Effects of Using a Shoulder/Scapular Brace on the Posture and Muscle Activity of Healthy University Students during Prolonged Typing—A Randomized Controlled Cross-Over Trial
Abstract
1. Introduction
2. Methods
2.1. Participants
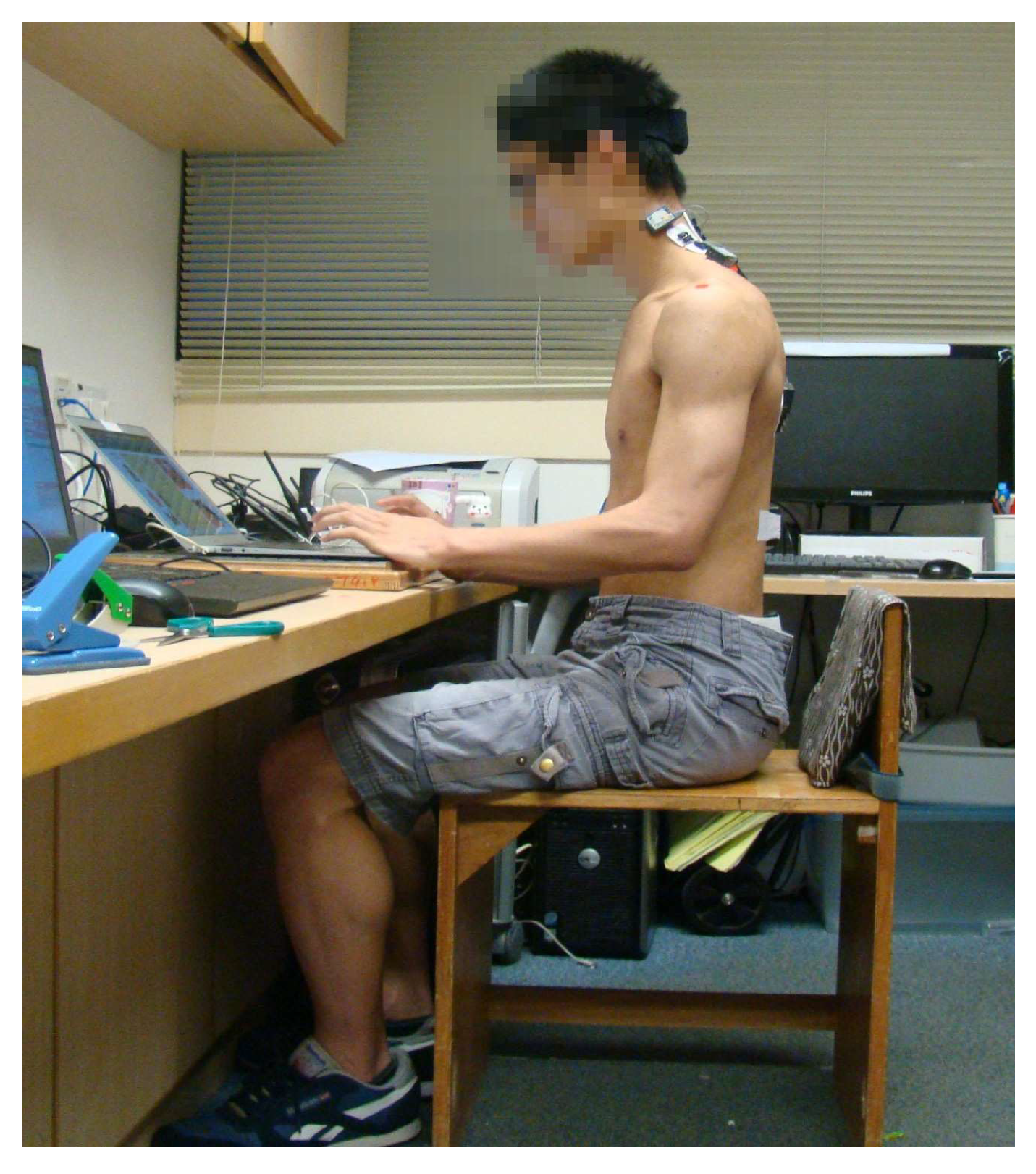
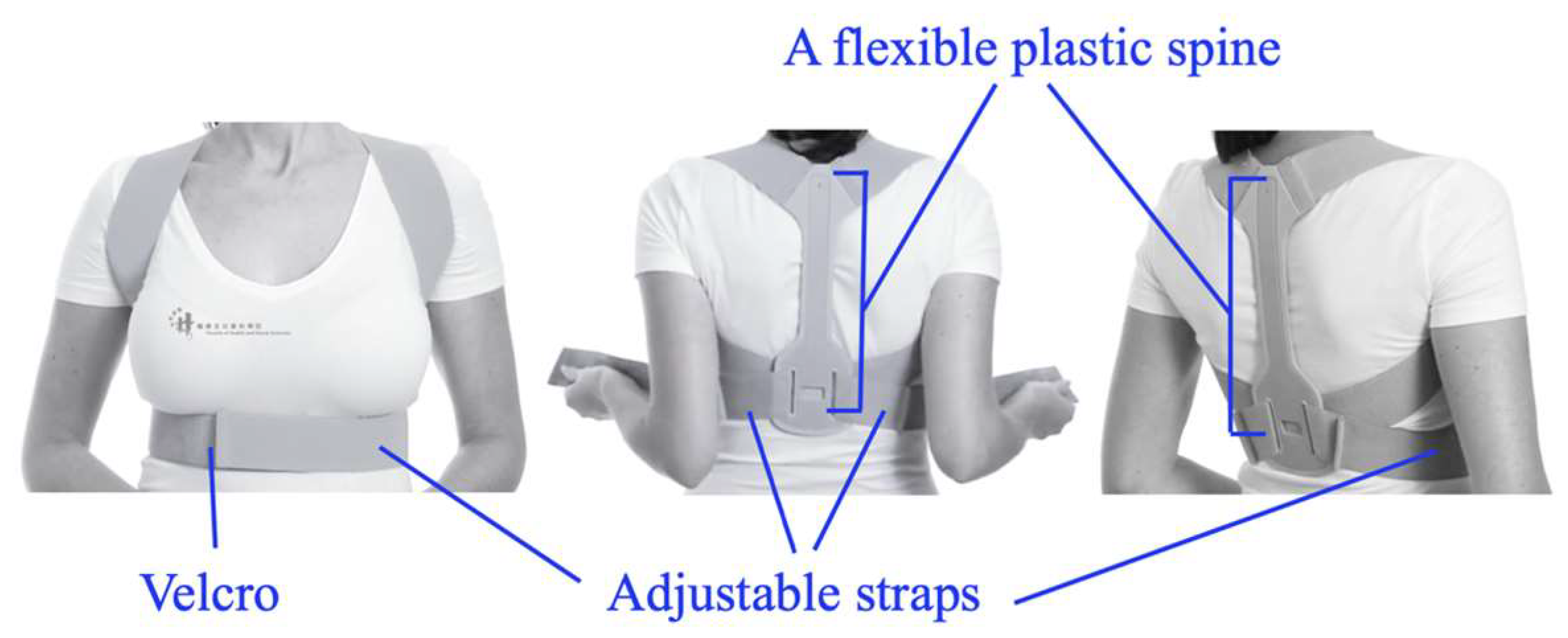
2.2. Experimental Design and Procedure
2.3. Measurements
2.3.1. Subjective Pain and Fatigue
2.3.2. Surface Electromyography (sEMG)
Amplitude
Median Frequency (MF)
2.3.3. IMUs
2.3.4. Digital Photographs
2.4. Statistical Analysis
3. Results
3.1. Subjective Fatigue/Pain Scores
3.2. 50% APDF
3.3. MF Slopes
3.4. IMU Measurements
3.5. FHA and FSA
4. Discussion
4.1. Subjective Neck Pain/Fatigue
4.2. sEMG Activity and APDF
4.3. Motion Analysis, FHA, and FSA
4.4. Limitations and Future Research Directions
4.5. Ergonomic Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, D.; Cho, M.; Park, Y.; Yang, Y. Effect of an exercise program for posture correction on musculoskeletal pain. J. Phys. Ther. Sci. 2015, 27, 1791–1794. [Google Scholar] [CrossRef] [PubMed]
- Hussain, H.M.; Khanzada, S.R.; Khan, K.; Memon, A.U.R.; Feroz, J.; Ali, S.Z.; Khwaja, A. Awareness of good posture and computer ergonomics among medical students of Isra University. Int. J. Physiother. 2015, 2, 987–991. [Google Scholar] [CrossRef]
- Van Nieuwenhuyse, A.; Somville, P.R.; Crombez, G.; Burdorf, A.; Verbeke, G.; Johannik, K.; Van den Bergh, O.; Masschelein, R.; Mairiaux, P.; Moens, G.F. The role of physical workload and pain related fear in the development of low back pain in young workers: Evidence from the BelCoBack Study; results after one year of follow up. Occup. Environ. Environ. Med. 2006, 63, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Chan, L.L.Y.; Wong, A.Y.L.; Wang, M.H.; Cheung, K.; Samartzis, D. The prevalence of neck pain and associated risk factors among undergraduate students: A large-scale cross-sectional study. Int. J. Ind. Ergon. 2020, 76, 102934. [Google Scholar] [CrossRef]
- Kanchanomai, S.; Janwantanakul, P.; Pensri, P.; Jiamjarasrangsi, W. Risk factors for the onset and persistence of neck pain in undergraduate students: 1-year prospective cohort study. BMC Public Health 2011, 11, 566. [Google Scholar] [CrossRef]
- Jenkins, M.; Menéndez, C.C.; Amick, B.C.; Tullar, J.; Hupert, N.; Robertson, M.M.; Katz, J.N. Undergraduate college students’ upper extremity symptoms and functional limitations related to computer use: A replication study. Work 2007, 28, 231–238. [Google Scholar]
- Hupert, N.; Amick, B.C.; Fossel, A.H.; Coley, C.M.; Robertson, M.M.; Katz, J.N. Upper extremity musculoskeletal symptoms and functional impairment associated with computer use among college students. Work 2004, 23, 85–93. [Google Scholar]
