Modeling Consumer Acceptance and Usage Behaviors of m-Health: An Integrated Model of Self-Determination Theory, Task–Technology Fit, and the Technology Acceptance Model
Abstract
1. Introduction
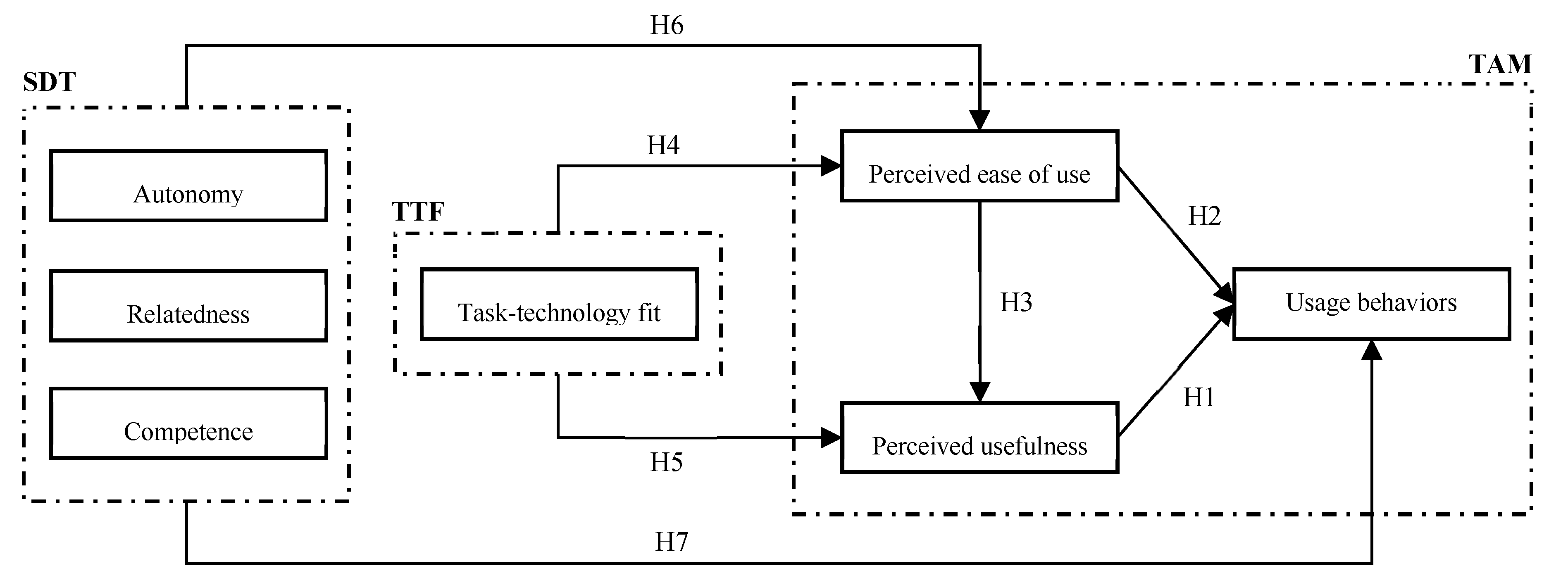
2. Theoretical Background and Research Hypotheses
2.1. Technology Acceptance Model
2.2. Task–Technology Fit Model
2.3. Self-Determination Theory of Motivation
2.3.1. Autonomy
2.3.2. Relatedness
2.3.3. Competence
3. Methods
3.1. Participants
3.2. Instruments
3.3. Data Analysis
4. Results
4.1. Reliability and Validity Assessment
4.2. Model Testing
4.3. Multi-Group SEM Analysis
5. Discussion
6. Conclusions
6.1. Implications
6.2. Limitations and Future Work
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Measurement Items and Sources of the Constructs Examined in the Model
| Constructs | Items | Sources |
| Autonomy | AUT1: I would have more control of my health management while using m-health services. | [45] |
| AUT2: The m-health services give me more chances to control my health management. | ||
| AUT3: The m-health services provide me with more opportunities to control my health management. | ||
| Relatedness | REL1: The m-health services give me more chances to interact with others. | [45] |
| REL2: I feel close to others while using m-health services. | ||
| REL3: I have more opportunities to be close to others while using m-health services. | ||
| Competence | COM1: I am better than others in using m-health services. | [45] |
| COM2: I have a stronger capability than others in using m-health services. | ||
| COM3: I am better than others in using m-health services. | ||
| Task–technology fit | TTF1: The m-health services are fit for the requirements of my health management. | [42] |
| TTF2: Using m-health services fits with my health management practice. | ||
| TTF3: The functions in m-health services fit with my health management. | ||
| TTF4: The m-health services are suitable for helping me with my health management. | ||
| Perceived usefulness | PU1: Using m-health services improves my health management performance. | [35] |
| PU2: Using m-health services increases my productivity in my health management. | ||
| PU3: Using m-health services enhances my effectiveness in my health management. | ||
| PU4: I find m-health services to be useful in my health management. | ||
| Perceived ease of use | PEOU1: My interaction with m-health services is clear and understandable. | [35] |
| PEOU2: Interaction with m-health services does not require a lot of mental effort. | ||
