Functional Status of Patients over 65 Years Old Intervened on for a Hip Fracture One Year after the Operation
Abstract
1. Introduction
2. Materials and Methods
2.1. Procedure
2.2. Assessment at the Admission
2.3. Discharge Evaluation
2.4. Status at One Year
2.5. Statistical Analysis
3. Results
3.1. Information at Admission
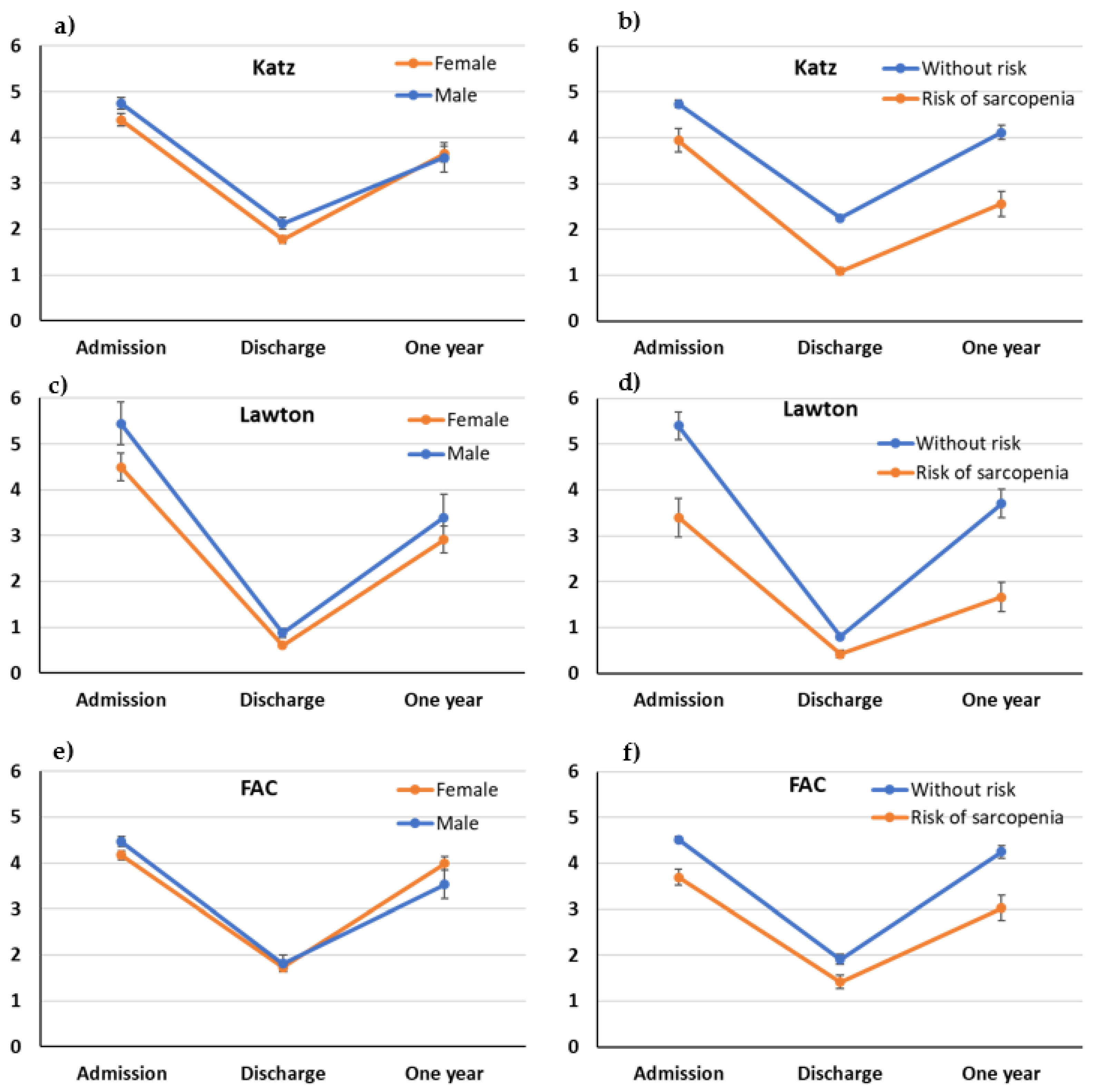
3.2. Follow-up Study Based on the Risk of Sarcopenia
3.3. Functional Status at One Year
4. Discussion
Status One Year after the Surgery
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dong, Y.; Zhang, Y.; Song, K.; Kang, H.; Ye, D.; Li, F. What was the Epidemiology and Global Burden of Disease of Hip Fractures From 1990 to 2019? Results From and Additional Analysis of the Global Burden of Disease Study 2019. Clin. Orthop. Relat. Res. 2022, 481, 1209–1220. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-P.; Kuo, Y.-J.; Hung, S.-W.; Wen, T.-W.; Chien, P.-C.; Chiang, M.-H.; Maffulli, N.; Lin, C.-Y. Loss of skeletal muscle mass can be predicted by sarcopenia and reflects poor functional recovery at one year after surgery for geriatric hip fractures. Injury 2021, 52, 3446–3452. [Google Scholar] [CrossRef] [PubMed]
- Mayoral, A.P.; Ibarz, E.; Gracia, L.; Mateo, J.; Herrera, A. The use of Barthel index for the assessment of the functional recovery after osteoporotic hip fracture: One year follow-up. PLoS ONE 2019, 14, e0212000. [Google Scholar] [CrossRef]
- Steihaug, O.M.; Gjesdal, C.G.; Bogen, B.; Kristoffersen, M.H.; Lien, G.; Ranhoff, A.H. Sarcopenia in patients with hip fracture: A multicenter cross-sectional study. PLoS ONE 2017, 12, e0184780. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E.; Abbatecola, A.M.; Argiles, J.M.; Baracos, V.; Bauer, J.; Bhasin, S.; Cederholm, T.; Coats, A.J.S.; Cummings, S.R.; Evans, W.J.; et al. Sarcopenia with Limited Mobility: An International Consensus. J. Am. Med. Dir. Assoc. 2011, 12, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Ledesma, I.J. Sarcopenia y desempeño ocupacional de las actividades básicas de la vida diaria en mayores institucionalizados. Rev. Astur. Ter. Ocup. 2015, 22–29. [Google Scholar]
- Vetrano, D.L.; Landi, F.; Volpato, S.; Corsonello, A.; Meloni, E.; Bernabei, R.; Onder, G. Association of Sarcopenia with Short- and Long-term Mortality in Older Adults Admitted to Acute Care Wards: Results from the CRIME Study. J. Gerontol. Ser. A 2014, 69, 1154–1161. [Google Scholar] [CrossRef]
- Rosenberg, I.H. Sarcopenia: Origins and clinical relevance. Clin. Geriatr. Med. 2011, 27, 337–339. [Google Scholar] [CrossRef]
- Yeung, S.S.Y.; Reijnierse, E.M.; Pham, V.K.; Trappenburg, M.C.; Lim, W.K.; Meskers, C.G.M.; Maier, A.B. Sarcopenia and its association with falls and fractures in older adults: A systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle 2019, 10, 485–500. [Google Scholar] [CrossRef]
