Constructing a Learning Curve to Discuss the Medical Treatments and the Effect of Vaccination of COVID-19
Abstract
1. Background
2. Materials and Methods
2.1. Equation and Model Interpretation
2.2. Criterion of Sample Selection
2.3. Data Collection
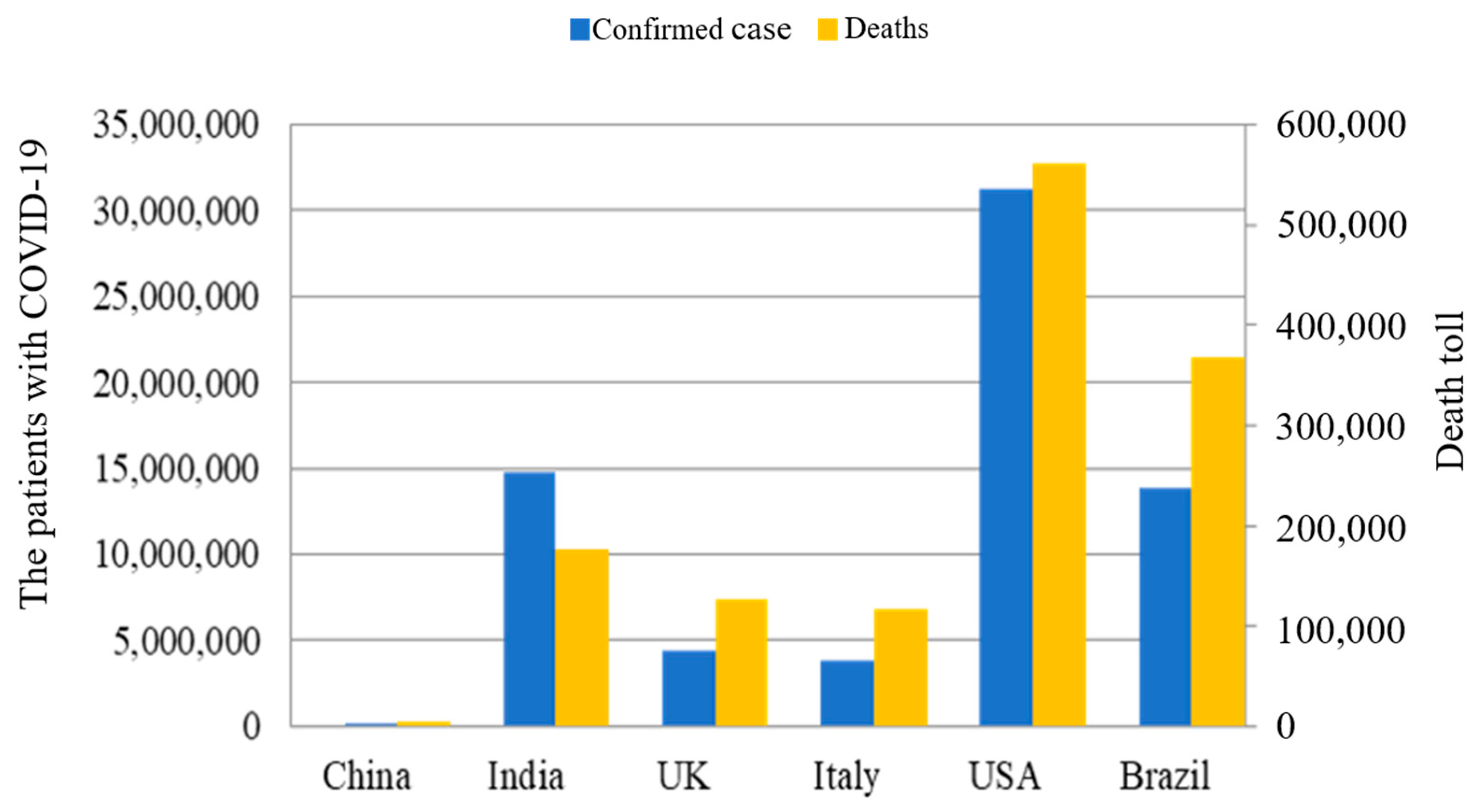
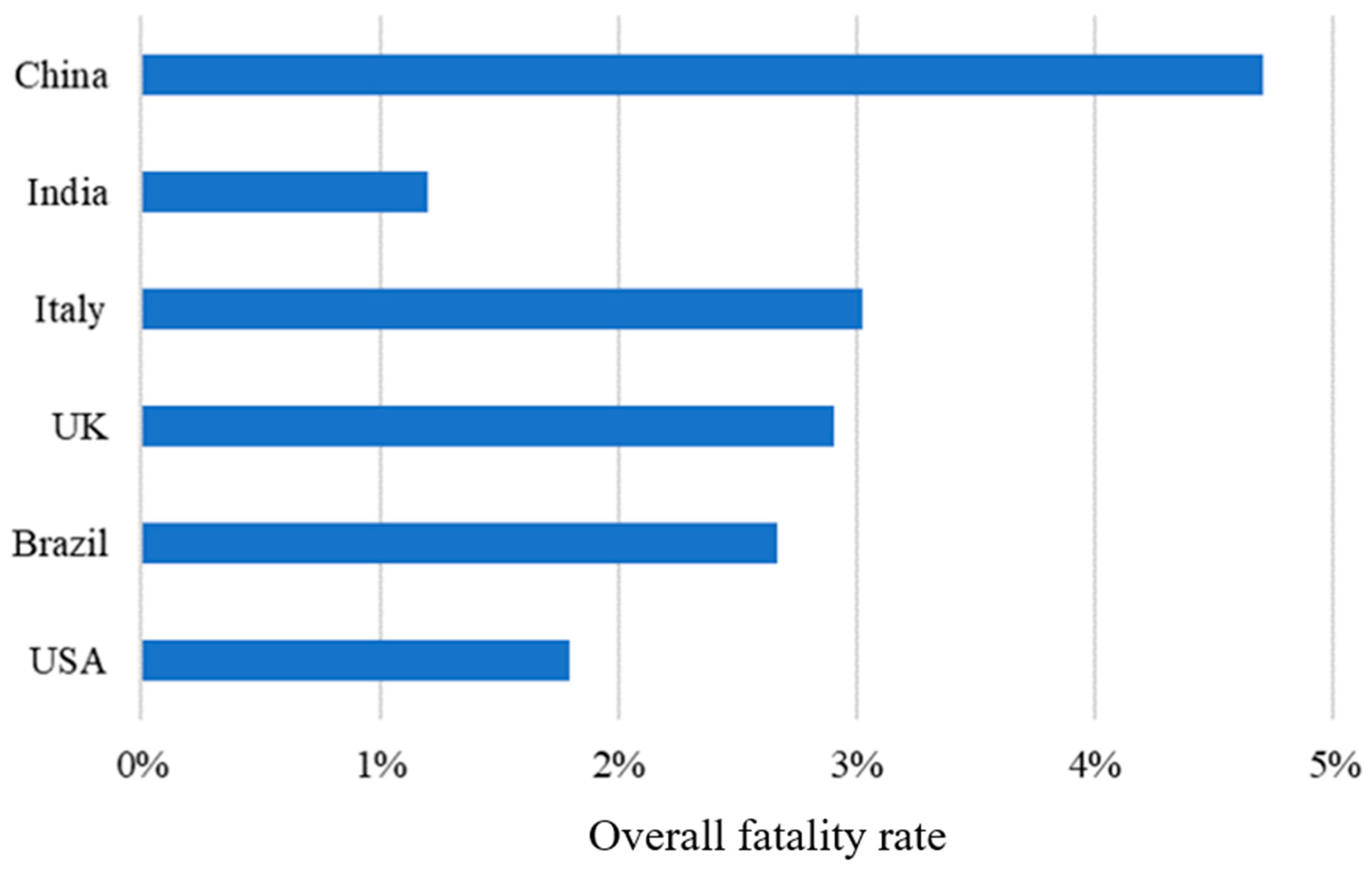