| PEOU3: I find m-health services to be easy to use. | ||
| PEOU4: It is easy to use m-health services to do what I want. | ||
| Usage behaviors | UB1: When I can use m-health services for health management, I always use it. | [22] |
| UB2: I often use m-health services to manage my health. | ||
| UB3: I use m-health services as much as I should. |
References
- Statista. Global digital population as of October 2020. Available online: https://www.statista.com/statistics/617136/digital-populationworldwide/ (accessed on 4 April 2023).
- Sun, L.; Buijsen, M. Mobile Health in China: Well Integrated or a New Divide? Camb. Q. Healthc. Ethics 2023, 32, 244–253. [Google Scholar] [CrossRef]
- Tao, D.; Wang, T.; Wang, T.; Zhang, T.; Zhang, X.; Qu, X. A systematic review and meta-analysis of user acceptance of consumer-oriented health information technologies. Comput. Hum. Behav. 2020, 104, 106147. [Google Scholar] [CrossRef]
- Tao, D.; Wang, T.; Wang, T.; Liu, S.; Qu, X. Effects of consumer-oriented health information technologies in diabetes management over time: A systematic review and meta-analysis of randomized controlled trials. J. Am. Med. Inform. Assoc. 2017, 24, 1014–1023. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liu, K.; Tao, D. The roles of trust, personalization, loss of privacy, and anthropomorphism in public acceptance of smart healthcare services. Comput. Hum. Behav. 2022, 127, 107026. [Google Scholar] [CrossRef]
- Wang, H.; Zhang, J.; Luximon, Y.; Qin, M.; Geng, P.; Tao, D. The determinants of user acceptance of mobile medical platforms: An investigation integrating the TPB, TAM, and patient-centered factors. Int. J. Environ. Res. Public Health 2022, 19, 10758. [Google Scholar] [CrossRef]
- Anwar, M.; Joshi, J.; Tan, J. Anytime, anywhere access to secure, privacy-aware healthcare services: Issues, approaches and challenges. Health Policy Technol. 2015, 4, 299–311. [Google Scholar] [CrossRef]
- Jin, X.; Yuan, Z.; Zhou, Z. Understanding the Antecedents and Effects of mHealth App Use in Pandemics: A Sequential Mixed-Method Investigation. Int. J. Environ. Res. Public Health 2023, 20, 834. [Google Scholar] [CrossRef] [PubMed]
- Madrigal, L.E.C. Electronic health behaviors among US adults with chronic disease: Cross-sectional survey. J. Med. Internet Res. 2019, 21, e11240. [Google Scholar] [CrossRef]
- Research2guidance. Diabetes App Market Report; 2014. Available online: https://research2guidance.com/top-14-diabetes-app-publishers-capture-65-market-share-of-the-diabetes-app-market-2/ (accessed on 19 August 2022).
