Visits during the COVID-19 Pandemic. Am. J. Emerg. Med. 2021, 41, 201–204. [Google Scholar] [CrossRef]
- Haber, N.A.; Clarke-Deelder, E.; Salomon, J.A.; Feller, A.; Stuart, E.A. Impact Evaluation of Coronavirus Disease 2019 Policy: A Guide to Common Design Issues. Am. J. Epidemiol. 2021, 190, 2474–2486. [Google Scholar] [CrossRef]
- West, S.G.; Biesanz, J.C.; Pitts, S.C. Causal Inference and Generalization in Field Settings: Experimental and Quasi-Experimental Designs. In Handbook of Research Methods in Social and Personality Psychology; Cambridge University Press: New York, NY, USA, 2000; pp. 40–84. ISBN 978-0-521-55128-1. [Google Scholar]
- Irvine, M.A.; Portales-Casamar, E.; Goldman, R.D. An Interrupted Time-Series Analysis of Pediatric Emergency Department Visits During the Coronavirus Disease 2019 Pandemic. Pediatr. Emerg. Care 2021, 37, 325. [Google Scholar] [CrossRef]
- Nicholson, E.; McDonnell, T.; Conlon, C.; Barrett, M.; Cummins, F.; Hensey, C.; McAuliffe, E. Parental Hesitancy and Concerns around Accessing Paediatric Unscheduled Healthcare during COVID-19: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2020, 17, 9264. [Google Scholar] [CrossRef]
- Islam, M.I.; Freeman, J.; Chadwick, V.; Martiniuk, A. Healthcare Avoidance before and during the COVID-19 Pandemic among Australian Youth: A Longitudinal Study. Healthcare 2022, 10, 1261. [Google Scholar] [CrossRef]
- Gerall, C.D.; DeFazio, J.R.; Kahan, A.M.; Fan, W.; Fallon, E.M.; Middlesworth, W.; Stylianos, S.; Zitsman, J.L.; Kadenhe-Chiweshe, A.V.; Spigland, N.A.; et al. Delayed Presentation and Sub-Optimal Outcomes of Pediatric Patients with Acute Appendicitis during the COVID-19 Pandemic. J. Pediatr. Surg. 2021, 56, 905–910. [Google Scholar] [CrossRef]
- Lazzerini, M.; Barbi, E.; Apicella, A.; Marchetti, F.; Cardinale, F.; Trobia, G. Delayed Access or Provision of Care in Italy Resulting from Fear of COVID-19. Lancet Child. Adolesc. Health 2020, 4, e10–e11. [Google Scholar] [CrossRef]
- Ginsburg, P.B.; Koretz, D.M. Bed Availability and Hospital Utilization: Estimates of the “Roemer Effect”. Health Care Financ. Rev. 1983, 5, 87–92. [Google Scholar]
- Moynihan, R.; Johansson, M.; Maybee, A.; Lang, E.; Légaré, F. COVID-19: An Opportunity to Reduce Unnecessary Healthcare. BMJ 2020, 370, m2752. [Google Scholar] [CrossRef]
- Vásquez-Hoyos, P.; Diaz-Rubio, F.; Monteverde-Fernandez, N.; Jaramillo-Bustamante, J.C.; Carvajal, C.; Serra, A.; Karsies, T.; Rotta, A.T.; González-Dambrauskas, S. Reduced PICU Respiratory Admissions during COVID-19. Arch. Dis. Child. 2021, 106, 808–811. [Google Scholar] [CrossRef] [PubMed]
- Todd, I.M.F.; Miller, J.E.; Rowe, S.L.; Burgner, D.P.; Sullivan, S.G. Changes in Infection-Related Hospitalizations in Children Following Pandemic Restrictions: An Interrupted Time-Series Analysis of Total Population Data. Int. J. Epidemiol. 2021, 50, dyab101. [Google Scholar] [CrossRef] [PubMed]