- Mahmoud, N.A.; Abu Raddaha, A.H.; Zaghamir, D.E. Impact of Digital Device Use on Neck and Low Back Pain Intensity among Nursing Students at a Saudi Government University: A Cross-Sectional Study. Healthcare 2022, 10, 2424. [Google Scholar] [CrossRef]
- Blyth, F.M.; Briggs, A.M.; Schneider, C.H.; Hoy, D.G.; March, L.M. The Global Burden of Musculoskeletal Pain—Where to From Here? Am. J. Public Health 2018, 109, 35–40. [Google Scholar] [CrossRef]
- Kitiş, A.; Büker, N.; Ünal, A.; Şavkın, R. Effects of musculoskeletal system problems on quality of life and depression in students preparing for university entrance exam. Korean J. Pain. 2017, 30, 192–196. [Google Scholar] [CrossRef]
- Caneiro, J.P.; O’Sullivan, P.; Burnett, A.; Barach, A.; O’Neil, D.; Tveit, O.; Olafsdottir, K. The influence of different sitting postures on head/neck posture and muscle activity. Man. Ther. 2010, 15, 54–60. [Google Scholar] [CrossRef]
- Lee, R.; James, C.; Edwards, S.; Snodgrass, S.J. Posture during the use of electronic devices in people with chronic neck pain: A 3D motion analysis project. Work 2021, 68, 491–505. [Google Scholar] [CrossRef]
- Szeto, G.P.; Straker, L.M.; O’sullivan, P.B. EMG median frequency changes in the neck-shoulder stabilizers of symptomatic office workers when challenged by different physical stressors. J. Electromyogr. Kinesiol. 2005, 15, 544–555. [Google Scholar] [CrossRef]
- Nairn, B.C.; Chisholm, S.R.; Drake, J.D. What is slumped sitting? A kinematic and electromyographical evaluation. Man Ther. 2013, 18, 498–505. [Google Scholar] [CrossRef]
- Shaghayeghfard, B.; Ahmadi, A.; Maroufi, N.; Sarrafzadeh, J. Evaluation of forward head posture in sitting and standing positions. Eur. Spine J. 2016, 25, 3577–3582. [Google Scholar] [CrossRef]
- Choi, J.-H.; Jung, M.-H.; Yoo, K.-T. An analysis of the activity and muscle fatigue of the muscles around the neck under the three most frequent postures while using a smartphone. J. Phys. Ther.Sci. 2016, 28, 1660–1664. [Google Scholar] [CrossRef]
- Karimi, A.; Dianat, I.; Barkhordari, A.; Yusefzade, I.; Rohani-Rasaf, M. A multicomponent ergonomic intervention involving individual and organisational changes for improving musculoskeletal outcomes and exposure risks among dairy workers. Appl. Ergon. 2020, 88, 103159. [Google Scholar] [CrossRef]
- Lee, J.-H.; Cynn, H.-S.; Yoon, T.-L.; Ko, C.-H.; Choi, W.-J.; Choi, S.-A.; Choi, B.-S. The effect of scapular posterior tilt exercise, pectoralis minor stretching, and shoulder brace on scapular alignment and muscles activity in subjects with round-shoulder posture. J. Electromyogr. Kinesiol. 2015, 25, 107–114. [Google Scholar] [CrossRef]
- Cole, A.K.; McGrath, M.L.; Harrington, S.E.; Padua, D.A.; Rucinski, T.J.; Prentice, W.E. Scapular bracing and alteration of posture and muscle activity in overhead athletes with poor posture. J. Athl. Train. 2013, 48, 12–24. [Google Scholar] [CrossRef]