3. Results
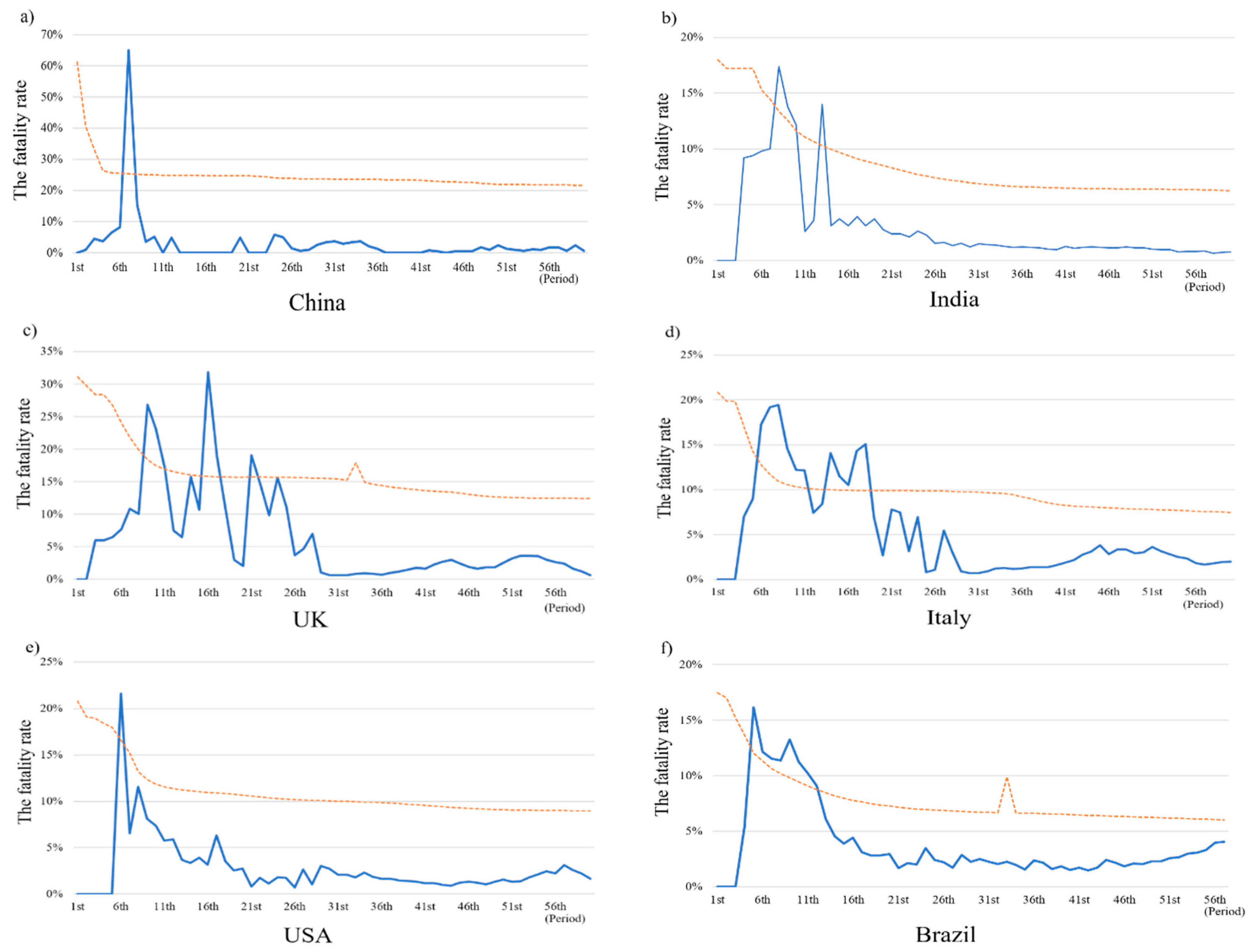
3.1. The Trend of Fatality Rates
3.2. The Effect of Learning in Medical Treatment on Fatality Rates Reduction
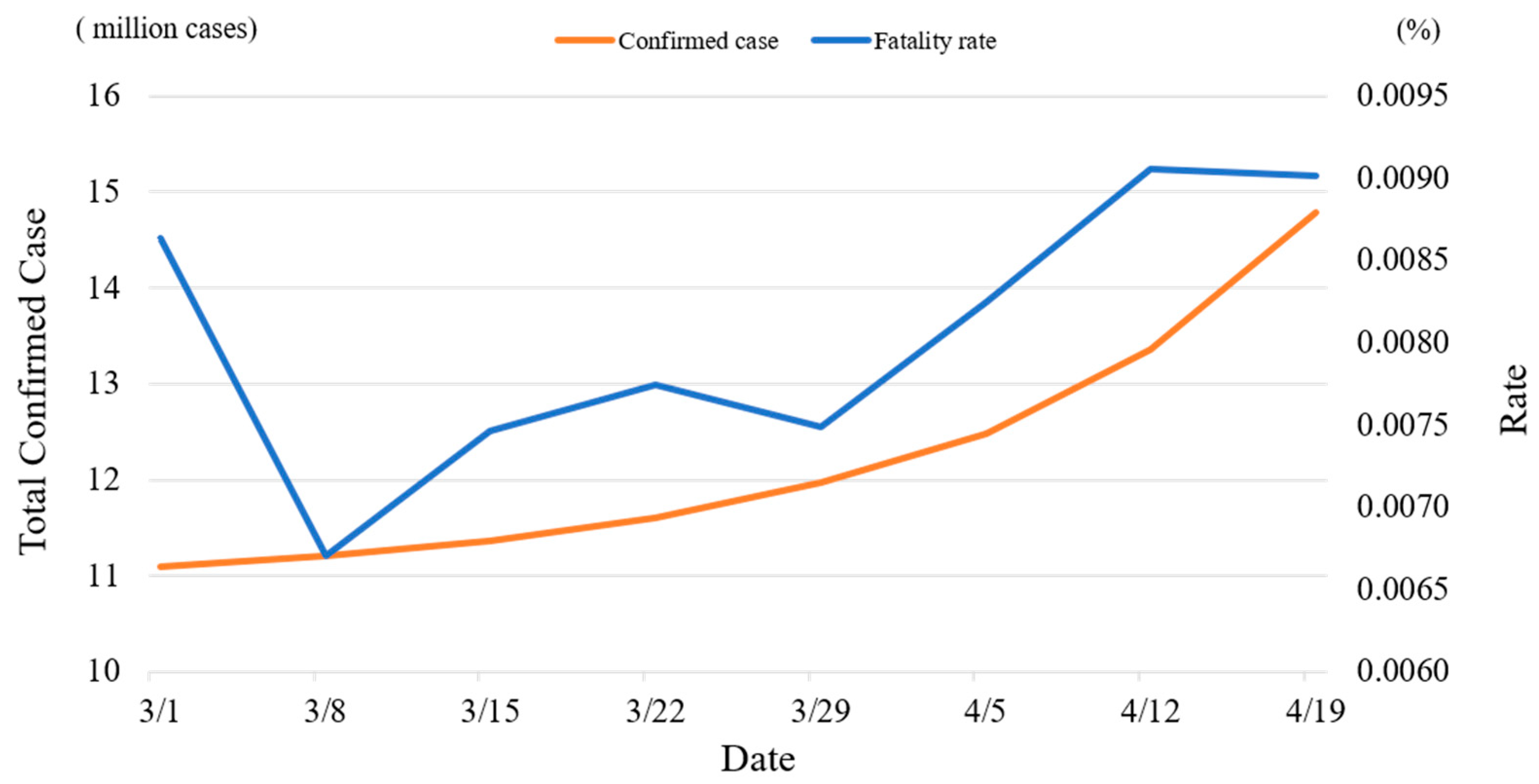
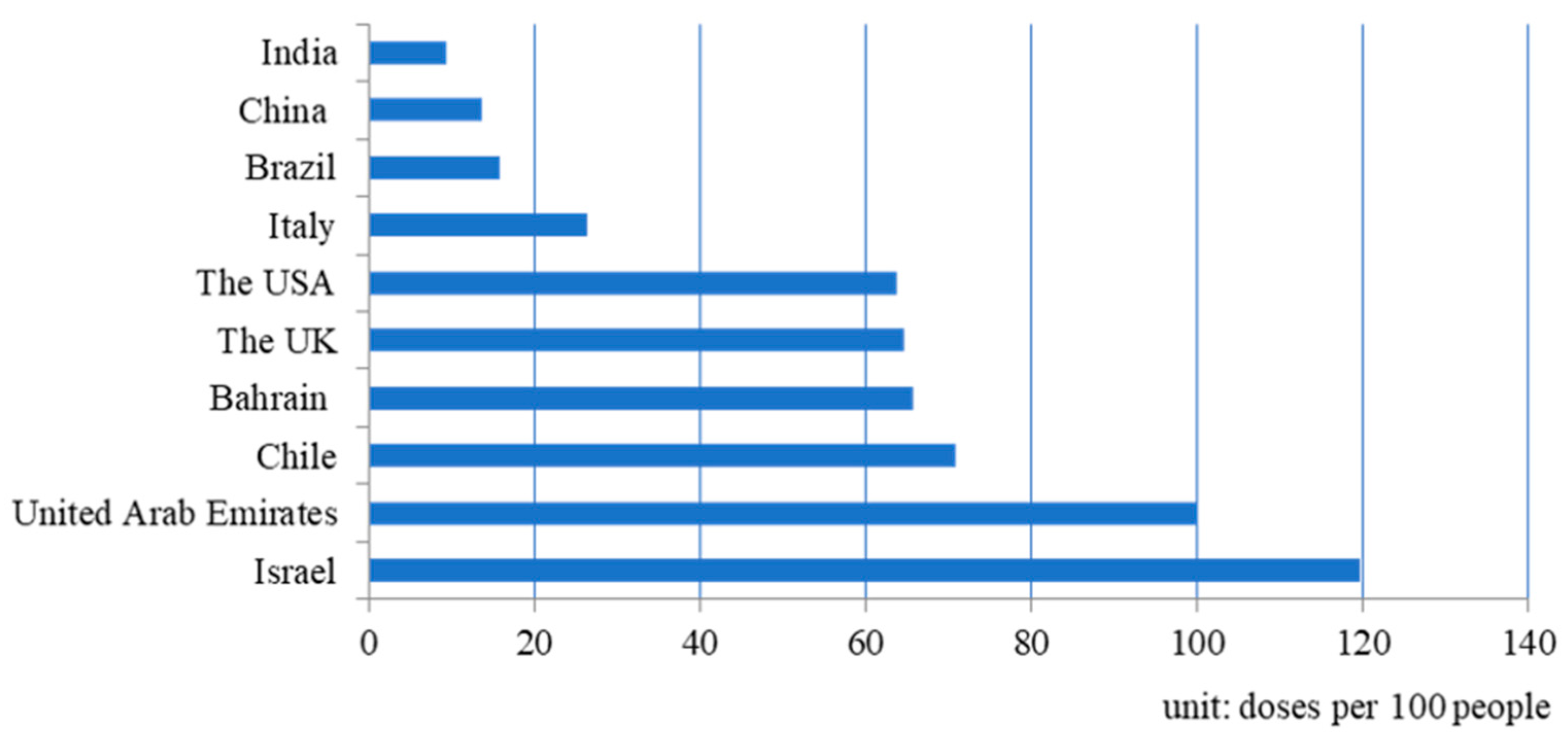
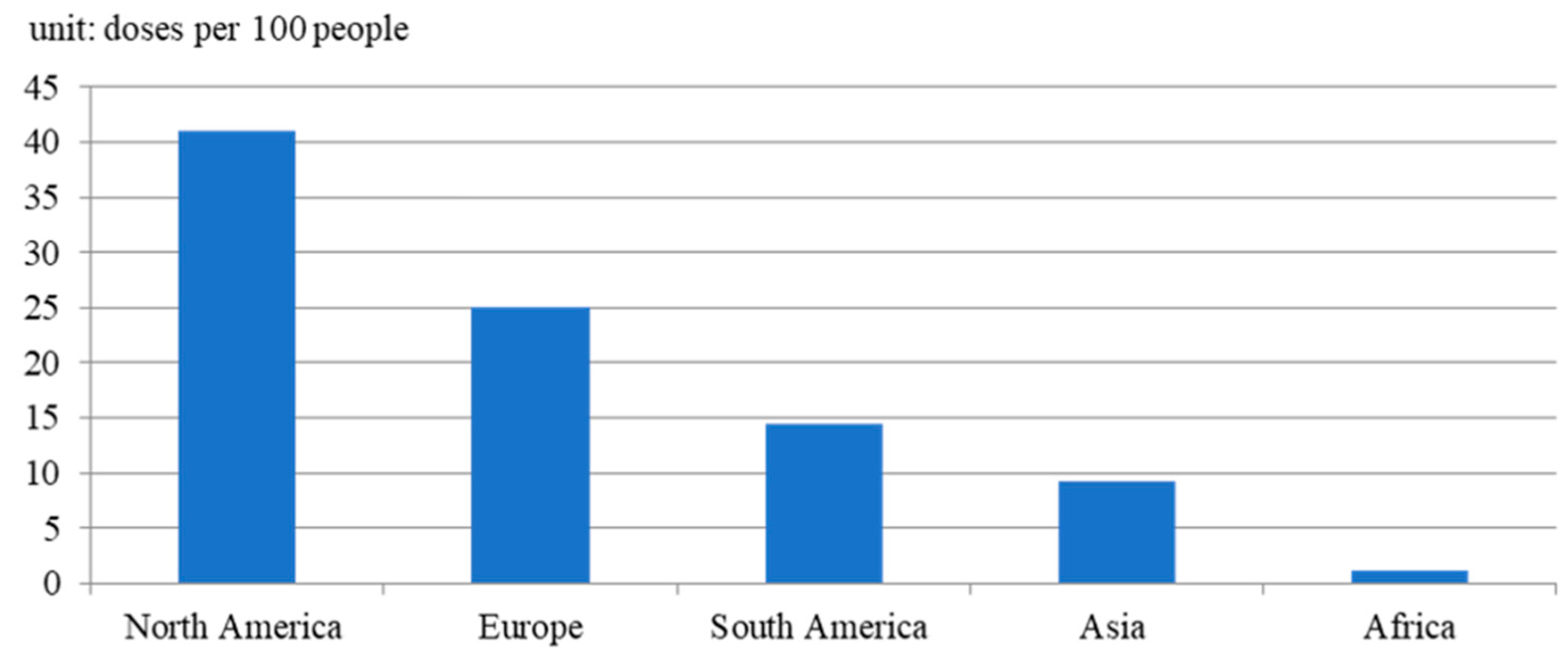
3.3. The Effect of Vaccination on Fatality Rates Reduction
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Novel Coronavirus (2019-nCoV): Situation Report. 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 25 May 2021).
- Shams, S.A.; Haleem, A.; Javaid, M. Analyzing COVID-19 pandemic for unequal distribution of tests, identified cases, deaths, and fatality rates in the top 18 countries. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 953–961. [Google Scholar] [CrossRef] [PubMed]
- Segovia-Juarez, J.; Castagnetto, J.M.; Gonzales, G.F. High altitude reduces infection rate of COVID-19 but not case-fatality rate. Respir. Physiol. Neurobiol. 2020, 281, 103494. [Google Scholar] [CrossRef] [PubMed]
- Development of COVID-19 Vaccines. Available online: https://en.wikipedia.org/wiki/Deployment_of_COVID-19_vaccines (accessed on 13 February 2023).
- Coronavirus (COVID-19) Testing. Available online: https://ourworldindata.org/coronavirus-testing (accessed on 1 July 2021).
