Locating Medical Information during an Infodemic: Information Seeking Behavior and Strategies of Health-Care Workers in Germany
Abstract
:1. Introduction
2. Materials and Methods
2.1. Surveys
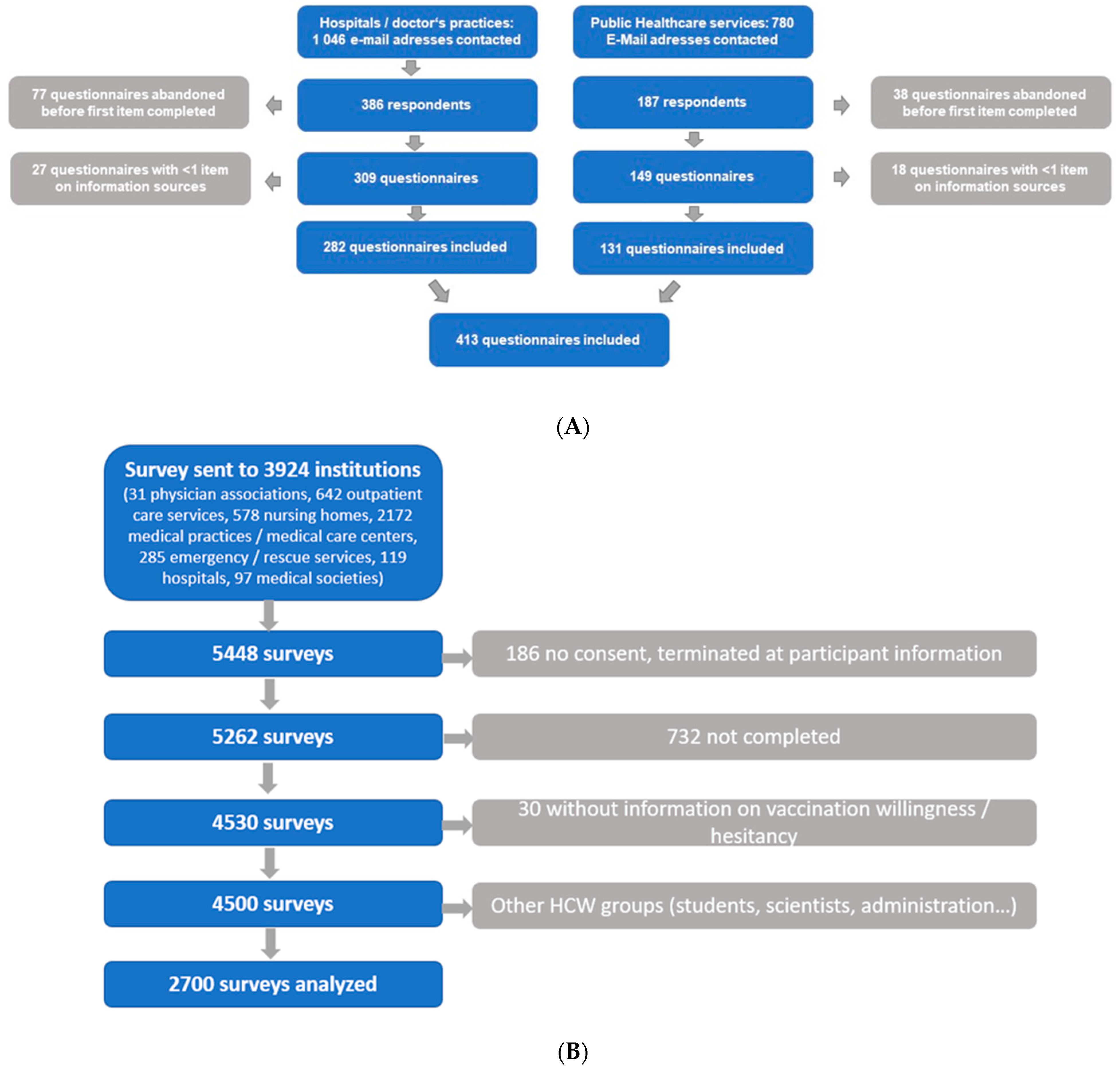
2.1.1. COVID-19 Informational Needs and Strategies Study (Study 1)
Survey Participants (Study 1)
Questionnaire (Study 1)
2.1.2. COVID-19 Vaccination Acceptance and Hesitance Study (Study 2)
Participants
Questionnaire
2.2. Ethics and Data Protection
2.3. Statistics
3. Results
3.1. Participants
3.2. COVID-19 Information Needs and Strategies Study (Study 1)
3.2.1. Information Channels
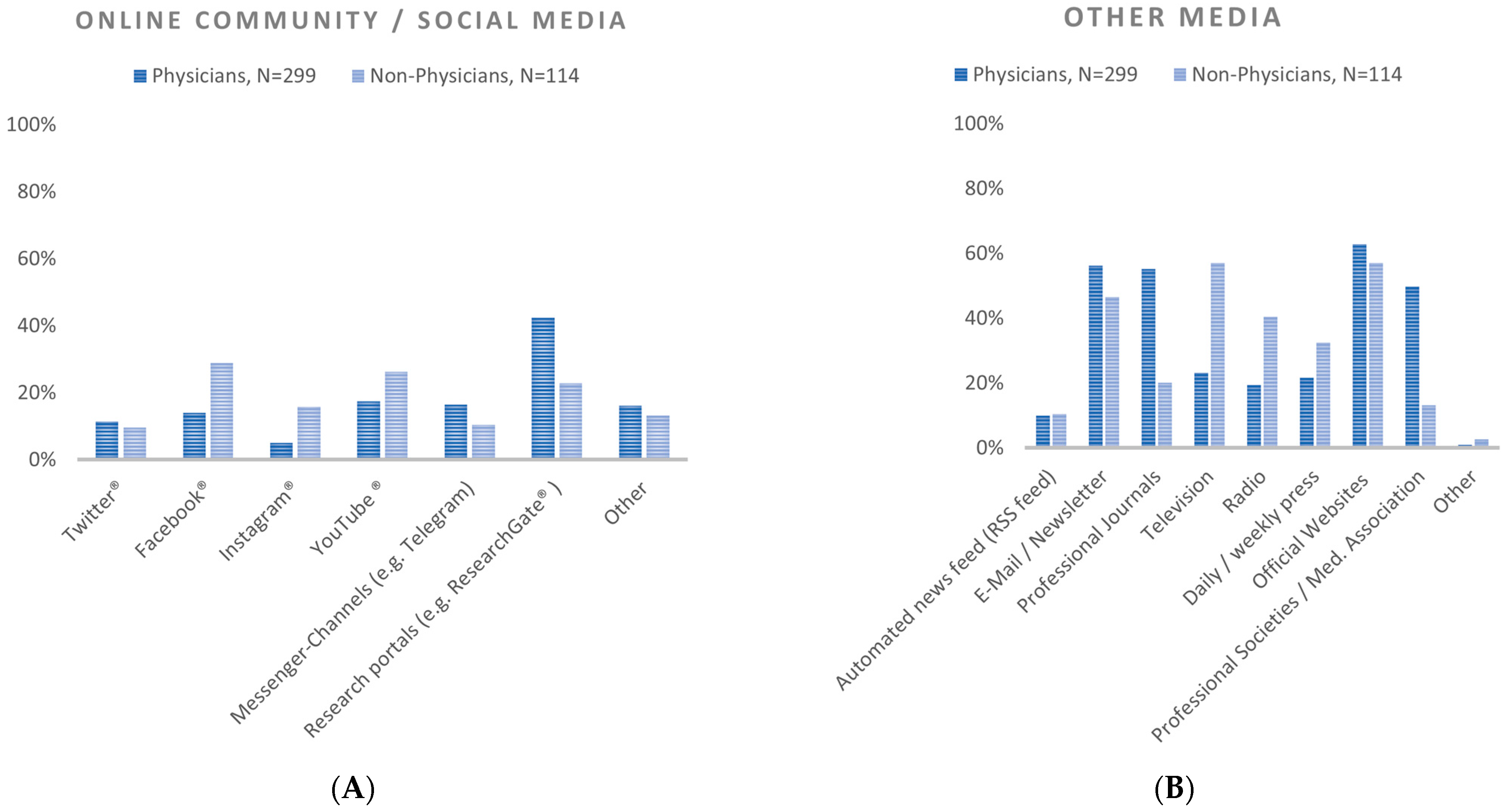
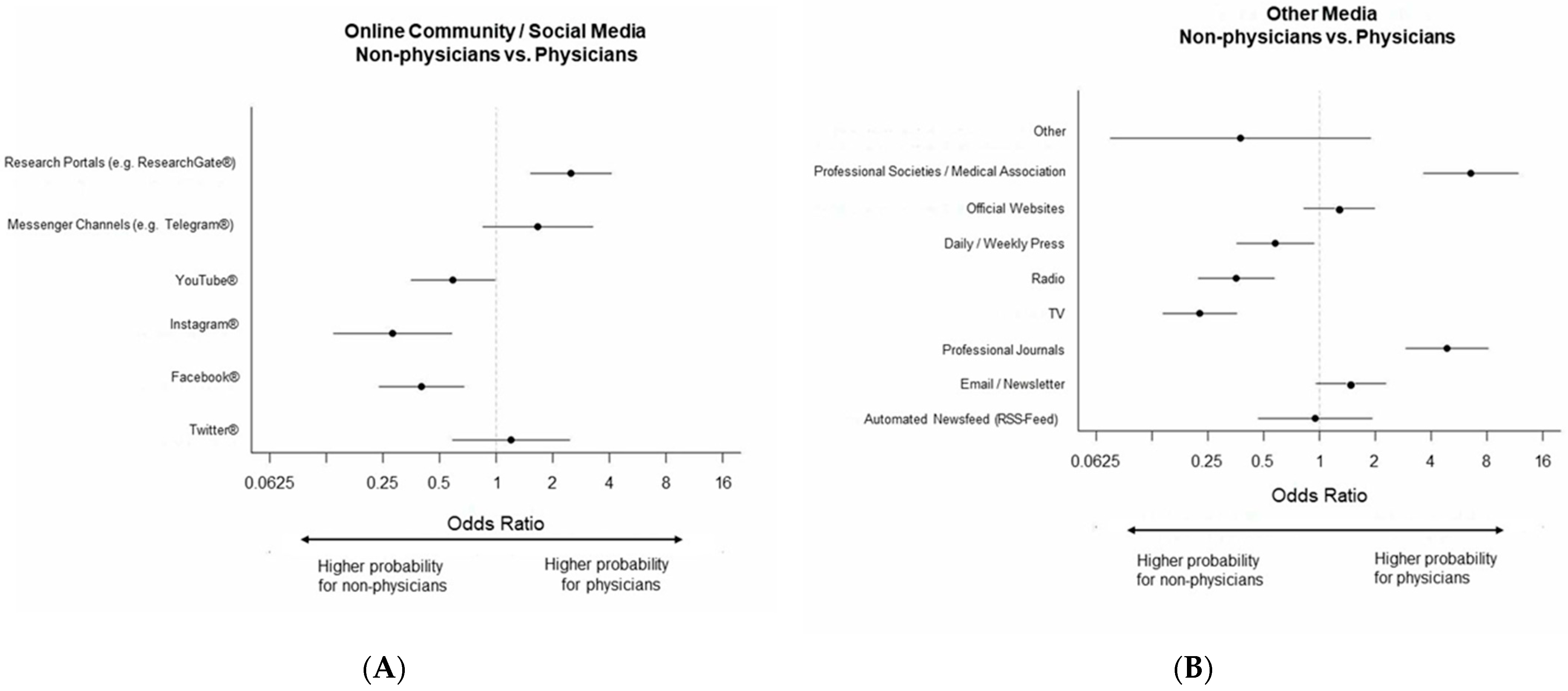
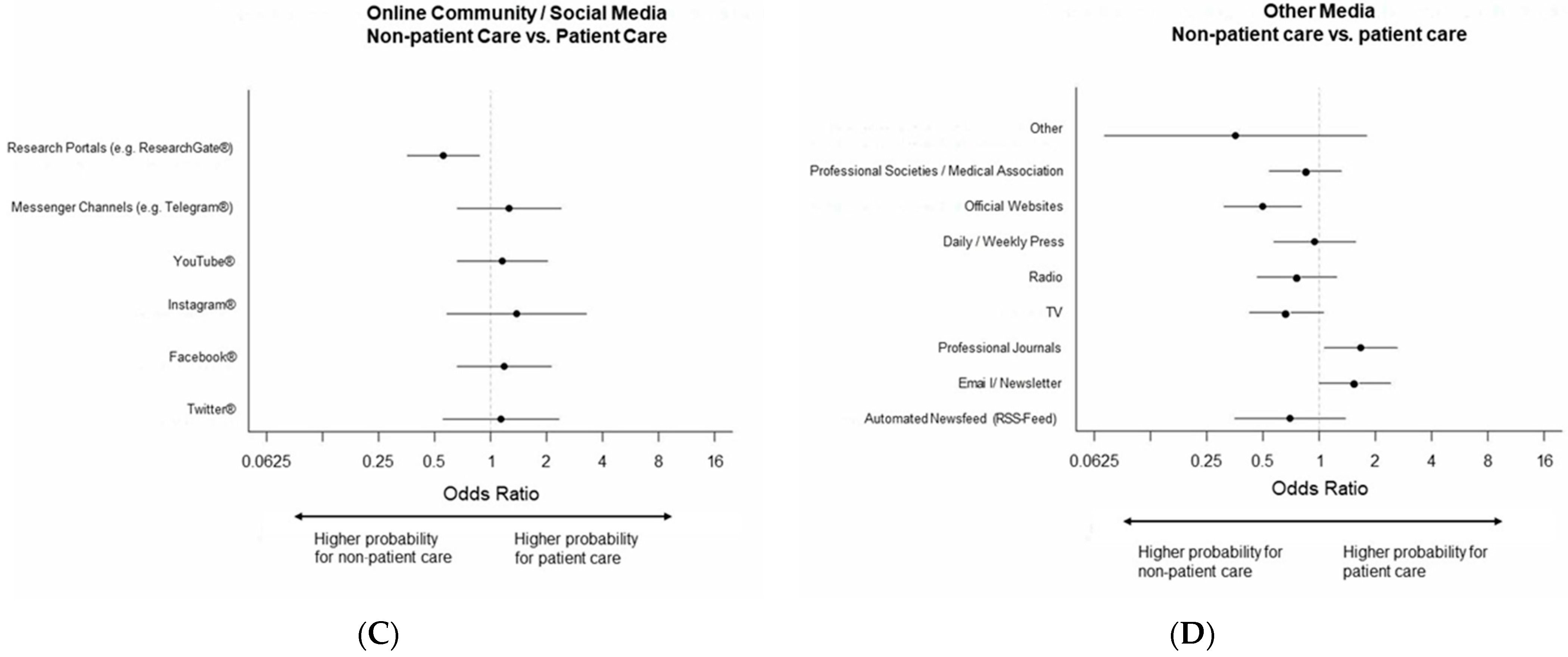
Social Media
Other Media
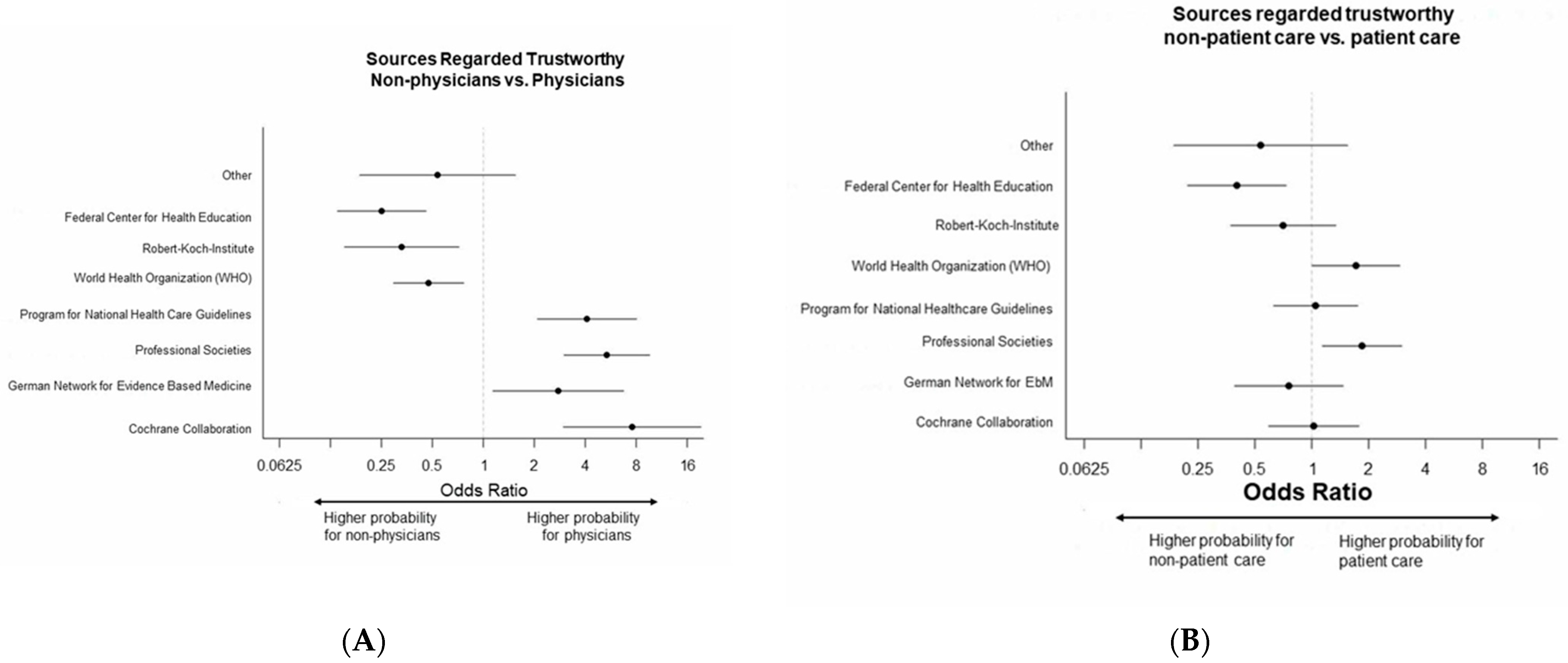
3.2.2. Information Sources Regarded as Trustworthy
3.2.3. Barriers to Using Evidence Syntheses
3.2.4. Information Formats
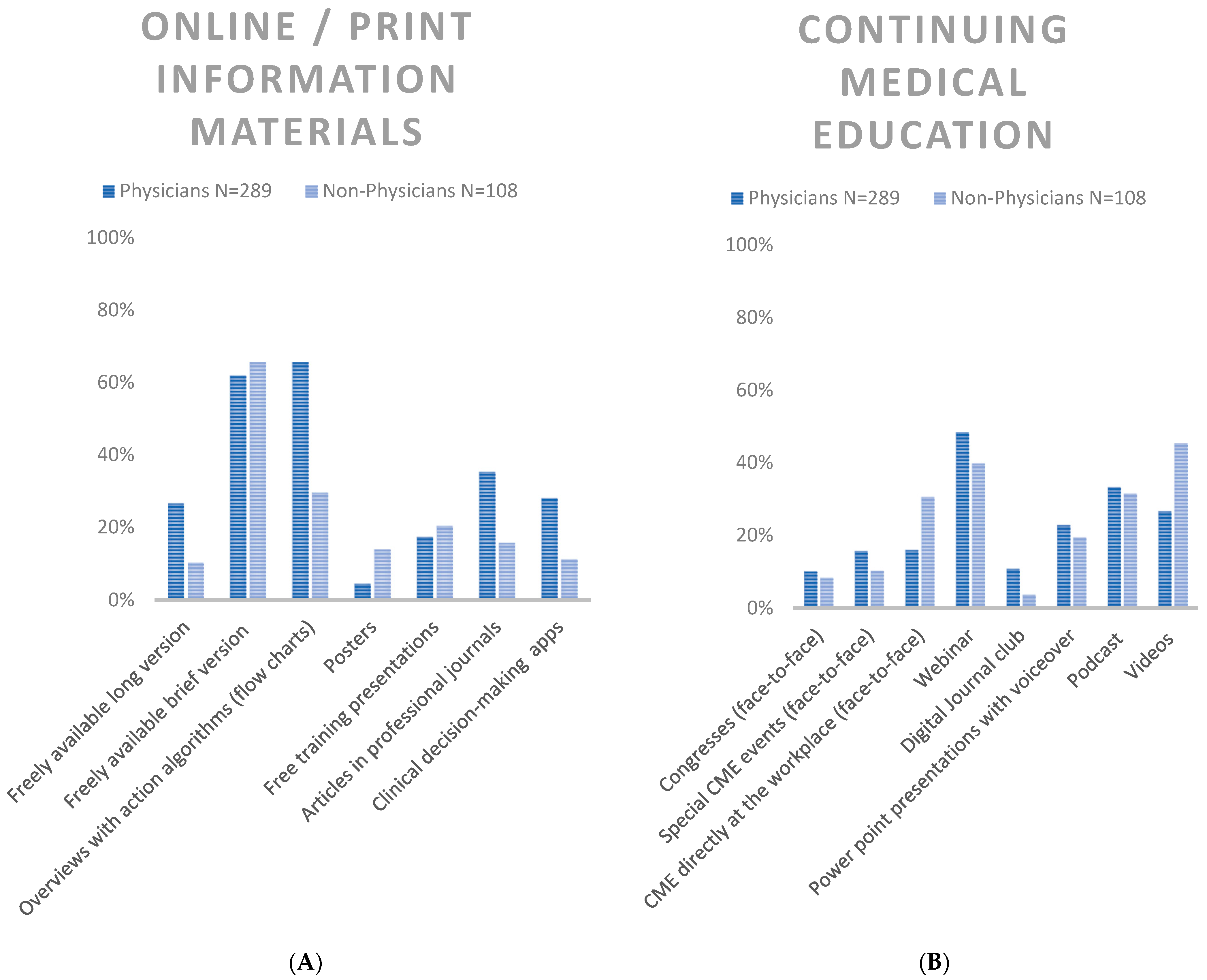
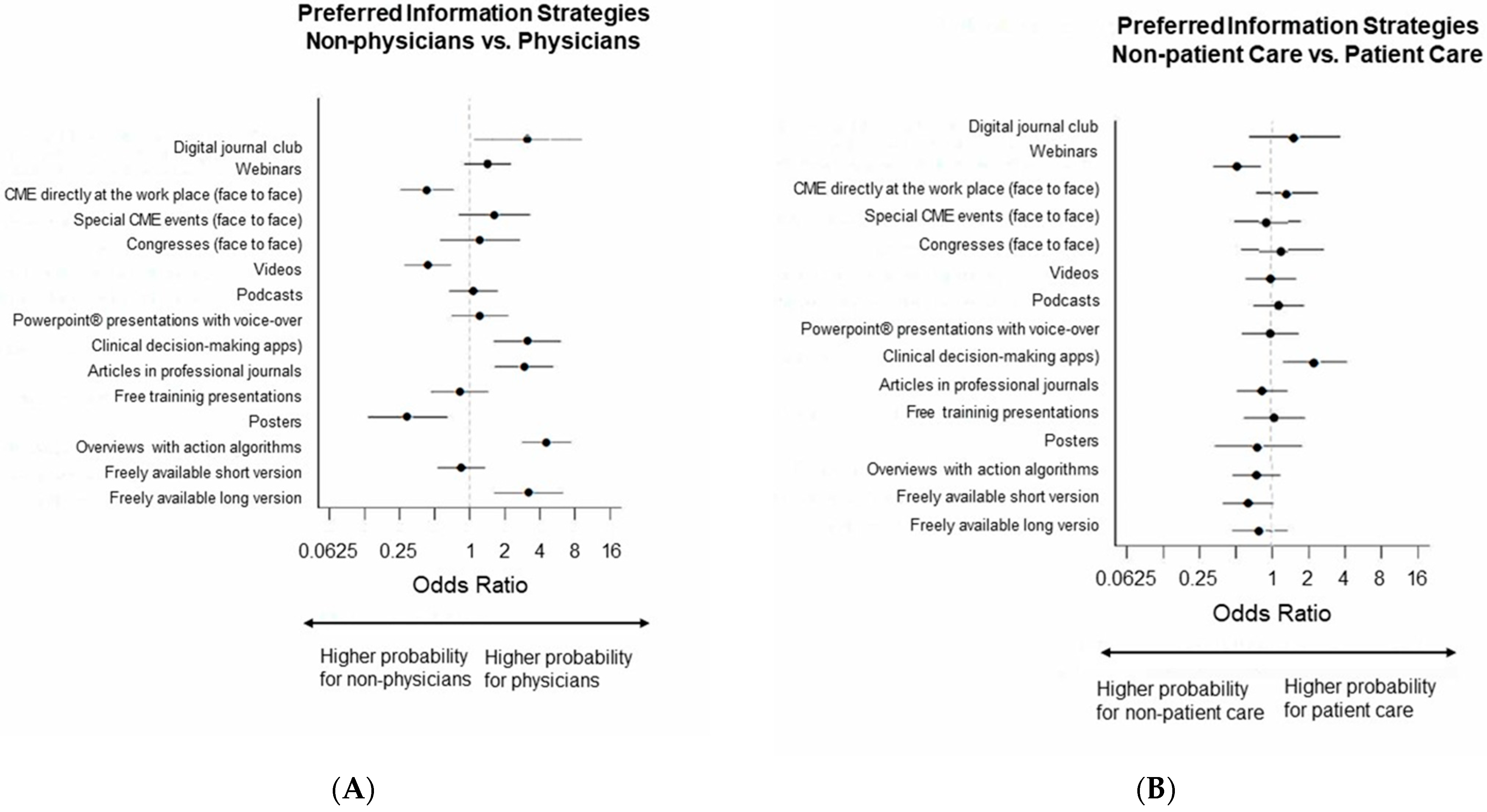
Online/Print Information Materials (in Professional Websites, Apps, Journals)
Continuing Medical Education
3.3. COVID-19 Vaccination Acceptance and Hesitancy Study (Study 2)
3.3.1. Media Usage
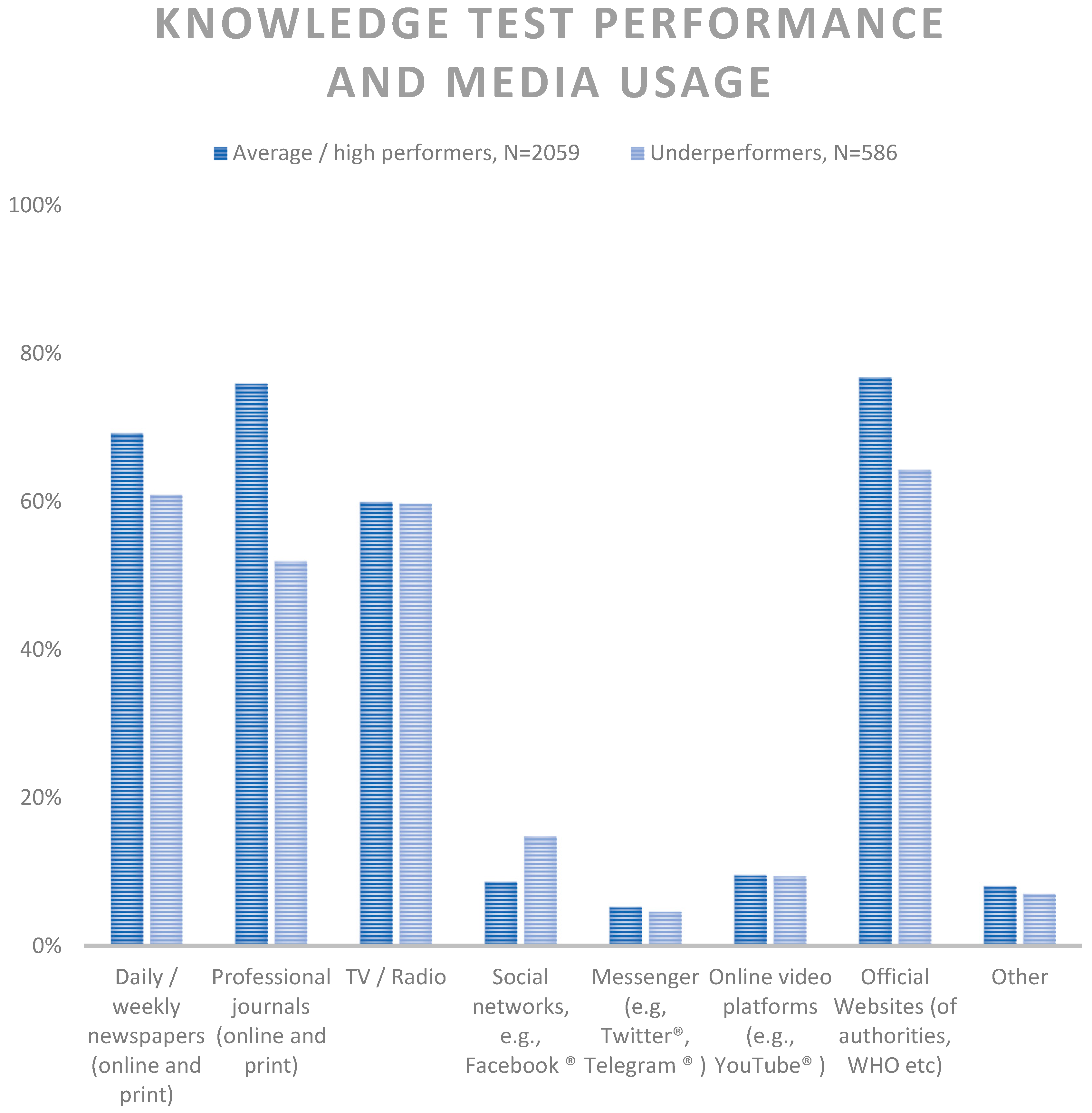
3.3.2. COVID-19 Knowledge Test Results and Media Usage
3.3.3. Trust in Authorities
4. Discussion
4.1. Information Channels
4.2. Information Sources Regarded as Trustworthy
4.3. Information Formats
4.4. Information Barriers
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dong, E.; Du, H.; Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020, 20, 533–534. [Google Scholar] [CrossRef] [PubMed]