- Lewis, J.S.; Green, A.; Wright, C. Subacromial impingement syndrome: The role of posture and muscle imbalance. J. Shoulder Elb. Surg. 2005, 14, 385–392. [Google Scholar] [CrossRef]
- Chiu, Y.-C.; Tsai, Y.-S.; Shen, C.-L.; Wang, T.-G.; Yang, J.-L.; Lin, J.-J. The immediate effects of a shoulder brace on muscle activity and scapular kinematics in subjects with shoulder impingement syndrome and rounded shoulder posture: A randomized crossover design. Gait Posture 2020, 79, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Borstad, J.D. Resting position variables at the shoulder: Evidence to support a posture-impairment association. Phys. Ther. 2006, 86, 549–557. [Google Scholar] [CrossRef]
- Ko, C.-H.; Cynn, H.-S.; Lee, J.-H.; Yoon, T.-L.; Choi, S.-A. Figure-8 strap application: Immediate alteration of pectoralis minor length and scapular alignment during arm-lifting exercise in participants with forward shoulder posture. J. Sport Rehabil. 2016, 25, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Birmingham, T.B.; Inglis, J.T.; Kramer, J.F.; Vandervoort, A.A. Effect of a neoprene sleeve on knee joint kinesthesis: Influence of different testing procedures. Med. Sci. Sport. Exerc. 2000, 32, 304–308. [Google Scholar] [CrossRef] [PubMed]
- Ulkar, B.; Kunduracioglu, B.; Çetin, C.; Güner, R.S. Effect of positioning and bracing on passive position sense of shoulder joint. Br. J. Sport. Med. 2004, 38, 549–552. [Google Scholar] [CrossRef]
- Uhl, T.L.; Kibler, W.B.; Tripp, B.L.; Spigelman, T.H.; McClelland, R.I. Effects of S3 brace on scapular resting position and kinematics. In Proceedings of the Annual Meeting of the American Orthopaedic Society for Sports Medicine, Chicago, IL, USA, 17–26 March 2006. [Google Scholar]
- Uhl, T.L.; Kibler, W.B.; Tripp, B.L.; Spigelman, T.H.; McClelland, R.I. The effectiveness of a scapular brace on scapular kinematics. In Proceedings of the Annual Conference of the Society of Shoulder and Elbow Therapists, West Palm Beach, FL, USA, 9–12 November 2005; pp. 9–12. [Google Scholar]
- Tanoue, H.; Mitsuhashi, T.; Sako, S.; Goto, R.; Nakai, T.; Inaba, R. Effects of a dynamic chair on pelvic mobility, fatigue, and work efficiency during work performed while sitting: A comparison of dynamic sitting and static sitting. J. Phys. Ther.Sci. 2016, 28, 1759–1763. [Google Scholar] [CrossRef]
- Goda, H.; Hatta, T.; Kishigami, H.; Suzuki, A.; Ikeda, T. Does a Novel-Developed Product of Wheelchair Incorporating Pelvic Support Prevent Forward Head Posture during Prolonged Sitting? PLoS ONE 2015, 10, e0142617. [Google Scholar] [CrossRef]