- Bischoff-Ferrari, H.A.; Orav, J.E.; Kanis, J.A.; Rizzoli, R.; Schlögl, M.; Staehelin, H.B.; Willett, W.C. Comparative performance of current definitions of sarcopenia against the prospective incidence of falls among community-dwelling seniors age 65 and older. Osteoporos. Int. 2015, 26, 2793–2802. [Google Scholar] [CrossRef]
- Malmstrom, T.K.; Miller, D.K.; Simonsick, E.M.; Ferrucci, L.; Morley, J.E. SARC-F: A symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J. Cachexia Sarcopenia Muscle 2016, 7, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Messina, C.; Albano, D.; Gitto, S.; Tofanelli, L.; Bazzocchi, A.; Ulivieri, F.M.; Guglielmi, G.; Sconfienza, L.M. Body composition with dual energy X-ray absorptiometry: From basics to new tools. Quant. Imaging Med. Surg. 2020, 10, 1687–1698. [Google Scholar] [CrossRef]
- Lauretani, F.; Ticinesi, A.; Gionti, L.; Prati, B.; Nouvenne, A.; Tana, C.; Meschi, T.; Maggio, M. Short-Physical Performance Battery (SPPB) score is associated with falls in older outpatients. Aging Clin. Exp. Res. 2019, 31, 1435–1442. [Google Scholar] [CrossRef]
- Martinez, B.P.; Gomes, I.B.; de Oliveira, C.S.; Ramos, I.R.; Rocha, M.D.M.; Júnior, L.A.F.; Camelier, F.W.R.; Camelier, A.A. Accuracy of the Timed Up and Go test for predicting sarcopenia in elderly hospitalized patients. Clinics 2015, 70, 369–372. [Google Scholar] [CrossRef] [PubMed]
- Mijnarends, D.M.; Luiking, Y.C.; Halfens, R.J.G.; Evers, S.M.A.A.; Lenaerts, E.L.A.; Verlaan, S.; Wallace, M.; Schols, J.M.G.A.; Meijers, J.M.M. Muscle, Health and Costs: A Glance at their Relationship. J. Nutr. Health Aging 2018, 22, 766–773. [Google Scholar] [CrossRef] [PubMed]
- Cawthon, P.M.; Lui, L.-Y.; Taylor, B.C.; Mcculloch, C.E.; Cauley, J.A.; Lapidus, J.; Orwoll, E.; Ensrud, K.E. Clinical Definitions of Sarcopenia and Risk of Hospitalization in Community-Dwelling Older Men: The Osteoporotic Fractures in Men Study. J. Gerontol. Ser. A 2017, 72, 1383–1389. [Google Scholar] [CrossRef]
- Chang, C.-D.; Wu, J.S.; Ni Mhuircheartaigh, J.; Hochman, M.G.; Rodriguez, E.K.; Appleton, P.T.; Mcmahon, C.J. Effect of sarcopenia on clinical and surgical outcome in elderly patients with proximal femur fractures. Skelet. Radiol. 2018, 47, 771–777. [Google Scholar] [CrossRef]
- Maresova, P.; Javanmardi, E.; Barakovic, S.; Husic, J.B.; Tomsone, S.; Krejcar, O.; Kuca, K. Consequences of chronic diseases and other limitations associated with old age—A scoping review. BMC Public Health 2019, 19, S170–S182. [Google Scholar] [CrossRef]
- Sidney, K.; Ford, A.B.; Moskowitz, R.W.; Jackson, B.A.; Jaffe, M.W. Studies of illness in the aged: The index of ADL: A standardized measure of biological and psychosocial function. JAMA 1963, 185, 914–919. [Google Scholar]