- Maia Chagas, A.; Molloy, J.C.; Prieto-Godino, L.L.; Baden, T. Leveraging open hardware to alleviate the burden of COVID-19 on global health systems. PLoS Biol. 2020, 18, e3000730. [Google Scholar] [CrossRef] [PubMed]
- The, L. India under COVID-19 lockdown. Lancet 2020, 395, 1315. [Google Scholar] [CrossRef]
- Haider, N.; Osman, A.Y.; Gadzekpo, A.; Akipede, G.O.; Asogun, D.; Ansumana, R.; Lessells, R.J.; Khan, P.; Hamid, M.M.A.; Yeboah-Manu, D.; et al. Lockdown measures in response to COVID-19 in nine sub-Saharan African countries. BMJ Glob. Health 2020, 5, e003319. [Google Scholar] [CrossRef]
- Jassat, W.; Abdool Karim, S.S.; Ozougwu, L.; Welch, R.; Mudara, C.; Masha, M.; Rousseau, P.; Wolmarans, M.; Selikow, A.; Govender, N.; et al. Trends in Cases, Hospitalization and Mortality Related to the Omicron BA.4/BA.5 Sub-Variants in South Africa. Clin. Infect. Dis. 2022, 76, 1468–1475. [Google Scholar] [CrossRef]
- Webster, H.H.; Nyberg, T.; Sinnathamby, M.A.; Aziz, N.A.; Ferguson, N.; Seghezzo, G.; Blomquist, P.B.; Bridgen, J.; Chand, M.; Groves, N.; et al. Hospitalisation and mortality risk of SARS-CoV-2 variant omicron sub-lineage BA.2 compared to BA.1 in England. Nat. Commun. 2022, 13, 6053. [Google Scholar] [CrossRef]
- Kantrowitz-Gordon, I. A New Normal After the COVID-19 Pandemic. J. Midwifery Womens Health 2021, 66, 293–294. [Google Scholar] [CrossRef]
- Rathore, F.A.; Farooq, F. Information Overload and Infodemic in the COVID-19 Pandemic. J. Pak. Med. Assoc. 2020, 70 (Suppl. S3), S162–S165. [Google Scholar] [CrossRef]