- Glock, C.H.; Grosse, E.H.; Jaber, M.Y.; Smunt, T.L. Applications of learning curves in production and operations management: A systematic literature review. Comput. Ind. Eng. 2019, 131, 422–441. [Google Scholar] [CrossRef]
- Jaber, M. Learning Curves; CRC Press: Boca Raton, FL, USA, 2016. [Google Scholar]
- Carpenter, S.; Walker, B.; Anderies, J.M.; Abel, N. From metaphor to measurement: Resilience of what to what? Ecosystems 2001, 4, 765–781. [Google Scholar] [CrossRef]
- Gunderson, L.H.; Holling, C.S. Panarchy: Understanding Transformations in Human and Natural Systems; Island Press: Washington, DC, USA, 2002. [Google Scholar]
- Herishanu, Y.; Avivi, I.; Aharon, A.; Shefer, G.; Levi, S.; Bronstein, Y.; Morales, M.; Ziv, T.; Shorer Arbel, Y.; Scarfò, L. Efficacy of the BNT162b2 mRNA COVID-19 vaccine in patients with chronic lymphocytic leukemia. Blood 2021, 137, 3165–3173. [Google Scholar] [CrossRef]
- Sadarangani, M.; Raya, B.A.; Conway, J.M.; Iyaniwura, S.A.; Falcao, R.C.; Colijn, C.; Coombs, D.; Gantt, S. Importance of COVID-19 vaccine efficacy in older age groups. Vaccine 2021, 39, 2020–2023. [Google Scholar] [CrossRef]
- Peltokorpi, J.; Jaber, M.Y. Potential Models of Group Learning in Production. SPS2020 2020, 205–216. [Google Scholar] [CrossRef]
- Carrignon, S.; Bentley, R.A.; Silk, M.; Fefferman, N.H. How social learning shapes the efficacy of preventative health behaviors in an outbreak. PLoS ONE 2022, 17, e0262505. [Google Scholar] [CrossRef] [PubMed]
- Duffey, R.B.; Zio, E. Analysing recovery from pandemics by Learning Theory: The case of COVID-19. IEEE Access 2020, 8, 110789–110795. [Google Scholar] [CrossRef]
- Alkundi, A.; Mahmoud, I.; Musa, A.; Naveed, S.; Alshawwaf, M. Clinical characteristics and outcomes of COVID-19 hospitalized patients with diabetes in the United Kingdom: A retrospective single centre study. Diabetes Res. Clin. Pract. 2020, 165, 108263. [Google Scholar] [CrossRef]
- Rees, E.M.; Nightingale, E.S.; Jafari, Y.; Waterlow, N.R.; Clifford, S.; Pearson, C.A.B.; Group, C.W.; Jombart, T.; Procter, S.R.; Knight, G.M. COVID-19 length of hospital stay: A systematic review and data synthesis. BMC Med. 2020, 18, 270. [Google Scholar] [CrossRef] [PubMed]
- Garcia, P.D.W.; Fumeaux, T.; Guerci, P.; Heuberger, D.M.; Montomoli, J.; Roche-Campo, F.; Schuepbach, R.A.; Hilty, M.P.; Farias, M.A.; Margarit, A. Prognostic factors associated with mortality risk and disease progression in 639 critically ill patients with COVID-19 in Europe: Initial report of the international RISC-19-ICU prospective observational cohort. EClinicalMedicine 2020, 25, 100449. [Google Scholar] [CrossRef] [PubMed]
- Now More Than Ever, We Have to Be Honest about Intensive Care Beds. Available online: https://www.theguardian.com/commentisfree/2020/mar/17/now-more-than-ever-we-have-to-be-honest-about-intensive-care-beds (accessed on 1 August 2021).
- Arrow, K.J. The economic implications of learning by doing. Rev. Econ. Stud. 1962, 29, 155–173. [Google Scholar] [CrossRef]
- Tregoning, J.S.; Flight, K.E.; Higham, S.L.; Wang, Z.; Pierce, B.F. Progress of the COVID-19 vaccine effort: Viruses, vaccines and variants versus efficacy, effectiveness and escape. Nat. Rev. Immunol. 2021, 21, 626–636. [Google Scholar] [CrossRef] [PubMed]
- Shahhosseini, N.; Babuadze, G.G.; Wong, G.; Kobinger, G.P. Mutation Signatures and In Silico Docking of Novel SARS-CoV-2 Variants of Concern. Microorganisms 2021, 9, 926. [Google Scholar] [CrossRef] [PubMed]
- Kupferschmidt, K. New coronavirus variants could cause more reinfections, require updated vaccines. Science 2021. Available online: https://www.science.org/content/article/new-coronavirus-variants-could-cause-more-reinfections-require-updated-vaccines (accessed on 5 May 2023). [CrossRef]
- World Health Organziation. WHO Announces Simple, Easy-to-Say Labels for SARS-CoV-2 Variants of Interest and Concern. 2021. Available online: https://www.who.int/news/item/31-05-2021-who-announces-simple-easy-to-say-labels-for-sars-cov-2-variants-of-interest-and-concern (accessed on 5 May 2023).