- Yeoh, D.K.; Foley, D.A.; Minney-Smith, C.A.; Martin, A.C.; Mace, A.O.; Sikazwe, C.T.; Le, H.; Levy, A.; Blyth, C.C.; Moore, H.C. Impact of Coronavirus Disease 2019 Public Health Measures on Detections of Influenza and Respiratory Syncytial Virus in Children During the 2020 Australian Winter. Clin. Infect. Dis. 2021, 72, 2199–2202. [Google Scholar] [CrossRef] [PubMed]
- Kishimoto, K.; Bun, S.; Shin, J.-H.; Takada, D.; Morishita, T.; Kunisawa, S.; Imanaka, Y. Early Impact of School Closure and Social Distancing for COVID-19 on the Number of Inpatients with Childhood Non-COVID-19 Acute Infections in Japan. Eur. J. Pediatr. 2021, 180, 2871–2878. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.; Fries, A.C.; DeMarcus, L.S.; Thervil, J.W.; Kwaah, B.; Brown, K.N.; Sjoberg, P.A.; Robbins, A.S. Circulating Trends of Influenza and Other Seasonal Respiratory Viruses among the US Department of Defense Personnel in the United States: Impact of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 5942. [Google Scholar] [CrossRef]
- Pelletier, J.H.; Rakkar, J.; Au, A.K.; Fuhrman, D.; Clark, R.S.B.; Horvat, C.M. Trends in US Pediatric Hospital Admissions in 2020 Compared with the Decade Before the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e2037227. [Google Scholar] [CrossRef]
- Matera, L.; Nenna, R.; Ardenti Morini, F.; Banderali, G.; Calvani, M.; Calvi, M.; Cozzi, G.; Falsaperla, R.; Guidi, R.; Kantar, A.; et al. Effects of Relaxed Lockdown on Pediatric ER Visits during SARS-CoV-2 Pandemic in Italy. Int. J. Environ. Res. Public Health 2021, 18, 9547. [Google Scholar] [CrossRef]
- Maglione, M.; Pascarella, A.; Botti, C.; Ricci, G.; Morelli, F.; Camelia, F.; Micillo, A.; Calì, C.; Savoia, F.; Tipo, V.; et al. Changing Epidemiology of Acute Viral Respiratory Infections in Hospitalized Children: The Post-Lockdown Effect. Children 2022, 9, 1242. [Google Scholar] [CrossRef]
- Billard, M.-N.; van de Ven, P.M.; Baraldi, B.; Kragten-Tabatabaie, L.; Bont, L.J.; Wildenbeest, J.G. International Changes in Respiratory Syncytial Virus (RSV) Epidemiology during the COVID-19 Pandemic: Association with School Closures. Influenza Other Respir. Viruses 2022, 16, 926–936. [Google Scholar] [CrossRef]
- Risk of Severe Pressure on Healthcare Systems Due to RSV, Flu and COVID-19 Co-Circulation. Available online: https://www.ecdc.europa.eu/en/news-events/risk-severe-pressure-healthcare-systems-due-rsv-flu-and-covid-19-co-circulation (accessed on 2 February 2023).
- Nuñez, J.H.; Sallent, A.; Lakhani, K.; Guerra-Farfan, E.; Vidal, N.; Ekhtiari, S.; Minguell, J. Impact of the COVID-19 Pandemic on an Emergency Traumatology Service: Experience at a Tertiary Trauma Centre in Spain. Injury 2020, 51, 1414–1418. [Google Scholar] [CrossRef]
- Ruzzini, L.; De Salvatore, S.; Lamberti, D.; Maglione, P.; Piergentili, I.; Crea, F.; Ossella, C.; Costici, P.F. COVID-19 Changed the Incidence and the Pattern of Pediatric Traumas: A Single-Centre Study in a Pediatric Emergency Department. Int. J. Environ. Res. Public Health 2021, 18, 6573. [Google Scholar] [CrossRef]