- Mohammed, M.; Sha’aban, A.; Jatau, A.I.; Yunusa, I.; Isa, A.M.; Wada, A.S.; Obamiro, K.; Zainal, H.; Ibrahim, B. Assessment of COVID-19 Information Overload Among the General Public. J. Racial Ethn. Health Disparities 2021, 9, 184–192. [Google Scholar] [CrossRef]
- Bawden, D.; Robinson, L. Information overload: An overview. In Oxford Encyclopedia of Political Decision Making; Oxford University Press: Oxford, UK, 2020. [Google Scholar]
- World Health Organization. WHO Policy Brief: COVID-19: Infodemic Management, 14 September 2022; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Hong, H.; Kim, H.J. Antecedents and Consequences of Information Overload in the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 9305. [Google Scholar] [CrossRef]
- International Labour Organization. International Standard Classification of Occupations 2008 (ISCO-08): Structure, Group Definitions and Correspondence Tables; International Labour Organization: Geneva, Switzerland, 2012. [Google Scholar]
- World Health Organization. Classifying Health Workers: Mapping Occupations to the International Stadard Classification; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Hermes-DeSantis, E.R.; Hunter, R.T.; Welch, J.; Bhavsar, R.; Boulos, D.; Noue, M.-A. Preferences for Accessing Medical Information in the Digital Age: Health Care Professional Survey. J. Med. Internet Res. 2021, 23, e25868. [Google Scholar] [PubMed]
- Albano, D.; Soloff, A.; Heim, K.; Mavila, S. A Theory on the Relativity of Factors Impacting the Utilization of Medical Information Services From the Pharmaceutical Industry. Ther. Innov. Regul. Sci. 2016, 50, 554–559. [Google Scholar] [CrossRef]