- Jain, V.K.; Iyengar, K.; Vaish, A.; Vaishya, R. Differential mortality in COVID-19 patients from India and western countries. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1037–1041. [Google Scholar] [CrossRef]
- How India Could Fill in The Blanks on Excess Mortality. Available online: https://www.bloombergquint.com/coronavirus-outbreak/covid-19-deaths-in-india-how-india-could-fill-in-the-blanks-on-excess-mortality (accessed on 20 July 2020).
- Our World in Data. Coronavirus (COVID-19) Vaccination. 2023. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 22 May 2023).
- Birkmeyer, J.D.; Stukel, T.A.; Siewers, A.E.; Goodney, P.P.; Wennberg, D.E.; Lucas, F.L. Surgeon volume and operative mortality in the United States. N. Engl. J. Med. 2003, 349, 2117–2127. [Google Scholar] [CrossRef]
- Borowski, D.; Bradburn, D.; Mills, S.; Bharathan, B.; Wilson, R.; Ratcliffe, A.; Kelly, S. Volume–outcome analysis of colorectal cancer-related outcomes. J. Br. Surg. 2010, 97, 1416–1430. [Google Scholar] [CrossRef]
- Kulu, Y.; Fathi, P.; Golriz, M.; Khajeh, E.; Sabagh, M.; Ghamarnejad, O.; Mieth, M.; Ulrich, A.; Hackert, T.; Müller-Stich, B.P. Impact of surgeon’s experience on vascular and haemorrhagic complications after kidney transplantation. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 139–149. [Google Scholar] [CrossRef]
- Mi, Y.-N.; Huang, T.-T.; Zhang, J.-X.; Qin, Q.; Gong, Y.-X.; Liu, S.-Y.; Xue, H.-M.; Ning, C.-H.; Cao, L.; Cao, Y.-X. Estimating the instant case fatality rate of COVID-19 in China. Int. J. Infect. Dis. 2020, 97, 1–6. [Google Scholar] [CrossRef] [PubMed]
- China is Promoting Coronavirus Treatments Based on Unproven Traditional Mediciens, Scientists Say Rigorous Trial Data Are Needed to Show that Remedies Are Safe and Effective. Available online: https://www.nature.com/articles/d41586-020-01284-x (accessed on 5 June 2020).
- Pan, X.; Dong, L.; Yang, L.; Chen, D.; Peng, C. Potential drugs for the treatment of the novel coronavirus pneumonia (COVID-19) in China. Virus Res. 2020, 286, 198057. [Google Scholar] [CrossRef] [PubMed]
- Treatments for COVID-19. Available online: https://www.health.harvard.edu/diseases-and-conditions/treatments-for-covid-19 (accessed on 15 July 2021).
- Coronavirus Cure: What Progress Are We Making on Treatments? Available online: https://www.bbc.com/news/health-52354520. (accessed on 15 July 2021).
- Aschwanden, C. Five Reasons Why COVID Herd Immunity Is Probably Impossible. Nature 2021, 591, 520–522. Available online: https://www.nature.com/articles/d41586-021-00728-2 (accessed on 15 April 2021). [CrossRef] [PubMed]
- How Can Supply Keep Up with Demand for COVID-19 Vaccines? Available online: https://www.gavi.org/vaccineswork/how-can-supply-keep-demand-covid-19-vaccines (accessed on 20 July 2021).
- Irwin, A.; Nkengasong, J. What it will take to vaccinate the world against COVID-19. Nature 2021, 592, 176–178. Available online: https://www.nature.com/articles/d41586-021-00727-3 (accessed on 10 April 2021). [CrossRef] [PubMed]
- WHO Says More than 87% of the World’s Covid Vaccine Supply Has Gone to Higher-Income Countries. Available online: https://www.bbc.com/news/world-asia-india-56507988 (accessed on 20 July 2021).
- Coronavirus: “Double Mutant” Covid Variant Found in India. Available online: https://www.npr.org/sections/goatsandsoda/2021/04/24/988744811/people-are-talking-about-a-double-mutant-variant-in-india-what-does-that-mean (accessed on 20 July 2021).
- People Are Talking About A ‘Double Mutant’ Variant In India. What Does That Mean? Available online: https://www.wabe.org/people-are-talking-about-a-double-mutant-variant-in-india-what-does-that-mean/ (accessed on 21 July 2021).