- Isik, E.I.; Yilmaz, S.; Uysal, I.; Basar, S. Adaptation of the Lawton Instrumental Activities of Daily Living Scale to Turkish: Validity and Reliability Study. Ann. Geriatr. Med. Res. 2020, 24, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Elord, C.; Corrêa, F.I.; Pereira, G.S.; Silva, S.M.; Corrêa, J.C. Translation into Brazilian Portuguese, cross-cultural adaptation, reliability and validation of the Functional Ambulation Classification for the categorization of ambulation following a stroke in a clinical setting. Rev. Neurol. 2020, 70, 365–371. [Google Scholar]
- Teigão, F.C.M.; de Lima Moser, A.D.; Jerez-Roig, J. Translation and cross-cultural adaptation of Pfeiffer’s Short Portable Mental Status Questionnaire (SPMSQ) for brazilians older adults. Rev. Bras. Geriatr. Gerontol. 2021, 23. [Google Scholar] [CrossRef]
- Ida, S.; Kaneko, R.; Murata, K. SARC-F for Screening of Sarcopenia Among Older Adults: A Meta-analysis of Screening Test Accuracy. J. Am. Med. Dir. Assoc. 2018, 19, 685–689. [Google Scholar] [CrossRef]
- Ha, Y.-C.; Won, C.W.; Kim, M.; Chun, K.-J.; Yoo, J.-I. SARC-F as a Useful Tool for Screening Sarcopenia in Elderly Patients with Hip Fractures. J. Nutr. Health Aging 2019, 24, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Inouye, S.K.; van Dyck, C.H.; Alessi, C.A.; Balkin, S.; Siegal, A.P.; Horwitz, R.I. Clarifying confusion: The confusion assessment method: A new method for detection of delirium. Ann. Intern. Med. 1990, 113, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Bahat, G.; Erdoğan, T.; İlhan, B. SARC-F and other screening tests for sarcopenia. Curr. Opin. Clin. Nutr. Metab. Care 2022, 25, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Meskers, C.; Reijnierse, E.M.; Numans, S.T.; Kruizinga, R.C.; Pierik, V.D.; van Ancum, J.M.; Slee-Valentijn, M.; Scheerman, K.; Verlaan, S.; Maier, A.B. Association of handgrip strength and muscle mass with dependency in (instrumental) activities of daily living in hospitalized older adults-the EMPOWER study. J. Nutr. Health Aging 2019, 23, 232–238. [Google Scholar] [CrossRef]
- Wu, T.-Y.; Liaw, C.-K.; Chen, F.-C.; Kuo, K.-L.; Chie, W.-C.; Yang, R.-S. Sarcopenia Screened With SARC-F Questionnaire Is Associated with Quality of Life and 4-Year Mortality. J. Am. Med. Dir. Assoc. 2016, 17, 1129–1135. [Google Scholar] [CrossRef]
- Xu, W.; Chen, T.; Cai, Y.; Hu, Y.; Fan, L.; Wu, C. Sarcopenia in Community-Dwelling Oldest Old is Associated with Disability and Poor Physical Function. J. Nutr. Health Aging 2020, 24, 339–345. [Google Scholar] [CrossRef]
- Landi, F.; Calvani, R.; Ortolani, E.; Salini, S.; Martone, A.M.; Santoro, L.; Santoliquido, A.; Sisto, A.; Picca, A.; Marzetti, E. The association between sarcopenia and functional outcomes among older patients with hip fracture undergoing in-hospital rehabilitation. Osteoporos. Int. 2017, 28, 1569–1576. [Google Scholar] [CrossRef] [PubMed]