- Deng, Z.M.X.; Liu, S. Comparison of the middle-aged and older users’ adoption of mobile health services in China. Int. J. Med. Inform. 2014, 83, 210–224. [Google Scholar] [CrossRef]
- Zhang, X.; Guo, X.; Lai, K.H.; Guo, F.; Li, C. Understanding gender differences in m-health adoption: A modified theory of reasoned action model. Telemed. E-Health 2014, 20, 39–46. [Google Scholar] [CrossRef]
- Gao, Y.; Li, H.; Luo, Y. An empirical study of wearable technology acceptance in healthcare. Ind. Manag. Data Syst. 2015, 115, 1704–1723. [Google Scholar] [CrossRef]
- Cho, J. The impact of post-adoption beliefs on the continued use of health apps. Int. J. Med. Inform. 2016, 87, 75–83. [Google Scholar] [CrossRef]
- Hoque, R.; Sorwar, G. Understanding factors influencing the adoption of mHealth by the elderly: An extension of the UTAUT model. Int. J. Med. Inform. 2017, 101, 75–84. [Google Scholar] [CrossRef]
- Zhu, Z.; Liu, Y.; Che, X.; Chen, X. Moderating factors influencing adoption of a mobile chronic disease management system in China. Inform. Health Soc. Care 2018, 43, 22–41. [Google Scholar] [CrossRef]
- Zhang, X.; Han, X.; Dang, Y.; Meng, F.; Guo, X.; Lin, J. User acceptance of mobile health services from users’ perspectives: The role of self-efficacy and response-efficacy in technology acceptance. Inform. Health Soc. Care 2017, 42, 194–206. [Google Scholar] [CrossRef]
- Cilliers, L.; Viljoen, K.L.-A.; Chinyamurindi, W.T. A study on students’ acceptance of mobile phone use to seek health information in South Africa. Health Inf. Manag. J. 2018, 47, 59–69. [Google Scholar] [CrossRef]
- Nunes, A.L.T.; Castro, S.L. Acceptance of mobile health applications: Examining key determinants and moderators. Front. Psychol. 2019, 10, 2791. [Google Scholar] [CrossRef] [PubMed]
- Alaiad, A.; Alsharo, M.; Alnsour, Y. The determinants of m-health adoption in developing countries: An empirical investigation. Appl. Clin. Inform. 2019, 10, 820–840. [Google Scholar] [CrossRef] [PubMed]
- Lu, F.; Wang, X.; Huang, X. Counseling for Health: How Psychological Distance Influences Continuance Intention towards Mobile Medical Consultation. Int. J. Environ. Res. Public Health 2023, 20, 1718. [Google Scholar] [CrossRef]
- Or, C.K.; Karsh, B.T.; Severtson, D.J.; Burke, L.J.; Brown, R.L.; Brennan, P.F. Factors affecting home care patients' acceptance of a web-based interactive self-management technology. J. Am. Med. Inform. Assoc. 2011, 18, 51–59. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Calegari, L.P.; RD, B.; Fettermann, D.C. A meta-analysis of a comprehensive m-health technology acceptance. Int. J. Lean Six Sigma, 2023; ahead of print. [Google Scholar] [CrossRef]
- Wang, H.; Tao, D.; Yu, N.; Qu, X. Understanding consumer acceptance of healthcare wearable devices: An integrated model of UTAUT and TTF. Int. J. Med. Inform. 2020, 139, 104156. [Google Scholar] [CrossRef]
- Lee, W.-I.; Fu, H.-P.; Mendoza, N.; Liu, T.-Y. Determinants Impacting User Behavior towards Emergency Use Intentions of m-Health Services in Taiwan. Healthcare 2021, 9, 535. [Google Scholar] [CrossRef] [PubMed]