- Samji, H.; Wu, J.; Ladak, A.; Vossen, C.; Stewart, E.; Dove, N.; Long, D.; Snell, G. Review: Mental Health Impacts of the COVID-19 Pandemic on Children and Youth—A Systematic Review. Child Adolesc. Ment. Health 2022, 27, 173–189. [Google Scholar] [CrossRef]
- Sheridan, D.C.; Cloutier, R.; Johnson, K.; Marshall, R. Where Have All the Emergency Paediatric Mental Health Patients Gone during COVID-19? Acta Paediatr. 2021, 110, 598–599. [Google Scholar] [CrossRef]
- Hu, N.; Nassar, N.; Shrapnel, J.; Perkes, I.; Hodgins, M.; O’Leary, F.; Trudgett, C.; Eapen, V.; Woolfenden, S.; Knight, K.; et al. The Impact of the COVID-19 Pandemic on Paediatric Health Service Use within One Year after the First Pandemic Outbreak in New South Wales Australia—A Time Series Analysis. Lancet Reg. Health—West. Pac. 2022, 19, 100311. [Google Scholar] [CrossRef]
- Shankar, L.G.; Habich, M.; Rosenman, M.; Arzu, J.; Lales, G.; Hoffmann, J.A. Mental Health Emergency Department Visits by Children Before and During the COVID-19 Pandemic. Acad. Pediatr. 2022, 22, 1127–1132. [Google Scholar] [CrossRef]
- Dror, C.; Hertz-Palmor, N.; Yadan-Barzilai, Y.; Saker, T.; Kritchmann-Lupo, M.; Bloch, Y. Increase in Referrals of Children and Adolescents to the Psychiatric Emergency Room Is Evident Only in the Second Year of the COVID-19 Pandemic—Evaluating 9156 Visits from 2010 through 2021 in a Single Psychiatric Emergency Room. Int. J. Environ. Res. Public Health 2022, 19, 8924. [Google Scholar] [CrossRef]
- Sokoloff, W.C.; Krief, W.I.; Giusto, K.A.; Mohaimin, T.; Murphy-Hockett, C.; Rocker, J.; Williamson, K.A. Pediatric Emergency Department Utilization during the COVID-19 Pandemic in New York City. Am. J. Emerg. Med. 2021, 45, 100–104. [Google Scholar] [CrossRef]
- Bortoletto, R.; Di Gennaro, G.; Antolini, G.; Mondini, F.; Passarella, L.; Rizzo, V.; Silvestri, M.; Darra, F.; Zoccante, L.; Colizzi, M. Sociodemographic and Clinical Changes in Pediatric In-Patient Admissions for Mental Health Emergencies during the COVID-19 Pandemic: March 2020 to June 2021. Psychiatry Res. Commun. 2022, 2, 100023. [Google Scholar] [CrossRef]
- Yard, E.; Radhakrishnan, L.; Ballesteros, M.F.; Sheppard, M.; Gates, A.; Stein, Z.; Hartnett, K.; Kite-Powell, A.; Rodgers, L.; Adjemian, J.; et al. Emergency Department Visits for Suspected Suicide Attempts Among Persons Aged 12-25 Years Before and During the COVID-19 Pandemic—United States, January 2019–May 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 888–894. [Google Scholar] [CrossRef]
- Copeland, J.N.; Babyak, M.; Inscoe, A.B.; Maslow, G.R. Seasonality of Pediatric Mental Health Emergency Department Visits, School, and COVID-19. Pediatr. Emer. Care 2022, 38, e1673–e1677. [Google Scholar] [CrossRef]
- Suicide during COVID-19: Myths, Realities and Lessons Learned|UBC Medical Journal. Available online: https://ojs.library.ubc.ca/index.php/ubcmj/article/view/195378 (accessed on 2 February 2023).