- Huang, T.-S.; Cheng, W.-C.; Lin, J.-J. Relationship between trapezius muscle activity and typing speed: Taping effect. Ergonomics 2012, 55, 1404–1411. [Google Scholar] [CrossRef]
- Takasaki, H.; Delbridge, B.M.; Johnston, V. Taping across the upper trapezius muscle reduces activity during a standardized typing task—An assessor-blinded randomized cross-over study. J. Electromyogr. Kinesiol. 2015, 25, 115–120. [Google Scholar] [CrossRef]
- Cazzola, M.; MacNee, W.; Martinez, F.J.; Rabe, K.F.; Franciosi, L.G.; Barnes, P.J.; Brusasco, V.; Burge, P.S.; Calverley, P.M.A.; Celli, B.R.; et al. Outcomes for COPD pharmacological trials: From lung function to biomarkers. Eur. Respir. J. 2008, 31, 416–469. [Google Scholar] [CrossRef]
- Herr, K.A.; Spratt, K.; Mobily, P.R.; Richardson, G. Pain intensity assessment in older adults: Use of experimental pain to compare psychometric properties and usability of selected pain scales with younger adults. Clin. J. Pain. 2004, 20, 207–219. [Google Scholar] [CrossRef] [PubMed]
- Morishita, S.; Yamauchi, S.; Fujisawa, C.; Domen, K. Rating of Perceived Exertion for Quantification of the Intensity of Resistance Exercise. Int. J. Phys. Med. Rehabil. 2013, 1, 1–4. [Google Scholar]
- Farrar, J.T.; Young, J.P., Jr.; LaMoreaux, L.; Werth, J.L.; Poole, R.M. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001, 94, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Ries, A.L. Minimally clinically important difference for the UCSD Shortness of Breath Questionnaire, Borg Scale, and Visual Analog Scale. COPD 2005, 2, 105–110. [Google Scholar] [CrossRef]
- Holtermann, A.; Roeleveld, K.; Mork, P.; Grönlund, C.; Karlsson, J.; Andersen, L.; Olsen, H.; Zebis, M.; Sjøgaard, G.; Søgaard, K. Selective activation of neuromuscular compartments within the human trapezius muscle. J. Electromyogr. Kinesiol. 2009, 19, 896–902. [Google Scholar] [CrossRef]
- Mathiassen, S.E.; Winkel, J.; Hägg, G. Normalization of surface EMG amplitude from the upper trapezius muscle in ergonomic studies—A review. J. Electromyogr. Kinesiol. 1995, 5, 197–226. [Google Scholar] [CrossRef]
- Wong, A.Y.; Chan, T.P.; Chau, A.W.; Cheung, H.T.; Kwan, K.C.; Lam, A.K.; Wong, P.Y.; De Carvalho, D. Do different sitting postures affect spinal biomechanics of asymptomatic individuals? Gait Posture 2019, 67, 230–235. [Google Scholar] [CrossRef]
- Umer, W.; Li, H.; Szeto, G.P.Y.; Wong, A.Y.L. Identification of biomechanical risk factors for the development of lower-back disorders during manual rebar tying. J. Constr. Eng. Manag. 2017, 143, 04016080. [Google Scholar] [CrossRef]
- Hu, Y.; Wong, Y.; Lu, W.W.; Kawchuk, G.N. Creation of an asymmetrical gradient of back muscle activity and spinal stiffness during asymmetrical hip extension. Clin. Biomech. 2009, 24, 799–806. [Google Scholar] [CrossRef]