- Debon, R.; Coleone, J.D.; Bellei, E.A.; Bertoletti De Marchi, A.C. Mobile health applications for chronic diseases: A systematic review of features for lifestyle improvement. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 2507–2512. [Google Scholar] [CrossRef] [PubMed]
- Deci, E.L.; Ryan, R.M. The general causality orientations scale: Self-determination in personality. J. Res. Personal. 1985, 19, 109–134. [Google Scholar] [CrossRef]
- Alsyouf, A.; Lutfi, A.; Al-Bsheish, M.; Jarrar, M.T.; Al-Mugheed, K.; Almaiah, M.A.; Alhazmi, F.N.; Masa’deh, R.E.; Anshasi, R.J.; Ashour, A. Exposure detection applications acceptance: The case of COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 7307. [Google Scholar] [CrossRef]
- Cao, J.; Zhang, G.; Liu, D. The Impact of Using mHealth Apps on Improving Public Health Satisfaction during the COVID-19 Pandemic: A Digital Content Value Chain Perspective. Healthcare 2022, 10, 479. [Google Scholar] [CrossRef]
- Chuenyindee, T.; Ong, A.K.S.; Prasetyo, Y.T.; Persada, S.F.; Nadlifatin, R.; Sittiwatethanasiri, T. Factors affecting the perceived usability of the COVID-19 contact-tracing application “Thai chana” during the early COVID-19 omicron period. Int. J. Environ. Res. Public Health 2022, 19, 4383. [Google Scholar] [CrossRef] [PubMed]
- Alsyouf, A.; Lutfi, A.; Alsubahi, N.; Alhazmi, F.N.; Al-Mugheed, K.; Anshasi, R.J.; Alharbi, N.I.; Albugami, M. The use of a Technology Acceptance Model (TAM) to predict patients’ usage of a personal health record system: The role of security, privacy, and usability. Int. J. Environ. Res. Public Health 2023, 20, 1347. [Google Scholar] [CrossRef]
- Goodhue, D.L.; Thompson, R.L. Task-technology fit and individual performance. MIS Q. 1995, 19, 213–236. [Google Scholar] [CrossRef]
- Marikyan, D.; Papagiannidis, S.; Alamanos, E. “Smart home sweet smart home”: An examination of smart home acceptance. Int. J. E-Bus. Res. 2021, 17, 1–23. [Google Scholar] [CrossRef]
- Or, C.; Tao, D. Usability study of a computer-based self-management system for older adults with chronic diseases. JMIR Res. Protoc. 2012, 1, e2184. [Google Scholar] [CrossRef] [PubMed]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef][Green Version]
- Zhang, T.; Tao, D.; Qu, X.; Zhang, X.; Zeng, J.; Zhu, H.; Zhu, H. Automated vehicle acceptance in China: Social influence and initial trust are key determinants. Transp. Res. Part C Emerg. Technol. 2020, 112, 220–233. [Google Scholar] [CrossRef]
- Cheng, M.; Yuen, A.H.K. Junior secondary students’ acceptance and continuance of e-learning system use: A multi-group analysis across social backgrounds. Behav. Inf. Technol. 2020, 41, 324–347. [Google Scholar] [CrossRef]
- Tao, D.; Shao, F.; Wang, H.; Yan, M.; Qu, X. Integrating usability and social cognitive theories with the technology acceptance model to understand young users’ acceptance of a health information portal. Health Inform. J. 2019, 26, 1347–1362. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User acceptance of computer technology: A comparison of two theoretical models. Manag. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef][Green Version]
- Zhang, T.; Tao, D.; Qu, X.; Zhang, X.; Lin, R.; Zhang, W. The roles of initial trust and perceived risk in public’s acceptance of automated vehicles. Transp. Res. Part C Emerg. Technol. 2019, 98, 207–220. [Google Scholar] [CrossRef]