- McCormack, L.; Sheridan, S.; Lewis, M.; Boudewyns, V.; Melvin, C.L.; Kistler, C.; Lux, L.J.; Cullen, K.; Lohr, K.N. Communication and dissemination strategies to facilitate the use of health-related evidence. In Database of Abstracts of Reviews of Effects (DARE): Quality-Assessed Reviews; Evidence Report/Technology Assessment; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2013; Volume 213, pp. 1–520. [Google Scholar]
- Robson, A.; Robinson, L. Building on models of information behaviour: Linking information seeking and communication. J. Doc. 2013, 69, 169–193. [Google Scholar] [CrossRef]
- Wilson, T.D. Human information behavior. Inf. Sci. 2000, 3, 49. [Google Scholar] [CrossRef] [PubMed]
- Clarke, M.A.; Belden, J.L.; Koopman, R.J.; Steege, L.M.; Moore, J.L.; Canfield, S.M.; Kim, M.S. Information needs and information-seeking behaviour analysis of primary care physicians and nurses: A literature review. Health Inf. Libr. J. 2013, 30, 178–190. [Google Scholar] [CrossRef] [PubMed]
- Seeber, C.; Popp, M.; Meerpohl, J.J.; Fichtner, F.; Werner, A.; Schmaderer, C.; Holzmann-Littig, C.; Dickel, S.; Grimm, C.; Moerer, O. COVID-19-Pandemie: Präferenzen und Barrieren für die Disseminierung von Evidenzsynthesen. Anaesthesist 2021, 71, 281–290. [Google Scholar] [CrossRef]
- Werner, A.; Popp, M.; Fichtner, F.; Holzmann-Littig, C.; Kranke, P.; Steckelberg, A.; Lühnen, J.; Redlich, L.M.; Dickel, S.; Grimm, C.; et al. COVID-19 Intensive Care-Evaluation of Public Information Sources and Current Standards of Care in German Intensive Care Units: A Cross Sectional Online Survey on Intensive Care Staff in Germany. Healthcare 2022, 10, 1315. [Google Scholar] [CrossRef]