- Di Monaco, M.; Castiglioni, C.; Vallero, F.; Di Monaco, R.; Tappero, R. Sarcopenia is more prevalent in men than in women after hip fracture: A cross-sectional study of 591 inpatients. Arch. Gerontol. Geriatr. 2012, 55, e48–e52. [Google Scholar] [CrossRef] [PubMed]
- Iranzo, M.A.C.I.; Arnal-Gómez, A.; Tortosa-Chuliá, M.A.; Balasch-Bernat, M.; Forcano, S.; Sentandreu-Mañó, T.; Tomas, J.M.; Cezón-Serrano, N. Functional and clinical characteristics for predicting sarcopenia in institutionalised older adults: Identifying tools for clinical screening. Int. J. Environ. Res. Public Health 2020, 17, 4483. [Google Scholar] [CrossRef] [PubMed]
- Tanimoto, Y.; Watanabe, M.; Sun, W.; Sugiura, Y.; Tsuda, Y.; Kimura, M.; Hayashida, I.; Kusabiraki, T.; Kono, K. Association between sarcopenia and higher-level functional capacity in daily living in community-dwelling elderly subjects in Japan. Arch. Gerontol. Geriatr. 2012, 55, e9–e13. [Google Scholar] [CrossRef]
- Wearing, J.; Konings, P.; De Bie, R.A.; Stokes, M.; De Bruin, E.D. Prevalence of probable sarcopenia in community-dwelling older Swiss people—A cross-sectional study. BMC Geriatr. 2020, 20, 307. [Google Scholar] [CrossRef]
- Fernández, S.S.; Muñoz, A.C.; Sanz, G.L.; Hernandez, B.M.; Marco, M.A.M.; Lampré, P.M. Preliminary Evidence on the Effectiveness of a Multidisciplinary Nutritional Support for Older People with Femur Fracture at an Orthogeriatric Unit in Spain. J. Nutr. Gerontol. Geriatr. 2022, 41, 270–293. [Google Scholar] [CrossRef] [PubMed]
- Roche-Albero, A.; Cassinello-Ogea, C.; Martín-Hernández, C. Factors of presenting an acute confusional syndrome after a hip fracture. Injury 2021, 52, S54–S60. [Google Scholar] [CrossRef]
- Lim, S.-K.; Beom, J.; Lee, S.Y.; Lim, J.-Y. Functional Outcomes of Fragility Fracture Integrated Rehabilitation Management in Sarcopenic Patients after Hip Fracture Surgery and Predictors of Independent Ambulation. J. Nutr. Health Aging 2019, 23, 1034–1042. [Google Scholar] [CrossRef]
- Steihaug, O.M.; Gjesdal, C.G.; Bogen, B.; Kristoffersen, M.H.; Lien, G.; Hufthammer, K.O.; Ranhoff, A.H. Does sarcopenia predict change in mobility after hip fracture? A multicenter observational study with one-year follow-up. BMC Geriatr. 2018, 18, 65. [Google Scholar] [CrossRef]
- Kristensen, M.T.; Kehlet, H. Most patients regain prefracture basic mobility after hip fracture surgery in a fast-track programme. Dan. Med. J. 2012, 59, A4447. [Google Scholar]
- Gherardini, S.; Biricolti, C.; Benvenuti, E.; Almaviva, M.G.; Lombardi, M.; Pezzano, P.; Bertini, C.; Baccini, M.; Di Bari, M. Prognostic Implications of Predischarge Assessment of Gait Speed After Hip Fracture Surgery. J. Geriatr. Phys. Ther. 2019, 42, 148–152. [Google Scholar] [CrossRef] [PubMed]