- Wu, B.; Chen, X. Continuance intention to use MOOCs: Integrating the technology acceptance model (TAM) and task technology fit (TTF) model. Comput. Hum. Behav. 2017, 67, 221–232. [Google Scholar] [CrossRef]
- Yu, T.K.; Yu, T.Y. Modelling the factors that affect individuals’ utilisation of online learning systems: An empirical study combining the task technology fit model with the theory of planned behaviour. Br. J. Educ. Technol. 2010, 41, 1003–1017. [Google Scholar] [CrossRef]
- Liu, K.; Yao, J.; Tao, D.; Yang, T. Influence of individual-technology-task-environment fit on university student online learning performance: The mediating role of behavioral, emotional, and cognitive engagement. Educ. Inf. Technol. 2023, 1–20. [Google Scholar] [CrossRef]
- Tao, D.; Li, W.; Qin, M.; Cheng, M. Understanding students’ acceptance and usage behaviors of online learning in mandatory contexts: A three-wave longitudinal study during the COVID-19 pandemic. Sustainability 2022, 14, 7830. [Google Scholar] [CrossRef]
- Grolnick, W.S.; Deci, E.L.; Ryan, R.M. Internalization within the family: The self-determination theory perspective. In Parenting and Children’s Internalization of Values: A Handbook of Contemporary Theory; Grusec, J.E., Kuczynski, L., Eds.; Wiley: New York, NY, USA, 1997; pp. 135–161. [Google Scholar]
- Ryan, R.M.; Deci, E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2000, 55, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Fathali, S.; Okada, T. Technology acceptance model in technology-enhanced OCLL contexts: A self-determination theory approach. Australas. J. Educ. Technol. 2018, 34, 138–154. [Google Scholar] [CrossRef][Green Version]
- Nikou, S.A.; Economides, A.A. Mobile-Based Assessment: Integrating acceptance and motivational factors into a combined model of Self-Determination Theory and Technology Acceptance. Comput. Hum. Behav. 2017, 68, 83–95. [Google Scholar] [CrossRef]
- Liaw, S.S.; Huang, H.M.; Chen, G.D. An activity-theoretical approach to investigate learners’ factors toward e-learning systems. Comput. Hum. Behav. 2007, 23, 1906–1920. [Google Scholar] [CrossRef]
- Roca, J.C.; Gagné, M. Understanding e-learning continuance intention in the workplace: A self-determination theory perspective. Comput. Hum. Behav. 2008, 24, 1585–1604. [Google Scholar] [CrossRef]
- Khan, I.U.; Hameed, Z.; Yu, Y.; Islam, T.; Sheikh, Z.; Khan, S.U. Predicting the acceptance of MOOCs in a developing country: Application of task-technology fit model, social motivation, and self-determination theory. Telemat. Inform. 2018, 35, 964–978. [Google Scholar] [CrossRef]
- DeVellis, R.F.; Thorpe, C.T. Scale Development: Theory and Applications; Sage publications: Newbury Park, CA, USA, 2021. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Cangur, S.; Ercan, I. Comparison of model fit indices used in structural equation modeling under multivariate normality. J. Mod. Appl. Stat. Methods 2015, 14, 152–167. [Google Scholar] [CrossRef][Green Version]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Heine, S.J. An exploration of cultural variation in self-enhancing and self-improving motivations. In Cross-Cultural Differences in Perspectives on the Self; Volume 49 of the Nebraska symposium on motivation; University of Nebraska Press: Lincoln, NE, USA, 2003; pp. 118–145. [Google Scholar]