- Kahil, K.; Cheaito, M.A.; El Hayek, R.; Nofal, M.; El Halabi, S.; Kudva, K.G.; Pereira-Sanchez, V.; El Hayek, S. Suicide during COVID-19 and Other Major International Respiratory Outbreaks: A Systematic Review. Asian J. Psychiatry 2021, 56, 102509. [Google Scholar] [CrossRef] [PubMed]
- Amodio, E.; Battisti, M.; Maida, C.M.; Zarcone, M.; Casuccio, A.; Vitale, F. Socio-Demographic Factors Involved in a Low-Incidence Phase of SARS-CoV-2 Spread in Sicily, Italy. Healthcare 2021, 9, 867. [Google Scholar] [CrossRef] [PubMed]




| Variable | Pandemic Period, N = 13,180 | Pre-Pandemic Period, N = 112,701 | p-Value |
|---|---|---|---|
| Total visits | 337 (279–389) 1 | 668 (620–722) 1 | <0.001 2 |
| Triage code | <0.001 3 | ||
| Non urgent (white code) | 101 (0.8%) | 881 (0.8%) | |
| Low acuity (green code) | 9201 (70%) | 78,231 (73%) | |
| High acuity (yellow code) | 3765 (29%) | 27,020 (25%) | |
| Dead on arrival (black code) | 0 (0%) | 23 (<0.1%) | |
| Critical illness visits (red code) | 113 (0.9%) | 649 (0.6%) | <0.001 4 |
| Hospitalizations | 3769 (29%) | 22,502 (20%) | <0.001 4 |
| Transmissible infectious diseases | 2759 (21%) | 39,008 (35%) | <0.001 4 |
| Non-transmissible infectious diseases | 330 (2.5%) | 4425 (3.9%) | <0.001 4 |
| Trauma | 3112 (24%) | 15,961 (14%) | <0.001 4 |
| Mental health | 115 (0.9%) | 610 (0.5%) | <0.001 4 |
| ICU admissions | 33 (0.3%) | 168 (0.1%) | 0.006 4 |
| Age (yrs.) | 5.0 (2.0–10.0) 1 | 5.0 (2.0–9.0) 1 | <0.001 1 |
| Age (strata) | <0.001 4 | ||
| 0–6 | 7583 (58%) | 67,573 (60%) | |
| 7–12 | 4150 (31%) | 34,441 (31%) | |
| >12 | 1447 (11%) | 10,687 (9.5%) | |
| Comorbidity | 122 (0.9%) | 1528 (1.4%) | <0.001 3 |
| Characteristic | Pandemic Period, N = 113 | Pre-Pandemic Period, N = 647 | p-Value |
|---|---|---|---|
| Age | 4.0 (2.0–8.0) 1 | 4.0 (2.0–8.0) 1 | 0.600 2 |
| Comorbidity | 1 (0.9%) | 18 (2.8%) | 0.300 3 |
| Visit outcome | |||
| Proposed admission | 93 (82%) | 512 (79%) | 0.500 3 |
| Refused admission | 5 (4.4%) | 23 (3.6%) | 0.600 3 |
| Refused brief intensive observation | 6 (5.3%) | 17 (2.6%) | 0.140 3 |
| Deceased | 1 (0.9%) | 2 (0.3%) | 0.400 3 |
| ICU admission | 13 (12%) | 75 (12%) | 0.999 3 |
| Etiology | |||
| Transmissible infectious diseases | 23 (20%) | 188 (29%) | 0.068 3 |
| Non-transmissible infectious diseases | 0 (0%) | 2 (0.3%) | 0.999 3 |
| Trauma | 11 (9.7%) | 76 (12%) | 0.600 3 |
| Mental health | 0 (0%) | 3 (0.5%) | 0.999 3 |
| Neurologic diseases | 38 (34%) | 163 (25%) | 0.065 3 |
| Variable | IRR | 95% CI | p-Value |
|---|---|---|---|
| Level | |||
| FL | 0.31 | 0.27, 0.37 | <0.001 |
| PL | 0.36 | 0.27, 0.48 | <0.001 |
| SL | 0.40 | 0.29, 0.57 | <0.001 |
| Trend | |||
| FL | 1.07 | 1.04, 1.11 | <0.001 |
| PL | 0.92 | 0.89, 0.96 | <0.001 |
| SL | 0.94 | 0.90, 0.98 | 0.006 |
| s (week) | <0.001 | ||
| s (time) | <0.001 |
| Variable | IRR | 95% CI | p-Value |
|---|---|---|---|
| Level | |||
| FL | 0.37 | 0.13, 0.88 | 0.040 |