- Duke, R.G.; Keating, J.L. An investigation of factors predictive of independence in transfers and ambulation after hip fracture. Arch. Phys. Med. Rehabil. 2002, 83, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Heiden Jace, J.; Goodin Stephen, R.; Mormino Matthew, A.; Siebler Justin, C.; Putnam Sara, M.; Lyden Elizabeth, R.; Tao Matthew, A. Early ambulation after hip fracture surgery is associated with decreased 30-day mortali-ty. JAAOS-J. Am. Acad. Orthop. Surg. 2021, 29, e238–e242. [Google Scholar] [CrossRef]
- Dufournet, M.; the MEMORA group; Moutet, C.; Achi, S.; Delphin-Combe, F.; Krolak-Salmon, P.; Dauphinot, V. Proposition of a corrected measure of the Lawton instrumental activities of daily living score. BMC Geriatr. 2021, 21, 39. [Google Scholar] [CrossRef] [PubMed]
- Ravensbergen, W.M.; Timmer, I.L.; Gussekloo, J.; Blom, J.W.; van Eijk, M.; Achterberg, W.P.; Evers, A.W.M.; van Dijk, S.; Drewes, Y.M. Self-perceived functioning and (instrumental) activities of daily living questionnaires after a hip fracture: Do they tell the same story? Age Ageing 2022, 51, afac259. [Google Scholar] [CrossRef]
| Risk of Sarcopenia | p-Value | ||
|---|---|---|---|
| Yes (Sarc-F ≥ 4) (n = 48) | No (Sarc-F < 4) (n = 87) | ||
| Age, years | 84.1 ± 6.7 | 80.2 ± 7.8 | 0.005 |
| Female, n (%) | 40 (83) | 57 (65) | 0.030 |
| Body mass index, kg/m2 | 26.7 ± 4.9 | 26.9 ± 4.1 | 0.850 |
| Type of fracture, n (%) | 0.263 | ||
| Intracapsular | 18 (37) | 39 (45) | |
| Subtrochanteric | 9 (19) | 8 (9) | |
| Pertrochanteric | 21 (44) | 40 (46) | |
| Osteosynthesis material, n (%) | 0.905 | ||
| Nail | 30 (63) | 52 (60) | |
| Partial prosthesis | 16 (33) | 30 (34) | |
| Total prosthesis | 2 (4) | 5 (6) | |
| Charlson index | 5.3 ± 1.6 | 4.5 ± 1.3 | 0.003 |
| Delirium | 5 (10) | 5 (6) | 0.326 |
| Number of physiotherapy sessions | 6.3 ± 3.4 | 4.9 ± 3.1 | 0.017 |
| Days of hospital stay | 16.1 ± 8.7 | 12.9 ± 6.7 | 0.020 |
| Patient location before, n (%) | 0.721 | ||
| Home | 44 (92) | 82 (94) | |
| Elderly residence | 4 (8) | 5 (6) | |
| Patient location after, n (%) | 0.250 | ||
| Home | 36 (77) | 76 (87) | |
| Social health centre | 5 (10) | 6 (7) | |
| Elderly residence | 6 (13) | 5 (6) | |
| Functional tests | |||
| Katz | |||
| Average ± s.d. | 4.1 ± 1.4 | 4.8 ± 0.7 | <0.001 |
| Katz, n (%) | 0.003 | ||
| Severe disability (0–2) | 7 (15) | 2 (2) | |
| Moderate disability (3–4) | 14 (29) | 15 (17) | |
| Mild or no disability (5–6) | 27 (56) | 70 (81) | |
| Lawton | |||
| Average ± s.d. | 3.6 ± 2.5 | 5.5 ± 2.6 | <0.001 |
| Median (P25; P75) | 4 (1; 5.8) | 6.0 (3.2; 8) | <0.001 |
| Lawton, n (%) | 0.001 | ||
| Severe dependence (0–2) | 20 (42) | 15 (17) | |
| Mild dependence (3–5) | 16 (33) | 24 (28) | |