- Smith, S. Digital Signal Processing: A Practical Guide for Engineers and Scientists; Elsevier Science Technology: Oxford, UK, 2013. [Google Scholar]
- Kellis, E.; Katis, A. Reliability of EMG power-spectrum and amplitude of the semitendinosus and biceps femoris muscles during ramp isometric contractions. J. Electromyogr. Kinesiol. 2008, 18, 351–358. [Google Scholar] [CrossRef]
- O’sullivan, P.B.; Grahamslaw, K.M.; Kendell, M.; Lapenskie, S.C.; Möller, N.E.; Richards, K.V. The effect of different standing and sitting postures on trunk muscle activity in a pain-free population. Spine 2002, 27, 1238–1244. [Google Scholar] [CrossRef]
- Perry, M.; Smith, A.; Straker, L.; Coleman, J.; O’Sullivan, P. Reliability of sagittal photographic spinal posture assessment in adolescents. Adv. Physiother. 2008, 10, 66–75. [Google Scholar] [CrossRef]
- Thigpen, C.A.; Padua, D.A.; Michener, L.A.; Guskiewicz, K.; Giuliani, C.; Keener, J.D.; Stergiou, N. Head and shoulder posture affect scapular mechanics and muscle activity in overhead tasks. J. Electromyogr. Kinesiol. 2010, 20, 701–709. [Google Scholar] [CrossRef]
- Talebian, S.; Bagheri, H.; Hosseini, M.; Olyaei, G.R. The Investigation of Median Frequency Changes in Paraspinal Muscles Following Fatigue. Iran. Rehabil. J. 2009, 7, 31–35. [Google Scholar]
- Hsu, Y.-H.; Chen, W.-Y.; Lin, H.-C.; Wang, W.T.; Shih, Y.-F. The effects of taping on scapular kinematics and muscle performance in baseball players with shoulder impingement syndrome. J. Electromyogr. Kinesiol. 2009, 19, 1092–1099. [Google Scholar] [CrossRef]
- Miller, P.; Osmotherly, P. Does scapula taping facilitate recovery for shoulder impingement symptoms? A pilot randomized controlled trial. J. Man. Manip. Ther. 2009, 17, 6E–13E. [Google Scholar] [CrossRef]
- Selkowitz, D.M.; Chaney, C.; Stuckey, S.J.; Vlad, G. The effects of scapular taping on the surface electromyographic signal amplitude of shoulder girdle muscles during upper extremity elevation in individuals with suspected shoulder impingement syndrome. J. Orthop. Sport. Phys. Ther. 2007, 37, 694–702. [Google Scholar] [CrossRef]
- Walther, M.; Werner, A.; Stahlschmidt, T.; Woelfel, R.; Gohlke, F. The subacromial impingement syndrome of the shoulder treated by conventional physiotherapy, self-training, and a shoulder brace: Results of a prospective, randomized study. J. Shoulder Elb. Surg. 2004, 13, 417–423. [Google Scholar] [CrossRef]
- Michener, L.A.; Snyder, A.R.; Leggin, B.G. Responsiveness of the numeric pain rating scale in patients with shoulder pain and the effect of surgical status. J. Sport. Rehabil. 2011, 20, 115–128. [Google Scholar] [CrossRef]
- Szeto, G.P.; Straker, L.M.; O’Sullivan, P.B. During computing tasks symptomatic female office workers demonstrate a trend towards higher cervical postural muscle load than asymptomatic office workers: An experimental study. Aust. J. Physiother. 2009, 55, 257–262. [Google Scholar] [CrossRef]