- Meerpohl, J.J.; Voigt-Radloff, S.; Rueschemeyer, G.; Balzer, F.; Benstoem, C.; Binder, H.; Boeker, M.; Burns, J.; Dirnagl, U.; Featherstone, R.; et al. CEOsys: Creating an ecosystem for COVID-19 evidence. In Collaborating in Response to COVID-19: Editorial and Methods Initiatives across Cochrane; The Cochrane Collaboration: London, UK, 2020. [Google Scholar]
- Holzmann-Littig, C.; Braunisch, M.C.; Kranke, P.; Popp, M.; Seeber, C.; Fichtner, F.; Littig, B.; Carbajo-Lozoya, J.; Allwang, C.; Frank, T. COVID-19 Vaccination Acceptance and Hesitancy among Healthcare Workers in Germany. Vaccines 2021, 9, 777. [Google Scholar] [CrossRef]
- Holzmann-Littig, C.; Frank, T.; Schmaderer, C.; Braunisch, M.C.; Renders, L.; Kranke, P.; Popp, M.; Seeber, C.; Fichtner, F.; Littig, B.; et al. COVID-19 Vaccines: Fear of Side Effects among German Health Care Workers. Vaccines 2022, 10, 689. [Google Scholar] [CrossRef]
- Strengthening the Reporting of Observational Studies in Epidemiology. In STROBE Statement—Checklist of Items That Should Be Included in Reports of Cross-Sectional Studies; 2023; Available online: https://www.strobe-statement.org/checklists/ (accessed on 22 March 2023).
- Stebbins, R.A. Exploratory Research in the Social Sciences; Sage: Newcastle upon Tyne, UK, 2001; Volume 48. [Google Scholar]
- Leiner, D.J. SoSci Survey; 2019; Available online: https://www.soscisurvey.de (accessed on 27 May 2023).