- Rivera, R.; Rosenbaum, J.E.; Quispe, W. Estimating excess deaths in the United States early in the COVID-19 pandemic. medRxiv 2020. [Google Scholar] [CrossRef]
- Gibertoni, D.; Adja, K.Y.C.; Golinelli, D.; Reno, C.; Regazzi, L.; Fantini, M.P. Patterns of COVID-19 related excess mortality in the municipalities of Northern Italy. medRxiv 2020. [Google Scholar] [CrossRef]
- Mannucci, E.; Nreu, B.; Monami, M. Factors associated with increased all-cause mortality during the COVID-19 pandemic in Italy. Int. J. Infect. Dis. 2020, 98, 121–124. [Google Scholar] [CrossRef]
| China | India | UK | Italy | USA | Brazil | |
|---|---|---|---|---|---|---|
| First case | 2019/12/31 | 2020/01/30 | 2020/02/01 | 2020/01/31 | 2020/01/23 | 2020/02/27 |
| First death | 2020/02/02 | 2020/03/14 | 2020/03/07 | 2020/02/23 | 2020/03/03 | 2020/03/19 |
| First vaccination | 2020/12/15 | 2021/01/16 | 2021/01/10 | 2020/12/27 | 2020/12/20 | 2021/01/19 |
| Vaccination rate # | 0.05 | 0.01 | 0.42 | 0.11 | 0.46 | 0.01 |
| China | India | UK | Italy | USA | Brazil | |
|---|---|---|---|---|---|---|
| α | 1.24 × 10−01 | 4.50 × 10−02 *** | 1.04 × 10−01 *** | 8.76 × 10−02 *** | 3.79 × 10−02 *** | 6.79 × 10−02 *** |
| (8.43 × 10−02) | (7.68 × 10−03) | (2.55 × 10−02) | (1.41 × 10−02) | (6.46 × 10−03) | (1.27 × 10−02) | |
| −9.99 × 10−07 | −3.98 × 10−09 *** | −6.04 × 10−08 * | −4.83 × 10−08 ** | −2.18 × 10−09 ** | −8.24 × 10−09 ** | |
| (9.96 × 10−07) | (1.47 × 10−09) | (3.29 × 10−08) | (2.37 × 10−08) | (1.11 × 10−09) | (3.37 × 10−09) | |
| R2 | 0.1566 | 0.2952 | 0.222 | 0.3034 | 0.2952 | 0.2952 |
| Observation number | 46 | 50 | 47 | 45 | 46 | 44 |
| China | India | UK | Italy | USA | Brazil | |
|---|---|---|---|---|---|---|
| α | −8.45 × 10−03 | 1.68 × 10−04 | −6.61 × 10−02 *** | 7.42 × 10−02 *** | −4.57 × 10−02 ** | 3.73 × 10−02 ** |
| (9.94 × 10−02) | (2.38 × 10−02) | (1.53 × 10−02) | (1.85 × 10−02) | 1.84 × 10−02 | (1.27 × 10−02) | |
| 2.17 × 10−07 | 8.43 × 10−10 | 3.10 × 10−08 *** | −1.93 × 10−08 ** | 2.81 × 10−09 *** | −2.11 × 10−09 | |
| (1.02 × 10−06) | (2.25 × 10−09) | (4.88 × 10−09) | (8.52 × 10−09) | 8.01 × 10−10 | (1.48 × 10−09) | |
| −7.34 × 10−04 | −3.73 × 10−04 | −9.66 × 10−04 *** | 6.77 × 10−04 | −3.95 × 10−04 ** | 2.03 × 10−03 | |
| (8.19 × 10−04) | (5.92 × 10−04) | (1.34 × 10−04) | (5.94 × 10−04) | 1.31 × 10−04 | (1.99 × 10−03) | |
| R2 | 0.1292 | 0.1228 | 0.0945 | 0.3034 | 0.462 | 0.8509 |
| Observation number | 17 | 12 | 13 | 15 | 16 | 12 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.-T.; Su, E.C.-Y.; Hung, F.M.; Hiramatsu, T.; Hung, T.-J.; Kuo, C.-Y. Constructing a Learning Curve to Discuss the Medical Treatments and the Effect of Vaccination of COVID-19. Healthcare 2023, 11, 1591. https://doi.org/10.3390/healthcare11111591
Chen Y-T, Su EC-Y, Hung FM, Hiramatsu T, Hung T-J, Kuo C-Y. Constructing a Learning Curve to Discuss the Medical Treatments and the Effect of Vaccination of COVID-19. Healthcare. 2023; 11(11):1591. https://doi.org/10.3390/healthcare11111591
Chicago/Turabian StyleChen, Yi-Tui, Emily Chia-Yu Su, Fang Ming Hung, Tomoru Hiramatsu, Tzu-Jen Hung, and Chao-Yang Kuo. 2023. "Constructing a Learning Curve to Discuss the Medical Treatments and the Effect of Vaccination of COVID-19" Healthcare 11, no. 11: 1591. https://doi.org/10.3390/healthcare11111591
APA StyleChen, Y.-T., Su, E. C.-Y., Hung, F. M., Hiramatsu, T., Hung, T.-J., & Kuo, C.-Y. (2023). Constructing a Learning Curve to Discuss the Medical Treatments and the Effect of Vaccination of COVID-19. Healthcare, 11(11), 1591. https://doi.org/10.3390/healthcare11111591