- Cools, A.M.; Declercq, G.A.; Cambier, D.C.; Mahieu, N.N.; Witvrouw, E.E. Trapezius activity and intramuscular balance during isokinetic exercise in overhead athletes with impingement symptoms. Scand. J. Med. Sci. Sport. 2007, 17, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Diaz, K.M.; Howard, V.J.; Hutto, B.; Colabianchi, N.; Vena, J.E.; Safford, M.M.; Blair, S.N.; Hooker, S.P. Patterns of Sedentary Behavior and Mortality in U.S. Middle-Aged and Older Adults: A National Cohort Study. Ann. Intern. Med. 2017, 167, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Schory, A.; Bidinger, E.; Wolf, J.; Murray, L. A systematic review of the exercises that produce optimal muscle ratios of thescapular stabilizers in normal shoulders. Int. J. Sport. Phys. Ther. 2016, 11, 321–336. [Google Scholar]
- Hirashima, M.; Oya, T. How does the brain solve muscle redundancy? Filling the gap between optimization and muscle synergy hypotheses. Neurosci. Res. 2016, 104, 80–87. [Google Scholar] [CrossRef]
- Johnson, G.; Bogduk, N.; Nowitzke, A.; House, D. Anatomy and actions of the trapezius muscle. Clin. Biomech. 1994, 9, 44–50. [Google Scholar] [CrossRef]
- Balasubramanian, S. Comparsion of Angle Measurements between Vicon and Myomotion Systems. Master’s Thesis, Arizona State University, Tempe, AZ, USA, 23 August 2013. [Google Scholar]
- Straker, L.M.; O’Sullivan, P.B.; Smith, A.J.; Perry, M.C. Relationships between prolonged neck/shoulder pain and sitting spinal posture in male and female adolescents. Man Ther. 2009, 14, 321–329. [Google Scholar] [CrossRef]
- Mohamed, M.A.; Radwan, N.L. Optimal Work-Rest Schedule for Computer Users. Int. J. Physiother. 2017, 4, 71–76. [Google Scholar] [CrossRef]
- Luger, T.; Mathiassen, S.E.; Bosch, T.; Hoozemans, M.; Douwes, M.; Veeger, D.; De Looze, M. Influence of Posture Variation on Shoulder Muscle Activity, Heart Rate, and Perceived Exertion in a Repetitive Manual Task. IISE Trans. Occup. Ergon. Hum. Factors 2017, 5, 47–64. [Google Scholar] [CrossRef]
- De Carvalho, D.E.; de Luca, K.; Funabashi, M.; Breen, A.; Wong, A.Y.; Johansson, M.S.; Ferreira, M.L.; Swab, M.; Kawchuk, G.N.; Adams, J.; et al. Association of exposures to seated postures with immediate increases in back pain: A systematic review of studies with objectively measured sitting time. J. Manip. Physiol. Ther. 2020, 43, 1–12. [Google Scholar] [CrossRef]

| Testing Order | EMG Electrode Landmarks | MVIC Positioning |
|---|---|---|
| 1. Cervical Erector Spinae (CES) | 2 cm lateral from the C4 spinous process | A participant sat with arms by the side of the body and performed maximal neck extension against manual resistance at the back of the head, applied by an examiner. |