- Lühnen, J.; Frese, T.; Mau, W.; Meyer, G.; Mikolajczyk, R.; Richter, M.; Schildmann, J.; Braunisch, M.C.; Fichtner, F.; Holzmann-Littig, C.; et al. Public information needs and preferences on COVID-19: A cross-sectional study. BMC Public Health 2023, 23, 394. [Google Scholar] [CrossRef]
- Robert Koch Institute. Aktualisierte Phaseneinteilung der COVID-19-Pandemie|Virushepatitis C im Jahr 2021. In Aktuelle Daten und Informationen zu Infektionskrankheiten und Public Health Epidemiologisches Bulletin; Robert Koch Institute: Berlin, Germany, 2022. [Google Scholar]
- Döring, N.; Bortz, J. Forschungsmethoden und Evaluation; Springer: Wiesbaden, Germany, 2016. [Google Scholar]
- Rechel, B.; Jakubowski, E.; McKee, M.; Nolte, E. Organization and Financing of Public Health Services in Europe; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Grimshaw, J.M.; Eccles, M.P.; Lavis, J.N.; Hill, S.J.; Squires, J.E. Knowledge translation of research findings. Implement. Sci. 2012, 7, 50. [Google Scholar] [CrossRef]
- Kernohan, W.G.; Brown, M.J.; Payne, C.; Guerin, S. Barriers and facilitators to knowledge transfer and exchange in palliative care research. BMJ Evid.-Based Med. 2018, 23, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Lafuente-Lafuente, C.; Leitao, C.; Kilani, I.; Kacher, Z.; Engels, C.; Canouï-Poitrine, F.; Belmin, J. Knowledge and use of evidence-based medicine in daily practice by health professionals: A cross-sectional survey. BMJ Open 2019, 9, e025224. [Google Scholar] [CrossRef]
- O’Keeffe, J.; Willinsky, J.; Maggio, L. Public access and use of health research: An exploratory study of the National Institutes of Health (NIH) Public Access Policy using interviews and surveys of health personnel. J. Med. Internet Res. 2011, 13, e97. [Google Scholar] [CrossRef]
- LaGrone, L.N.; Fuhs, A.K.; Egoavil, E.H.; Langdale, L.A.; Fuangworawong, P.; Hamasaki, J.L.; Gyedu, A.; Mock, C.N. A Global Assessment of Access to and Use of Medical Information: The State of Evidence-Based Surgery. World J. Surg. 2018, 42, 521–531. [Google Scholar] [CrossRef]
- Lenzner, T.; Menold, N. Question Wording, Version 2.0; GESIS—Leibniz-Institut für Sozialwissenschaften: Mannheim, Germany, 2016. [Google Scholar]
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
- Bundeszentrale für Gesundheitliche Aufklärung. Begleitforschung zur Kommunikation der Corona-Schutzimpfung in Deutschland (CoSiD); Deutschlandweite Zusatzbefragung des Medizinischen und Pflegerischen Personals im Juli 2021; BZgA-Forschungsbericht; Bundeszentrale für Gesundheitliche Aufklärung: Cologne, Germany, 2022. [Google Scholar] [CrossRef]
- D’Souza, R.S.; D’Souza, S.; Strand, N.; Anderson, A.; Vogt, M.N.P.; Olatoye, O. YouTube as a source of medical information on the novel coronavirus 2019 disease (COVID-19) pandemic. Glob. Public Health 2020, 15, 935–942. [Google Scholar] [CrossRef]
- Lohiniva, A.-L.; Hussein, I.; Lehtinen, J.-M.; Sivelä, J.; Hyökki, S.; Nohynek, H.; Nuorti, P.; Lyytikäinen, O. Qualitative Insights into Vaccine Uptake of Nursing Staff in Long-Term Care Facilities in Finland. Vaccines 2023, 11, 530. [Google Scholar] [CrossRef]
- Rathnayake, S.; Dasanayake, D.; Maithreepala, S.D.; Ekanayake, R.; Basnayake, P.L. Nurses’ perspectives of taking care of patients with Coronavirus disease 2019: A phenomenological study. PLoS ONE 2021, 16, e0257064. [Google Scholar] [CrossRef] [PubMed]
- Sasso, L.; Bagnasco, A.; Catania, G.; Zanini, M.; Aleo, G.; Watson, R. Push and pull factors of nurses’ intention to leave. J. Nurs. Manag. 2019, 27, 946–954. [Google Scholar] [CrossRef] [PubMed]
- Gustavsson, K.; Goetz-Kundera, Z.; Flaga-Łuczkiewicz, M.; Wichniak, A. Which Aspects of Work Safety Satisfaction Are Important to Mental Health of Healthcare Workers during COVID-19 Pandemic in Poland? Int. J. Environ. Res. Public Health 2023, 20, 2870. [Google Scholar] [CrossRef]
- Wan, J.; Xia, H. How Advanced Practice Nurses Can Be Better Managed in Hospitals: A Multi-Case Study. Healthcare 2023, 11, 780. [Google Scholar] [CrossRef]
- Magnavita, N.; Chiorri, C.; Acquadro Maran, D.; Garbarino, S.; Di Prinzio, R.R.; Gasbarri, M.; Matera, C.; Cerrina, A.; Gabriele, M.; Labella, M. Organizational Justice and Health: A Survey in Hospital Workers. Int. J. Environ. Res. Public Health 2022, 19, 9739. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.C.; Guo, Y.L.; Chin, W.S.; Cheng, N.Y.; Ho, J.J.; Shiao, J.S. Patient-Nurse Ratio is Related to Nurses’ Intention to Leave Their Job through Mediating Factors of Burnout and Job Dissatisfaction. Int. J. Environ. Res. Public Health 2019, 16, 4801. [Google Scholar] [CrossRef] [PubMed]
- Drennan, V.M.; Ross, F. Global nurse shortages-the facts, the impact and action for change. Br. Med. Bull. 2019, 130, 25–37. [Google Scholar] [CrossRef]
- Toscano, F.; Tommasi, F.; Giusino, D. Burnout in Intensive Care Nurses during the COVID-19 Pandemic: A Scoping Review on Its Prevalence and Risk and Protective Factors. Int. J. Environ. Res. Public Health 2022, 19, 12914. [Google Scholar] [CrossRef]
- Ghare, F.; Meckawy, R.; Moore, M.; Lomazzi, M. Determinants of Acceptance of COVID-19 Vaccination in Healthcare and Public Health Professionals: A Review. Vaccines 2023, 11, 311. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Clarke, R.M.; Jarrett, C.; Eckersberger, E.; Levine, Z.; Schulz, W.S.; Paterson, P. Measuring trust in vaccination: A systematic review. Hum. Vaccines Immunother. 2018, 14, 1599–1609. [Google Scholar] [CrossRef] [PubMed]
- Peterson, C.J.; Lee, B.; Nugent, K. COVID-19 Vaccination Hesitancy among Healthcare Workers—A Review. Vaccines 2022, 10, 948. [Google Scholar] [CrossRef]
- Torres, R.M.; Reviglio, V.; Basanta, I.; Srikumaran, D. Webinars and Continuing Medical Education: Pros, Cons, and Controversies. South Med. J. 2022, 115, 301–303. [Google Scholar] [CrossRef]
- Knoepke, C.E.; Ingle, M.P.; Matlock, D.D.; Brownson, R.C.; Glasgow, R.E. Dissemination and stakeholder engagement practices among dissemination & implementation scientists: Results from an online survey. PLoS ONE 2019, 14, e0216971. [Google Scholar] [CrossRef]