| Independence (6–8) | 12 (25) | 48 (55) | |
| FAC | |||
| Average ± s.d. | 3.8 ± 0.9 | 4.5 ± 0.6 | <0.001 |
| FAC, n (%) | <0.001 | ||
| Walking with aid (0–1) | 2 (4) | - | |
| Supervised walking (2–3) | 12 (25) | 4 (5) | |
| Independent walking (4–5) | 34 (71) | 83 (95) | |
| Cognitive Impairment | |||
| Pfeiffer | |||
| Average ± s.d. | 4.7 ± 2.4 | 3.5 ± 2.5 | 0.008 |
| Median (P25; P75) | 5 (3; 7) | 3 (1; 5) | 0.007 |
| Pfeiffer, n (%) | 0.098 | ||
| No impairment (0–2) | 11 (23) | 34 (39) | |
| Mild impairment (3–4) | 10 (21) | 23 (26) | |
| Moderate impairment (5–7) | 21 (44) | 23 (26) | |
| Severe impairment (8–10) | 6 (12) | 7 (8) | |
| p-Value * | ||||||
|---|---|---|---|---|---|---|
| Admission | Discharge | One Year | Time (Linear; Quadratic) | Time * Sex | Time * Sarc-F | |
| Katz, points | (0.077; <0.001) | 0.118 | 0.008 | |||
| Sarc-F < 4 | 4.7 ± 0.7 | 1.9 ± 0.9 | 4.1 ± 1.3 | |||
| Sarc-F (≥4) | 3.9 ± 1.5 | 1.4 ± 0.8 | 2.6 ± 1.6 | |||
| Katz, n (%) | (0.001; <0.001) | 0.282 | 0.084 | |||
| Sarc-F < 4 | ||||||
| Severe disability | 2 (3) | 61 (79) | 12 (16) | |||
| Moderate disability | 14 (18) | 15 (20) | 21 (27) | |||
| Mild or no disability | 61 (79) | 1 (1) | 44 (57) | |||
| Sarc-F (≥4) | ||||||
| Severe disability | 7 (19) | 31 (86) | 19 (53) | |||
| Moderate disability | 10 (28) | 5 (14) | 11 (30) | |||
| Mild or no disability | 19 (53) | - | 6 (17) | |||
| Lawton, points | (0.032; <0.001) | 0.001 | 0.012 | |||
| Sarc-F < 4 | ||||||
| Average ± s.d. | 5.4 ± 2.6 | 0.8 ± 0.5 | 3.7 ± 2.7 | |||
| Median (P25; P75) | 6 (3.1; 8) | 1 (1; 1) | 4 (1; 6) | |||
| Sarc-F (≥4) | ||||||
| Average ± s.d. | 3.4 ± 2.5 | 0.4 ± 0.5 | 1.7 ± 1.9 | |||
| Median (P25; P75) | 3 (1; 5.8) | 0 (0; 1) | 1 (0; 2) | |||
| Lawton, n (%) | (0.041; <0.001) | 0.099 | 0.001 | |||
| Sarc-F < 4 | ||||||
| Severe dependence | 14 (18) | 77 (100) | 31 (40) | |||
| Mild dependence | 21 (27) | - | 25 (33) | |||
| Independence | 42 (55) | - | 21 (27) | |||
| Sarc-F (≥4) | ||||||
| Severe dependence | 16 (44) | 36 (100) | 28 (78) | |||
| Mild dependence | 11 (31) | - | 5 (14) | |||
| Independence | 9 (25) | - | 3 (8) | |||
| FAC, points | (0.394; 0.035) | 0.001 | 0.183 | |||
| Sarc-F < 4 | 4.5 ± 0.6 | 2.3 ± 0.6 | 4.3 ± 1.2 | |||
| Sarc-F (≥4) | 3.7 ± 1.0 | 1.1 ± 0.4 | 3.0 ± 1.6 | |||
| FAC, n (%) | (0.002; 0.003) | 0.022 | 0.215 | |||
| Sarc-F < 4 | ||||||
| Walking with aid | - | 5 (6) | 5 (7) | |||
| Supervised walking | 4 (5) | 72 (94) | 11 (14) | |||
| Independent walking | 73 (95) | - | 61 (79) | |||
| Sarc-F (≥4) | ||||||
| Walking with aid | 2 (5) | 31 (86) | 8 (22) | |||
| Supervised walking | 10 (28) | 5 (14) | 9 (25) | |||
| Independent walking | 24 (67) | - | 19 (53) | |||
| Coefficient | s.e. | t | p-Value | |
|---|---|---|---|---|
| Katz | <0.001 | |||