| 2. Upper Trapezius (UT) | Midway between the mastoid process and root of the spine of scapula | A participant sat with arms beside the body, and then performed maximal shrugging of shoulders against an examiners’ downward resistance applied to the acromion. |
| 3. Lower Trapezius (LT) | 2 finger-widths medial to the inferior angle of the scapula, at a 45° angle towards the T10 spinous process | A participant in prone lying with arms lifted overhead, in line with lower trapezius muscle fiber orientation. The participant raised the arms towards the ceiling using maximal effort against the examiner’s downward force applied just distal to the humeroulnar joint line. |
| Motion Sensor Location | Regional Angle |
|---|---|
| Back of Head + C7 | Cervical Spine |
| C7 + T12 | Thoracic Spine |
| T12 + S2 | Lumbar Spine |
| Brace | No Brace | Between-Condition Cohen’s d | |||
|---|---|---|---|---|---|
| Mean ± SE | 95% CI | Mean ± SE | 95% CI | ||
| Mean NPRS scores | |||||
| Pre-trial | 0.30 ± 0.15 * | 0.003, 0.60 | 0.23 ± 0.11 * | 0.0004, 0.47 | 0.06 |
| Post-trial | 1.07 ± 0.29 * | 0.48, 1.65 | 1.03 ± 0.26 * | 0.51, 1.56 | |
| Mean RPE scores | |||||
| Pre-trial | 0.67 ± 0.20 * | 0.26, 1.07 | 0.47 ± 0.16 * | 0.13, 0.80 | 0.16 |
| Post-trial | 2.50 ± 0.40 * | 1.69, 3.31 | 2.90 ± 0.40 * | 2.09, 3.71 | |
| Brace | No Brace | Between-Condition Cohen’s d | |||
|---|---|---|---|---|---|
| Mean ± SE | 95% CI | Mean ± SE | 95% CI | ||
| %MVIC at 50% APDF | |||||
| Left erector spinae | 10.98 ± 1.15 | 10.57, 11.39 | 11.52 ± 1.48 | 10.99, 12.05 | 0.07 |
| Right erector spinae | 12.17 ± 1.82 | 11.52, 12.82 | 12.18 ± 2.08 | 11.44, 12.92 | 0.02 |
| Left upper trapezius | 1.68 ± 0.17 | 1.62, 1.74 | 1.71 ± 0.21 | 1.63, 1.79 | 0.02 |
| Right upper trapezius | 2.19 ± 0.36 | 2.06, 2.32 | 2.17 ± 0.33 | 2.05, 2.29 | 0.01 |
| Left lower trapezius | 3.74 ± 0.54 * | 3.55, 3.93 | 4.25 ± 0.57 * | 4.05, 4.45 | 0.07 |
| Right lower trapezius | 4.15 ± 0.49 * | 3.97, 4.33 | 4.81 ± 0.59 * | 4.60, 5.02 | 0.06 |
| Brace | No Brace | Between-Condition Cohen’s d | |||
|---|---|---|---|---|---|
| Mean ± SE | 95% CI | Mean ± SE | 95% CI | ||
| Slope of median frequency (%) | |||||
| Left cervical erector spinae | −0.051 ± 0.131 | −0.320, 0.218 | 0.449 ± 0.167 | 0.108, 0.790 | 0.61 |
| Right cervical erector spinae | 0.068 ± 0.086 | −0.168, 0.182 | 0.072 ± 0.057 | −0.045, 0.189 | 0.16 |
| Left upper trapezius | 0.179 ± 0.096 | −0.017, 0.375 | 0.116 ± 0.074 | −0.036, 0.268 | 0.13 |
| Right upper trapezius | −0153 ± 0.087 | −0.331, 0.025 | −0.088 ± 0.088 | −0.269, 0.092 | 0.14 |
| Left lower trapezius | 0.379 ± 0.296 | −0.226, 0.984 | 0.199 ± 0.102 | −0.091, 0.408 | 0.15 |
| Right lower trapezius | 0.065 ± 0.071 | −0.079, 0.209 | 0.036 ± 0.079 | −0.125, 0.197 | 0.07 |