- Tseng, V. Family interdependence and academic adjustment in college: Youth from immigrant and US-born families. Child Dev. 2004, 75, 966–983. [Google Scholar] [CrossRef] [PubMed]
- Vansteenkiste, M.; Zhou, M.; Lens, W.; Soenens, B. Experiences of autonomy and control among Chinese learners: Vitalizing or immobilizing? J. Educ. Psychol. 2005, 97, 468. [Google Scholar] [CrossRef][Green Version]
- Tao, D.; Fu, P.; Wang, Y.; Zhang, T.; Qu, X. Key characteristics in designing massive open online courses (MOOCs) for user acceptance: An application of the extended technology acceptance model. Interact. Learn. Environ. 2022, 30, 882–895. [Google Scholar] [CrossRef]

| Study | Country | Type of m-Health | Sample Size | Theory Base | Factors Examined in the Model (Significant Factors Are Emboldened) |
| Zhang et al., 2014 [12] | China | M-health service | 481 | TRA | ATT, FC, SN, and gender |
| Deng et al., 2014 [11] | China | M-health service | 424 | TAM, TPB, and value–attitude–behavior model | ATT, PBC, perceived value, RC, SN, TA, self-actualization need, perceived physical condition, and age |
| Gao et al., 2015 [13] | China | Wearable healthcare technology | 462 | UTAUT2, protection motivation theory, and privacy calculus theory | PEOU, PU, PPR, SI, self-efficacy, perceived severity, and perceived vulnerability |
| Cho, 2016 [14] | Korea | Mobile health Apps | 343 | TAM | PEOU, PU, and confirmation |
| Hoque and Sorwar, 2017 [15] | Bangladesh | M-health services | 274 | UTAUT | PEOU, PU, SI, RC, TA, and FC |
| Zhu et al., 2017 [16] | China | Mobile chronic disease management systems | 279 | TAM | PEOU, PU, TA, perceived disease threat, initial trust, and perceived risk |
| Zhang et al., 2017 [17] | China | M-health services | 650 | TAM | PEOU, PU, self-efficacy, and response-efficacy |
| Cilliers et al., 2018 [18] | South Africa | Mobile phone-based health information | 202 | UTAUT | PU, ATT, SI, and mobile experience |
| Alaiad et al., 2019 [20] | Jordan | M-health services | 280 | UTAUT, dual-factor model, and health belief model | PEOU, PU, SI, RC, perceived health threat, m-health app quality, life quality expectancy, security, and privacy risks |
| Nunes and Castro, 2019 [19] | Portugal | Mobile health applications | 394 | UTAUT | PEOU, PU, SI, FC, age, smartphone experience, and gender |
| Liu and Tao, 2022 [5] | China | Smart healthcare services | 769 | TAM | PEOU, PU, trust, personalization, loss of privacy, and anthropomorphism |
| Wang et al., 2022 [6] | China | Mobile medical platforms | 389 | TAM, TPB | PEOU, PU, ATT, PBC, PPR, SI, perceived convenience, and perceived credibility |
| Alsyouf et al., 2022 [28] | Saudi Arabia | Exposure detection apps | 586 | TAM | PEOU, PU, perceived privacy, and social media awareness |
| Cao et al., 2022 [29] | China | M-health Apps | 500 | Digital content value chain framework | User–functional interaction, user–information interaction, user–doctor interaction, healthcare assurance capacity, healthcare confidence, and parasocial relationships |