| Constant | 4.436 | 0.238 | 18.633 | <0.001 |
| Sarc-F (≥4) | −1.392 | 0.283 | −4.921 | <0.001 |
| Delirium | −1.014 | 0.543 | −1.866 | 0.065 |
| Pfeiffer (ref. no impairment) | ||||
| Mild impairment (3–4) | 0.002 | 0.338 | 0.006 | 0.995 |
| Moderate impairment (5–7) | −0.675 | 0.332 | −2.031 | 0.045 |
| Severe impairment (8–10) | −1.111 | 0.471 | −2.357 | 0.020 |
| Lawton | <0.001 | |||
| Constant | 13.718 | 2.063 | 6.649 | <0.001 |
| Sarc-F (≥4) | −1.237 | 0.426 | −2.906 | 0.004 |
| Delirium | −1.950 | 0.804 | −3.670 | <0.001 |
| Age | −0.110 | 0.026 | −4.204 | <0.001 |
| Pfeiffer (ref. no impairment) | ||||
| Mild impairment (3–4) | −1.216 | 0.503 | −2.417 | 0.017 |
| Moderate impairment (5–7) | −2.209 | 0.495 | −4.463 | <0.001 |
| Severe impairment (8–10) | −2.332 | 0.720 | −3.239 | 0.002 |
| FAC | <0.001 | |||
| Constant | 4.715 | 0.249 | 18.940 | <0.001 |
| Sarc-F (≥4) | −1.224 | 0.263 | −4.649 | <0.001 |
| Delirium | −1.342 | 0.504 | −2.662 | 0.009 |
| Sex (Male) | −0.843 | 0.275 | −3.068 | 0.003 |
| Pfeiffer (ref. no impairment) | ||||
| Mild impairment (3–4) | 0.186 | 0.312 | 0.596 | 0.553 |
| Moderate impairment (5–7) | −0.417 | 0.305 | −1.371 | 0.173 |
| Severe impairment (8–10) | −0.707 | 0.353 | −2.160 | 0.036 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marrero-Morales, P.A.; González-Dávila, E.; Hernández-Gutiérrez, M.F.; Gallego-González, E.M.; Jiménez-Hernández, M.; Sanz-Álvarez, E.J.; Rodríguez-Novo, N.; Rodríguez-Novo, Y.M. Functional Status of Patients over 65 Years Old Intervened on for a Hip Fracture One Year after the Operation. Healthcare 2023, 11, 1520. https://doi.org/10.3390/healthcare11101520
Marrero-Morales PA, González-Dávila E, Hernández-Gutiérrez MF, Gallego-González EM, Jiménez-Hernández M, Sanz-Álvarez EJ, Rodríguez-Novo N, Rodríguez-Novo YM. Functional Status of Patients over 65 Years Old Intervened on for a Hip Fracture One Year after the Operation. Healthcare. 2023; 11(10):1520. https://doi.org/10.3390/healthcare11101520
Chicago/Turabian StyleMarrero-Morales, Pablo A., Enrique González-Dávila, María Fernanda Hernández-Gutiérrez, Eva M. Gallego-González, Martina Jiménez-Hernández, Emilio J. Sanz-Álvarez, Natalia Rodríguez-Novo, and Yurena M. Rodríguez-Novo. 2023. "Functional Status of Patients over 65 Years Old Intervened on for a Hip Fracture One Year after the Operation" Healthcare 11, no. 10: 1520. https://doi.org/10.3390/healthcare11101520
APA StyleMarrero-Morales, P. A., González-Dávila, E., Hernández-Gutiérrez, M. F., Gallego-González, E. M., Jiménez-Hernández, M., Sanz-Álvarez, E. J., Rodríguez-Novo, N., & Rodríguez-Novo, Y. M. (2023). Functional Status of Patients over 65 Years Old Intervened on for a Hip Fracture One Year after the Operation. Healthcare, 11(10), 1520. https://doi.org/10.3390/healthcare11101520