| Brace | No-Brace | Between-Condition Cohen’s d | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1st minute | 15th minute | 30th minute | 1st minute | 15th minute | 30th minute | ||||||||
| Mean ± SE | 95% CI | Mean ± SE | 95% CI | Mean ± SE | 95% CI | Mean ± SE | 95% CI | Mean ± SE | 95% CI | Mean ± SE | 95% CI | ||
| IMU Measurements | |||||||||||||
| Cervical spine | 8.7 ± 1.6 | 5.5, 12.0 | 8.7 ± 1.6 | 5.4, 12.0 | 7.5 ± 1.6 | 4.2, 10.9 | 8.6 ± 1.4 * | 5.8, 11.4 | 6.2 ± 1.6 * | 3.0, 9.5 | 7.3 ± 1.4 | 4.4, 10.2 | 0.12 |
| Thoracic spine | 2.5 ± 1.2 | −0.3, 5.0 | 4.5 ± 1.4 | 1.7, 7.4 | 4.7 ± 1.3 | 5.2, 7.3 | 4.2 ± 0.7 | 2.7, 5.7 | 7.0 ± 0.9 | 5.1, 8.9 | 6.5 ± 0.9 | 4.6, 8.3 | 0.02 |
| Lumbar spine | 2.4 ± 7.5 | −6.3, 24.4 | 0.1 ± 1.5 | −2.2, 3.9 | 6.5 ± 1.0 | −1.6, 2.3 | 1.6 ± 1.0 | -4.3, 3.7 | 2.5 ± 1.6 | −7.2, 5.8 | 1.8 ± 1.7 | −1.6, 5.2 | 0.05 |
| Digital Photograph Measurements | |||||||||||||
| Forward head angle | 51.0 ± 1.2 | 48.6, 53.5 | 52.7 ± 1.3 | 50.2, 55.3 | 52.8 ± 1.5 | 49.8, 55.9 | 50.6 ± 1.1 | 48.3, 52.9 | 51.3 ± 1.1 | 49.0, 53.5 | 52.6 ± 1.3 | 50.0, 55.3 | 0.03 |
| Forward shoulder angle | 45.5 ± 3.3 | 38.7, 52.4 | 46.0 ±3.6 | 38.8, 53.2 | 45.4 ± 3.6 | 38.1, 52.8 | 52.0 ± 2.7 | 46.6, 57.4 | 52.3 ± 2.7 | 47.2, 58.3 | 51.6 ± 2.8 | 45.9, 57.4 | 0.12 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leung, M.; Kan, M.M.P.; Cheng, H.M.H.; De Carvalho, D.E.; Anwer, S.; Li, H.; Wong, A.Y.L. Effects of Using a Shoulder/Scapular Brace on the Posture and Muscle Activity of Healthy University Students during Prolonged Typing—A Randomized Controlled Cross-Over Trial. Healthcare 2023, 11, 1555. https://doi.org/10.3390/healthcare11111555
Leung M, Kan MMP, Cheng HMH, De Carvalho DE, Anwer S, Li H, Wong AYL. Effects of Using a Shoulder/Scapular Brace on the Posture and Muscle Activity of Healthy University Students during Prolonged Typing—A Randomized Controlled Cross-Over Trial. Healthcare. 2023; 11(11):1555. https://doi.org/10.3390/healthcare11111555
Chicago/Turabian StyleLeung, Melissa, Mandy M. P. Kan, Hugo M. H. Cheng, Diana E. De Carvalho, Shahnawaz Anwer, Heng Li, and Arnold Y. L. Wong. 2023. "Effects of Using a Shoulder/Scapular Brace on the Posture and Muscle Activity of Healthy University Students during Prolonged Typing—A Randomized Controlled Cross-Over Trial" Healthcare 11, no. 11: 1555. https://doi.org/10.3390/healthcare11111555
APA StyleLeung, M., Kan, M. M. P., Cheng, H. M. H., De Carvalho, D. E., Anwer, S., Li, H., & Wong, A. Y. L. (2023). Effects of Using a Shoulder/Scapular Brace on the Posture and Muscle Activity of Healthy University Students during Prolonged Typing—A Randomized Controlled Cross-Over Trial. Healthcare, 11(11), 1555. https://doi.org/10.3390/healthcare11111555