| Chuenyindee et al., 2022 [30] | Thailand | COVID-19 contact-tracing application | 800 | TAM and protection motivation theory | PEOU and PU |
| Lu et al., 2023 [21] | China | Mobile medical consultation | 475 | Information systems continuance model | Immediacy, telepresence, intimacy, substitutability, pandemic-induced anxiety, and satisfaction |
| Alsyouf et al., 2023 [31] | Saudi Arabia | Personal health record system | 389 | TAM | PEOU, PU, security, privacy, and usability |
| Items | Classification | Number of Participants | Percentage (%) |
|---|---|---|---|
| Gender | Male | 266 | 42.7% |
| Female | 357 | 57.3% | |
| Age | 18–29 | 302 | 48.5% |
| 30 or above | 321 | 51.5% | |
| Education | High school or less | 23 | 3.7% |
| University/college | 547 | 87.8% | |
| Postgraduate | 53 | 8.5% | |
| Duration of using m-health | Less than 3 years | 403 | 64.7% |
| 3 years or more | 220 | 35.3% | |
| Frequency of using m-health | Yearly | 352 | 56.5% |
| Monthly | 207 | 33.2% | |
| Weekly | 56 | 9% | |
| Daily | 8 | 1.3% | |
| Main purpose of using m-health | Online healthcare consultation | 302 | 48.5% |
| Appointment registration | 83 | 13.3% | |
| Medical/health information inquiry | 112 | 18% | |
| Self-monitoring of health status | 70 | 11.2% | |
| Purchase of medication | 10 | 1.6% | |
| Comprehensive health management | 46 | 7.4% |
| Constructs | Items | Factor Loadings | Cronbach’s α | Composite Reliability | Average Variance Extracted (AVE) |
|---|---|---|---|---|---|
| Autonomy | AUT1 | 0.82 | 0.66 | 0.82 | 0.61 |
| AUT2 | 0.81 | ||||
| AUT3 | 0.70 | ||||
| Relatedness | REL1 | 0.80 | 0.82 | 0.89 | 0.74 |
| REL2 | 0.89 | ||||
| REL3 | 0.89 | ||||
| Competence | COM1 | 0.84 | 0.86 | 0.91 | 0.78 |
| COM2 | 0.92 | ||||
| COM3 | 0.89 | ||||
| Task–technology fit | TTF1 | 0.75 | 0.72 | 0.83 | 0.55 |
| TTF2 | 0.74 | ||||
| TTF3 | 0.78 | ||||
| TTF4 | 0.70 | ||||
| Perceived usefulness | PU1 | 0.78 | 0.72 | 0.83 | 0.55 |
| PU2 | 0.66 | ||||
| PU3 | 0.78 | ||||
| PU4 | 0.73 | ||||
| Perceived ease of use | PEOU1 | 0.77 | 0.76 | 0.85 | 0.59 |
| PEOU2 | 0.75 | ||||
| PEOU3 | 0.78 | ||||
| PEOU4 | 0.76 | ||||
| Usage behaviors | UB1 | 0.80 | 0.75 | 0.86 | 0.67 |
| UB2 | 0.81 | ||||
| UB3 | 0.85 |
| AUT | REL | COM | TTF | PEOU | PU | UB | |
|---|---|---|---|---|---|---|---|
| AUT | 0.78 | ||||||
| REL | 0.42 ** | 0.86 | |||||
| COM | 0.36 ** | 0.35 ** | 0.88 | ||||
| TTF | 0.66 ** | 0.42 ** | 0.40 ** | 0.74 | |||
| PEOU | 0.46 ** | 0.34 ** | 0.32 ** | 0.51 ** | 0.77 | ||
| PU | 0.61 ** | 0.42 ** | 0.34 ** | 0.63 ** | 0.54 ** | 0.74 | |
| UB | 0.53 ** | 0.31 ** | 0.29 ** | 0.51 ** | 0.54 ** | 0.62 ** | 0.82 |
| Model Fit Indices | Recommended Value | Tested Model |
|---|---|---|
| χ2/df | <3.0 | 2.76 |
| GFI | >0.9 | 0.92 |
| AGFI | >0.8 | 0.90 |
| CFI | >0.9 | 0.93 |
| IFI | >0.9 | 0.93 |
| TLI | >0.9 | 0.91 |
| RMSEA | <0.08 | 0.05 |
| Hypotheses | Path | Path Coefficient (β) | Standard Deviation | t Value | p Value | Supported? (Yes/No) |
|---|---|---|---|---|---|---|
| H1 | PU→UB | 0.619 *** | 4.143 | 4.507 | <0.001 | Yes |
| H2 | PEOU→UB | 0.243 ** | 2.221 | 2.973 | 0.003 | Yes |
| H3 | PEOU→PU | 0.319 *** | 1.348 | 5.267 | <0.001 | Yes |