| PL | 0.28 | 0.05, 1.62 | 0.200 |
| SL | 0.09 | 0.01, 0.74 | 0.027 |
| Trend | |||
| FL | 1.08 | 0.87, 1.34 | 0.500 |
| PL | 0.96 | 0.77, 1.19 | 0.700 |
| SL | 0.95 | 0.75, 1.22 | 0.700 |
| Month | |||
| January | — | — | — |
| February | 1.26 | 0.98, 1.62 | 0.068 |
| March | 0.89 | 0.68, 1.17 | 0.400 |
| April | 0.78 | 0.59, 1.04 | 0.094 |
| May | 0.76 | 0.56, 1.01 | 0.062 |
| June | 0.68 | 0.50, 0.92 | 0.012 |
| July | 0.67 | 0.50, 0.89 | 0.006 |
| August | 0.78 | 0.59, 1.04 | 0.093 |
| September | 0.75 | 0.56, 0.99 | 0.042 |
| October | 0.61 | 0.45, 0.82 | 0.001 |
| November | 0.65 | 0.47, 0.88 | 0.006 |
| December | 0.90 | 0.68, 1.18 | 0.400 |
| Transmissible Infectious Disease | Non-Transmissible Infectious Disease | Trauma | Mental Health | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Level | IRR | 95% CI | p | IRR | 95% CI | p | IRR | 95% CI | p | IRR | 95% CI | p |
| FL | 0.18 | 0.14, 0.24 | <0.001 | 0.1 | 0.04, 0.25 | <0.001 | 0.6 | 0.48, 0.76 | <0.001 | 0.23 | 0.06, 0.92 | 0.037 |
| PL | 0.2 | 0.13, 0.31 | <0.001 | 0.24 | 0.06, 1.04 | 0.056 | 0.64 | 0.42, 0.96 | 0.033 | 0.23 | 0.03, 1.57 | 0.130 |
| SL | 0.17 | 0.10, 0.29 | <0.001 | 0.15 | 0.03, 0.79 | 0.025 | 0.99 | 0.61, 1.60 | >0.9 | 0.41 | 0.05, 3.63 | 0.400 |
| Trend | ||||||||||||
| FL | 1.05 | 0.99, 1.11 | 0.081 | 1.07 | 0.90, 1.28 | 0.400 | 1.08 | 1.03, 1.14 | 0.002 | 1.17 | 0.92, 1.48 | 0.200 |
| PL | 0.97 | 0.91, 1.02 | 0.200 | 0.94 | 0.78, 1.12 | 0.500 | 0.91 | 0.86, 0.96 | <0.001 | 0.85 | 0.67, 1.08 | 0.200 |
| SL | 0.91 | 0.85, 0.97 | 0.006 | 0.97 | 0.84, 1.11 | 0.600 | 0.96 | 0.92, 1.01 | 0.150 | 0.95 | 0.80, 1.14 | 0.600 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alongi, A.; D’Aiuto, F.; Montomoli, C.; Borrelli, P. Impact of the First Year of the COVID-19 Pandemic on Pediatric Emergency Department Attendance in a Tertiary Center in South Italy: An Interrupted Time-Series Analysis. Healthcare 2023, 11, 1638. https://doi.org/10.3390/healthcare11111638
Alongi A, D’Aiuto F, Montomoli C, Borrelli P. Impact of the First Year of the COVID-19 Pandemic on Pediatric Emergency Department Attendance in a Tertiary Center in South Italy: An Interrupted Time-Series Analysis. Healthcare. 2023; 11(11):1638. https://doi.org/10.3390/healthcare11111638
Chicago/Turabian StyleAlongi, Alessandra, Francesca D’Aiuto, Cristina Montomoli, and Paola Borrelli. 2023. "Impact of the First Year of the COVID-19 Pandemic on Pediatric Emergency Department Attendance in a Tertiary Center in South Italy: An Interrupted Time-Series Analysis" Healthcare 11, no. 11: 1638. https://doi.org/10.3390/healthcare11111638
APA StyleAlongi, A., D’Aiuto, F., Montomoli, C., & Borrelli, P. (2023). Impact of the First Year of the COVID-19 Pandemic on Pediatric Emergency Department Attendance in a Tertiary Center in South Italy: An Interrupted Time-Series Analysis. Healthcare, 11(11), 1638. https://doi.org/10.3390/healthcare11111638