- Gulland, A. Doctors cite lack of time as greatest barrier to research. BMJ 2016, 352, i1488. [Google Scholar] [CrossRef]
- AlRyalat, S.A.; Saleh, M.; Alaqraa, M.; Alfukaha, A.; Alkayed, Y.; Abaza, M.; Abu Saa, H.; Alshamiry, M. The impact of the open-access status on journal indices: A review of medical journals. F1000Res 2019, 8, 266. [Google Scholar] [CrossRef]
- Aakre, C.A.; Maggio, L.A.; Fiol, G.D.; Cook, D.A. Barriers and facilitators to clinical information seeking: A systematic review. J. Am. Med. Inform. Assoc. 2019, 26, 1129–1140. [Google Scholar] [CrossRef] [PubMed]
- Hlatshwako, T.G.; Shah, S.J.; Kosana, P.; Adebayo, E.; Hendriks, J.; Larsson, E.C.; Hensel, D.J.; Erausquin, J.T.; Marks, M.; Michielsen, K. Online health survey research during COVID-19. Lancet Digit. Health 2021, 3, e76–e77. [Google Scholar] [CrossRef] [PubMed]
- Bethlehem, J. Selection bias in web surveys. Int. Stat. Rev. 2010, 78, 161–188. [Google Scholar] [CrossRef]
- Hurst, D.; Mickan, S. Describing knowledge encounters in healthcare: A mixed studies systematic review and development of a classification. Implement. Sci. 2017, 12, 35. [Google Scholar] [CrossRef]
- Daei, A.; Soleymani, M.R.; Ashrafi-Rizi, H.; Zargham-Boroujeni, A.; Kelishadi, R. Clinical information seeking behavior of physicians: A systematic review. Int. J. Med. Inform. 2020, 139, 104144. [Google Scholar] [CrossRef]
| Study 1 | Study 2 | ||||
|---|---|---|---|---|---|
| Hospitals/Doctor’s Practices | Public Health Care Services | Inpatient and Outpatient Care, N = 2700 | |||
| Physicians, N = 211 | Non-physicians, N = 71 | Physicians, N = 88 | Non-Physicians, N = 43 | Physicians, N = 1841 | Non-Physicians, N = 859 |
| Residents, N = 91 Specialist physicians, N = 120 | Nursing staff, N = 45 Other non-physician medical professionals, e.g., medical technical assistants, N = 26 | Physicians, practically active, N = 42 Physicians, administra-tively active, N = 46 | Non-physician health care professionals, hands-on, N = 5 Non-physician health care professional, administrative, N = 6 Other function in administration/organization, N = 23 Other, N = 9 | Residents, N = 323 Specialist Physicians, N = 1329 Dentists, N = 189 | Nursing staff, N = 466 Other non-physician medical professionals, e.g., medical technical assistants, N = 346 Dentistry non-physician medical personnel, N = 47 |
| Study 1, N = 413 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Item | Physicians, N = 299; N (%) | Non-Physicians, N = 114; N (%) | p | Odds Ratio [95% CI] | Patient Care, N = 303; N (%) | Non-Patient Care, N = 110; N (%) | p | Odds Ratio [95% CI] |
| Which of the following platforms and channels do you or would you use to become aware of newly generated evidence/treatment recommendations | ||||||||
| Online Community or Social Media | ||||||||
| Missing | 0 | 0 | 0 | 0 | ||||
| 34 (11.4) | 11 (9.6) | 0.616 | 1.20 [0.59–2.46] | 34 (11.2) | 11 (10.0) | 0.725 | 1.14 [0.55–2.33] | |
| 42 (14.0) | 33 (28.9) | <0.001 | 0.40 [0.24–0.67] | 57 (18.8) | 18 (16.4) | 0.568 | 1.18 [0.66–2.12] | |
| 15 (5.0) | 18 (15.8) | <0.001 | 0.28 [0.14–0.58] | 26 (8.6) | 7 (6.4) | 0.463 | 1.38 [0.58–3.28] | |
| Youtube | 52 (17.4) | 30 (26.3) | 0.042 | 0.59 [0.35–0.98] | 62 (20.5) | 20 (18.2) | 0.608 | 1.16 [0.66–2.03] |
| Messenger channel (e.g., Telegram) | 49 (16.4) | 12 (10.5) | 0.133 | 1.67 [0.85–3.26] | 47 (15.5) | 14 (12.7) | 0.481 | 1.26 [0.66–2.03] |
| Networking in a research portal (e.g., ResearchGate) | 127 (42.5) | 26 (22.8) | <0.001 | 2.50 [1.52–4.10] | 101 (33.3) | 52 (47.3) | 0.010 | 0.56 [0.36–0.87] |
| Other | 48 (16.1) | 15 (13.2) | 0.464 | 1.26 [0.68–2.36] | 48 (15.8) | 15 (13.6) | 0.582 | 1.19 [0.64–2.23] |
| Campaigns or advertisements via | ||||||||
| automated newsfeed (RSS feed) | 30 (10.0) | 12 (10.5) | 0.882 | 0.95 [0.47–1.92] | 28 (9.2) | 14 (12.7) | 0.300 | 0.70 [0.35–1.38] |
| Email/newsletter | 168 (56.2) | 53 (46.5) | 0.077 | 1.48 [0.96–2.28] | 171 (56.4) | 50 (45.5) | 0.048 | 1.55 [1.00–2.41] |
| Professional journals | 165 (55.2) | 23 (20.2) | <0.001 | 4.87 [2.92–8.12] | 148 (48.8) | 40 (36.4) | 0.024 | 1.67 [1.07–2.62] |
| Television | 69 (23.1) | 65 (57.0) | <0.001 | 0.23 [0.14–0.36] | 91 (30.0) | 43 (49.1) | 0.082 | 0.67 [0.42–1.05] |
| Radio | 58 (19.4) | 46 (40.4) | <0.001 | 0.36 [0.22–0.57] | 72 (23.8) | 32 (29.1) | 0.270 | 0.76 [0.47–1.24] |
| Daily/weekly press | 65 (21.7) | 37 (32.5) | 0.024 | 0.58 [0.36–0.93] | 74 (24.4) | 28 (25.5) | 0.830 | 0.95 [0.57–1.56] |
| Internet pages of the Robert Koch Institute, AWMF, Federal Ministry of Health, etc. | 188 (62.9) | 65 (57.0) | 0.275 | 1.28 [0.82–1.98] | 173 (57.1) | 80 (72.2) | 0.004 | 0.50 [0.31–0.80] |
| Professional societies/medical associations | 149 (49.8) | 15 (13.2) | <0.001 | 6.56 [3.64–11.81] | 117 (38.6) | 47 (42.7) | 0.450 | 0.84 [0.54–1.31] |
| Other | 3 (1.0) | 3 (2.6) | 0.216 | 0.38 [0.07–1.89] | 3 (1.0) | 3 (2.7) | 0.192 | 0.36 [0.07–1.79] |
| Study 1, N = 413 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Item | Physicians, N = 299; N (%) | Non-Physicians, N = 114; N (%) | p | Odds Ratio [95% CI] | Patient Care, N = 303; N (%) | Non-Patient Care, N = 110; N (%) | p | Odds Ratio [95% CI] |
| Which organizations (source of information) do you rate as most trustworthy regarding information on COVID-19 medical therapy? | ||||||||
| Missing | 19 | 11 | 23 | 7 | ||||
| Cochrane Collaboration | 78 (27.9) | 5 (4.9) | <0.001 | 7.57 [2.97–19.29] | 61 (21.8) | 22 (21.4) | 0.928 | 1.03 [0.59–1.78] |
| German Network for Evidence-Based Medicine (EbM Network) | 41 (14.6) | 6 (5.8) | 0.020 | 2.77 [1.14–6.74] | 32 (11.4) | 15 (14.6) | 0.407 | 0.76 [0.39–1.46] |
| Professional societies (e.g., DIVI, DGAI, DGIIN) | 139 (49.6) | 16 (15.5) | <0.001 | 5.36 [2.99–9.60] | 124 (44.3) | 31 (30.1) | 0.012 | 1.85 [1.14–2.99] |
| Program for National Health Care Guidelines (cooperation of German Medical Association, KBV, AWMF) | 92 (32.9) | 11 (10.7) | <0.001 | 4.09 [2.09–8.02] | 76 (27.1) | 27 (26.2) | 0.856 | 1.05 [0.63–1.75] |