| H4 | TTF→PEOU | 0.427 | 6.889 | 1.566 | 0.117 | No |
| H5 | TTF→PU | 0.657 *** | 1.647 | 9.050 | <0.001 | Yes |
| H6a | AUT→PEOU | 0.161 | 9.385 | 0.579 | 0.562 | No |
| H6b | REL→PEOU | 0.137 * | 0.899 | 2.195 | 0.028 | Yes |
| H6c | COM→PEOU | 0.130 * | 0.824 | 2.418 | 0.016 | Yes |
| H7a | AUT→UB | 0.118 | 3.894 | 1.109 | 0.267 | No |
| H7b | REL→UB | −0.022 | 0.749 | −0.474 | 0.636 | No |
| H7c | COM→UB | 0.008 | 0.749 | 0.170 | 0.865 | No |
| Hypotheses | Whole | Gender | Age | Usage Experience | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male (N = 266) | Female (N = 357) | Z Score | Younger Users (N = 302) | Middle-Aged Users (N = 321) | Z Score | Less Experienced Users (N = 403) | More Experienced Users (N = 220) | Z Score | ||
| H1: PU→UB | 0.619 *** | 0.745 ** | 0.382 * | −1.978 * | 0.591 * | 0.565 * | −0.032 | 0.614 *** | 0.4 | −0.544 |
| H2: PEOU→UB | 0.243 ** | −0.046 | 0.326 * | 1.707 | 0.291 | 0.28 * | −0.470 | 0.24 ** | 0.368 * | 0.566 |
| H3: PEOU→PU | 0.319 *** | 0.343 *** | 0.288 *** | −0.206 | 0.419 *** | 0.292 *** | −1.777 | 0.281 *** | 0.46 *** | 0.960 |
| H4: TTF→PEOU | 0.427 | 0.564 | 0.31 | −0.639 | 0.516 | 0.277 | −0.187 | 0.819 | 0.221 | −0.775 |
| H5: TTF→PU | 0.657 *** | 0.68 *** | 0.688 *** | −0.228 | 0.561 *** | 0.691 *** | 0.997 | 0.663 *** | 0.561 *** | −0.655 |
| H6a: AUT→PEOU | 0.161 | 0.056 | 0.271 | 0.415 | 0.13 | 0.273 | 0.297 | −0.28 | 0.468 | 0.985 |
| H6b: REL→PEOU | 0.137 * | 0.1 | 0.188 ** | 0.405 | 0.163 | 0.127 | 0.113 | 0.197 * | 0.048 | −1.199 |
| H6c: COM→PEOU | 0.13 * | 0.147 * | 0.076 | −0.953 | 0.15 | 0.099 | −0.198 | 0.126 | 0.117 | −0.162 |
| H7a: AUT→UB | 0.118 | −0.705 | 0.214 | 2.120 * | 0.091 | 0.174 | 0.294 | 0.15 | 0.177 | 0.040 |
| H7b: REL→UB | −0.022 | 0.091 | −0.023 | −0.951 | 0.037 | 0.134 * | −1.831 | −0.033 | −0.027 | 0.100 |
| H7c: COM→UB | 0.008 | −0.014 | 0.037 | 0.518 | −0.012 | −0.011 | 0.013 | −0.024 | 0.042 | 0.673 |
| R2 (overall model) | 81.1% | 83.2% | 86.4% | 83.5% | 83.7% | 82.1% | 76.5% | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tao, D.; Chen, Z.; Qin, M.; Cheng, M. Modeling Consumer Acceptance and Usage Behaviors of m-Health: An Integrated Model of Self-Determination Theory, Task–Technology Fit, and the Technology Acceptance Model. Healthcare 2023, 11, 1550. https://doi.org/10.3390/healthcare11111550
Tao D, Chen Z, Qin M, Cheng M. Modeling Consumer Acceptance and Usage Behaviors of m-Health: An Integrated Model of Self-Determination Theory, Task–Technology Fit, and the Technology Acceptance Model. Healthcare. 2023; 11(11):1550. https://doi.org/10.3390/healthcare11111550
Chicago/Turabian StyleTao, Da, Zhixi Chen, Mingfu Qin, and Miaoting Cheng. 2023. "Modeling Consumer Acceptance and Usage Behaviors of m-Health: An Integrated Model of Self-Determination Theory, Task–Technology Fit, and the Technology Acceptance Model" Healthcare 11, no. 11: 1550. https://doi.org/10.3390/healthcare11111550
APA StyleTao, D., Chen, Z., Qin, M., & Cheng, M. (2023). Modeling Consumer Acceptance and Usage Behaviors of m-Health: An Integrated Model of Self-Determination Theory, Task–Technology Fit, and the Technology Acceptance Model. Healthcare, 11(11), 1550. https://doi.org/10.3390/healthcare11111550