| World Health Organization (WHO) | 69 (24.6) | 42 (40.8) | 0.002 | 0.47 [0.29–0.77] | 89 (31.8) | 22 (21.4) | 0.046 | 1.72 [1.01–2.93] |
| Robert Koch Institute | 223 (79.6) | 95 (92.2) | 0.004 | 0.33 [0.15–0.72] | 229 (81.8) | 89 (86.4) | 0.285 | 0.71 [0.37–1.34] |
| Federal Center for Health Education | 24 (8.6) | 28 (27.2) | <0.001 | 0.25 [0.14–0.46] | 29 (10.4) | 23 (22.3) | 0.002 | 0.40 [0.22–0.73] |
| Other | 9 (3.2) | 6 (5.8) | 0.243 | 0.54 [0.19–1.55] | 9 (3.2) | 6 (5.8) | 0.243 | 0.54 [0.19–1.55] |
| Study 1, N = 413 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Item | Physicians, N = 299; N (%) | Non-Physicians, N = 114; N (%) | p | Odds Ratio [95% CI] | Patient Care, N = 303; N (%) | Non-Patient Care, N = 110; N (%) | p | Odds Ratio [95% CI] |
| What barriers do you face to acquiring evidence-based knowledge | ||||||||
| Missing | 23 | 14 | 27 | 10 | ||||
| I have too little time in my daily work to deal with evidence syntheses. | 218 (79.0) | 55 (55.0) | <0.001 | 3.08 [1.89–5.01] | 200 (72.5) | 73 (73.0) | 0.918 | 0.97 [0.58–1.63] |
| The independent acquisition of evidence-based knowledge is not encouraged by my superiors. | 30 (10.9) | 10 (10.0) | 0.809 | 1.10 [0.52–2.34] | 34 (12.3) | 6 (6.0) | 0.079 | 2.20 [0.89–5.41] |
| I have no experience in dealing with evidence syntheses. | 28 (10.1) | 30 (30.0) | <0.001 | 0.26 [0.15–0.47] | 40 (14.5) | 18 (18.0) | 0.405 | 0.75 [0.41–1.39] |
| I am unsure/don’t know where or how to access reliable evidence syntheses. | 53 (19.2) | 21 (21.0) | 0.699 | 0.89 [0.51–1.58] | 61 (22.0) | 13 (13.0) | 0.050 | 1.90 [0.99–3.63] |
| Access to evidence syntheses is too cumbersome (e.g., paid subscriptions/memberships). | 99 (35.9) | 17 (17.0) | <0.001 | 2.73 [1.53–4.86] | 81 (29.3) | 35 (35.0) | 0.294 | 0.77 [0.47–1.25] |
| The language in evidence syntheses is too complex and difficult for me to understand. | 13 (4.7) | 20 (20.0) | <0.001 | 0.20 [0.09–0.42] | 21 (7.6) | 12 (12.0) | 0.184 | 0.60 [0.29–1.28] |
| The content in evidence syntheses is not well matched to my target audience (e.g., in terms of prior knowledge, relevance). | 31 (11.2) | 17 (17.0) | 0.139 | 0.62 [0.33–1.17] | 33 (12.0) | 15 (15.0) | 0.435 | 0.77 [0.40–1.49] |
| I reject the acquisition of knowledge from evidence syntheses, because in my opinion the contents are not practicable in everyday life (e.g. too undifferentiated, not applicable to the individual). | 3 (1.1) | 1 (1.0) | 0.942 | 1.09 [0.11–10.58] | 1 (0.4) | 3 (3.0) | 0.028 | 0.12 [0.01–1.14] |
| Other | 11 (4.0) | 3 (3.0) | 0.656 | 1.342 [0.37–4.91] | 13 (4.7) | 1 (1.0) | 0.093 | 4.89 [0.63–37.90] |
| COVID-19 Vaccination Acceptance and Hesitancy Study | ||||
|---|---|---|---|---|
| Physicians N = 1841 | Non-Physicians N = 859 | p | Odd’s Ratio [95% CI] | |
| From what media do you get your information on COVID-19 vaccination, N = 2700 | ||||
| Missing | 0 | 0 | ||
| Daily newspapers, weekly magazines (print) | 620 (33.7) | 231 (26.9) | <0.001 | 1.38 [1.15–1.65] |
| Daily newspapers, weekly magazines (online) | 996 (54.1) | 405 (47.1) | <0.001 | 1.32 [1.12–1.55] |
| Daily/weekly newspapers and magazines (online and print) | 1280 (69.5) | 537 (62.5) | <0.001 | 1.37 [1.15–1.62] |
| Scientific journals (print) | 599 (32.5) | 108 (12.6) | <0.001 | 3.35 [2.68–4.20] |
| Scientific journals (online) | 1269 (68.9) | 406 (47.3) | <0.001 | 2.48 [2.10–2.92] |
| Scientific journals (print and online) | 1449 (78.7) | 439 (51.1) | <0.001 | 3.54 [2.97–4.21] |
| Television/radio | 1077 (58.5) | 540 (62.9) | 0.031 | 0.83 [0.71–0.98] |
| Social networks (e.g., Facebook) | 150 (8.1) | 122 (14.2) | <0.001 | 0.54 [0.42–0.69] |
| Messenger services (e.g., Twitter, Telegram) | 94 (5.1) | 43 (5.0) | 0.912 | 1.02 [0.71–1.48] |
| Online video platforms (e.g., YouTube) | 157 (8.5) | 100 (11.6) | 0.010 | 0.71 [0.54–0.92} |
| Websites/information portals of government health authorities (e.g., RKI, WHO) | 1346 (73.1) | 649 (75.6) | 0.179 | 0.88 [0.73–1.06] |
| Other | 114 (6.2) | 95 (11.1) | <0.001 | 0.53 [0.40–0.71] |
| Knowledge test | ||||
| Missing | 20 | 35 | ||
| 0 points | 34 (1.9) | 40 (4.9) | <0.001 | 0.37 [0.23–0.59] |
| 1 point | 62 (3.4) | 71 (8.6) | <0.001 | 0.37 [0.26–0.53] |
| 2 points | 215 (11.8) | 164 (19.9) | <0.001 | 0.54 [0.43–0.67] |
| 3 points | 485 (26.6) | 299 (36.3) | <0.001 | 0.64 [0.53–0.76] |
| 4 points | 1025 (56.3) | 250 (30.3) | <0.001 | 2.96 [2.48–3.52] |
| I trust the regulatory authorities of vaccines in Germany in general | ||||
| Missing | 0 | 0 | ||
| I fully agree/I rather agree | 1655 (90.0) | 727 (85.0) | <0.001 | 1.62 [1.27–2.05] |
| I trust the European regulatory authorities of COVID-19 vaccines used in Germany | ||||
| Missing | 0 | 0 | ||
| I fully agree/I rather agree | 1530 (83.1) | 670 (78.6) | <0.001 | 1.39 [1.13–1.70] |
| I generally trust in the German health care politics | ||||
| Missing | 0 | 0 | ||
| I fully agree/I rather agree | 1081 (58.8) | 483 (56.7) | 0.299 | 1.11 [0.94–1.30] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Holzmann-Littig, C.; Stadler, D.; Popp, M.; Kranke, P.; Fichtner, F.; Schmaderer, C.; Renders, L.; Braunisch, M.C.; Assali, T.; Platen, L.; et al. Locating Medical Information during an Infodemic: Information Seeking Behavior and Strategies of Health-Care Workers in Germany. Healthcare 2023, 11, 1602. https://doi.org/10.3390/healthcare11111602
Holzmann-Littig C, Stadler D, Popp M, Kranke P, Fichtner F, Schmaderer C, Renders L, Braunisch MC, Assali T, Platen L, et al. Locating Medical Information during an Infodemic: Information Seeking Behavior and Strategies of Health-Care Workers in Germany. Healthcare. 2023; 11(11):1602. https://doi.org/10.3390/healthcare11111602
Chicago/Turabian StyleHolzmann-Littig, Christopher, David Stadler, Maria Popp, Peter Kranke, Falk Fichtner, Christoph Schmaderer, Lutz Renders, Matthias Christoph Braunisch, Tarek Assali, Louise Platen, and et al. 2023. "Locating Medical Information during an Infodemic: Information Seeking Behavior and Strategies of Health-Care Workers in Germany" Healthcare 11, no. 11: 1602. https://doi.org/10.3390/healthcare11111602






